Академический Документы
Профессиональный Документы
Культура Документы
Introduction To Nervous System
Загружено:
Ernie G. Bautista II, RN, MDОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Introduction To Nervous System
Загружено:
Ernie G. Bautista II, RN, MDАвторское право:
Доступные форматы
INTRODUCTION TO NERVOUS SYSTEM I. CNS (brain & spinal cord) II.
PNS contains: - Nerves cranial & spinal - Plexus - Ganglia Functional Divisions I. Somatic NS II. Autonomic NS a. Sympathetic b. Parasympathetic Anatomical Levels of Nervous System 1. SUPRATENTORIAL level a. Located above tentorium cerebelli 2. INFRATENTORTIAL/ Posterior Fossa level a. Located below tentorium cerebelli BUT above foramen magnum 3. SPINAL level a. Located below foramen magnum BUT contained within the vertebral column 4. PERIPHERAL level a. Located outside the skull & vertebral column SUPRATENTORIAL 1. CNs 1 & 2 2. Basal ganglia 3. Cerebrum 4. Hypothalamus 5. Thalamus INFRATENTORIAL 1. CNs 3-7 2. Brainstem 3. Cerebellum 4. Midbrain 5. Pons & Medulla of Oblangata SPINAL - - compression is inside 1. Spinal Cord 2. Spinal nerves within vertebral column PERIPHERAL - - compression is outside
1.
Neuromuscular structures located outside skull & cerebral column including Cranial nerves & Spinal nerves and their peripheral branches
Lesions of the Nervous Systems A. TOPOGRAPHY of the Lesions - Anatomical location of the pathologic process and a judgment as to whether the abnormality is: o FOCAL strictly confined to a single circumscribed anatomical area Localized o DIFFUSE distributed over a wide areas; may involve only a single level or it may be distributed over multiple levels; bilateral Ex: meningitis, Alzheimers dse. B. MORPHOLOGY of the Lesions - The gross & histologic appearance of the abnormal area & the judgment whether the pathologic is: o NON MASS altering cellular function in the area of the lesion but is not significantly interfering w/ neighboring function; NOT compressing/destroying or damaging nearby structures o MASS lesion is of sufficient size & volume to interfere with neighboring cell structure Ex: tumor, blood clot, abscess formation C. DEVELOPMENT of SYMPTOMS - ACUTE within minutes - SUBACUTE within days - CHRONIC within weeks, months or years o Ex. Tumor D. EVOLUTION of SYMPTOMS 1. TRANSIENT when symptoms have resolved completely after onset 2. IMPROVING when symptoms have decreased from the maximum but have not completely resolved 3. PROGRESSIVE when symptoms continue to increase in severity; addition of new symptoms 4. STATIONARY when symptoms remain unchanged after reaching maximum severity
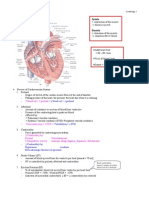
E. ETIOLOGY OF LESIONS 1. Degenerative chronic, progressive, diffuse (alzheimers & parkinsons) 2. Neoplastic chronic, progressive, focal (tumors) 3. Vascular 4. Inflammatory 5. Toxic metabolic 6. Traumatic 7. Immunologic SPINAL CORD ANATOMY & LESIONS spinal cord terminates at lower border of L1 & upper border of L2 - vertebral column i. cervical 8 ii. thoracic 12 iii. lumbar 5 - VERTEBRA HAS i. ANTERIOR segment ii. POSTERIOR segment iii. INTERVERTEBRAL disc SPINAL CORD - Lies within the vertebral canal & protected by 3 surrounding fibrous membranes called MENINGES - Held in position by the DENTICULATE ligaments on each side & FILUM TERMINALE inferiorly - Segmented & paired posteriorly/sensory and anterior/motor roots corresponsing to each segment of the cord. - Leave the vertebral canal through the INTERVERTEBRAL FORAMINA - Shorter than the vertebral column & terminates in the adult at the level of the lower L1 and upper border of L2 - Composed of: o Gray & White matter o Central Canal Parts of Gray Matter - Anterior horn - Posterior horn - Lateral horn - Gray commisure/ central canal Columns in the White Matter - POSTERIOR funiculus - LATERAL funiculus
NOTE: >Spinal nerve = all MIXED NERVE
>Cranial nerve = SENSORY NERVE
EGBautistaII
ANTERIOR funiculus
