Академический Документы
Профессиональный Документы
Культура Документы
Microbio Lab 9,10,11,12 & Review
Загружено:
api-3743217Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Microbio Lab 9,10,11,12 & Review
Загружено:
api-3743217Авторское право:
Доступные форматы
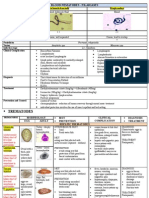
MICROBIOLOGY LABORATORY 9,10,11,12 (review) making the slide safe to handle.
Care must be taken not to
USTMED ’07 Sec C AsM; Photos provided by JV.N & MeaM. overheat which will char the cells.
4. Once cool, the slide is transferred to a
DEMONSTRATIONS: MICROSCOPIC MORPHOLOGY OF DIFFERENT MICROORGANIMSMS support over a sink and flooded with a stain
called Gentian Violet (a dye consisting of a
Sputum smear stained with methyl derivative of pararosaniline). The
Gram’s stain shows neutrophils, stain is left on the slide for about 1 minute.
amorphous debris, and This stains all the bacteria on the slide a
filamentous, beaded, branched dark purple colour. Note, this stain will not
gram-positive bacilli (oil penetrate the waxy cell walls of some
immersion). bacteria eg mycobacteria.
5. The Gentian Violet is gently washed off the slide with running
water
6. The bacterial smear is then treated with Gram’s solution
which consists of 1 part iodine, 2 parts potassium iodide, and
300 parts water. This iodine solution reacts with the Gentian
Violet turning it a very dark shade of blue. It also causes it
to be retained by certain types of bacteria in a way which is
not really understood.
7. After about 30 seconds the slide is gently rinsed with ethyl
Gram stain of Bacillus cereus. The arrow is pointed at a spore, alcohol which causes the dye-iodine complex to be washed
which is clear inside the gram-positive vegetative cell. out of some bacteria but not others. This is called
decolourisation.
If we now look at the smear down a microscope, the
bacteria which had retained the Gentian Violet-iodine
complex will appear blue-black. These are called Gram-
positive. However wi would not be able to see those which
had lost the dye-iodine complex which are called Gram-
negative. The final step in the gram stain method is,
therefore, to stain the Gram-negative cells so they can be
seen.
8. This is achieved by treating the smear with a compound
Escherichia coli. which stains the Gram-negative cells a colour which contrasts
Stain used: Gram stain markedly with the blue-black colour of the gram-posiitve
Gram rxn: Gram negative (red) cells. The stain common used for this is either eosin or
Morphology: Coccobacilli arranged singly or random fuchsin, both of which are red. These are called
Note: E. coli is a Gram Negative Bacilli but it appears as a short counterstains. Bacteria in the smear which are Gram-
plump bacilli so it is called coccobacilli. positive are unaffected by the counterstain.
9. The counterstain is left on the smear for about 30-60 seconds
Bacillus subtilis. and then gently rinsed away with running water.
Stain used: Gram Stain 10. After the counterstain has been rinsed off, the slide is placed
Gram rxn: Gram Positive between some absorbent paper and the excess water gently
Morphology: Bacilli in chain blotted off. Care must be taken not to rub the slide with the
(violet rods in chain). Aerobic blotting paper because this would remove the adhering
sporeformer bacilli. bacteria.
Note: spores elliptical and 11. The slide is gently warmed to dry off any residual moisture
centrally located and then a drop of oil immersion oil is placed on the stained
• spores – unstained bacterial smear. This helps transmit light through the
• vegetative portion – violet specimen directly to the high-powered microscope lens.
12. The slide is the placed on a microscope stage and the oil-
Pseudomonas aeruginosa immersion lens lowered into the immersion oil. High-
Stain used: Gram Stain powered lenses are required because bacteria are very small
Gram rxn: Gram Negative bacilli in (hindi nga???!!!)
singly/random (red slender rods in
singly or random) The results
Gram positive Gram negative
Staphylococcus aureus Escherichia coli
The Gram staining method Typical Gram-positive cocci in Typical Gram-negative
clusters coccobacilli, singly
Gram’s Stain is a widely used method of staining bacteria as
an aid to their identification. It was originally devised by Hans
Christian Joachim Gram, a Danish doctor.
