Академический Документы
Профессиональный Документы
Культура Документы
Novel Therapies CRPC
Загружено:
Razvan BardanИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Novel Therapies CRPC
Загружено:
Razvan BardanАвторское право:
Доступные форматы
Review Article
Novel Therapeutic Strategies for Castration Resistant Prostate Cancer: Inhibition of Persistent Androgen Production and Androgen Receptor Mediated Signaling
Arturo Molina*, and Arie Belldegrun
From the OrthoBiotech Oncology Research and Development, A Unit of Cougar Biotechnology and Institute of Urologic Oncology, David Geffen School of Medicine at University of California-Los Angeles (AB), Los Angeles, California
Purpose: Androgen receptor signaling remains essential for many prostate cancers that have progressed despite androgen deprivation therapy. After medical or surgical castration persistent though not insignicant low levels of androgens are produced from nongonadal sources, such as the adrenal glands. Some castration resistant prostate cancers acquire the ability to convert adrenal steroids to androgens, maintaining levels sufcient to activate androgen receptor. Inhibition of persistent androgen production and androgen receptor mediated signaling are relevant therapeutic strategies for castration resistant prostate cancer. Materials and Methods: The scientic foundation of and clinical experience with secondary hormonal therapy as well as the development of new investigational agents for castration resistant prostate cancer, specically selective cytochrome p450 17 inhibitors and second generation antiandrogens, are discussed. Results: Selective inhibition of cytochrome p450 17 has emerged as an important therapeutic pathway for castration resistant prostate cancer. The selective cytochrome p450 17 inhibitor abiraterone acetate showed promising activity and tolerability in phase I-II trials. Phase III studies are underway in men with chemotherapy nave castration resistant prostate cancer as well as those with progression after docetaxel based chemotherapy. TAK-700 and TOK-001 (formerly VN124-1) are novel selective cytochrome p450 17 inhibitors that recently entered phase I/II evaluation. MDV3100 is a second generation antiandrogen that blocks androgen receptor signaling by inhibiting nuclear translocation of the ligand-receptor complex. Clinical data on MDV3100 are encouraging and support continued phase III study. Conclusions: Novel therapies for castration resistant prostate cancer that target persistent androgen production and androgen receptor mediated signaling have demonstrated promising activity in many men with castration resistant prostate cancer and may redene the clinical management of these patients. Key Words: prostate, prostatic neoplasms, androgens, abiraterone, castration ANDROGEN deprivation therapy is the cornerstone of treatment for advanced or metastatic prostate cancer. Approximately 90% of patients respond to current rst line ADT strategies of medical castration with an LH-releasing hormone agonist (with or without an antiandrogen) or surgical castration.1 However,
0022-5347/11/1853-0787/0 THE JOURNAL OF UROLOGY 2011 by AMERICAN UROLOGICAL ASSOCIATION EDUCATION
Abbreviations and Acronyms AAWD antiandrogen withdrawal ACTH adrenocorticotropic hormone ADT androgen deprivation therapy AR androgen receptor CRPC castration resistant prostate cancer CYP17 DES DHEA LH PSA TTPP cytochrome p450 17 diethylstilbestrol dehydroepiandrostenedione luteinizing hormone prostate specic antigen time to PSA progression
Submitted for publication March 17, 2010. * Correspondence: OrthoBiotech Oncology Research and Development, A Unit of Cougar Biotechnology, 10990 Wilshire Blvd., Suite 1200, Los Angeles, California 90024 (telephone: 310-943-8040, extension 124; e-mail: AMolina7@its.jnj.com). Financial interest and/or other relationship with Ortho Biotech and Cougar Biotechnology.