Each Column is subdivided into tracts: - Ascending tracts - Descending tracts - Intersegmentral tracts Laminae of nerve groupings Location Laminae 1-6 - Posterior horn Laminae 7 - Lateral horn Laminae 8-9 - Anterior horn Laminae 10 - Gray substance surrounding the central canal 3 Principal Fibers Tracts I. Dorsal Tracts 1. Fasciculus gracilis (medial/ more upper) a. provides proprioception of the lower limbs and trunk to the brain stem b. Additional functions of the fasciculus gracilis include carrying deep touch, vibrational, and visceral pain information to the brain stem. 2. Fasciculus cuneatus (lateral/ more lower) a. The cuneate fasiculus carries information from vertebral level T6 and up, while the fasiculus gracilis carries information from vertebral levels below T6. NOTE: The fasciculus gracilis and the cuneate fasiculus offer the same functions but can be differentiated by the vertebral level at which information is provided. The 2 fasciculus is divided by POSTEROINTERMEDIATE SULCUS The fibre tracts within the white matter of the spinal cord are named to indicate whether they are ascending (sensory) or descending (motor) tracts. Ascending tracts usually start with the prefix spino- and end with the name of the brain region where the spinal cord fibres first synapse. The anterior spinothalamic tract, for example, carries impulses conveying the sense of touch and pressure, and synapses in the thalamus. From there it is relayed to the cerebral cortex. Descending motor tracts, conversely, begin with a prefix denoting the brain region that gives rise to the fibres and end with the suffix -spinal. The lateral corticospinal tracts, for
EGBautistaII
example, begin in the cerebral cortex and descend the spinal cord. Ascending - convey sensory information from cutaneous receptors, proprioceptors (muscle and joint senses), and visceral receptors. Most of the sensory information that originates in the right side of the body crosses over and eventually reach the region on the left side of the brain, which analyses this information. (vice vesa) Information arising in the left side of the body is ultimately analyzed by the right side of the brain. Descending Two major groups of descending tracts from the brain: o corticospinal, or pyramidal tracts, and o extrapyramidal tracts. corticospinal fibres decussate in the pyramids of the medulla oblongata (hence the name "pyramidal tracts") and descend in the lateral corticospinal tracts, which decussate in the spinal cord. Because of the crossing of fibres, the right cerebral hemisphere controls the musculature on the left side of the body, where the left hemisphere controls the right musculature. The corticospinal tracts are primarily concerned with the control of fine movement that requires dexterity. extrapyramidal motor tracts, which originate in the midbrain and brain stem regions. o Reticulospinal tracts are the major descending pathways of the extrapyramidal system.
3. Touch 4. Pain 5. Temperature DERMATOMES to localize levels of lesions C2 Back of head C5 Tip of the shoulder C6 Thumb C7 Middle finger C8 Small finger T4-T5 Nipple T10 Umbilicus L1 Inguinal L4-L5 Big toe S1 Small toe S5 Perineum
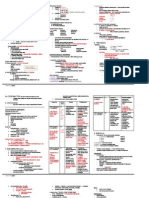
DESCENDING TRACTS MOTOR pathway only
Composed of: 1. Lateral Corticospinal 2. Rubrospinal 3. Lateral & Medial Reticulospinal 4. Vesibulospinal 5. Tectospinal 6. Anterior Corticogninal Injury in the following affects (motor/sensory) o Posterior horn SENSORY o Anterior horn MOTOR o Corticospinal tract MOTOR o Lateral Spinothalamic tract SNESORY
ASCENDING TRACTS SENSORY pathway only
Functions of DORSAL/ POSTERIOR column: o Position sense o 2 point discrimination o Fine, discriminative o Vibration sense o Stereognosis Functions of SPINOTHALAMIC TRACT o ANTERIOR stt for pressure & touch o LATERAL stt for pain & temperature (5) PROPRIOCEPTION: 1. Functions of Dorsal/Posterior column 2. Pressure
PYRAMIDAL SYSTEM Provides voluntary control of skeletal muscles Owes its name tot eh pyramidal cells of the primary motor cortex Sometimes called the direct activation systems because of its straight pathway from the cortex to the cranial & spinal nerves Its fibers are divided into: o Corticospinal & Corticobulbar tracts Corticospinal tracts o Made up of axons that descend down from the cortex, through the internal capsule, the brainstem, and into the spinal cord. The axons terminate in the