Gram’s stain differentiates between two major cell wall
types. Bacterial species with walls containing small amounts of
peptidoglycan and, characteristically, lipopolysaccharide, are
Gram-negative whereas bacteria w/ walls containing reltively
large amounts of peptidoglycan and no lipopolysaccharide are Capsule stain.
Gram-positive. The cell is the purple rod in the center of
the clear area. The purple color is from the
- It’s a mystery - basic stain, crystal violet.
Although it may seem strange, the reason why bacteria with
these two major types of bacteria cell walls react differently with The clear area is the capsule, and the
Gram’s stain appears to be unconnected with the wall structure background is colored by the negative,
itself. The exact method of the staining reaction is not fully acidic stain (India ink).
understood, however, this does not detract from its usefulness.
1. A small sample of a bacterial culture is removed from a
culture. In this example it is being taken from a broth culture
of the pure microbe but it could be removed from a culture
on solid medium or from material containing bacteria eg
faeces or soil.
2. The bacterial suspension is smeared onto a clean glass slide.
If the bacteria have been removed from a culture on solid
media or it is from a soil or faeces sample it will have to be
mixed with a drop of bacteria-free saline solution.
3. The bacterial smear is then dried slowly at first and the, Loefflers methylene blue stain.
when dry, heated for a few seconds to the point when the Corynebacterium diptheriae demonstrate metachromatic granules
glass slide is too hot to handle. This fixes ie kills the bacteria when stained with Loeffler methylene blue stain or Neisser stain.
The stain is best performed on colonies grown on a Loeffler agar must be kept in mind then interpreting the zone of inhibition of
slant. Metachromatic deposits are reddish purple in Loeffler various antibiotics.
methylene blue stain.
MATERIALS:
Flagella stain. - culture of the organisms in Mueller-Hinton agar plate
with antibiotic sensitivity discs
Proteus sp. Peritrichous flagella – - Ruler graduated in millimeters
flagella distributed over the entire
surface. NOTE:
- The complete procedure is in you(r) lab manual.
1. Measure the zone of inhibition and record your results.
2. Interpret the results based on the table provided
Vibrio cholera Monotrichous flagella – one polar flagellum. 3. Indicate if the antibiotics discs used is Sensitive,
Intermediate or Resistant.
Spore stain Disk Diffusion Method
Bacillus cereus. The arrows are
pointed at green spores in a pink Procedure
vegetative cell. 1. dip the sterile swab into bacterial suspension compared
to 0.5 MF standard then swab onto the surface of
Mueller Hinton Agar using Overlapping technique.
2. Allow the organism to be absorbed by the medium.
Culture of Microorganisms Place the appropriate antimicrobial (sensitivity) discs
using the dispenser or a sterile forceps. Incubate for 24
Different Streaking Methods hours at 37o
3. Reading and Interpretation of the results. Measure the
Culture Media Used: Eosin Methylene Blue diameter of the Zone of Inhibition (area wherein there is
Organisms Used: Escherichia Coli no growth around the discs) using the millimeter of a
Method of Streaking: Simple Streaking ruler. Record your results and Interpret based on the
table provided. Determine if the Antibiotic (organism) is
Illustration: Sensitive, Intermediate or Resistant. If there is
overlapping in the zone of inhibition, you can just
measure the radius and multiply the reading by 2 to get
the diameter.
Culture Media Used: Eosin Methylene Blue
Organisms Used: Escherichia Coli
Method of Streaking: 4 Quadrant Method of Streaking
Pseudomonas aeruginosa, a resistant strain.
Note: This method of streaking is used for better isolation of the
Growth on this Mueller-Hinton agar plate
organism
indicates that the isolate is resistant to six of
12 antimicrobial agents and susceptible to
Illustration:
the remaing. The isolate is resistant to SXT,
GM, ATM, TIM, TIC and MMZ. The isolate is
susceptible to CIP, AN, NN, CA, IPM and PIP.
