Академический Документы
Профессиональный Документы
Культура Документы
Communicable Diseases
Загружено:
Carlo DadisИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Communicable Diseases
Загружено:
Carlo DadisАвторское право:
Доступные форматы
COMMUNICABLE DISEASES NEUROLOGICAL SYSTEM
TETANUS ALSO KNOWN AS LOCK JAW
Description: Etiology:
An acute infection associated with painful muscular spasm Caused by Clostridium tetani which are found on soils and human feces Contamination of wound 5 10 days The organism enters the wound and under low oxidation reduction potential the organism reproduces and secrets tetanolysin which causes RBC and WBC lysis. Tetanospamin which attaches to and destroy inhibitory neurons which leads to painful muscle spasm. Fever, lock jaw, the most important sign is trismus and risus sardonicus. While laryngospasm is the most life threatening condition. None. History of wound and possible contamination are usually enough to arouse suspicion and take necessary management. Wash wound, apply wound antiseptic. Assess for history of immunization Give tetanus toxoid for negative history of immunization Administer Antitoxin after negative skin test Penicillin is the drug of choice Prepare for intubation. NGT feeding may become necessary. Avoid over stimulation to prevent painful muscle contraction. Diazepam is the drug of choice for muscle spasm MENINGITIS
Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms
Diagnostic procedure Management
Description: Etiology:
An acute inflammation of the meninges Caused by Nesseria meningitides this is usually a normal inhabitant of the nasopharynx. Droplet infection 2 10 days The organism enters the bloodstream after invading the respiratory tissues. Reaches the spinal cord and of course the meninges. It stimulates chemotaxis that leads to leukocyte infiltration of the
Mode of transmission: Incubation period: Pathophysiology:
meninges. As a result inflammation follows. This build up pressure, pus and compresses sensitive nervous tissues, that may decrease the level of consciousness and in more severe cases pus could impede blood flow and brain infarct my ensue. Signs and symptoms The most significant finding indicating meningeal irritation: brudzinski and kernigs sign. Other sign observable are headache, opisthotonus, fever and petechiae Lumbar puncture (CSF analysis)
Diagnostic procedure
Management
Institute droplet precaution Rifampicin or Ciprofloxacin for prophylaxis Ampicillin is the drug of choice Ceftriaxone for systemic and CNS infection given in combination with Ampicillin to combat resistant organism. Mass prophylaxis is not needed provided that all children in day care centers who have been exposed are exempted hence they need prophylaxis, this also includes all other children who are close to the infected patient such as when they share eating utensils. Nurses and Doctors are not at risk of having the disease except when close contact occurred like in mouth to mouth resuscitation.
ENCEPHALITIS
Description: Etiology:
Inflammation of the tissues of the Brain Mosquito borne Japanese enceph, West Nile enceph etc Viral borne Complication of chicken pox or measles Amebic Acanthamoeba hystolytica Mosquito borne bite of the infected mosquito Viral may be droplet or airborne Amebic accidental entry in the naso - pharynx due to swimming in infested waters. Mosquito borne varied Viral 5 15 days Amebic 3 7 days
Mode of transmission:
Incubation period:
Pathophysiology:
The infectious organism regardless of the type penetrate the brain and causes inflammation of the brain tissues it self. the inflammatory response compresses the brain structure which explains the rapid deterioration of the LOC. Encephalitis is more severe than meningitis. Marked decrease in LOC. Brudzinski and kernigs may also be present if meningeal irritation result. The most significant though is the appearance of decorticate and decerebate rigidity. Lumbar Tap (CSF analysis) EEG
Signs and symptoms
Diagnostic procedure
Management
Primarily supportive. The body can neutralize the organism thru the presence of antibody. Amebic encephalitis may benefit from metronidazole. Anti inflammatory may be given Mannitol could decrease ICP
POLIOMYELITIS
Description: Etiology: Mode of transmission:
An acute paralytic infection that destroys the affected nerves. Caused by polio virus 1 (Brunhilde), 2 (Lansing), 3 (Leon) Fecal oral route. Particularly rampant among those in the squatters area who have no access to sanitary toilet facilities 7 14 days The virus enters the oral cavity and reproduces in the intestines which later penetrate the intestinal wall causing viremia and reaching the motor nerves and the spinal cord. The virus reproduces inside the nerve and as they are released, the infected cell die, hence paralysis results. Pokers sign, Haynes sign, tonsillitis, abdominal pain and flaccid paralysis Stool exam, pandys test, EMG Prevention OPV No anti viral therapy. Toilet hygiene must be reinforced Watch out for respiratory paralysis Assist in rehabilitation (physical therapy and comfort measures OPV is preferred over IPV because the latter can only provide RABIES
Incubation period: Pathophysiology:
Signs and symptoms
Diagnostic procedure Management
Description: Etiology:
Another acute viral infection which have a zoonotic origin Primarily carried by mammals specially land and aerial mammals. In the Philippines Dogs and Cats are among the most important reservoir. The causative organism is Rhabdo Virus Bite of infected animal. Scratch wound from cats can also cause infection since cats usually lick their paws. 10 days for man 14 days for animals The virus replicates at sight of infection which later proceeds to infect the nearby axons and then reaches the nerve it self. From that point onwards the virus travels along the nerve pathway to reach the brain.
Mode of transmission:
Incubation period: Pathophysiology:
In the brain the virus insights inflammatory reaction that give rise to the appearance of encephalitis like symptoms later the organism descends from the brain and exit to affect other nerves in he body. The affectation of trigeminal nerve causes throat spasms which gives rise to its classic finding hydrophobia Signs and symptoms Hydrophobia, aerophobia, laryngeal, Pharyngeal spasm excessive salivation. Fluorescent antibody Staining, Negri bodies found in brain biopsy of the infected animal Human Diploid Cell Vaccine, Rabies Immunoglobulin, Rabies Anti serum. tetanus anti serum is also given if with negative or inadequate immunization history Wash wound with soap and water, may apply wound antiseptic Once sign and symptoms are present passive immunization is already useless. Supportive therapy comes next. Protect from glare and sunlight, protect from water and air current. Cover IV bottle and tubing with carbon paper or any other else that can effectively hide the iv fluids. Secure consent and restrain the patient. Observed contact and droplet precaution.
Diagnostic procedure
Management
LEPROSY
Description:
A chronic infection that usually affects the peripheral nerves and leads to paresthesias A possible zoonotic infection which is rarely cultured in laboratory but seen to be growing freely among armadillo. Causative organism is Mycobacterium leprae
Etiology:
Mode of transmission:
Droplet infection is the most important transmission. Skin contact may cause infection only if there is an open lesion with prolonged contact. 6 months to 8 years The organism enters the body via droplet infection. It is ingested by macrophages but cant be killed, as this circulating macrophage reaches the skin the bacteria penetrate the nerves. Later due to immune recognition WBC attacks the infected cell which results to the destruction of the affected cell hence the appearance of paresthesias and consumption of the involved extremity becomes apparent due to immune response it self. Painless wound, paresthesias, ulcer that does not heal, leonine appearance, maderosis. Nerve involvement with acid fast bacilli is the pathognomic sign of leprosy Scraped incision method.