spinal cord, where many of them synapse with spinal nerves. Corticobulbar tracts o Also made up of axons descending from cortex, but its axons terminate in brainstem, where synapse eventually with the cranial nerves Originates: primary motor cortex Axons of pyramidal cells descend in the internal capsule & extend into the brainstem & spinal cord to synapse on lower motor neurons Descending pathways referred to as upper motor neuron In order to have PARALYSIS, it must have injury in: o CORTICOSPINAL TRACT Leading to upper motor neuron lesion o ANTERIOR HORN cells Leading to lower motor neuron lesion Ex: POLIO POLIO Acute viral infection of the neurons of anterior gray columns of spinal cord The muscles of lower limb are more affected Note: Injury in CORTICOSPINAL TRACT o Contra lateral o Injury in RIGHT side = LEFT side paralysis Traumatic injury in SPINAL CORD o Ipsilateral o Injury in RIGHT spinal cord = RIGHT side para. Lower motor neuron lesions Flaccid + + decresed
CLINICAL SIGNS of spinal cord disorders 1. Motor findings 2. sensory level 3. DTR 4. _
AMYOTROPHIC LATERAL SCLEROSIS (ALS) MOTOR
-
Pure motor disease involving the degeneration of anterior horn cells (Lower motor neuron lesion) & coticospinal tract (upper motor neuron lesion)
SPINAL SHOCK
Follows acute damage to the spinal cord; temporary interruption of the function of spinal cord following injury All cord functions below the level of lesions & become depressed or lost Persists for less than 24 hours or may persist for as long as 14 weeks Can be determined by testing for the activity of anal sphincter reflex
SUBACUTE COMBINED DEGENERATION - BOTH
Caused by vitamin B12 deficiency Degenerations of posterior & lateral column Loss of position sense & vibration in legs associated with UMNL Spinal cord hemisection Features o Contralateral loss of pain & temperature o Ipsilateral loss of proprioception o Ipsilateral manifestations of upper & lower motor neuron lesions L2-L3 level with nerve root compression
BROWN-SEQUARDs SYNDROME BOTH
-
Manifestations of Spinal Shock Flaccid, areflexic paralysis Complete loss of sensation Loss of autonomic function Loss of reflex activity paralysis of bladder & rectum Destructive spinal cord syndromes Complete core transaction Anterior cord Central cord Brown Sequards = hemisection (R&L side paralysis SPINAL CORD LESIONS SYRINGOMYELIA - SENSORY - Progressive cavitation around central canal - Loss of pain & temperature sensations in hands & forearm - Common in cervical - Sensory loss dissociated
HERNIATED LUMBAR DISC
LEMNISCAL PATHWAY The sensory pathway responsible for transmitting touch, vibration and conscious proprioceptive information from the body to the cerebral cortex. Clinical signs of injury to the Lemniscal pathway (Dorsal/posterior column lemniscus pathway) 1. Inability to recognize limb position 2. Astereognosis - inability to identify an object by touch without visual input. 3. Loss of 2-point discrimination 4. Loss of vibration sense 5. (+) Romberg sign a. Test for drunken driving b. The exam is based on the premise that a person requires at least two of the three following senses to maintain balance while standing: proprioception (the ability to know one's body in space), sensation (the ability to feel touch, pressure, or vibration -- e.g., to feel one's feet against the ground), and vision (which can be used to monitor changes in balance).
SIGNS OF MOTOR NEURON LESIONS Upper motor neuron lesions Paralysis Spastic Atropy Fasciculations Clonus + Pathologic reflexes + Muscle tone Increased LESIONS OF CORTICOSPINAL TRACT
POLIOMYELITIS - MOTOR
-
Attacks the anterior horn cells leading to lower motor neuron loss Caused by neurosyphilis Dorsal root involvement with secondary degeneration of dorsal columns sensory loss Loss of vibrations & position sense
TABES DORSALIS - SENSORY
-
EGBautistaII
c.
Used to investigate the cause of loss of motor coordination (ataxia). A positive Romberg test suggests that the ataxia is sensory in nature, which is, depending on loss of proprioception.