E. coli ATCC 25922. The isolate tested on
this Mueller-Hinton agar plate is interpreted
as susceptible (S) to all antimicrobial agents.
Reading clockwise from the top, MZ, AN, AM,
Culture Media Used: Eosin Methylene Blue
CZ, CTX, CXM, CF, GM, NN: the three discs in
Organisms Used: Escherichia Coli
the center of the plate are SXT, FOX and TIM.
Method of Streaking: Overlapping method of streaking
Єtest – The Problem Solver in Antimicrobial
Note: This method of streaking is used for sensitivity testing
Susceptibility Testing
Illustration:
Etest is an antimicrobial
gradient strip for the
quantitative determination of
susceptibility or resistance of
microorganisms. It is a robust
and simple technique,
minimally affected by
laboratory variations and can
be used to test most
microorganisms. An accurate
Antibiotic Sensitivity Testing Using The Kirby-Bauer Procedure
and reproducible Minimum
Inhibitory Concentration (MIC)
Kirby Bauer method. The test, introduced by William Kirby and
is generated for reliable
Alfred Bauer in 1966, consists of exposing a newly-seeded lawn of
guidance of antimicrobial
the bacterium to be tested, growing on a nutrient medium
therapy.
(Mueller-Hinton agar) to filter paper disks impregnated with
various antibiotics. The culture is incubated for 16 to 18 hours
Єtest Susceptibility Testing
and then examined for growth. If the organism is inhibited by one
of the antibiotics, there will be a zone of inhibition around the
Procedure
disk, representing the area in which the organism was inhibited by
that antibiotic. 1. inoculation of the
organism for testing
The diameter of the zone of inhibition around an antibiotic disk is using cotton swab by
an indication of the sensitivity of the tested microorganism to that overlapping streaking
antibiotic. The diameter of the zone, however, is also related to using Mueller Hinton
the rate of diffusion of the antibiotic in the medium. This fact Agar Plate.
2. Overlaying of Єtest 25. Clostridia on egg yolk agar
strip on the previously 26. Clostridium tetati on Brucella blood agar
inoculated culture 27. Clostridium perfringens on brucella
media 28. Gelatin hydrolysis test
29. Growth of bacillus spp on egg yolk agar
3. Reading of the strip and recording the results 30. colonies of bacillus spp on 5% sheep blood agar
31. sputum stained w/ gram’s stain shown w/ many
neutrophils
32. colonies of c. diphtheriae on tinsdale agar
33. colonies of c. diptheriae on 5% sheep blood agar
34. Erysipelothrix on TSI agar
35. colonies of erysipelothrix rhusiopathiae
36. Esculin hydrolysis test
37. colonies of listeria monocytogenes on 5% sheep blood
agar
38. colonies of bacteroides fragilis on bile esculin
A/N: … looks familiar right?! the next pictures are just recaps
of our previous laboratory exercises. I’ll just list down the stuff
39. colonies of bacteroides on brucella
40. Gomori methenamine silver stain of actinomyces spp
that was brought out again for the review..
41. Molar tooth appearance of actinomyces
42. Amino acid hydrolysis rxn of nocardia asteroids
Review…
43. colonies of nocardia asteroids growing on bay plate
1. Optochin sensitivity of pneumococci… 44. modified kinyoun acid fast. Nocardia
45. amino acid hydrolysis rxn of streptomyces
46. gram stain of streptomyces
47. gram stain of nocardia
2. Growth of pneumococci on blood agar 48. identification of the genus nocardia w/ biochemical rxns
showing draughtsman colonies…
ustmedc3@yahoogroups.com
audrey_cl@yahoo.com
3. Catalase test]
4. Slide and tube coagulase tests
5. Mannitol Salt Agar (MSA)..S. aureus
6. Staph aureus on Blood Agar plate (BAP)
7. gram stain of staph aureus
8. Neisseria gonorrhea. Urethral
discharge..