Incubation period: Pathophysiology:
Signs and symptoms
Diagnostic procedure
Management
Institute concurrent disinfection specially of nasal discharge. Prevention is achieved by BCG immunization Rifampin, Dapsone and lampreme are effective treatment against this infection
CIRCULATORY SYSTEM DENGUE HEMORRHAGIC SHOCK SYNDROME
Description: Etiology:
An acute arthropod borne infection which causes massive bleeding. Causative organism is Dengue virus 1, 2, 3 and 4 the primary vector is Aedes egypti other wise known as tiger mosquito because of the black stripes present at the dorsal legs of the insect. The mosquito prefers to thrive on clean stagnant water. Bite of the infected vector mosquito 6 7 days The virus is carried by the infected mosquito and transferred through bites in the victim. Once the proboscis pierced the capillaries it also leaves the viral organism. The virus mixes in the bloodstream survive and reproduce causing viremia which explains the appearance of generalized flushing. The virus will then successfully enters the bone marrow and arrest the maturation of megakaryocyte. Since the precursor of platelets can not take full course it will result to massive drop in the patients platelet count which significantly raises the risk for hemorrhage. Petechiae, bleeding, epitaxis, Hermans sign and fever Tourniquet test, platelet count. Watch out for bleeding. Minimize injections and other parenteral procedures if possible. Apply pressure for 10 minutes on injection site. Avoid aspirin use acetaminophen provide TSB as an adjunct to anti pyretics. Monitor platelet closely. Prepare for platelet concentrate or fresh whole blood as the need may call for it. Hydrate with PNSS Preventive measure focuses on 4 o clock habit Use DEET as an effective mosquito repellant Use mosquito nets MALARIA
Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms Diagnostic procedure Management
Description: Etiology:
Another type of mosquito borne infection most common in the tropics The causative organisms are Plasmodium Vivax, Falciparum, Ovale,
and Malariae. The primary vectors are anopheles mosquitoes. Mode of transmission: Incubation period: Bite of the infected mosquito For Falciparum 12 days, for Vivax and Ovale 14 days and for Malariae 30 days From the bite of the infected mosquito the organism enters the body via bloodstream and immediately proceed to the liver in the form of sporozoites. Inside the hepatocytes reproduction continues until the host burst releasing the parasite in the form trophozoites that enters the RBC, inside it the organism divides and form schizont. This will later produce merozoites that enters RBC the process causes drop in the number of circulating RBC leading to anemia and cachexia. A cycle of hot stage (high fever) followed by diaphoretic stage (sweating) and then cold stage (chilling). The cycle repeats leading to malarial cachexia Malarial smear or peripheral blood smear Chloroquine is the drug of choice. Primaquine must be given to prevent relapse. Prevent by using mosquito repellant and mosquito net Chloroquine is the drug of choice for prophylaxis.
Pathophysiology:
Signs and symptoms
Diagnostic procedure Management
FILIRIASIS
Description: Etiology: Mode of transmission: Incubation period: Pathophysiology:
A chronic lymphatic disorder that is related to elephantiasis Causative organism is Wuchereria bancrofti primary vector Culex spp. Bite of the infected mosquito 6 12 months The organism enters the body after the vectors bite, it then matures and migrate on the lymphatic vessels but it usually affects those in the lower extremity. The protozoal parasite crowds and destroy the filtering ability of the lymph nodes which then leads to the accumulation of lymph or body fluids causing edema and at worst cases gross deformity hence it could lead to elephantiasis. Recurrent low grade fever, lymphangitis, nocturnal asthma and in worst cases elephantiasis Microscopic examination of peripheral blood. Use of mosquito repellant and nets
Signs and symptoms
Diagnostic procedure Management
Hetrazan is effective against Filiriasis adverse reaction though are seen in a number of patients, if such may be present may use Ivermectin
RESPIRATORY SYSTEM DIPHTHERIA
Description:
An acute infection of the upper respiratory system whose complication may include the lower respiratory tract. The organism, Corynebacterium diphtheriae is ubiquitous. Droplet infection is the means of spread 1 7 days The organism infects the oral cavity which later due to its ability of releasing toxins causes the death of the involved tissues. This gives rise to the appearance of psudomembarne which may be dislodge and block the airway. As toxins are secreted the heart, kidney and the nerves absorb it, this toxins halt protein synthesis of the infected cell which later on causes its death. Pathognomonic Sign is pseudo membrane. Tonsillitis may also be present. Fever and malaise. If complication arises paralysis, endocarditis and kidney failure may be seen. Throat swab Gather specimen for culture Prepare for epinephrine and possible intubation Be ready for antitoxin therapy after checking for allergy Administer penicillin or erythromycin
Etiology: Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms
Diagnostic procedure Management
PERTUSIS
Description:
A widespread organism that threaten any one who have no immunity against it. Causative organism is Bordetella pertussis Droplet infection
Etiology: Mode of transmission: Incubation period:
7 21 days Pathophysiology: The organism enters the upper respiratory tract attaches to the respiratory epithelium and causes an increased production of cyclic amino phosphate that essentially leads to hyperactivity of the mucous secreting cells. Thick tenacious secretions blocks the airway. The organism also halts the mucociliary escalator leaving coughing reflex the last effective protective mechanism of expelling sputum. Due to its relative tenaciousness the body experiences difficulty in coughing out phlegm thus we observe patient to manifest violent cough. Pathognomonic of this infection is violent cough w/out intervening inhalation followed by an inspiratory whoop. Vomiting may be present, Increased in ICP and IOP are also seen. Hernia is also a high risk incident. Throat swab Penicillin, Erythromycin ; Mucolytic may be ordered. Nebulization may also be indicated; Provide small feedings Apply abdominal binder ; Avoid dust and drafts TUBERCULOSIS
Signs and symptoms
Diagnostic procedure Management
Description: Etiology: Mode of transmission: Incubation period: Pathophysiology:
A chronic lung infection that leads to consumption of alveolar tissues Causative organism is acid fast bacillus mycobacterium tuberculosis. Droplet infection as well as airborne 2 4 weeks The bacilli is inhaled and taken in the alveoli where macrophage will ingest but fail to kill the organism. As these macrophages migrate to nearby lymph nodes it will die and leave the capsulated bacteria undigested. Once the bodys immune system dropped, the bacteria will be activated and stimulate immune response which likewise damage the alveolar tissues leading to casseation necrosis and could eventually consume the entire lungs if the process is repeated frequently Afternoon fever, night sweats, cough for 2 weeks, anorexia weight loss. Sputum microscopy, CXR, Mantoux test Institute DOTS Give as ordered; Pyrazinamide, Izoniazid, Rifampicin, Ethambutol and Streptomycin. Check for sensitivity to any of the drug mentioned Provide B6 if receiving Izoniazid Watch out for visual problem if receiving Ethambutol Ethambutol is contra indicated for children who cant verbalize visual
Signs and symptoms
Diagnostic procedure Management
problems yet.
PNEUMONIA
Description: Etiology:
an acute usually bacterial in nature the most common causative organism is strptococcus pneumoniae ubiquitous, orgainsm and may be transferred among population that has poor ventilation and impaired respiratory cilliary function. certain disease like measles may promote the development of pneumonia Droplet infection 24 to 72 hrs usually 48 hrs the organism enters the respiratory tract and if the cilliary mechanism fails to prevent its further entry the organism then infects the lower respiratory centers where it stimulate an inflammatory reaction. this response leads to migration of WBC in particular with neutrophil hence leukocyte infiltration is seen in chest x-rays as consolidation. the build up puss increases the alveolar presure causing in atelectasis once collapsed alveoli cant participate in gas exchange anymore leading to impaired DOB. Rusty colored sputum is the pathognomonic sign this is caused by WBC infiltrates, RBC and sputum. DOB, increased RR, coughing and in late cases lethargy, cyanosis and death.
Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms
Diagnostic procedure
sputum exam
Management
Co Trimoxazole and gentamycin are the drug of choice. although Cotri is used more widely than gentamycin because of its oral preparation which are allowed to be administered by midwives for patient in far flung areas. instruct the mothers to continue the administration of antibiotic for 5 straight days TSB if in case fever may arise Promote proper room ventilation avoid crowding as much as possible Use Pneumococcal vaccine as indicated
COLDS (CORYZA)
Description: Mode of transmission: Incubation period:
The causative agent comes from adenovirus and rhino virus. Droplet infection, direct contact. 1 3 days
Pathophysiology:
As the virus enters the respiratory tract, it attaches itself to the mucous membrane and causes local irritation and inflammation. In response, the mucous membrane releases mucous to flush out the virus. Since there is an increased in the production of the mucous it usually flows back and causes rhino rhea and because of the nasolacrymal duct, increased mucous production impedes the drainage of tears thus watery eyes is present. Complications: Children otitis media and bronchopneumonia Adult sinusitis General malaise Fever, chills Sneezing, dry and scratchy throat Teary eyes, headache Continues water discharge from nares a. Provide adequate rest and sleep b. Increase fluid intake c. Provide adequate and nutritious diet Encourage vitamins specially vitamin C
Signs and symptoms
Management
INFLUENZA (LA GRIPPE OF FLU)
Description:
A highly contagious disease characterized by sudden onset of aches and pains. Influenza virus A, B, C Droplet infection, contact with nasopharyngeal secretions 24 48 hrs. Upon entry in the upper respiratory tract, it is deposited in the same site and penetrates the mucosal cells. Causing lysis and destruction of the ciliated epithelium the virus releases neuramidase that decreases the viscosity of the mucosa. Facilitating the spread of the infected exudates to the lower respiratory tract, this causes intestinal inflammation, and necrosis of the alveolar and bronchiolar epithelium. Thus, the alveoli are filled with exudates containing WBC, RBC and hyaline cartilage. This places the patient to increased possibility of acquiring bacterial pneumonia usually caused by S. Aureus.
Etiology: Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms
Respiratory most common fever anorexia chills muscle pain and aches coryza sore throat bitter taste orbital pain Intestinal vomiting severe abdominal pain
fever obstinate constipation severe diarrhea Nervous headache Management a. b. c. d. e. f. sulfonamides INTEGUMENTARY SYSTEM SCARLET FEVER (SCARLATINA) provide adequate rest and ventilation tepid sponge bath to reduce the temperature monitor the vital signs provide adequate nutrition assist the patient in conserving strength when she is very weak drug of choice: antibiotics
Description:
Is an acute, febrile, contagious condition characterized by sudden onset usually with vomiting and by punctuate erythematous skin eruption followed by characteristic exfoliation of the skin during convalescence, rapid pulse and sore throat. Group A hemolytic streptococcus group Direct contact, droplet infection and indirect contact 1 7 days The bacterium releases erythrogenic toxins, which causes sensitivity reaction in the body. The toxin can cause toxic injury to the small capillaries of vascular epithelium found in the body. The skin is the site where the manifestations are most visible where one will observed strawberry like tongue, rashes, etc. Complications: sinusitis nephritis otitis media myocarditis/endocarditis mastoiditis
Etiology: Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms
I. Prodomal stage fever tachycardia sore throat vomiting headache abdominal pain body malaise II. Eruptive stage rashes: appears at the end of 24 hours on the chest spread gradually upward and downward enanthem: macular eruption on the hard palate
pastias line: due to the grouping of macules found around the folds of the skin particularly on the elbow tiny subcuticular vesicles: found in the cuticles of the nails strawberry tongue: tongue becomes red at the edges and enlarged papillae show raspberry tongue: circumoral pallor III. Desquamation (8 10 days) skin begins to peel shedding of the hair and nails Diagnostic procedure Scultz-Charlton rash extinction or blanching test for sensitivity to scarlet fever antitoxin Dick test determines whether or not a person is naturally immune to scarlatine nasal swab Laboratory: positive throat culture for strep elevated ASO titer white and differentiated count high as 50,000 increae in eosinophils isolation medical aseptic technique bed rest keep the patient warm at all times and avoid drafts apply ice cap/packs for high fever give TSB for high temperature increase oral fluid intake take vital signs q 3 4 hrs daily bath should be given: sodium bicarbonate or starch is used in excessive itching and oil rub after bath is useful i. use of mouthwashes and gargles for good oral hygiene j. prevent exoriations by wiping nasal discharges with soft tissues and application of cold creams k. encourage daily elimination l. diet should be of high calorie foods and fruit juices, milk cream and soups Medical management: a. antitoxins b. convalescent serum c. samma globin administered IM d. sulfonamides antibiotics penicillin (for cleaning the throat of streptococcus) a. b. c. d. e. f. g. h.
Management
LEPROSY (HANSENS DISEASE, HANSENOSIS, LEPRAE, LEONTHIASIS)
Description:
A chronic infectious disease characterized by the appearance of modules in the skin or mucous membranes or by changes in the nerves leading to anesthesia, paralysis or other changes
Etiology:
Mycobacterium leprae (acid fast bacillus), sporadic/endemic cases, occurs in tropical and semitropical countries throughout the world. It can be contracted in childhood (manifested at age 15 and diagnosed by the age of 20 years). Prognosis: > the longer the time of active disease, severe lesions, the more rapidly they have advanced without ability to produce the lepromin reaction the poorer the prognosis
> case under 21 years old high relapse rate Mode of transmission: Incubation period: Pathophysiology: Prolonged intimate skin to skin contact, nasal secretions Prolonged, undetermined and varies from one to many years The bacterium, which is an acid-fast bacillus, attacks the skin tissues and peripheral nerve, which causes skin lesions, anesthesia, infection and deformities Assessment: 1. Tuberculoid type shows high resistance to Hansens bacilli. Clinical manifestations are mainly in the skin and nerves and usually are used or non-infectious. 2. Lepromatous type minimal resistance to the multiplication, existence of the bacillus, constant presence of large numbers in the lesions and form globi (characteristic manifestations in the skin and mucus membranes) and peripheral nerves. 3. Open or infectious cases 4. Inderterminate type clinical manifestations are located chiefly in skin and nerves; lesions are flat macules. 5. Borderline Clinical Manifestations: 1. Early stage loss of sensation paralysis of extremities absence of sweating (anhydrosis) nasal obstruction loss of hair (eyebrows) eye redness change in the skin color ulcers that does not heal muscle weakness 2. Late symptoms contractures leonine appearance (due to nodular and thickened skin of the forehead and face) madarosis (falling of eyebrows) synecomastia sinking of bridge of nose 3. Cardinal signs presence of Hansens bacilli presence of localized areas of anesrhesia peripheral nerve enlargement a. Lepromin reaction a positive test develops a nodule at the site of inoculation (first and third week) b. Wassermann reaction Planning and implementation a. Prevention separate infants from lepromatous parents at birth segregate and treat open cases of leprosy require public health supervision and control of cases of Hansens disease b. Medical management 1. Multiple drug therapy paucibacillary treatment six months or until negative (-) results occur refampicin once a month dapsone - once a day
Signs and symptoms
Diagnostic procedure
Management
c. d. e. f. g. h.
