Академический Документы
Профессиональный Документы
Культура Документы
Letter To The Editor Hydrotherapy in Heart Failure: A Case: Background
Загружено:
Elizabete MonteiroИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Letter To The Editor Hydrotherapy in Heart Failure: A Case: Background
Загружено:
Elizabete MonteiroАвторское право:
Доступные форматы
CLINICS 2009;64(8):824-7
LETTER TO THE EDITOR HYDROTHERAPY IN HEART FAILURE: A CASE REPORT
doi: 10.1590/S1807-59322009000800020
Vitor Oliveira Carvalho,I,II Edimar Alcides Bocchi,I,II Guilherme Veiga GuimaresI,II
BACKGROUND Heart failure is considered to be the last stage of heart disease and a significant cause of morbidity and mortality worldwide.1,2,3 It is characterized by the persistent activation of the neurohormonal system,4 endothelial dysfunction,5 exercise intolerance,6,7,8,9 high mortality10 and a poor quality of life.11 Exercise training has been strongly recommended as a safe and important tool for the non-pharmacological treatment of heart failure. Exercise training improves exercise capacity, 12,13 quality of life, 14 endothelial dysfunction,15 skeletal muscle oxidative capacity, 16 the cathecolamine plasma level 17 and the autonomic and ventilatory responses.18 In heart failure patients, designing an appropriate aerobic exercise routine is crucial for obtaining both an increase in exercise capacity and the reasonable control of exercise-related risks.1,6 Hydrotherapy (i.e., exercise in warm water) had been considered potentially dangerous in heart failure patients due to the increased venous return caused by the hydrostatic pressure. However, it is now known that cardiac function actually improves during water immersion due to the increase in early diastolic filling and decrease in heart rate, resulting in improvements in stroke volume and ejection fraction.19 Studies with sauna therapy (i.e., warming) have demonstrated important improvements in neurohormonal attenuation and exercise status in heart failure patients. These data suggest that hydrotherapy is a good potential treatment for heart failure patients. However, few studies are available,
Unidade Clnica de Insuficincia Cardaca e Transplante do Instituto do Corao do Hospital das Clnicas da Faculdade de Medicina da USP (InCor HC-FMUSP) - So Paulo/SP, Brazil. II Laboratrio de Atividade Fsica e Sade do Centro de Prticas Esportivas da Universidade de So Paulo (LATIS-CEPEUSP) - So Paulo/SP, Brazil. Email: vitor.carvalho@usp.br
I
and none have compared conventional rehabilitation to hydrotherapy.20 This study was partially supported by Coordenao de Aperfeioamento de Pessoal de Nvel Superior. CASE REPORT A 51-year-old male heart failure patient (ischemic etiology with 40% left ventricular ejection fraction) was recruited from a cardiology hospital to this rehabilitation program (Table 1). This patient underwent 24 exercise sessions in a 2224C temperature-controlled gym (conventional exercises) between May and July 2007. After the exercise training program, this patient was invited to continue in our rehabilitation program but opted out. After 6 months, the patient returned to our program to continue the exercise program, and we assigned him to hydrotherapy. Between January and March 2008, he had 24 more exercise sessions in a 3031C temperaturecontrolled swimming pool (hydrotherapy). The exercise training protocol was almost the same for both methods: 5 minutes of warm up exercises (stretching), 30 minutes of aerobic exercise training (90% of ventilatory threshold), 25 minutes of strength exercises (lower and upper limbs) and 5 minutes of cool down exercises (stretching). A treadmill (Max 1; Marquette Electronics; Milwaukee, WI, USA) cardiopulmonary exercise test (Vmax 229 model, SensorMedics, Yorba Linda, CA, USA), 24-hour ambulatory blood pressure measurement (Space Labs Redmond, Wash, USA), New York Heart Association functional classification and a Minnesota Living With Heart Failure Questionnaire were performed before and after the exercise training protocols (the cardiopulmonary exercise test was performed 2 days prior to the other evaluations). The medications were not changed during the protocols (150 mg/day Carvedilol, 100 mg/day Losartan, 40 mg/day Furosemide, 25 mg/day
824
CLINICS 2009;64(8):824-7
Cardiovascular rehabilitation Carvalho VO et al.