9. Myco TB on LJ media
10. Scotochromogen M. gordonae
11. M. Tb fluorochrome stain
12. M Tb kinyoun
13. Kinyoun acid fast stain
14. MTB kinyoun
15. KInyoun’s acid fast stain
16. Photochromogen M. kansasii
17. MTb on LJ 8 weeks
18. MTb on Middlebrook
19. Mtb on middlebrook cording
20. Gram stain of clostridium
21. Gram stain of clostridium paraputrificum. Terminal
swollen spores
22. Gram stain of Bacillus spp.
23. Clostridium difficile, lecithinase
24. Gram’s stain of a smear of exudates, gas bubbles
Вам также может понравиться
- StreptococcusДокумент6 страницStreptococcusAyessa VillacorteОценок пока нет
- Immuno Sero CompleteДокумент33 страницыImmuno Sero CompleteAngela ReyesОценок пока нет
- Staphylococcus Spp. Gram Positive. ClusteredДокумент15 страницStaphylococcus Spp. Gram Positive. ClusteredIvy NОценок пока нет
- Molecular Biology and Diagnostic Intro To CytogeneticsДокумент6 страницMolecular Biology and Diagnostic Intro To Cytogeneticselijah montefalcoОценок пока нет
- Campylobacter & Plesiomonas - Bacter ReportДокумент55 страницCampylobacter & Plesiomonas - Bacter ReportRona SalandoОценок пока нет
- Family of StreptococcaceaeДокумент10 страницFamily of StreptococcaceaeLovely B. AlipatОценок пока нет
- Mycobacteria: Nocardia, Rhodococcus, Tsukamurella and GordoniaДокумент7 страницMycobacteria: Nocardia, Rhodococcus, Tsukamurella and Gordonia20C – Gorospe, Rhai Chezka V.Оценок пока нет
- DermatophytesДокумент1 страницаDermatophytesKoo ThaОценок пока нет
- MycoViro 2Документ44 страницыMycoViro 2Ria AlcantaraОценок пока нет
- Microbio Lec 1 - Bacterial Morphology and Ultra StructureДокумент8 страницMicrobio Lec 1 - Bacterial Morphology and Ultra Structureapi-3743217100% (3)
- Gram Negative Cocci (Lecture Notes)Документ5 страницGram Negative Cocci (Lecture Notes)Dayledaniel Sorveto100% (1)
- Serological TestsДокумент2 страницыSerological TestsKimberly EspaldonОценок пока нет
- Gram Positive Cocci Sem 1 1Документ45 страницGram Positive Cocci Sem 1 1Charmaine Corpuz Granil100% (1)
- (Bacteriology) Chapter 8: Use of Colonial Morphology For The Presumptive Identification of MicroorganismsДокумент6 страниц(Bacteriology) Chapter 8: Use of Colonial Morphology For The Presumptive Identification of MicroorganismsJean BelciñaОценок пока нет
- Mycology Shereena V. Opiniano, RMT, MSMT. Terms: Saprobes Symbionts Asexual Types: A. SporangiosporesДокумент7 страницMycology Shereena V. Opiniano, RMT, MSMT. Terms: Saprobes Symbionts Asexual Types: A. SporangiosporesStephie Mae100% (1)
- Gram Positive: CoccusДокумент8 страницGram Positive: CoccusLM MysОценок пока нет
- A. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusДокумент8 страницA. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusRuel MaddawinОценок пока нет
- MYCO-VIRO LEC Practical Exam ReviewerДокумент5 страницMYCO-VIRO LEC Practical Exam ReviewerJoseph SabidoОценок пока нет
- Practical 4 Staphylococci PresentationДокумент24 страницыPractical 4 Staphylococci PresentationPatrisha BuanОценок пока нет
- 4th Shifting Micro Lab ReviewerДокумент154 страницы4th Shifting Micro Lab ReviewerJade MonrealОценок пока нет
- 2 PARA 1 - Protozoa - FlagellatesДокумент13 страниц2 PARA 1 - Protozoa - FlagellatesTricia LlorinОценок пока нет
- Hacek GroupДокумент24 страницыHacek GroupHanna Isabela Bausin0% (1)