2. Multibacillary treatment for 2 consecutive years or until negative (-) for leprosy test rifampicin once a month lamprene once a day dapsone once a day full, wholesome generous diet alcohol or TSB may be used for high fever patient should have a daily cleansing bath and change of clothing good oral hygiene normal elimination should be maintained meticulous skin care for ulcers
MEASLES (RUBEOLA, MORBILLI, 7 DAY MEASLES) An extremely contagious exanthematous disease of acute onset which most often affects children and the chief symptoms of which are referable to the upper respiratory passages. The causative agent is the paramyxo virus Etiology: Nasal throat secretions, droplet infection, indirect contact with articles Mode of transmission: 8 20 days Incubation period: Pathophysiology: As the virus enters the body it immediately multiplies in the respiratory epiyhelium. It disseminate by way of the lymphatic system causing hyperplasia of the infected lymphoid tissue. As a result there is a primary viremia which infects the leukocyte and involves the whole reticuloendothelial system. As the infected cells die it necrose and release more viruses to infect other leukocytes leading to secondary viremia, which also causes edema of upper respiratory tract producing its symptoms and it may predispose to pneumonia. Complications: otitis media bronchopnuemonia severe bronchitis Prognosis: death rate is highest in the first two years of life (20%) after 4 years uncommon over all mortality less than Assessment: a. Stages 1. incubation period (average of 10 days) 2. Pre-eruptive stage or stage of invasion (3-6 days) from the appearance of the first signs and symptoms to the earliest evidence of the eruption. fever, severe cold frequent sneezing profuse nasal discharge eyes are red and swollen with mucopurulent discharge (lids stick together) Stimsons sign (puffiness of lower eyelids with definite line of congestion on the conjunctivae) redness of both eardrums vomiting, drowsiness
Description:
Signs and symptoms
hard, dry cough Kopliks spot (appears on second day): small bright, red macules or papules with a tiny or bluish-white specks on the center and can be found on the buccal cavity macupapular rashes (seen late in 4th day): appears first on the cheeks or at the hairline true measles rash: slightly elevated sensation to touch, appears first on the face and spreads downward over neck, chest trunk, limbs and appearing last on the wrist and back of the hand 3. Eruptive stage characterized by a general intensification of all local constitutional symptoms of the preeruptive stage with the appearance of bronchitis and loose bowels irritability and restlessness red and swollen throat enlargement of cervical glands fever subsides 4. Desquamation stage follows after the rash fades follows the order of distribution seen in the formation of eruption Diagnostic procedure No specific diagnostic exam except only for the presence of leucopenia. a. prevention education of parents regarding the disease passive immunization of infants and children (gammaglobulin) active immunization (1st year of life) b. management drugs antibiotics sulfodiazine isolation meticulous skin care warm alcohol rub to prevent pressure sores good oral and nasal hygiene increase oral fluid intake proper care of the eyes eye screen to avoid direct light; wear dark glasses ears should be cleaned after bath if there is discharges patient should lie the affected ear down or towards the bed give ample of fluids during febrile stage
Management
GERMAN MEASLES (RUBELLA, ROTHEIN, ROSEOLA, 3-DAY MEASLES)
Description:
An acute infectious disease characterized by mild constitutional symptoms, rose colored macular eruption which may resembles measles and enlargement and tenderness Caused by myxovirus. Occurs mostly in spring and seen mostly in children over 5 years of age
Etiology:
Mode of transmission:
Direct contact
Incubation period:
14 21 days Period of communicability 7 days before to 5 days after the rash appears As the virus gains entrance to the nasopharynx, it immediately invades the nearest lymph gland causing lymphadenopathy. Later on, the virus enters the blood stream that stimulates the immune response, which is the cause of rashes found in the body of infected individual. If rashes has appeared it means that viremia has subsided. Since the disease is generally mild and serious complication has ha been very rare, what should be watched out rather are its congenital effects because it can cross the placental barrier, which may kill the fetus or cause congenital rubella syndrome. Complications: otitis media encephalitis transient albuminuria arthritis congenital defects for babies whos mother were exposed in early pregnancy Prognosis: very favorable fever, cough loss of appetite enlargement of lymph nodes sweating leucopenia vomiting (in some cases) headache, mild sore throat desquamation follows the rash enanthem of uvula with tiny red spots rash (cardinal symptom) accompanied with cervical adenitis: begins on the face including the area around the mouth; oval, pale, rose-red papules about the size of a pinhead; covers the body within 24 hours and gone by the end of the 4th day
Pathophysiology:
Signs and symptoms
Management
Planning and implementation a. Prevention: vaccination gamma globulin given to pregnant women with negative history and who have been exposed in the first trimester of pregnancy include in MMR given at 15months to the baby b. management isolation (catarrhal stage to prevent infection to others) bed rest for first few days meticulous skin care especially after the rash fades good oral and nasal hygiene (use of petroleum jelly if lips become dry) no special diet is necessary, increase oral fluid intake
VARICELLA (CHICKEN POX)
Description:
A very contagious acute disease usually occurring in small children, characterized by the appearance of vesicles frequently preceded by papules, occasionally followed by postules but ending in crusting Varicella zoster virus (airborne) Droplet infection, direct contact 2 -3 weeks The virus gain entrance via the upper respiratory tract it crosses the mucous membrane and cause systemic infection followed by appearance of numerous macupapular rash. The rash are fluid filled that contain polymorphonuclear leukocytes. Period of communicability: highly contagious from 2 days prior to rash to 6 days after rash erupt. Full blown case imports permanent immunity. Complications: pneumonia nephritis encephalitis impetigo pitting or scarring of the skin slight fever: first to appear body malaise, muscle pain eruption (maculopapular) then progresses to vesicle (3-4 days); begins on trunk and spreads to extremities and face (even on the scalp, throat and mucus membranes) intense pruritus vesicles ended as a granular scab irritability
Etiology: Mode of transmission: Incubation period: Pathophysiology:
Signs and symptoms
Management 1.
Drugs penicillin can be used when the crusts are severe or infected to prevent scarring or secondary invasion alkalinizing agent to prevent nephritis and to stop vomiting acyclovir, immunosin antiviral hydrocortisone lotion 1% for itching 2. isolation in a room by itself 3. provide a well ventilated, warm room to the patient 4. warm bath should be given daily to relieve itching; use a calamine lotion 5. avoid injuring the lesions by using soft absorbent towel and the patient should be patted dry instead of rubbed dry 6. maintain good oral hygiene, if lesions are found in the mouth or nasal passages, antiseptic prep may be used diet should be regular
HERPES ZOSTER (SHINGLES) Description: Acute viral infection of the peripheral nervous system due to
reactivation of varicella zoster virus. The virus causes an inflammatory reaction in isolated spinal and cranial sensory ganglia and the posterior gray matter of the spinal cord. Contagious to anyone who has not had varicella or who immunosupressed. Signs and symptoms neuralgic pain malaise burning fever cluster of skin vesicles along course of peripheral sensory nerves (unilateral and found in trunk, thorax or face); appears 3-4 days 1. drugs analgesics corticosteroids acetic acid compresses or white petrolatum anti-viral (acyclovir) 2. isolate client 3. apply drying lotion 4. administer medications as ordered instruct client to preventive measures
Management
SCABIES
Description:
An infection of the skin produced by burrowing action of a parasite mite resulting in irritation and the formation of vesicles or postules. Itchmite, sarcoptes scabei, occurs in individual living in area of poverty where cleanliness is lacking. Direct contact with infected persons, indirect contact through soiled bed linens, clothing and others. Both female and male parasites live on the skin. A female parasite burrows into the superficial skin to deposit eggs. Pruritus occurs and scratching of skin may produce secondary infection. Scattered follicular. Eruption contains immature mites. Inflammation may produce postules and crust. Eggs is hatched in 4 days. Larvae undergo a series of matts before becoming adult. Life cycle is complete in 1-2 weeks. intense itching especially at night sites between fingers or flexor surfaces of wrists and palms, around nipples, umbilicus, in axillary folds, near groin or gluteal folds, penis, scrotum. Presence on skin of female mite, ova and feces upon skin scrapping. a. Take a warm soapy shower bath or bath to remove scaling debris from crusts. b. Apply prescribed scabicide such as: lindane lotion (kwell) 1% crotamiton (Eurax) cream or lotion
Etiology:
Mode of transmission:
Incubation period: Pathophysiology:
Signs and symptoms
Diagnostic procedure Management
c.