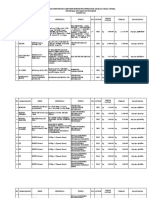
Table 1 - Patient data before and after exercise training
Conventional (pre-training) BMI (kg/m2) Waist (cm) Hip (cm) Peak VO2 (mLO2.kg .min )
-1 -1
Conventional (post-training) 37.1 119 110 28.7 13.3 21.7 27.5 1.04 19 1 49 117 67 76 117 67 78 118 68 72
Hydrotherapy (pre-training) 38.8 123 121 16.5 9.0 16.1 33.3 1.04 14 3 68 130 70 91 137 74 94 116 62 85
Hydrotherapy (post-training) 37.5 121 117 26.9 12.5 20.5 24.5 1.07 16 1 26 125 66 69 127 69 67 122 61 73
36.7 120 110 21.5 12.8 17.3 28.7 1.05 17 2 51 118 63 69 124 67 69 108 55 69
VO2 AT (mLO2.kg-1.min-1) VO2 VT (mLO2.kg .min )
-1 -1
VE/VCO2 slope RER Time (exercise test) NYHA MLHFQ SBP 24 hours (mmHg) DBP 24 hours (mmHg) HR 24 hours (bpm) SBP daytime (mmHg) DBP daytime (mmHg) HR daytime (bpm) SBP nighttime (mmHg) DBP nighttime (mmHg) HR nighttime (bpm)
VO2, Oxygen consumption; RER, Respiratory exchange ratio; NYHA, New York Heart Association Functional Class; MLHFQ, Minnesota Living with Heart Failure Questionnaire; SBP, Systolic blood pressure; DBP, Diastolic blood pressure; HR, heart rate.
Spironolactone and 0.25 mg/day Digoxin). This protocol was approved by the ethical committee of our institution (number 1107/05). DISCUSSION Exercise training is a well-established non-pharmacological treatment for patients with heart failure. Hydrotherapy is a new and well-tolerated method of exercise rehabilitation for heart failure patients. It is an alternative for elderly patients and patients with impaired mobility.21 The patient in this case study did not have any orthopedic problems despite his high body mass index. Studies with sauna baths have shown that they can lead to great improvements in heart failure by attenuating the neurohormonal system.21,22 It is possible that hydrotherapy (i.e., exercise in a warm swimming pool) could provide the same beneficial effects of conventional exercise training and warming while also attenuating the neurohormonal system more significantly. Therefore, we expected the patient to improve more with hydrotherapy than with conventional exercise.
In this case, hydrotherapy was an effective method of cardiovascular rehabilitation and a safe alternative to conventional exercise. This is the first report in which a patient has performed both forms of exercise. The patients peak and anaerobic threshold oxygen consumption, VE/ VCO2 slope, Minnesota living with heart failure quality of life score, body mass index, 24-hour ambulatory blood pressure and waist and hip circumference improved with both methods of exercise rehabilitation, but the improvements were more pronounced with hydrotherapy. The patients peak and anaerobic threshold oxygen consumption showed an increase of 7.2 mLO2.kg-1.min-1 during regular exercise training versus 10.4 mLO2.kg-1. min-1 with hydrotherapy and an increase of 0.5 mLO2.kg-1. min-1 with regular training versus 3.5 mLO2.kg-1.min-1 with hydrotherapy, respectively. His VE/VCO2 slope decreased by 1.2 with regular training, while it decreased to 8.8 with hydrotherapy. The Minnesota living with heart failure quality of life score decreased by 2 with regular training and by 42 with hydrotherapy. The patients body mass index increased by 0.4 kg/m2 with regular training, while it decreased by 1.3 kg/m2 with hydrotherapy. His mean 24-hour systolic blood
825
Cardiovascular rehabilitation Carvalho VO et al.