ADT response duration is limited and most patients experience disease progression within 2 to 3 years. Traditional secondary hormonal manipulations, such as AAWD, or second line antiandrogens, glucocorticoids, estrogens or ketoconazole, can be of clinical benet in some patients after primary ADT failure (see
Vol. 185, 787-794, March 2011 Printed in U.S.A. DOI:10.1016/j.juro.2010.10.042
Editors Note: This article is the rst of 5 published in this issue for which category 1 CME credits can be earned. Instructions for obtaining credits are given with the questions on pages 1164 and 1165.
AND
RESEARCH, INC.
www.jurology.com
787
788
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
table).1 However, the response and duration of benet tend to decrease with each successive hormonal manipulation. Chemotherapy may be an option when hormone therapy fails. Docetaxel is currently the only agent to show improvement in overall survival in these patients as well as in pain and quality of life benets.2,3 Still, the incremental survival benet with docetaxel is only about 3 months.24 Currently median survival after failed initial ADT is approximately 18 months with fewer than 20% of patients surviving beyond 3 years.24 Prostate cancer remains the second leading cause of cancer related death in men in the United States and the need for new treatment options is critical. Disease progression despite medical or surgical castration signals the emergence of a prostate cancer phenotype that can survive and proliferate in a low androgen environment.5 Although it was once termed androgen independent or hormone refractory, it is now recognized that a signicant proportion of these tumors continue to rely on AR signaling6 and are more precisely characterized as CRPC. Selective inhibition of persistent androgen production in CRPC is emerging as a promising therapeutic strategy. Novel antiandrogens that interfere directly with AR mediated signaling pathways in CRPC are also generating substantial clinical interest. The current clinical development of these agents
as well as a brief review of hormonal strategies in CRPC to date is summarized. To standardize the measurement and reporting of the PSA response rate and TTPP clinical studies of these investigational agents are reported using criteria specied in the Prostate-Specic Antigen Working Group and/or Prostate Cancer Clinical Trials Working Group 2 guidelines.7,8
TRADITIONAL SECONDARY HORMONAL THERAPIES FOR CRPC
Cumulative experience with secondary hormonal therapies provides substantial clinical evidence that ligand mediated AR signaling remains functional in a large proportion of CRPCs. However, except for antiandrogens, current secondary hormonal strategies can be considered relatively nonspecic since they suppress pituitary-gonadal axis function or nonselectively inhibit adrenal and gonadal steroidogenesis. Clinical outcomes of traditional secondary hormonal therapies in CRPC are briey summarized. Antiandrogens The combination of an antiandrogen with gonadal androgen suppression (combined or maximal androgen blockade) or after failed initial androgen sup-
Select clinical trials of second line therapy with antiandrogens, estrogens and glucocorticoids, and nonspecic androgen inhibitors for CRPC PSA Response References 2nd Line antiandrogens: Fossa et al9 Small et al10 Suzuki et al11 Scher et al12 Kassouf et al13 Glucocorticoids: Bubley et al7 Small et al14 Kantoff et al15 Storlie et al16 Robertson et al17 Oh et al18 Smith et al19 Estrogens: Kruit et al20 Figg et al21 Ketoconazole: Scher et al8 Chen et al24 Linja et al25 Stanbrough et al26 Gregory et al27 Aminoglutehimide: Small et al22 Holzbeierlein et al23 * PSA responders combined. PSA decrease 80% or greater. Treatment (total daily mg) Flutamide (375), bicalutamide (80) High dose bicalutamide (150) High dose bicalutamide (150) High dose bicalutamide (200) Nilutamide (200 or 300) Prednisone (10) Prednisone (20) Hydrocortisone (40) Hydrocortisone (40) Dexamethasone (1.5) Dexamethasone (0.5-2) Dexamethasone (1.5) DES (3) DES (1) Ketoconazole Ketoconazole Ketoconazole Ketoconazole Ketoconazole (1,200) hydrocortisone (1,200) hydrocortisone (600) hydrocortisone (1,200) hydrocortisone (1,200) hydrocortisone AAWD No. Pts 193, 39 52 31 51 28 101 29 230 81 27 37 38 42 21 128 36 28 45 50 29 35 % 50% or Greater 34, 44 20 23 24 28 21 34 16 14 59 62 61 24 43 27 47 46 31 63 48 37 Median Duration (mos) 6.6* Not available Not available 4.0 7.0 Not available 2.0 2.3 2.3 Not available 9.0 Not available 3.8 Not available 8.6 6.3 7.5 Not available 3.5 4.0 9.0