EGBautistaII
Вам также может понравиться
- Neuro LesionsДокумент7 страницNeuro Lesionskep1313100% (5)
- Mnemonic For Medical Students For Upper and Lower Motor LesionsДокумент1 страницаMnemonic For Medical Students For Upper and Lower Motor LesionsLe-Ann Mariamlelue100% (2)
- Master Muscle ListДокумент7 страницMaster Muscle ListSyed AbudaheerОценок пока нет
- Differentials and Tests Condition Condition: TH THДокумент4 страницыDifferentials and Tests Condition Condition: TH THlawlor_jcОценок пока нет
- MED (Neuro) - NeuroanatomyДокумент6 страницMED (Neuro) - NeuroanatomyFlora XuОценок пока нет
- NeuroTracts - Ascending, Descending, UMN, LMNДокумент5 страницNeuroTracts - Ascending, Descending, UMN, LMNBrandi Allen HensonОценок пока нет
- Cerebellum and Brain Stem: DR Asim Shrestha SRCC Ped Neuro Fellow MumbaiДокумент71 страницаCerebellum and Brain Stem: DR Asim Shrestha SRCC Ped Neuro Fellow MumbaiAsim ShresthaОценок пока нет
- Muscles of Breathing and Posture - Functions and InnervationДокумент6 страницMuscles of Breathing and Posture - Functions and Innervatione jeighОценок пока нет
- Summary of Cranial Nerves and Their FunctionsДокумент2 страницыSummary of Cranial Nerves and Their Functionscrsoriano2011Оценок пока нет
- Cerebellar DisordersДокумент29 страницCerebellar DisordersArslan Aslam100% (1)
- Skeletal SystemДокумент29 страницSkeletal SystemCrii XiaОценок пока нет
- Anterior Triangle of The NeckДокумент6 страницAnterior Triangle of The NeckHugh JacobsОценок пока нет
- 21-Spinal Cord TractsДокумент23 страницы21-Spinal Cord TractsALFAHRUL CAHYADIОценок пока нет
- DiencephalonДокумент4 страницыDiencephalonErnie G. Bautista II, RN, MD100% (3)
- DiencephalonДокумент4 страницыDiencephalonErnie G. Bautista II, RN, MD100% (3)
- Basal GangliaДокумент29 страницBasal Gangliaapi-19916399Оценок пока нет
- B16M01L07 - Cranial Nerves ExaminationДокумент13 страницB16M01L07 - Cranial Nerves ExaminationDonnaBells Hermo LabaniegoОценок пока нет
- Lesions of Upper Motor Neurons and Lower Motor NeuronsДокумент9 страницLesions of Upper Motor Neurons and Lower Motor NeuronsJessy Ahmed El DamacyОценок пока нет
- Muscle Innervation Chart IIДокумент7 страницMuscle Innervation Chart IIkimsue9448Оценок пока нет
- Cardiac SystemДокумент7 страницCardiac Systemsccctutor100% (3)
- Pathways For Neuroanatomy SCT: R. Heaslip M. JamesДокумент15 страницPathways For Neuroanatomy SCT: R. Heaslip M. Jameshzol83Оценок пока нет
- Explore the Nervous System in 40 CharactersДокумент31 страницаExplore the Nervous System in 40 CharactersDeology JuaninoОценок пока нет
- Chapter 06 NeuroДокумент22 страницыChapter 06 NeuroKarla Fralala100% (1)
- Neuroscience - 4.3 - Examination of Cerebellar Systems and Meninges (KSD)Документ4 страницыNeuroscience - 4.3 - Examination of Cerebellar Systems and Meninges (KSD)Kevin C. AguilarОценок пока нет
- Somatosensory SystemДокумент5 страницSomatosensory Systemaloepathic100% (3)
- Motor and Sensory Examination: Dr. Bandar Al Jafen, MD Consultant NeurologistДокумент36 страницMotor and Sensory Examination: Dr. Bandar Al Jafen, MD Consultant NeurologistJim Jose Antony100% (1)
- SMP Neuro Lab ManualДокумент37 страницSMP Neuro Lab Manualsas345sas345Оценок пока нет
- Neurological Physical Exam GuideДокумент3 страницыNeurological Physical Exam Guidejyhn24Оценок пока нет
- Understanding the Cerebellum: Anatomy, Functions and Clinical LocalizationДокумент70 страницUnderstanding the Cerebellum: Anatomy, Functions and Clinical Localizationmandeep axonОценок пока нет