6-10% precipitate of sulfur in petrolatum encourage to change clothing frequently
RINGWORM (TRICHOPHYTOSIS)
Description:
A group of diseases caused by a number of vegetable fungi and affecting various portion of the body in different ways (skin, hair, nails) TINEA PEDIS (Athletes foot) a superficial fungal infection due to trichophyton Rubrum, mentagrophytes, or epidermophyton floccosum which may manifest itself as an acute, inflammatory, vesicular process or as chronic rash involving the soles of the feet and the inter-digital web spaces. particularly common in summer, contracted swimming area and locker rooms. TINEA CORPORIS or TINEA CIRCINATA ringworm of the body. TINEA CRURIS (Jock itch) superficial fungal infection of the groin which may extend to the inner thigh and buttocks areas and commonly associated with tinea pedis. TINEA CAPITIS (ringworm of the scalp) caused by microsporum canis, trichophyton tonsurans. usually spread through child to child contact, use of towels, combs, brushes and hats kitten and puppies may be the source of the infection primarily seen in children before puberty
Etiology:
Signs and symptoms
TINEA PEDIS scaly fissures between toes, vesicles on sides of feet pruritus burning and erethema lymphangitis and cellulites may occur TINEA CORPORIS or TINEA CIRCINATA intense itching appearance: begins as scaling erythematous lesions advancing to rings of vesicles with central clearing and appears on exposed areas of body. TINEA CRURIS dull red brown eruption of the upper thighs and extends to form circular plaques with elevated scaly or vesicular borders. itching seen most in joggers, obese individuals and those wearing tight undercoating. TINEA CAPITIS reddened, oval or round areas of alopecia presence of kerion: an acute inflammation that produces edema, postules and granulomatous swelling
Diagnostic procedure
TINEA PEDIS direct examination of scrapings (skin, nails, hair) isolation of the organisms in culture
TINEA CAPITIS
woods lamp microscopic evaluation
Management
TINEA PEDIS a. Prevention: instruct client to keep feet dry such as by using talcum powder. b. Management: Drugs: topical agent, clotrimazole, miconazole, tolnaftate Systemic anti-fungal therapy: griseofulvin, ketoconazole Elevate feet for vesicular type o pain infection. TINEA CORPORIS or TINEA CIRCINATA a. Prevention: infected pet is a common source and should be inspected and treated by a veterinarian. b. Management see treatment for tinea pedis wear clean cotton clothing next to skin use clean towel daily dry all areas and skin folds thoroughly use self monitoring for signs of re-infection after a course of therapy. TINEA CRURIS a. Prevention: avoid nylon underclothing, tight-fitting underwear and prolonged wearing of wet bathing suit. b. Management: Drugs topical therapy (miconazole cream); griseofulvin (oral) avoid excessive washing or scrubbing; wear cotton underwear. TINEA CAPITIS same with other fungal infection
GASTROINTESTINAL DISORDERS TYPHOID FEVER (ENTERIC FEVER)
Description:
A general infection characterized by the hyperplasia of the lymphoid tissues, especially enlargement and ulcerations of the Peyers patches and enlargement of the spleen, by parechymatous changes in various organs and liberation of an endotoxin in the blood. Salmonella typhosa, prevalent in temperate climates, high incidence in fall, and mostly affected are the males and in youth and infant. Infected urine and feces and intake of contaminated food and water The organism enters the body via the GI tract and invades the walls of the GI tract leading to bacteremia that localizes in mesenteric lymph nodes, in the masses of lymphatic tissue, in the mucus membrane of the intestinal wall (Peyers patches) and in small, solitary lymph follicles in the ileum and colon thus ulceration of the intestines may result. Complication: perforation of the intestine from erosion of one of the ulcers intestinal hemorrhage from erosion of blood vessels
Etiology:
Mode of transmission: Pathophysiology:
meningitis Signs and symptoms
relapse thrombophlebitis urinary infection
a. Gradual onset severe headache, malaise, muscle pains, nonproductive cough chills and fever, temperature rises slowly pulse is full and slow skin eruption irregularly spaced small rose spots on the abdomen, chest and back; fades 3-4 days splenomegally b. Second week fever remains consistently high abdominal distention and tenderness, constipation or diarrhea delirium in severe infection coma-vigil look; pupils dilate and patient appears to stare without seeing sultus tendium twitching of the tendon sets c. Third week gradual decline in fever and symptoms subsides
Diagnostic procedure
white blood cell counts blood or bone marrow culture positive urine and stool cultures in later stage blood serum agglutination (+) at the end of scond week a. Prevention: decontamination of water sources, milk pasteurization, individual vaccination of high risk persons, control carriers. b. Drugs chloramphenicol ampicillin sulfamethoxazole trimethoprim furazolidone c. intravenous infusion to treat dehydration and diarrhea d. Nursing care give supportive care position the patient to prevent aspiration use of enteric precautions TSB for high fever encourage high fluid intake monitor for complications e. intestinal decompression procedure, IV fluids and surgical intervention for perforation withhold food, blood transfusions and bowel resection for intestinal hemorrhage
Management
LEPTOSPIROSIS (WEILS DISEASE, CANICOLA FEVER, HEMMORHAGIC JAUNDICE, ICTEROHEMORRHAGIC SPIROCHETOSIS, SWINEHERDS DISEASE, MUD FEVER)
Description:
Worldwide in its distribution and especially in areas where sanitation is poorest; common in Japan. Usually those who are affected are the
sewer workers, miners and swimmers in polluted water. Etiology: Incubation period: Signs and symptoms Leptospira icterohaemorrhagiae carried by wild rat 5 6 days sudden onset with chills, vomiting and headache by severe fever and pains in the extremities intense itching of the conjunctivae severe jaundice with hemorrhage in the skin and mucus membranes hematemesis, hematuria and hepatomegaly for severe cases convalescence occurs in the third week unless there is a complication Positive agglutination test Prevention eradication of rats and environmental sanitation Drugs antiserum or convalescent serum; penicillin Nursing care supportive and symptomatic
Diagnostic procedure Management
DYSENTERY
Etiology:
BACILLARY DYSENTERY (shigellosis, bloody flux) caused by shigella dyseteriae and shigella paradysenteriae coming from bowel discharges of infected persons and carriers. VIOLENT DYSENTERY (Cholera) caused by vibrio cholera, vibrio comma (ogawa and inaba) from infected feces or vomitus.