CLINICS 2009;64(8):824-7
pressure showed a 1 cm H2O decrease with regular training, while it decreased by 5 cm H2O with hydrotherapy. On the other hand, his mean diastolic blood pressure was unchanged by regular training while it decreased by 5 cm H2O with hydrotherapy. The patients waist circumference showed a decrease of 1 cm with regular training and a decrease of 2 cm with hydrotherapy, while his hip circumference was unchanged by regular training but showed a 4 cm decrease with hydrotherapy. Exercise intolerance (low peak oxygen consumption) and poor quality of life have been negatively correlated to neurohormonal activity in heart failure patients.23 Some
clinical exams, such as the 24-hour ambulatory blood pressure, can detect the exacerbated neurohormonal activity seen in heart failure.24 These clinical data reflect the stronger neurohormonal attenuation provided by hydrotherapy. Importantly, signs and symptoms of exercise intolerance were not observed during either exercise regimen. CONCLUSION In this case report, we demonstrate that hydrotherapy is an effective method of cardiovascular rehabilitation and can be a safe alternative to conventional exercise.
REFERENCES
1. Working Group on Cardiac Rehabilitation & Excercise Physiology and Working Group on Heart Failure of the European Society of Cardiology. Eur Heart J. 2001;22:37-45. Bocchi EA, Carvalho VO, Guimaraes GV. Inverse correlation between testosterone and ventricle ejection fraction, hemodynamics and exercise capacity in heart failure patients with erectile dysfunction. Int Braz J Urol. 2008;34:302-10. Guimaraes GV, DAvila MV, Silva MS, Ciolac EG, Carvalho VO, Bocchi EA. A cutoff point for peak oxygen consumption in the prognosis of heart failure patients withbeta-blocker therapy, Int J Cardiol 2009, doi:10.1016/j.ijcard.2009.05.001 Chizzola PR, Gonalves de Freitas HF, Marinho NV, Mansur JA, Meneghetti JC, Bocchi EA. The effect of beta-adrenergic receptor antagonism in cardiac sympathetic neuronal remodeling in patients with heart failure. Int J Cardiol. 2006;106:29-34. Maruo T, Nakatani S, Kanzaki H, Kakuchi H, Yamagishi M, Kitakaze M, et al. Circadian variation of endothelial function in idiopathic dilated cardiomyopathy. Am J Cardiol 2006; 97:699-702. Ades PA, Savage PD, Brawner CA, Lyon CE, Ehrman JK, Bunn JY, et al. Aerobic capacity in patients entering cardiac rehabilitation. Circulation. 2006;133:2706-12. Carvalho VO, Guimares GV, Bocchi EA. The relationship between heart rate reserve and oxygen uptake reserve in heart failure patients on optimized and non-optmized beta-blocker therapy. Clinics.2008;63:725-30. Carvalho VO, Guimares GV, Ciolac EG, Bocchi EA. Heart rate dynamics during a treadmill cardiopulmonary exercise test in optimized beta-blocked heart failure patients. Clinics. 2008 ;63:479-82. Carvalho VO, Alves RXR, Bochi EA, Guimares GV. Heart rate dynamic during an exercise test in heart failure patients with different sensibilities of the carvedilol therapy. Int J Cardiol 2009: doi:10.1016/j. ijcard.2008.11.140. 10. Bocchi EA, Cruz F, Guimares G, Moreira LFP, Issa VS, Ferreira SMA, et al. Long-term prospective, randomized, controlled study using repetitive education at six-month intervals and monitoring for adherence in heart failure outpatients. The REMADHE study. Circ Heart Fail. 2008;1:115-24. 11. Carvalho VO, Guimares GV, Carrara D, Bacal F, Bocchi EA. Validation of the Portuguese Version of the Minnesota Living with Heart Failure Questionnaire. Arq Bras Cardiol 2009;93:36-41. 12. Keteyian SJ, Levine AB, Brawner CA, Kataoka T, Rogers FJ, Schairer JR, et al. Exercise training in patients with heart failure. A randomized, controlled trial. Ann Intern Med. 1996;124:1051-7. 13. Carvalho VO, Ciolac EG, Guimares GV, Bocchi EA. Effect of Exercise Training on 24-Hour Ambulatory Blood Pressure Monitoring in Heart Failure Patients. Congest Heart Fail. 2009;15:176-80. 14. Belardinelli R, Giorgiou D, Cianci G, Purcaro A. Randomized, controlled trial of long-term moderate exercise training in chronic heart failure: effects on functional capacity, quality of life, and clinical outcome. Circulation. 1999;99:1173-82. 15. Hornig B, Maier V, Drexler H. Physical training improves endothelial function in patients with chronic heart failure. Circulation. 1996;93:2104. 16. Hambrecht R, Niebauer J, Fiehn E, Klberer B, Offner B, Hauer K, et al. Physical training in patients with stable chronic heart failure: effects on cardiorespiratory fitness and ultrastructural abnormalities of leg muscles. J Am Coll Cardiol. 1995;25:1239-49. 17. Hambrecht R, Gielen S, Linke A, Fiehn E, Yu J, Walther C, et al. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure: A randomized trial. JAMA. 2000;283:3095-101. 18. Piepoli M, Clark AL, Volterrani M, Adamopoulos S, Sleight P, Coats AJ. Contribution of muscle afferents to the hemodynamic, autonomic, and ventilatory responses to exercise in patients with chronic heart failure: effects of physical training. Circulation. 1996;93:940-52.