- Introduction to the Somatosensory Axis of the Nervous SystemДокумент94 страницыIntroduction to the Somatosensory Axis of the Nervous SystemGks100% (1)
- Brainstem & LesionsДокумент4 страницыBrainstem & LesionsErnie G. Bautista II, RN, MDОценок пока нет
- Brainstem & LesionsДокумент4 страницыBrainstem & LesionsErnie G. Bautista II, RN, MDОценок пока нет
- UrolithiasisДокумент79 страницUrolithiasisErnie G. Bautista II, RN, MDОценок пока нет
- Neurology MnemonicsДокумент2 страницыNeurology MnemonicsJan Taplin100% (1)
- Cerebellar DisordersДокумент51 страницаCerebellar DisorderswasimОценок пока нет
- Introduction To Nervous SystemДокумент4 страницыIntroduction To Nervous SystemErnie G. Bautista II, RN, MD100% (1)
- Neurological History and ExaminationДокумент30 страницNeurological History and ExaminationMaria Agatha100% (1)
- RS 211 - Positioning ChartsДокумент55 страницRS 211 - Positioning ChartsKC FinnОценок пока нет
- LMN VS UmnДокумент10 страницLMN VS UmnyosuaОценок пока нет
- Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)Документ6 страницChapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD90% (21)
- CerebrumДокумент12 страницCerebrumDr santoshОценок пока нет
- Spinal Cord LesionsДокумент110 страницSpinal Cord Lesionsgtaha80100% (1)
- Motor Neuron Disease.Документ38 страницMotor Neuron Disease.sanjana sangleОценок пока нет
- Action Potential NotesДокумент2 страницыAction Potential NotesJohn OsborneОценок пока нет
- Crocodiles - Biology, Husbandry and DiseasesДокумент352 страницыCrocodiles - Biology, Husbandry and DiseasesSiva Subramanian100% (1)
- Chapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Документ3 страницыChapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD91% (34)
- Cranial Nerves (Association & Motor Neurons)Документ2 страницыCranial Nerves (Association & Motor Neurons)Ernie G. Bautista II, RN, MD100% (3)
- Cranial Nerves (Association & Motor Neurons)Документ2 страницыCranial Nerves (Association & Motor Neurons)Ernie G. Bautista II, RN, MD100% (3)
- AnatomyThe Vertebral ColumnДокумент70 страницAnatomyThe Vertebral ColumnJardee DatsimaОценок пока нет
- Antimicrobial AgentsДокумент3 страницыAntimicrobial AgentsErnie G. Bautista II, RN, MD100% (2)
- Ascending Descending TractsДокумент46 страницAscending Descending Tractsyasrul izad100% (3)
- 06 - Sullivan - A ReviewerДокумент56 страниц06 - Sullivan - A ReviewerCatrina Tan100% (2)
- Subcutaneous Systemic Opportunistic MycosesДокумент5 страницSubcutaneous Systemic Opportunistic MycosesErnie G. Bautista II, RN, MD100% (2)
- EnterobacteriaceaeДокумент3 страницыEnterobacteriaceaeErnie G. Bautista II, RN, MDОценок пока нет
- Descending Tracts: Dr. Niranjan Murthy H L Asst Prof of Physiology SSMC, TumkurДокумент23 страницыDescending Tracts: Dr. Niranjan Murthy H L Asst Prof of Physiology SSMC, Tumkurnirilib100% (1)
- 2017 Neuromuscular Pimp SheetДокумент30 страниц2017 Neuromuscular Pimp SheetAng LiОценок пока нет
- Herpes, Pox, Rhabdo, Arena VIRUSДокумент7 страницHerpes, Pox, Rhabdo, Arena VIRUSErnie G. Bautista II, RN, MDОценок пока нет
- Tracts of Spinal CordДокумент4 страницыTracts of Spinal CordBrian HelbigОценок пока нет
- OMM Year 1Документ22 страницыOMM Year 1bgav00Оценок пока нет
- 11-Acid-Base BalanceДокумент28 страниц11-Acid-Base BalanceKathlene BarasiОценок пока нет
- Ascending TractsДокумент42 страницыAscending TractsJustine Nyangaresi100% (2)
- Spinal Cord Disease by GadisaДокумент128 страницSpinal Cord Disease by GadisaGadisa DejeneОценок пока нет