Mode of transmission:
BACILLARY DYSENTERY eating of contaminated foods, hand to mouth transfer of contaminated material, flies, objects soiled with discharges of infected person, contaminated water. VIOLENT DYSENTERY direct or indirect fecal contamination of water or food supplies by soiled hands, utensils or mechanical carriers such as flies. BACILLARY DYSENTERY 1-7 days (average of 4 days) period of communicability during acute phase and until (-) stool exam VIOLENT DYSENTERY from a few hours to five days (average 3 days) period of communicability until the infectious organism is absent from the bowel discharges (7-14 days)
Incubation period:
Signs and symptoms
BACILLARY DYSENTERY chills fever nausea and vomiting tenesmus severe fiarrhea accompanied by blood and mucus alternating episodes of diarrhea and constipation (chronic) VIOLENT DYSENTERY a. Onset acute colicky pain in the abdomen mild diarrhea (yellowish)
marked mental depression headache, vomiting fever, may or may not be present b. Collapse stage after 1 or 2 days profuse watery stools (grayish white or rice water) thirst severe/violent cramps in the legs and feet thickly furred tongue sunken eyeballs ash-gray colored skin c. Reaction stage after 3 days increased consistency of stools skin becomes warm and cyanosis disappear peripheral circulation improves urine formation increases Diagnostic procedure BACILLARY DYSENTERY stool exam serologic test VIOLENT DYSENTERY (+) stool exam/vomitus BACILLARY DYSENTERY a. Methods of control and prevention recognition of disease and reporting concurrent disinfection from bowel discharges investigation of source of infection (food, water and milk supplies, general sanitation and search for carriers) prevention of flybreeding, screening sanitary disposal of human excreta protection and purification of public water supplies and prevention of subsequent contamination b. Drugs kaolin bismuth and paregoric (combination of sulfonamide) chloramphenicol c. Nursing care isolation by medical aseptic technique daily cleansing bath increase oral fluids in acute stage TSB for fever record and the character of stools passed, amount and frequency of vomiting VIOLENT DYSENTERY a. Prevention immunization screen the sickroom from flies protect the food supplies for contamination b. Drugs tetracycline c. Replacement of fluids and electrolytes d. Isolation e. Patient should be spared all unnecessary efforts during the acute stage f. Buttocks should be kept clean with warm water and soap and rubbed dry g. antiseptic mouthwash in case of vomiting fluids is given as soon as they can be tolerated
Management
MUMPS (INFECTIOUS OR EPIDEMIC PAROTITIS)
Description:
An acute contagious disease the characteristic feature of which is the swelling of one or both of the parotid glands usually occurring in epidemic form. Filterable virus, member of myxovirus family, infected oral and nasal secretions is the source of infection Complication: orchitis or epididymp-orchitis Prognosis: favorable in most cases of mumps, complete recovery ordinarily takes place even complications take place. Direct contact with a person who has the disease or by contact with articles which is contaminated. 14 21 days period of communicability: before the glands is swollen to the time present of localized swelling pain in the parotid region headache earache fever difficulty to open the mouth wide general malaise sore throat
Etiology:
Mode of transmission:
Incubation period:
Signs and symptoms
Diagnostic procedure
moderate leukocytosis complement fixation test skin test for susceptibility to mumps a.Prevention: immunization (MMR given at 15 months) b.Drugs aspirin for fever, cortisone c.isolation d.absolute bed rest to prevent complications (at least 4 days) e.daily bath should be given f.soft bland diet for sore jaw g.advise male to wear well fitting support to relieve the pull of gravity on the testes and blood vessels h.TSB for fever ice pack/collar application
Management
PARASITISM Description: Etiology: PINWORM (Enteropiasis) oxyuris vermicularis, occurs from fomites, autoinfection, fecal contamination, affects one in family and invariably infects entire family. GIANT INTESTINAL ROUNDWORMS (Ascariasis) ascaris lumbricoides, from sputum and ova in soil. THREADWORM strongyloides stercoralis, from fecal soil contamination WHIPWORM (trichuriasis) from fecal soil contamination HOOKWORM (ancylostomiasis) from larvae in fecal soil contamination TAPEWORM (taeniasis)
Types:
hymenolepis nana from fecal contamination taenia saginata (beef) from insufficiently cooked meat taenia solium (pork) contaminated meat diphyllobothrium latun poorly cooked infested fish
Mode of transmission:
PINWORM mouth GIANT INTESTINAL ROUNDWORMS mouth THREADWORM enter usually through the skin or feet WHIPWORM mouth HOOKWORM through skin of the feet TAPEWORM - mouth PINWORM eosinophilia, itching around the anus, convulsions in children. GIANT INTESTINAL ROUNDWORMS chest pain, cough after two months, malnutrition, indigestion, diarrhea, colicky abdominal pain. THREADWORM intermittent diarrhea WHIPWORM nausea and vomiting, diarrhea, anemia, stunted growth; may cause prolapse of rectum in children and occasionally appendicitis. HOOKWORM anemia, diarrhea, stunted growth, bronchial symptoms, obstruction of the biliary and pancreatic duct. PINWORM adults and ova in stool GIANT INTESTINAL ROUNDWORMS adults and ova in stool THREADWORM larvae WHIPWORM ova in stool HOOKWORM ova in stool TAPEWORM ova and segments of the worm in the stool THREADWORM Prevention: wear shoes and use sanitary toilets use of sanitary toilets provide hygiene education of the family dispose of the infected stools carefully meticulous cleansing of skin especially anal region, hands and nails drugs antihelminthic drugs, piperazine citrate, pyrantel pamoate, mebendazole
Signs and symptoms
Diagnostic procedure
Management
HEPATITIS
Description:
Widespread inflammation of the liver tissue with liver cell damage due to hepatic cell degeneration and necrosis; proliferation and enlargement of the Kuffer cells and inflammation of the periportal areas thus may cause interruption of bile flow. TYPE A (infectious hepatitis) occurs in crowded living conditions; with poor personal hygiene or from contaminated food, milk, water or shellfish. Common occurrence during fall and winter months usually affecting children and young adults. TYPE B (serum hepatitis, SH virus, viral hepatitis, transfusion hepatitis, homologous serum jaundice)
Etiology:
TYPE C (non-A, non-B hepatitis) Mode of transmission: TYPE A fecal/oral route TYPE B blood and body fluids (saliva, semen, vaginal secretions), often from contaminated needles among IV drug abusers, intimate/sexual contact. TYPE C by parenteral route, through blood and blood products, needles and syringes TYPE A 15-45 days period of communicability 3 weeks prior and one week after developing jaundice TYPE B 50-180 days TYPE C 7-50 days a.Pre-icteric stage anorexia nausea and vomiting fatigue constipation or diarrhea weight loss right upper quadrant discomfort hepatomegaly spleenomegaly lymphadenopathy b.Icteric stage fatigue weight loss light colored stools dark urine jaundice pruritus continued hepatomegaly with tenderness c.Post-icteric stage fatigue but increased sense of well being hepatomegaly: gradually decreasing a.All 3 types SGPT, SGOT, alkaline phospatase, bilirubin, ER all increased in pre-icteric leukocytes, lymphocytes, neutrophils all decreased prolonged PT b.HEPA A: Hepa A (HAV) in stool before onset Anti-HAV (IgG) appears soon after onset of jaundice, peaks in 1-2 months and persist indefinitely Anti-HA (IgM) positive in acute infection lasts 4-6 weeks c.HEPA B HbsAG (surface antigen) positive, develops 4-12 weeks after infection Anti-HbsAg negative in 80% cases Anti-HBC associated with infectivity, develops 2-16 weeks after infection ABeAG associated with ineffectively and disappears before jaundice Anti-Hbe present in carriers, represents low ineffectivity a. Prevention
Incubation period:
Pathophysiology: Signs and symptoms
Diagnostic procedure
Management
I.Type A II.Type B
good hand washing good personal hygiene control and screening of food handlers passive immunization ISG, to exposed individuals and prophylaxis for travelers to developing countries
b.