Aminoglutethimide (900) hydrocortisone AAWD Aminoglutethimide (1,000) hydrocortisone
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
789
pression is often an effective therapeutic maneuver, although responsiveness is inversely related to disease extent. In this setting utamide produces a 50% or greater decrease in PSA in 80% of patients with localized disease, 54% with metastatic disease and 23% with symptomatic metastatic disease.9 Changes in PSA have also been seen upon AAWD, is likely related to the potential of these agents to show partial agonist activity, particularly in the presence of altered or mutated AR. In prospective studies AAWD was associated with a 50% or greater decrease in PSA in 10% to 15% of patients with prostate cancer with responses lasting a median of about 6 months.10,11 Changing to an alternate second line antiandrogen, such as high dose bicalutamide or nilutamide, is associated with a 50% or greater decrease in PSA in about a third of patients, with a median response duration of typically between 4 and 7 months (see table).1113 Glucocorticoids Glucocorticoids, which have a history of use as supportive therapy with steroidogenesis suppressive agents or as a control arm in chemotherapy trials, have modest activity alone in prospective CRPC trials. A 50% or greater decrease in PSA was reported in up to 20% of patients with CRPC on various prednisone or hydrocortisone regimens and in up to 60% on dexamethasone with a response of typically a median of about 2 months.9,14 16 The mechanisms underlying the glucocorticoid activity in CRPC are not well dened and in the absence of comparative randomized data no 1 particular agent or regimen is considered preferable. Estrogens Estrogens have long been known to be active against prostate cancer. The synthetic estrogen DES suppresses testosterone by decreasing LH-releasing hormone secretion as well as directly affecting pituitary LH production. Also, DES has direct cytotoxic activity in prostate cancer cell lines.17 A 50% or greater decrease in PSA was reported in 20% to 40% of patients with CRPC treated with DES with a median response duration of about 4 months (see table).18,19 However, a substantially increased risk of cardiac and vascular toxicities, including myocardial infarction, stroke and pulmonary embolism, is known to occur with DES and concomitant anticoagulation therapy is recommended with its use in patients with CRPC.1 Steroidogenesis Inhibitors Ketoconazole and aminoglutethimide, which are nonspecic androgen synthesis inhibitors, have efcacy for CRPC (see table). By blocking the conversion of cholesterol to pregnenolone, aminoglutethimide broadly inhibits adrenal steroid synthesis and its use necessitates cor-
ticosteroid supplementation.20 Common adverse effects include lethargy, nausea, skin rash, peripheral edema, hypothyroidism and increased hepatic enzyme. Aminoglutethimide has largely been supplanted by ketoconazole, an azole antifungal that inhibits multiple cytochrome p450 enzymes involved in androgen biosynthesis, including conversion of cholesterol to pregnenolone, 11 -hydroxylation and 17 -hydroxylase/C17,20-lyase (CYP17) activity.10 Ketoconazole produces a 50% or greater decrease in PSA in approximately 30% to 60% of CRPC cases with a median response duration of about 7 months.10,21,22 In the largest randomized study to date the combination of high dose ketoconazole with hydrocortisone and AAWD produced a 50% or greater decrease in PSA in 28% of CRPC cases compared to 11% for AAWD alone.10 Deferred use of ketoconazole after AAWD was associated with a 50% or greater decrease in PSA in 32% of patients. Circulating androgen, which initially decreased on ketoconazole therapy, increased at the time of disease progression, indicating failure of this agent to continuously suppress androgen biosynthesis. Side effects of ketoconazole, including lethargy, rash, gastrointestinal issues and potential adrenal suppression, can often limit treatment duration. Also, as a nonspecic p450 inhibitor ketoconazole has the potential to provoke drug-drug interactions by interfering with the metabolism of other drugs, including warfarin and various statins.