- Spinal Cord InjuryДокумент17 страницSpinal Cord InjuryTom MallinsonОценок пока нет
- Localizing The LesionДокумент30 страницLocalizing The LesionTracy NwanneОценок пока нет
- Eye and Ear HistologyДокумент96 страницEye and Ear HistologyErnie G. Bautista II, RN, MD100% (1)
- Vertebral Arteries, and Their Divisions. Arteries Fuse To Form The Basilar ArteryДокумент6 страницVertebral Arteries, and Their Divisions. Arteries Fuse To Form The Basilar Arterymurali_bharadwazОценок пока нет
- Cranial Nerve Exam Part 1Документ9 страницCranial Nerve Exam Part 1Jennifer Pisco LiracОценок пока нет
- MISC Bacteria (Legionella, Listeria, Gardnerella, Actinobacillus, Bartonella, Calymato-Bacterium, Flavobacterium, Streptobacillus)Документ6 страницMISC Bacteria (Legionella, Listeria, Gardnerella, Actinobacillus, Bartonella, Calymato-Bacterium, Flavobacterium, Streptobacillus)Ernie G. Bautista II, RN, MDОценок пока нет
- Chapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Документ3 страницыChapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD100% (5)
- Histology of Sensory & Motor Nerve EndingsДокумент2 страницыHistology of Sensory & Motor Nerve EndingsErnie G. Bautista II, RN, MD100% (1)
- Ricketsiae BacteriaДокумент2 страницыRicketsiae BacteriaErnie G. Bautista II, RN, MDОценок пока нет
- Spinal CordДокумент48 страницSpinal CordDr.Saber - Ar - Raffi100% (1)
- Sporeforming & Non-Spore Forming BacteriaДокумент9 страницSporeforming & Non-Spore Forming BacteriaErnie G. Bautista II, RN, MD100% (1)
- Guide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Документ8 страницGuide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Ernie G. Bautista II, RN, MD100% (6)
- Diseases of The Spinal CordДокумент89 страницDiseases of The Spinal CordLolla SinwarОценок пока нет
- Neurological AssessmentДокумент10 страницNeurological AssessmentmatsumotoОценок пока нет
- Stroke FullДокумент10 страницStroke Fullshowkat3Оценок пока нет
- Blood Supply of The BrainДокумент55 страницBlood Supply of The BrainueumanaОценок пока нет
- Anatomy MnemonicsДокумент2 страницыAnatomy MnemonicsPia Boni0% (1)
- Physical and Neurological ExaminationДокумент7 страницPhysical and Neurological ExaminationMelissa Marie SkillingsОценок пока нет
- Neuroscience I - Neurologic History Taking and Examination (POBLETE)Документ9 страницNeuroscience I - Neurologic History Taking and Examination (POBLETE)Johanna Hamnia PobleteОценок пока нет
- Blood Supply To The Brain: Presenter: Kondapaneni AnushaДокумент44 страницыBlood Supply To The Brain: Presenter: Kondapaneni Anushaabhi4manyuОценок пока нет
- Jugular Venous PressureДокумент9 страницJugular Venous Pressuremoh86-Оценок пока нет
- LungsДокумент16 страницLungsJoher100% (1)
- Cranial Nerves OverviewДокумент17 страницCranial Nerves OverviewRiki AntoОценок пока нет
- KCR 2020 Guideline For Scientific ExhibitionДокумент2 страницыKCR 2020 Guideline For Scientific ExhibitionErnie G. Bautista II, RN, MDОценок пока нет
- Acne VulgarisДокумент49 страницAcne VulgarisErnie G. Bautista II, RN, MD100% (1)
- Antivirals, Rubella, Peecorna VIRUSДокумент3 страницыAntivirals, Rubella, Peecorna VIRUSErnie G. Bautista II, RN, MDОценок пока нет
- Parvo BacteriaДокумент2 страницыParvo BacteriaErnie G. Bautista II, RN, MDОценок пока нет
- Histology of Female Reproductive SystemДокумент2 страницыHistology of Female Reproductive SystemErnie G. Bautista II, RN, MDОценок пока нет
- AstrocytomaДокумент11 страницAstrocytomaErnie G. Bautista II, RN, MDОценок пока нет