2.
3.
4.
5.
6.
7.
8.
9.
826
CLINICS 2009;64(8):824-7
Cardiovascular rehabilitation Carvalho VO et al. 22. Kihara T, Biro S, Imamura M, Yoshifuku S, Takasaki K, Ikeda Y, et al. Repeated Sauna Treatment Improves Vascular Endothelial and Cardiac Function in Patients With Chronic Heart Failure. J Am Coll Cardiol. 2002;39:754-9. 23. von Haehling S, Lainscak M, Springer J, Anker SD. Cardiac cachexia: A systematic overview. Pharmacol Ther. 2009;121:227-52. 24. Ingelsson E, Bjrklund-Bodegrd K, Lind L, Arnlv J, Sundstrm J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;28:2859-66.
19. Cider A, Svelv BG, Tng MS, Schaufelberger M, Andersson B. Immersion in warm water induces improvement in cardiac function in patients with chronic heart failure. Eur J Heart Fail. 2006;8:308-13. 20. Cider A, Schaufelberger M, Sunnerhagen KS, Andersson B. Hydrotherapy--a new approach to improve function in the older patient with chronic heart failure. Eur J Heart Fail. 2003;5:527-35. 21. Miyamoto H, Kai H, Nakaura H, Osada K, Mizuta Y, Matsumoto A, et al. Safety and Efficacy of Repeated Sauna Bathing in Patients With Chronic Systolic Heart Failure: A Preliminary Report. J Card Fail. 2005;11:432-6.
827
Вам также может понравиться
- T688 Series Instructions ManualДокумент14 страницT688 Series Instructions ManualKittiwat WongsuwanОценок пока нет
- Inter HugoДокумент10 страницInter HugorizkaОценок пока нет
- Final Project Exp590-3Документ19 страницFinal Project Exp590-3api-315973465Оценок пока нет
- 1 s2.0 S1836955322001163 MainДокумент2 страницы1 s2.0 S1836955322001163 MainIhuoma AnaghaОценок пока нет
- The Egyptian Heart Journal: Haitham Galal Mohammed, Adel Mohamed ShabanaДокумент6 страницThe Egyptian Heart Journal: Haitham Galal Mohammed, Adel Mohamed ShabanaDaniel Zagoto100% (1)
- Heart EksДокумент11 страницHeart EksAndri FerdianОценок пока нет
- 1 s2.0 S2405587515300263 MainДокумент8 страниц1 s2.0 S2405587515300263 Maindianaerlita97Оценок пока нет
- Cardiac Rehabilitation ThesisДокумент5 страницCardiac Rehabilitation ThesisScott Donald100% (1)
- Cardiovascular Disease and Exercise 2008Документ5 страницCardiovascular Disease and Exercise 2008OscarDavidGordilloGonzalezОценок пока нет
- Reading - Abses HeparДокумент6 страницReading - Abses HeparOulnstОценок пока нет
- Physiotherapy 3 1 2Документ4 страницыPhysiotherapy 3 1 2AjiОценок пока нет
- Diferent Exercise TrainingДокумент9 страницDiferent Exercise TrainingRenan Carraro RosaОценок пока нет
- JHH 2013 121Документ5 страницJHH 2013 121adri20121989Оценок пока нет
- Interval Endurance and Resistance Training As Part of A Community-Based Secondary Prevention Program For Patients With Diabetes Mellitus and Coronary Artery DiseaseДокумент7 страницInterval Endurance and Resistance Training As Part of A Community-Based Secondary Prevention Program For Patients With Diabetes Mellitus and Coronary Artery DiseaseMarcos Túlio de SáОценок пока нет
- WJC 3 248Документ8 страницWJC 3 248RIAN NUGRAHAОценок пока нет
- CHFfinalДокумент6 страницCHFfinalcrisanto valdezОценок пока нет
- Aerobic Exercise On CabgДокумент6 страницAerobic Exercise On CabgAmelia SianiparОценок пока нет