INSIGHTS INTO ANDROGEN PRODUCTION AND SIGNALING IN CRPC
AR Signaling Prostate cancer gene expression studies revealed that AR activated genes that are initially downregulated during ADT become reactivated upon transition to CRPC.23 Up-regulation of the AR gene coincides with this transition24 and AR gene amplication has been found in about 30% of CRPCs.25 The importance of ligand mediated AR signaling in CRPC is underscored by ndings of frequent AR over expression and heightened AR sensitivity related to increased receptor stabilization, enhanced nuclear localization and over expression of nuclear coactivators.23,2527 Point mutations may confer AR promiscuity, permitting activation by nonandrogenic ligands such as progesterone and estradiol.6 These nding support the theory that ligand dependent AR signaling may be a primary mediator of growth and survival among CRPCs. Ligand independent mechanisms may also have a role in persistent AR signaling in CRPC, as evidenced by the recent identication of several constitutively active AR splice variants.28
790
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
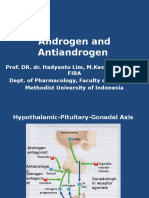
Persistent Androgen Production in Castrate Environment With current ADT strategies the suppression of gonadal androgen production results in castrate testosterone, dened as less than 50 ng/dl (less than 2.0 nM). Despite gonadal androgen suppression, low levels of circulating androgens persist, mainly due to peripheral conversion of adrenal steroids, and circulating testosterone may be seen at up to 10% of precastration levels.29 Recent ndings suggest that CRPCs acquire the ability to convert adrenal steroids to androgens, in essence creating an intracrine signaling system. Gene upregulation and expression of enzymes involved in androgen biosynthesis, including CYP17, have been documented in CRPC tissue23,26,30,31 with evidence of intratumor conversion of upstream precursors of testosterone and dihydrotestosterone present at concentrations sufcient to activate AR.32,33 These ndings have supported the clinical development of novel agents that selectively target persistent androgen production and ligand mediated AR binding in CRPCs. Role of CYP17 in Androgen Biosynthesis Cytochrome p450c17 (CYP17) catalyzes 2 essential reactions in androgen biosynthesis, including 17 hydroxylation of C21 steroids and cleavage of the C17,20 bond of C21 steroids.34 These reactions are key in the biosynthesis of DHEA and androstenedione, precursors of testosterone and estradiol (see gure). The biological consequences of CYP17 inhibition are illustrated by the clinical and biochemical features
of patients with congenital CYP17 deciency, a rare disorder characterized by adrenal hyperplasia, and inadequate synthesis of cortisol, androgen and estrogen, accompanied by impaired sexual development.34 Because mineralocorticoid biosynthesis is not impaired and due to the weak glucocorticoid activity provided by corticosterone, these patients do not have adrenocortical insufciency. However, in response to low circulating cortisol the cortisolACTH feedback loop is stimulated, leading to increased pituitary release of ACTH. This results in excess mineralocorticoid production and a clinical syndrome characterized by hypertension, hypokalemia, uid overload and renin suppression. This syndrome is effectively managed by low dose glucocorticoids with or without mineralocorticoid antagonists to suppress ACTH release.