- Development of Endocrine SystemДокумент1 страницаDevelopment of Endocrine SystemErnie G. Bautista II, RN, MDОценок пока нет
- Histology of Male Reproductive SystemДокумент2 страницыHistology of Male Reproductive SystemErnie G. Bautista II, RN, MDОценок пока нет
- Histology of Endocrine SystemДокумент1 страницаHistology of Endocrine SystemErnie G. Bautista II, RN, MD100% (1)
- General Sensory PathwaysДокумент1 страницаGeneral Sensory PathwaysErnie G. Bautista II, RN, MDОценок пока нет
- Development of Reproductive SystemДокумент2 страницыDevelopment of Reproductive SystemErnie G. Bautista II, RN, MDОценок пока нет
- Lower Limb: Front and Medial Aspect of ThighДокумент8 страницLower Limb: Front and Medial Aspect of ThighErnie G. Bautista II, RN, MDОценок пока нет
- Herniated Nucleus PulposusДокумент12 страницHerniated Nucleus PulposusZascha Fushiany GunawanОценок пока нет
- Fish AnatomyДокумент44 страницыFish AnatomyZulficar Catamo100% (1)
- The Medico-Legal Back An Illustrated Guide, 2004 PDFДокумент210 страницThe Medico-Legal Back An Illustrated Guide, 2004 PDFvitaarfianaОценок пока нет
- SpondylodistitisДокумент32 страницыSpondylodistitisNurul Sakinah RosliОценок пока нет
- Orbicularis Oculi and Other Facial MusclesДокумент10 страницOrbicularis Oculi and Other Facial MusclesPATRICE ANNE ALCOREZAОценок пока нет
- Snakes Snake FactsДокумент34 страницыSnakes Snake FactsUday NakadeОценок пока нет
- Human Bones From A Late Minoan IB House at KnossosДокумент74 страницыHuman Bones From A Late Minoan IB House at KnossosAsterios AidonisОценок пока нет
- Nyeri Punggung Bawah (Low Back Pain) : DefinisiДокумент10 страницNyeri Punggung Bawah (Low Back Pain) : DefinisiheruОценок пока нет
- Thoracic Spine Quiz TestДокумент16 страницThoracic Spine Quiz TestAnuj AryanОценок пока нет
- ACFrOgBz6SCL6SA VJUDh46tP6NUDhw3P47 NPjiCaRlywgh9trN 5PhQeKcHqMl2xUsHtUBcc7n4mL1On5SlTP2X94BYDVb HoGkGegg5erftVOvtVci7Q4s0omLCXYn6dldjBQhk2bZ6Jpfl6cДокумент24 страницыACFrOgBz6SCL6SA VJUDh46tP6NUDhw3P47 NPjiCaRlywgh9trN 5PhQeKcHqMl2xUsHtUBcc7n4mL1On5SlTP2X94BYDVb HoGkGegg5erftVOvtVci7Q4s0omLCXYn6dldjBQhk2bZ6Jpfl6cMalavika A GОценок пока нет
- Biomedica Manikins CatalogДокумент64 страницыBiomedica Manikins CatalogRahul KashyapОценок пока нет
- RG 2021200079Документ16 страницRG 2021200079Rahul KashyapОценок пока нет
- AOSpine Thoracolumbar Classification System - Pocket Card PDFДокумент2 страницыAOSpine Thoracolumbar Classification System - Pocket Card PDFpatry_ordex100% (1)
- AxisДокумент1 страницаAxisLinОценок пока нет
- Vertebral Column of Teleosts Tail VertebraeДокумент3 страницыVertebral Column of Teleosts Tail VertebraeRosselle NoyoalОценок пока нет
- Lab Report Skeletal SystemДокумент9 страницLab Report Skeletal SystemLiza Shi0% (1)
- Lee Zu Ying Problem of The Spine 541-16-17Документ25 страницLee Zu Ying Problem of The Spine 541-16-17Star CruiseОценок пока нет
- Intra - and Inter-Rater Reliabilities of Infrasternal Angle MeasurementДокумент5 страницIntra - and Inter-Rater Reliabilities of Infrasternal Angle MeasurementJaime SousaОценок пока нет
- Kyphosis Physiotherapy From Childhood To Old Age: Jean Claude de MauroyДокумент26 страницKyphosis Physiotherapy From Childhood To Old Age: Jean Claude de MauroyromanciviОценок пока нет
- KyphosisДокумент22 страницыKyphosisRaiganОценок пока нет
- Ceratosaurus: (Dinosauria, Theropoda) A Revised OsteologyДокумент89 страницCeratosaurus: (Dinosauria, Theropoda) A Revised OsteologyMichael LovejoyОценок пока нет
- Osteology BonesДокумент48 страницOsteology BonesÂhmęd ĐoolaОценок пока нет