- Intro To Mycology Prelims2Документ47 страницIntro To Mycology Prelims2Annika AbadОценок пока нет
- IS LessonДокумент30 страницIS Lessonjohn dale duranoОценок пока нет
- Gram +ve BacteriaДокумент58 страницGram +ve BacteriaGx NavinОценок пока нет
- Gram Staining Clinical ExerciseДокумент10 страницGram Staining Clinical ExerciseHimani Aggarwal100% (1)
- Introduction To MycologyДокумент26 страницIntroduction To MycologyOsannah Irish InsongОценок пока нет
- Morphologic Differences Cestodes (Tapeworms) Trematodes (Flukes) Nematodes (Roundworms)Документ15 страницMorphologic Differences Cestodes (Tapeworms) Trematodes (Flukes) Nematodes (Roundworms)Noelle Grace Ulep BaromanОценок пока нет
- RMTnotes PARASITOLOGYДокумент68 страницRMTnotes PARASITOLOGYArvin O-CaféОценок пока нет
- Me EnterobacteriaceaeДокумент72 страницыMe Enterobacteriaceaewimarshana gamage100% (1)
- C. Bacteriology L6 Antimicrobial Susceptibility Testing LectureДокумент5 страницC. Bacteriology L6 Antimicrobial Susceptibility Testing LectureChelze Faith DizonОценок пока нет
- Stains NotesДокумент3 страницыStains NotesMdrrmo MaconaconОценок пока нет
- Corynebacterium and Other Non-spore-Forming Gram-Positive RodsДокумент3 страницыCorynebacterium and Other Non-spore-Forming Gram-Positive RodsYelai CarveroОценок пока нет
- Amoeba and CestodesДокумент5 страницAmoeba and Cestodes2013SecB100% (1)
- SELF STUDY Specimen Collection and TransportДокумент3 страницыSELF STUDY Specimen Collection and TransportAngelic AngelesОценок пока нет
- The Medically Important MycosesДокумент8 страницThe Medically Important MycosesNatasha JeanОценок пока нет
- Trematodes: Blood FlukesДокумент3 страницыTrematodes: Blood FlukesFrance Louie JutizОценок пока нет
- Micro para OSCE For YL6 BacteriaДокумент2 страницыMicro para OSCE For YL6 Bacteriagzldiwa100% (1)
- MV Lec PDFДокумент102 страницыMV Lec PDFJonas Datu100% (1)
- Sir Alvin Rey Flores: Echinococcus Granulosus, Taenia Solium)Документ5 страницSir Alvin Rey Flores: Echinococcus Granulosus, Taenia Solium)Corin LimОценок пока нет
- Rickettsia eДокумент10 страницRickettsia eDeep Iyaz100% (1)
- Para Lab 4Документ3 страницыPara Lab 4api-3743217Оценок пока нет
- Bacterial Genetics: Calvin Bisong EbaiДокумент58 страницBacterial Genetics: Calvin Bisong EbaiMBAH LOIS LA GRACEОценок пока нет
- 1 Antigens and AntibodiesДокумент31 страница1 Antigens and AntibodiesJohn Louis RanetОценок пока нет
- Medical MycologyДокумент1 страницаMedical MycologyHairul AnuarОценок пока нет
- s4 l3 Nematodes IIДокумент14 страницs4 l3 Nematodes II2013SecB100% (1)
- Flow Chart of Gram Negative OrganismsДокумент1 страницаFlow Chart of Gram Negative OrganismsKristine Marie PateñoОценок пока нет
- Mycology: Rochelle D. Darlucio-Yabut, RMT, MPH Our Lady of Fatima University College of Medical Laboratory ScienceДокумент59 страницMycology: Rochelle D. Darlucio-Yabut, RMT, MPH Our Lady of Fatima University College of Medical Laboratory ScienceClaire GonoОценок пока нет
- Nematodes, Plasmodium and Trematodes LabДокумент2 страницыNematodes, Plasmodium and Trematodes Lab2013SecBОценок пока нет
- ENTEROBACTERIACEAEДокумент13 страницENTEROBACTERIACEAEStephen Jao Ayala Ujano100% (1)
- Mycology 1 PrelimДокумент4 страницыMycology 1 PrelimKaye Angel VillonОценок пока нет