SELECTIVE TARGETING OF CYP17 FOR CRPC
Given its critical role in androgen biosynthesis, CYP17 has generated interest as a relevant biological target for CRPC. Several novel therapeutic entities that selectively inhibit CYP17 are currently under clinical evaluation for CRPC (see Appendix). Abiraterone Acetate Abiraterone is a highly potent, selective, irreversible inhibitor of CYP17.35 Abiraterone prevents conversion of pregnenolone to DHEA and progesterone to androstenedione in the testes and adrenal glands. Abiraterone also appears to suppress de novo andro-
ACTH
Cholesterol
Pregnenolone
Progesterone
Corticosterone
Aldosterone
(Mineralocortocoids)
CYP17 (17-hydroxylase)
17-hydroxypregnenolone
17-hydroxyprogesterone
Cortisol
(Glucocortocoids)
CYP17 (C17,20 lyase)
Dehydroepiandrostenedione (DHEA)
Testosterone Androstenedione Estrogens
5-dihydrotestosterone
Steroid biosynthesis pathways and role of CYP17
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
791
gen production in prostate tumors, as evidenced by inhibition of CRPC growth in xenograft models devoid of testicular and adrenal androgens.36 Unlike nonspecic CYP17 inhibitors such as ketoconazole, abiraterone was not anticipated to impair mineralocorticoid synthesis, providing potential improved clinical tolerability. Early clinical evaluation of oral abiraterone acetate in noncastrate men showed that initial androgen suppression was soon overcome by a compensatory surge in luteinizing hormone and, as such, development focused on a castrate population.37 In phase I studies abiraterone acetate further decreased castrate testosterone to concentrations below detection limits.38,39 Other systemic effects consistent with selective CYP17 inhibition included stimulation of ACTH release in response to decreased cortisol and resulting increases in mineralocorticoid precursors (deoxycorticosterone and corticosterone) with little effect on aldosterone due to a negative feedback loop. As learned in patients with congenital CYP17 deciency, adding a supplemental glucocorticoid such as dexamethasone or prednisone suppresses ACTH release and is often effective for signs of mineralocorticoid excess, including hypertension, hypokalemia and uid retention. Pharmacokinetic analysis suggested that interaction with food, such as a high fat meal, tended to increase drug exposure, although these ndings were quite variable. As such, abiraterone acetate is given in a fasting state to maintain drug exposure as consistently as possible. In phase I/II studies in men with chemotherapy nave CRPC in whom multiple prior hormonal therapies had failed the pharmacodynamic effects of abiraterone acetate appeared to plateau at a dose of 750 to 1,000 mg, leading to the selection of 1,000 mg for continued phase II evaluation.38 41 Common adverse events of consistent mineralocorticoid excess included hypertension, hypokalemia and edema, which responded to management by the selective mineralocorticoid receptor antagonist eplerenone or low dose corticosteroids. Spironolactone was specifically avoided because of its potential androgenic properties. Other common adverse events were fatigue, headache, nausea and diarrhea. No dose limiting toxicity was seen with the administration of up to 2,000 mg abiraterone acetate daily. In a cohort of 42 patients treated with abiraterone acetate at the phase II dose of 1,000 mg 28 (67%) had a 50% or greater PSA decrease with a greater than 90% decrease in 8 (19%).40 Objective partial responses were seen in 9 of 24 patients (37.5%) with measurable disease. Median TTPP overall was 225 days (95% CI 162 to 287) with a median TTPP of 253 days (95% CI 122 to 383) in patients with a 50% or
greater decrease in PSA. Of 30 patients given dexamethasone 0.5 mg at the time of progression, which was permitted by protocol, a secondary PSA response of 50% or greater was noted in 10 (33%). Of interest, steroid levels downstream of CYP17 did not increase at the time of disease progression, suggesting sustained CYP17 inhibition.38 Prior ketoconazole was permitted in the phase I portion of the second phase I/II study.39 Of 33 phase I patients 19 (58%) had a 50% or greater decrease in PSA, including 10 of 19 (53%) with prior ketoconazole exposure. These ndings suggested a potential lack of cross resistance with prior ketoconazole. The phase II portion of this study added prednisone 5 mg twice daily to abiraterone acetate 1,000 mg daily and excluded patients with prior ketoconazole exposure.41 Preliminary ndings indicated a 50% or greater PSA decrease in 29 of 33 patients (88%) with a median TTPP of 337 days (95% CI 280 days, never attained). The use of prednisone