screen blood donors HB3Ag use disposable needles and syringes registration of all carriers passive immunization ISG active immunization hepatavax B vaccine and formalin treated hepatitis B vaccine given in 3 doses Nursing management promote adequate nutrition small frequent meals of high CHO, moderate to high CHON, high vitamin, high caloric diet, avoid very hot or cold foods. ensure rest and relaxation monitor/relive pruritus cool, moist compresses, emollient lotion administer corticosteroid as ordered isolation procedures as required provide client teaching and discharge planning with regards to: importance of avoiding alcohol importance of not donating blood recognition/reporting of signs of inadequate convalescence avoidance of persons with known infections Drugs liver protector (essentiale, jectofer, interferon drug)
FOOD POISONING
Description:
A gastroenteritis often produced by the presence of a disease organism or its toxins. SALMONELLA GASTROENTERITIS salmonella typhimurium, salmonella paratyphi A, B, and C; salmonella newport STAPHYLOCOCCUS GASTROENTERITIS coagulase positive, gram positive: grows rapidly on food containing carbohydrates Recovery: within 24 36 hours BOTILISM clostridium botulinum
Etiology:
Incubation period:
SALMONELLA GASTROENTERITIS 6 to 48 hours after the ingestion of contaminated food STAPHYLOCOCCUS GASTROENTERITIS 2 to 6 hours after ingestion BOTILISM 24 hours after the ingestion SALMONELLA GASTROENTERITIS headache
Signs and symptoms
nausea and vomiting diarrhea (stools are usually fluid and contain mucus; bloody if in severe infection) STAPHYLOCOCCUS GASTROENTERITIS sudden abdominal pain excessive perspiration vomiting diarrhea pallor weakness BOTILISM peripheral nervous system vomiting ataxia constipation ocular paralysis aphonia other neufromascular signs paralysis of the respiratory system which may lead to death Diagnostic procedure SALMONELLA GASTROENTERITIS history of illness after ingestion of certain foods SALMONELLA GASTROENTERITIS/STAPHYLOCOCCUS GASTROENTERITIS replacement of fluids and salts sedatives and anticholinergic to reduce hypermobility of the intestine good oral hygiene application of heat to abdomen to relieve cramps BOTILISM prevention regulation of commercial processing of canned foods education of housewives concerning proper processing of home canned foods canned foods should be boiled first to destroy the toxins polyvalent antitoxins (botulinum antitoxin) patient with botulinum should be placed on quiet room and avoidance of unnecessary activity symptomatic intubation for feeding tracheostomy in respiratory failure oxygen by IPPB
Management
SEXUALLY TRANSMITTED DISEASE GONORRHEA (STRAIN, CLAP, JACK, MORNING DROP, G.C. GLEET)
Description:
An infectious disease, which causes inflammation of the mucous membranes of the genitourinary tract. Complications: MALE bilateral epididymitis, sterility FEMALE pelvic inflammatory disease, sterility NEWBORN opthalmia neonatorum mother to child Neisseria gonorrhea
Etiology: Mode of transmission:
Sexual contact Incubation period: Signs and symptoms 2 5 days MALE burning sensation in the urethra upon urination passage of purulent (yellowish) discharge pelvic pain fever painful urination FEMALE burning sensation upon urination presence or absence of vaginal discharge pelvic pain abdominal distention nausea and vomiting urinary frequency culture and sensitivity female: pap smear or cervical smear; male: urethral smear blood exam VDRL educate men and women to recognize signs of gonorrhea and to seek immediate treatment monitor urinary and vowel elimination important to treat sexual partner, as client may become reinfected make arrangements for follow-up culture 2 weeks after therapy is initiated Drugs penicillin: drug of choice tetracyclines ceftriaxone sodium (rocephin) amoxicillin (augmentin)
Diagnostic procedure
Management
SYPHILIS (LEUS, POX, BAD BLOOD DISEASE)
Description:
A contagious disease that leads to many structural and cutaneous lesions Complications: a.still birth b.child born with syphilis placenta is bigger than the baby persistent vesicular eruptions and nasal discharges old man feature mucus patches on mouth and anus c.child born with late syphilis (signs and symptoms after 2 years) hutchinsons teeth deafness saddle nose high palate Treponema pallidum Sexual contact
Etiology: Mode of transmission:
Incubation period: Signs and symptoms
3 6 weeks a.Primary syphilis chancre on genitalia, mouth or anus serous drainage from chancre enlarge lymph nodes maybe painful or painless highly infectious b.Secondary syphilis skin rash on palms and soles of feet reddish copper colored lesions on palms of hands and soles of feet condylomas: lesions/sores that fused together erosions of oral mucus membranes alopecia enlarged lymph nodes fever, headache, sore throat and general malaise c.Tertiary syphilis gumma the characteristic lesions cardiovascular changes ataxia stroke, blindness a.positive test for syphilis venereal disease research laboratory (VDRL) rapid plasma reagin circle card test (CRPR-CT) automate reagin test (ART) fluorescent treponemal antibody absorption test (FTA-ABS) wessermann test khan precipitation test kline, hinton and mazzin tests b.darkfield examination c.culture and sensitivity
Diagnostic procedure
Management
strict personal hygiene is an absolute requirement assist in case finding instruct client to avoid sexual contact until clearance is given by physician encourage monogamous relationship explain need to complete course of antibiotic therapy Drugs penicillin, tetracyclins/kithramycin
ACQUIRED IMMUNE DEFICIENCY SYNDROME (AIDS)
Description:
An acquired immune deficiency characterized by a defect in natural immunity Retrovirus, human immunodeficiency virus (HIV-1 and HIV-2) previously referred to as human T-lymphotropic virus type III (HTLVIII)
Etiology:
Mode of transmission:
Blood transfusion, sexual contact, contaminated needles, perinatal transmission
Incubation period: Pathophysiology: Signs and symptoms
6 months to 9 years
anorexia fatigue dyspnea night sweats fever diarrhea enlarged lymph nodes HIV encephalopathy: memory loss, lack of coordination, partial paralysis, mental deterioration HIV wasting syndrome, emaciation positive test for HIV antibody positive test for presence of HIV itself opportunistic infection: neumocystic carinii, cystomegalovirus, kaposis sarcoma ELISA test (enzyme-linked immunosorbent assay) a screening test western blot a confirmatory test provide frequent rest periods provide skin care provide high-calorie, high protein diet to prevent weight loss provide good oral hygiene provide oxygen and maintain pulmonary function provide measures to reduce pain protect the client from secondary infection; carefully assess for early signs encourage verbalization of feelings teach client the importance of: informing sexual contacts of diagnosis not sharing needle with other individuals continuing medical supervision
Diagnostic procedure
Management
CHLAMYDIAL INFECTION
Description: Etiology:
A sexually transmitted disease that is highly contagious caused by chlamydial organism Chlamydia trachomatis
Mode of transmission: Incubation period: Pathophysiology: Signs and symptoms
2 -3 weeks for males Sexual intercourse pruritus in vagina
burning sensation in vagina painful intercourse pruritus of urethral meatus in men burning sensation during urination Diagnostic procedure Culture of aspirated material from vaginal, anal or penile discharges
Management
doxycycline or azithromycin (recommended for pregnant woman) universal precaution should be practiced
TRICHOMONIASIS Description: Another type of sexually transmitted disease that may also be transmitted by other means such as handling of infected fomites. It is caused by a protozoan parasites. Etiology: Mode of transmission: Trichomonas vaginalis Sexual intercourse, contact with wet towels and wash clothes infected by the organism 4 20 days, usually 7 days vaginal discharge burning and pruritus of vagina redness of the introitus usually asymptomatic in men culture of obtained specimen metronidazole sitz bath may relieve symptom acid douches tetracyclines may be given on male who are also infected
Incubation period: Signs and symptoms
Diagnostic procedure Management
BIOTERRORISM AND PANDEMICS In the recent course of international conflicts, which has lead to war, has used weapon that are quite different from the conventional ones used before. The medical science is being used not to prolong life but to cause immediate death by infection of various biological organisms. The following gives an insight of these dangerous biological terrorism leading to pandemics.