- A Single Session of Aerobic Exercise Reduces Systolic Blood Pressure at Rest and in Response To Stress in Women With Rheumatoid Arthritis and HypertensionДокумент9 страницA Single Session of Aerobic Exercise Reduces Systolic Blood Pressure at Rest and in Response To Stress in Women With Rheumatoid Arthritis and HypertensionRobles Murillo Carlos Eduardo Augusto 1FОценок пока нет
- 04 - Cardiometabolic Effects of High-Intensity Hybrid Functional Electrical Stimulation Exercise After Spinal Cord InjuryДокумент20 страниц04 - Cardiometabolic Effects of High-Intensity Hybrid Functional Electrical Stimulation Exercise After Spinal Cord Injurywellington contieroОценок пока нет
- 1 SM PDFДокумент12 страниц1 SM PDFPutria Rezki ArgathyaОценок пока нет
- Interval and Strength Training in CAD Patients: AuthorsДокумент6 страницInterval and Strength Training in CAD Patients: AuthorsTito AlhoОценок пока нет
- Risom 2020Документ10 страницRisom 2020drewantaОценок пока нет
- 1 s2.0 S2405587515300263 MainДокумент8 страниц1 s2.0 S2405587515300263 MainmaracioОценок пока нет
- Cardiac Rehabilitation and Exercise PhysiologyДокумент30 страницCardiac Rehabilitation and Exercise PhysiologyNiko YuandikaОценок пока нет
- Pending 1666841661 DownloadДокумент8 страницPending 1666841661 Downloadmilena martinsОценок пока нет
- Fonseca Et Al - 2017Документ23 страницыFonseca Et Al - 2017TAINAH DE PAULAОценок пока нет
- Jurnal KardiovaskularДокумент6 страницJurnal Kardiovaskularrizk86Оценок пока нет
- Aerobic Versus Isometric Handgrip Exercise in Hypertension: A Randomized Controlled TrialДокумент8 страницAerobic Versus Isometric Handgrip Exercise in Hypertension: A Randomized Controlled TrialROSAОценок пока нет
- Engineering Journal The Effects of Individualized Physical Rehabilitation ProgramДокумент7 страницEngineering Journal The Effects of Individualized Physical Rehabilitation ProgramEngineering JournalОценок пока нет
- Exercise and Physical Activity in The Prevention and Treatment of Atherosclerotic Cardiovascular DiseaseДокумент1 страницаExercise and Physical Activity in The Prevention and Treatment of Atherosclerotic Cardiovascular Diseaseapi-394215505Оценок пока нет
- Session 2 - Faizah Maulidiyah With CommentsДокумент1 страницаSession 2 - Faizah Maulidiyah With Commentsrenata JeslynОценок пока нет
- 2014 Exercise and Health Rev Esp CardiolДокумент6 страниц2014 Exercise and Health Rev Esp CardiolLuis Solano NogalesОценок пока нет
- Effects of HIIT On Aerobic Capacity in Cardiac Patients, A Sistematic Review With Metanalysis - 2017Документ17 страницEffects of HIIT On Aerobic Capacity in Cardiac Patients, A Sistematic Review With Metanalysis - 2017alarconscamilaОценок пока нет
- S0003999321002963Документ10 страницS0003999321002963Nura Eky VОценок пока нет
- The Effect of Physical Training in Chronic Heart FailureДокумент5 страницThe Effect of Physical Training in Chronic Heart FailureDitaris GIОценок пока нет
- AHA Heart Article 2 Week 13Документ12 страницAHA Heart Article 2 Week 13beniak_preОценок пока нет
- Effects of High-Intensity Inspiratory Muscle Training Associated With Aerobic Exercise in Patients Undergoing CABG: Randomized Clinical TrialДокумент8 страницEffects of High-Intensity Inspiratory Muscle Training Associated With Aerobic Exercise in Patients Undergoing CABG: Randomized Clinical TrialJulenda CintarinovaОценок пока нет