markedly decreased the incidence and severity of hypokalemia, hypertension and uid retention. Except for single incidences of grade 3 hypertension and hypokalemia, most adverse events were grade 1 and no grade 4 events attributable to mineralocorticoid excess were seen. Phase II studies have evaluated abiraterone acetate as monotherapy and combined with low dose prednisone in men with CRPC and disease progression after docetaxel chemotherapy. In each study patients were heavily pretreated, and multiple hormonal therapies and up to 2 prior chemotherapies had failed. With abiraterone acetate monotherapy a 50% or greater decrease in PSA was seen in 24 of 47 patients (51%) with a median TTPP of 169 days (95% CI 130 to 281).42 Objective partial responses were seen in 6 patients (13%) and disease stabilization was noted in 25 (53%). In 11 patients (23%) there was improved performance status, a potential surrogate indicator of clinical benet. Consistent with expectations, adverse events included hypokalemia in 55% of cases, hypertension in 17% and uid retention in 15%, which responded to management by eplerenone or low dose corticosteroids. Abiraterone acetate combined with prednisone produced a 50% or greater decrease in PSA in 24 of 58 patients (41%), including 8 of 27 (30%) who were ketoconazole pretreated and 16 of 31 (52%) who were ketoconazole nave.43 Median TTPP was 99 days (95% CI 57 to 169) in patients with prior ketoconazole exposure and 198 days (95% CI 82 to not evaluable) in ketoconazole nave patients. The combination was well tolerated with adverse events consisting of primarily grade 1 or 2 hypokalemia, hypertension and uid retention. Abiraterone acetate is currently being evaluated in 2 randomized, mul-
792
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
ticenter, phase III studies of CRPC and accrual to these studies is complete. Features and characteristics that may predict response to abiraterone acetate are under evaluation. Pretreatment serum DHEA, DHEA-sulfate androstenedione and estradiol correlate with the probabilities of a 50% or greater PSA decrease and TTPP.44 In patients with a baseline circulating tumor cell count of 5/7.5 ml or greater a decrease to less than 5/7.5 ml was associated with a 50% or greater decrease in PSA.42,43 Correlations between serum testosterone levels and those in the tumor microenvironment in patients with CRPC with bone metastasis are also being explored.44 Preliminary ndings suggest that higher testosterone in the tumor microenvironment (bone marrow) may correlate with an increased likelihood of a response. These observations support a role for intracrine androgen production and persistent AR signaling in CRPC, and suggest a possible predictive indicator for response. CYP17 Inhibitors TAK-700 and TOK-001 TAK-700 and TOK-001 (formerly VN/124-1) are selective CYP17 inhibitors currently in phase I/II development (see Appendix). Preliminary phase I results with TAK-700, an oral selective C17,20-lyase inhibitor, summarized ndings with dose levels of 100 through 600 mg twice daily as well as 400 mg twice daily combined with low dose prednisone in 26 patients with metastatic CRPC.45 No dose limiting toxicity was seen. Fatigue was the most common treatment related adverse event, as seen in 16 patients (62%), including 3 with grade 3 or greater events at the 600 mg dose. Other common treatment related adverse events were nausea in 38% of cases, constipation in 35%, anorexia in 35% and vomiting in 30%. Decreases in median testosterone from 4.9 to 0.6 ng/dl and in DHEA-sulfate androstenedione from 53.8 to less than 0.1 g/dl were seen at the 400 mg dose. A blunted cortisol response after ACTH stimulation was seen in 2 of 7 patients at the 400 mg dose and in all 5 at the 600 mg dose. Doses at or above 300 mg twice daily produced a 50% or greater decrease in PSA in 11 of 14 patients (70%), of whom 4 (29%) had a 90% or greater PSA decrease. Continued phase II evaluation of TAK-700 at the 400 mg twice daily dose, including the need for concomitant prednisone, in men with metastatic CRPC is ongoing. Also, a phase II study of TAK-700 in men with nonmetastatic CRPC with increasing PSA has begun accrual. In preclinical experience TOK-001 selectively inhibited 17 -hydroxylase/C17,20-lyase activity and down-regulated AR expression.46 In the LAPC4 prostate cancer xenograft model TOK-001 combined with castration inhibited tumor growth and signi-
cantly down-regulated AR protein expression, in contrast to ndings with castration alone or bicalutamide, which showed up-regulation of AR expression. Phase I/II evaluation of TOK-001 in CRPC was initiated in late 2009.