SMALL POX
Description:
For about two decades the WHO has declared that the world is already small pox free. Although eliminated in the world over, the
specimen is still kept in two laboratory facility in the United States. Etiology: Mode of transmission: Incubation period: Signs and symptoms Variola virus (DNA virus) Direct contact or by droplet from person to person 12 days high fever malaise headache back ache maculopapular rash in the face, mouth and pharynx (the patients are contagious after the appearance of the rash)
Management
generally supportive care before rendering care transmission precaution should be specifically indicated autoclaving of soiled linens is needed isolation is necessary until no longer contagious
ANTHRAX
Description:
Also known as whoolsorters disease, the capsulated form of this organism is found in soil worldwide. The organism needs to take about 8,000 to 50,000 to put a person at risk of contracting the disease. Bacillus anthracis inhalation of spores ingestion of spores entrance through skin lesions For inhalation anthrax 60 days, for cutaneous anthrax 1-6 days a.Inhalation anthrax cough headache fever vomiting chills weakness dyspnea syncope b.Cutaneous anthrax nausea and vomiting abdominal pain hematochexia ascites massive diarrhea
Etiology: Mode of transmission:
Incubation period: Signs and symptoms
Management
a.standard precaution is already sufficient to control the spread of the infection b.ciprofloxacin/doxycycline is prescribed for mass exposure/casualty with infecting organism important pharmacologic interventions are penicillin, erythromycin, chlorampenicol and gentamycin
SEVERE ACUTE RESPIRATORY SYNDROME (SARS) Latest among all the rest of pandemics which has its origin from China and has spread to USA, Canada, Philippines and other South East Asian Country Corona virus Etiology: Airborne Mode of transmission: 7 10 days Incubation period: Signs and symptoms fever cough rapid respiratory compromise dyspnea atelectasis supportive treatment provide ventilatory assistance use N95 mask to avoid infection
Description:
Management
Вам также может понравиться
- Neurogenic Lower Urinary Tract Dysfunction: Guidelines OnДокумент52 страницыNeurogenic Lower Urinary Tract Dysfunction: Guidelines OnPatrascu CristiОценок пока нет
- EpiДокумент3 страницыEpiNiño PaoloОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Speech Hiv AidsДокумент4 страницыSpeech Hiv AidsAtika Andayani SelianОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Foundations of EpidemiologyДокумент106 страницFoundations of EpidemiologySudaysi AbdisalamОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- DOCU - MedA Charting GuidelinesДокумент3 страницыDOCU - MedA Charting GuidelinesTee Wood50% (2)
- Presentation On WalnutДокумент5 страницPresentation On WalnutSheikh JeelaniОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- 200-Article Text-1119-1-10-20200603Документ6 страниц200-Article Text-1119-1-10-20200603miaОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Case Study BlepharitisДокумент12 страницCase Study BlepharitisNorshahidah IedaОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Dengue Prevention CampaignДокумент24 страницыDengue Prevention CampaignMuhammad Umer Abdullah100% (1)
- Afectarea Pulmonară Din Diverse Boli Reumatice: Dr. Corina MogosanДокумент25 страницAfectarea Pulmonară Din Diverse Boli Reumatice: Dr. Corina MogosanCioca ElizaОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hepatitis PreventionДокумент3 страницыHepatitis PreventionazisbustariОценок пока нет
- Epidemiology and Outcomes of Burn Injuries at A Tertiary Burn Care Center in BangladeshДокумент7 страницEpidemiology and Outcomes of Burn Injuries at A Tertiary Burn Care Center in BangladeshE.sundara BharathiОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- To The Learners: English 8Документ9 страницTo The Learners: English 8Mark Angelo SuarezОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- CNS infections: recent advances in diagnosis and managementДокумент36 страницCNS infections: recent advances in diagnosis and managementIkaDian PuspitanzaОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- RNA VirusesДокумент404 страницыRNA VirusesSisayОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Designated Medical Event Dme List enДокумент3 страницыDesignated Medical Event Dme List enAmany HagageОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Form Annex B MDH Intan Daya 3Документ3 страницыForm Annex B MDH Intan Daya 3fajar jatmikoОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- EpiglДокумент2 страницыEpiglfifiОценок пока нет
- Use of Convalescent Plasma in Hospitalized Patients With Covid-19 - Case SerieДокумент12 страницUse of Convalescent Plasma in Hospitalized Patients With Covid-19 - Case SeriesamuelОценок пока нет
- Mobile Phones and HealthДокумент255 страницMobile Phones and HealthID100% (1)
- Antibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHДокумент5 страницAntibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHzia ul RahmanОценок пока нет
- The Child With Respiratory DysfunctionДокумент91 страницаThe Child With Respiratory DysfunctionSerbanОценок пока нет
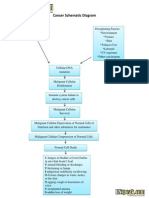
- Cancer Schematic DiagramДокумент1 страницаCancer Schematic DiagramCyrus De Asis100% (4)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- AS Level - Infectious Diseases (CH10) Summarised NotesДокумент31 страницаAS Level - Infectious Diseases (CH10) Summarised NotesRishika Pasupulati100% (1)
- Occupational Environment: and HealthДокумент32 страницыOccupational Environment: and Healthapi-19916399Оценок пока нет
- PE4Документ3 страницыPE4jovan teopizОценок пока нет
- Live Experiences of OFW Seafarers Covid Survivors This PandemicДокумент5 страницLive Experiences of OFW Seafarers Covid Survivors This PandemicParong, AallyjahОценок пока нет
- DN4 Assessment ToolДокумент1 страницаDN4 Assessment ToolrahmiОценок пока нет
- CDC 1st Quar. REPORT 2015Документ67 страницCDC 1st Quar. REPORT 2015abdi qanoОценок пока нет
- WP Contentuploads202208ExportFinalProgram 19082022113125 PDFДокумент423 страницыWP Contentuploads202208ExportFinalProgram 19082022113125 PDFMiguel AngelОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)