- Treinamento Dinâmico e de Força e Melhora Da Saúde Cardiovascular em ObesosДокумент11 страницTreinamento Dinâmico e de Força e Melhora Da Saúde Cardiovascular em ObesosDinho MengoОценок пока нет
- Optimal Timing of A Physical Exercise Intervention To Improve Cardiorespiratory Fitness During or After ChemotherapyДокумент13 страницOptimal Timing of A Physical Exercise Intervention To Improve Cardiorespiratory Fitness During or After ChemotherapyJoao da HoraОценок пока нет
- Tensión Arterial y Ejercicio de FuerzaДокумент8 страницTensión Arterial y Ejercicio de Fuerzaabraham landaetaОценок пока нет
- Cardiac Rehabilitatio N: Presented By: Priyanka GohereДокумент14 страницCardiac Rehabilitatio N: Presented By: Priyanka GoherePriyankaОценок пока нет
- Villelabeitia Jaureguizar 2016 Journal of Cardiopulmonary Rehabilitation and PreventionДокумент10 страницVillelabeitia Jaureguizar 2016 Journal of Cardiopulmonary Rehabilitation and PreventionPablo Damian LeivaОценок пока нет
- Recommendations For Prescribing Exercise To Patients With Heart DiseaseДокумент9 страницRecommendations For Prescribing Exercise To Patients With Heart DiseaseGeorge Blaire RasОценок пока нет
- Core Muscle StrengtheningДокумент56 страницCore Muscle StrengtheningVijayalaxmi KathareОценок пока нет
- Brazilian Journal of Physical TherapyДокумент12 страницBrazilian Journal of Physical TherapyKen ABОценок пока нет
- Am J Hypertens 2015 Sharman 147 58Документ12 страницAm J Hypertens 2015 Sharman 147 58yusnadiОценок пока нет
- 10 1111@sms 13853Документ17 страниц10 1111@sms 13853Cintia BeatrizОценок пока нет
- Angadi, 2015Документ6 страницAngadi, 2015Prana JagannathaОценок пока нет
- Ventrículo Esquerdo Mecânica, Cardíaca Autonômica e MetabólicaДокумент31 страницаVentrículo Esquerdo Mecânica, Cardíaca Autonômica e MetabólicaThiago SartiОценок пока нет
- Medical Sciences: The Effects of Acute High-Intensity Interval Training On Hematological Parameters in Sedentary SubjectsДокумент7 страницMedical Sciences: The Effects of Acute High-Intensity Interval Training On Hematological Parameters in Sedentary SubjectsKhalid AlfiadyОценок пока нет
- Ijerph 17 07233Документ12 страницIjerph 17 07233Mumtaz MaulanaОценок пока нет
- Keteyian 1996Документ7 страницKeteyian 1996muratigdi96Оценок пока нет
- Presentasi JurnalДокумент19 страницPresentasi JurnalReggie Christian GОценок пока нет
- CpetДокумент16 страницCpetFaizal AblansahОценок пока нет
- Anti-Inflammatory Effects of ExerciseДокумент10 страницAnti-Inflammatory Effects of Exercisejbone918Оценок пока нет
- BMC Cardiovascular DisordersДокумент9 страницBMC Cardiovascular DisordersRamaalgi OctaviantoОценок пока нет
- Exercício Físico e Autofagia Seletiva Benefício e Risco Na Saúde CardiovascularДокумент18 страницExercício Físico e Autofagia Seletiva Benefício e Risco Na Saúde CardiovascularHenrique WilliamОценок пока нет
- Hypertension and ExerciseДокумент8 страницHypertension and ExercisemeyqiОценок пока нет
- Presentation 1Документ31 страницаPresentation 1hababneh790Оценок пока нет
- Exercise Training For Blood Pressure: A Systematic Review and Meta-AnalysisДокумент9 страницExercise Training For Blood Pressure: A Systematic Review and Meta-AnalysisAnonymous 7dsX2F8nОценок пока нет