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterДокумент4 страницыLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoОценок пока нет
- Review Parasitology Exam (Permanent Stain Images)Документ12 страницReview Parasitology Exam (Permanent Stain Images)Tony DawaОценок пока нет
- Gram Negative BacilliДокумент15 страницGram Negative BacilliFabasyira JamalОценок пока нет
- Helminth 3Документ2 страницыHelminth 3Farlogy100% (6)
- 3 SEMR421 Bacteriology Part 3Документ14 страниц3 SEMR421 Bacteriology Part 3Micah Daniel TapiaОценок пока нет
- CHALLENGE QUESTIONS (Write Your Answer/s Here For Practice)Документ2 страницыCHALLENGE QUESTIONS (Write Your Answer/s Here For Practice)Roma Ann ManahanОценок пока нет
- Bacterial Stains and Smear Preparation: Lab 12 Prof - Dr.lazem AltaieДокумент8 страницBacterial Stains and Smear Preparation: Lab 12 Prof - Dr.lazem Altaieليث علي احمد حريفشОценок пока нет
- EXERCISE 4 Stains PDFДокумент3 страницыEXERCISE 4 Stains PDFOsannah Irish InsongОценок пока нет
- Clin Path Lab 6 Urinalysis Part 2Документ7 страницClin Path Lab 6 Urinalysis Part 2api-3743217100% (3)
- Microbio Lec 10 - Enterobacteriaceae Gen, Shigella and SalmoДокумент8 страницMicrobio Lec 10 - Enterobacteriaceae Gen, Shigella and Salmoapi-3743217100% (7)
- Clin Path Lab 6 UrinalysisДокумент5 страницClin Path Lab 6 Urinalysisapi-3743217100% (6)
- Microbio Lec 11 - Ecoli, Klebsiella Proteus, Citrobacter AnДокумент3 страницыMicrobio Lec 11 - Ecoli, Klebsiella Proteus, Citrobacter Anapi-374321750% (2)
- Microbio Lec 8 - MycobacteriaДокумент6 страницMicrobio Lec 8 - Mycobacteriaapi-374321750% (2)
- Microbio Lab 7 (Leigh)Документ8 страницMicrobio Lab 7 (Leigh)api-3743217100% (6)
- Microbio Lab 8Документ4 страницыMicrobio Lab 8api-3743217100% (5)
- Para Lab 8Документ2 страницыPara Lab 8api-3743217100% (2)
- Microbio Lab 6Документ4 страницыMicrobio Lab 6api-374321750% (2)
- Microbio Lec 5 - StaphylococcusДокумент6 страницMicrobio Lec 5 - Staphylococcusapi-3743217100% (2)
- Microbio Lec 5 - StreptococcusДокумент6 страницMicrobio Lec 5 - Streptococcusapi-3743217100% (4)
- Microbio Lec 1 - Bacterial Morphology and Ultra StructureДокумент8 страницMicrobio Lec 1 - Bacterial Morphology and Ultra Structureapi-3743217100% (3)
- Para Lab 11Документ3 страницыPara Lab 11api-3743217Оценок пока нет
- Para Lab 4Документ3 страницыPara Lab 4api-3743217Оценок пока нет
- Parasitology-Lec 13 MalariaДокумент6 страницParasitology-Lec 13 Malariaapi-3743217Оценок пока нет
- Parasitology-Lec 12 TrypanosomesДокумент6 страницParasitology-Lec 12 Trypanosomesapi-3743217Оценок пока нет
- Parasitology-Lec 10 EntamoebaДокумент7 страницParasitology-Lec 10 Entamoebaapi-3743217100% (2)
- Parasitology-Lec 9 CestodesДокумент5 страницParasitology-Lec 9 Cestodesapi-3743217100% (4)
- National Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaДокумент53 страницыNational Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaNational Dengue Control Unit,Sri Lanka100% (1)
- Massive Transfusion ProtocolДокумент2 страницыMassive Transfusion ProtocolmukriОценок пока нет
- Design Manual IndexДокумент4 страницыDesign Manual Indexellee6222100% (1)
- CystosДокумент1 страницаCystosgeorgeloto12Оценок пока нет
- Johns Hopkins Dean - Reflections On Medical School AdmissionsДокумент4 страницыJohns Hopkins Dean - Reflections On Medical School AdmissionstheintrepiddodgerОценок пока нет
- Systemic Inflammatory Response SyndromeДокумент3 страницыSystemic Inflammatory Response SyndromesujithasОценок пока нет
- Degnala DiseaseДокумент12 страницDegnala DiseaseSantosh Bhandari100% (1)
- Ra Lightning Protection SystemДокумент16 страницRa Lightning Protection SystemamalОценок пока нет
- Introduction To SpineДокумент29 страницIntroduction To Spinebmahmood1Оценок пока нет
- RXN For DR - SagamlaДокумент2 страницыRXN For DR - Sagamlayeng botzОценок пока нет
- Kosmetik BatalДокумент5 страницKosmetik BatalNurul AtikОценок пока нет
- Pharmacovigilance ReportДокумент21 страницаPharmacovigilance ReportPeter RutterОценок пока нет
- Sales Account Manager Biotechnology in Boston MA Resume Cynthia SmithДокумент2 страницыSales Account Manager Biotechnology in Boston MA Resume Cynthia SmithCynthiaSmith2Оценок пока нет
- Concept Map 3 MM (Abdominal Pain)Документ2 страницыConcept Map 3 MM (Abdominal Pain)Matt McKinleyОценок пока нет
- Icare Pivc GuidelineДокумент26 страницIcare Pivc GuidelineCarissa CkОценок пока нет
- Organon of Medicine All Years 2marks Question Viva Questions AnswersДокумент12 страницOrganon of Medicine All Years 2marks Question Viva Questions Answersabcxyz15021999Оценок пока нет
- Simultaneous Determination of Methylparaben + Propylparaben + Hidrocortisone Topical Cream PDFДокумент7 страницSimultaneous Determination of Methylparaben + Propylparaben + Hidrocortisone Topical Cream PDFNájla KassabОценок пока нет
- Grafic AsistentiДокумент64 страницыGrafic AsistentibadeaОценок пока нет
- Smear Layer Final2Документ10 страницSmear Layer Final2bhudentОценок пока нет
- Intrathecal Morphine Single DoseДокумент25 страницIntrathecal Morphine Single DoseVerghese GeorgeОценок пока нет
- GHA-Hospital List As of March 2019Документ1 страницаGHA-Hospital List As of March 2019JULIUS TIBERIOОценок пока нет
- Ch. 24 Older Adults Ageing in PlaceДокумент54 страницыCh. 24 Older Adults Ageing in PlacebaasheОценок пока нет
- Retirement HomesДокумент139 страницRetirement HomesAnu Alreja100% (2)
- Gay Issue A Century AgoДокумент4 страницыGay Issue A Century AgoElla Jane EngoОценок пока нет
- Photocatalysis PDFДокумент8 страницPhotocatalysis PDFLiliana GhiorghitaОценок пока нет
- Anatomy and Physiology Respiratory SystemДокумент7 страницAnatomy and Physiology Respiratory Systemnoronisa talusobОценок пока нет
- WarfarinДокумент2 страницыWarfarinWAHYU NOFANDARI HERDIYANTIОценок пока нет
- Dental ChartingДокумент51 страницаDental ChartingXuan5550% (1)
- Montana Polst FormДокумент2 страницыMontana Polst FormitargetingОценок пока нет
- Teratogenic ItyДокумент8 страницTeratogenic ItyValentin IanaОценок пока нет
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 4.5 из 5 звезд4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4.5 из 5 звезд4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceОт EverandTo Explain the World: The Discovery of Modern ScienceРейтинг: 3.5 из 5 звезд3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsОт EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsРейтинг: 4.5 из 5 звезд4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingОт EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingРейтинг: 4 из 5 звезд4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)