- Exercise Physiology for the Pediatric and Congenital CardiologistОт EverandExercise Physiology for the Pediatric and Congenital CardiologistОценок пока нет
- Rocker ScientificДокумент10 страницRocker ScientificRody JHОценок пока нет
- ProbДокумент10 страницProbKashif JawaidОценок пока нет
- Course DescriptionДокумент54 страницыCourse DescriptionMesafint lisanuОценок пока нет
- Contemp Person Act.1Документ1 страницаContemp Person Act.1Luisa Jane De LunaОценок пока нет
- User ManualДокумент96 страницUser ManualSherifОценок пока нет
- Ransomware: Prevention and Response ChecklistДокумент5 страницRansomware: Prevention and Response Checklistcapodelcapo100% (1)
- UBMM1011 Unit Plan 201501Документ12 страницUBMM1011 Unit Plan 201501摩羯座Оценок пока нет
- Personal Narrative RevisedДокумент3 страницыPersonal Narrative Revisedapi-549224109Оценок пока нет
- Investigative JournalismДокумент8 страницInvestigative JournalismMitchie LlagasОценок пока нет
- Nyamango Site Meeting 9 ReportДокумент18 страницNyamango Site Meeting 9 ReportMbayo David GodfreyОценок пока нет
- Energy-Roles-In-Ecosystems-Notes-7 12bДокумент10 страницEnergy-Roles-In-Ecosystems-Notes-7 12bapi-218158367Оценок пока нет
- Example of Flight PMDG MD 11 PDFДокумент2 страницыExample of Flight PMDG MD 11 PDFVivekОценок пока нет
- Check e Bae PDFДокумент28 страницCheck e Bae PDFjogoram219Оценок пока нет
- List of Olympic MascotsДокумент10 страницList of Olympic MascotsmukmukkumОценок пока нет
- Mindray PM 9000 User ID10240 PDFДокумент378 страницMindray PM 9000 User ID10240 PDFJuan FernandoОценок пока нет
- Reproduction in PlantsДокумент12 страницReproduction in PlantsAnand Philip PrasadОценок пока нет
- Exam First Grading 2nd Semester - ReadingДокумент3 страницыExam First Grading 2nd Semester - ReadingArleneRamosОценок пока нет
- Auto Turn-Off For Water Pump With Four Different Time SlotsДокумент3 страницыAuto Turn-Off For Water Pump With Four Different Time SlotsKethavath Sakrunaik K100% (1)
- New Microsoft Office Word DocumentДокумент5 страницNew Microsoft Office Word DocumentSukanya SinghОценок пока нет
- Carpentry Grade 8 Week 1 2Документ20 страницCarpentry Grade 8 Week 1 2SANTIAGO ALVISОценок пока нет
- BSDДокумент26 страницBSDEunnicePanaliganОценок пока нет
- PNGRB - Electrical Safety Audit ChecklistДокумент4 страницыPNGRB - Electrical Safety Audit ChecklistKritarth SrivastavОценок пока нет
- Process Description of Function For Every Unit OperationДокумент3 страницыProcess Description of Function For Every Unit OperationMauliduni M. AuniОценок пока нет
- Nyambe African Adventures An Introduction To African AdventuresДокумент5 страницNyambe African Adventures An Introduction To African AdventuresKaren LeongОценок пока нет
- What Are Some of The Best Books On Computer ScienceДокумент9 страницWhat Are Some of The Best Books On Computer ScienceSarthak ShahОценок пока нет
- Assembly InstructionsДокумент4 страницыAssembly InstructionsAghzuiОценок пока нет
- Guidelines For Plenipotentiary - 1Документ6 страницGuidelines For Plenipotentiary - 1Oladimeji Ibukun IjaodolaОценок пока нет
- What Are The Advantages and Disadvantages of UsingДокумент4 страницыWhat Are The Advantages and Disadvantages of UsingJofet Mendiola88% (8)
- Rab Sikda Optima 2016Документ20 страницRab Sikda Optima 2016Julius Chatry UniwalyОценок пока нет