NOVEL AR ANTAGONISTS FOR CRPC
Second Generation Antiandrogen MDV3100 AR over expression is known to be a mechanism of antiandrogen resistance in CRPC. Also, the partial agonist activity of current rst generation antiandrogens such as bicalutamide can be a factor in tumor progression. MDV3100 is a novel second generation antiandrogen that shows selective, potent afnity for AR while being devoid of any agonist AR activity in CRPC models.47 Compared to bicalutamide MDV3100 has greater binding afnity for AR. In CRPC cell lines MDV3100 effectively inhibits nuclear translocation and DNA binding to androgen response, leading to the induction of apoptosis. In tumor xenograft models known to over express AR treatment with MDV3100 led to substantial tumor regression while growth suppression was more modest. MDV3100 was clinically evaluated in a phase I/II multicenter study in 140 patients with progressive metastatic CRPC with oral dose escalations of 30 to 600 mg daily.48 The study population was relatively heavily pretreated with failure of at least 2 prior hormonal therapies in most patients, prior ketoconazole exposure in 63 (45%) and failure of at least 1 prior chemotherapy in 75 (54%). The most common treatment related adverse event with MDV3100 was fatigue, which had an onset of approximately 4 weeks with timing that corresponded to the achievement of steady-state drug concentrations. Grade 3/4 adverse events were seen predominantly at a dose of 360 mg or greater, including fatigue in 11% of patients, which generally responded to dose reduction, asthenia in 2% and seizures in 2%. Due to tolerability issues at doses above 360 mg and the potential concern for seizures a maximum tolerated dose of 240 mg was selected for sustained treatment. Efcacy was observed across all dose levels and appeared to be dose dependent, attaining a plateau at between 150 and 240 mg daily. Overall a 50% or greater PSA decrease was seen in 78 patients (56%) with objective partial responses in 13 (22%) with measurable disease. A similar 50% or greater PSA decrease was seen in patients parsed by prior chemotherapy exposure and extent of prior hormonal therapy, although a lower rate was seen in patients previously treated with ketoconazole. Overall median TTPP was 224 days (95% CI 147 to 315) with a median of 147 (95% CI 140 to 231) and 287 days (95% CI 203 to 427) in patients with and without
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
793
prior chemotherapy exposure, respectively. Also, 49% of patients with an unfavorable circulating tumor cell count (5/7.5 ml or greater) at baseline had conversion to favorable counts, of whom 19 (76%) also had a 50% or greater maximum PSA decrease. Currently MDV3100 at a dose of 160 mg is under phase III evaluation in patients with CRPC who were previously treated with docetaxel. AR Inhibitor BMS-641988 BMS-641988 is a highly potent AR inhibitor that was specically designed based on AR crystal structure.49 Compared to bicalutamide BMS-6410988 showed higher binding afnity and greater inhibition of AR mediated signaling in preclinical models. Two phase I studies of BMS-641988 in CRPC are complete but results have not yet been reported.
survival. Adaptive mechanisms, including up-regulation of AR expression and enhanced receptor sensitivity, permit tumor growth in the castrate environment. In castration resistant prostate tumor tissues the expression of enzymes involved in androgen biosynthesis suggests that these tumors may also develop intracrine signaling mechanisms. Novel agents that target CYP17 and selectively inhibit persistent androgen production show promise for CRPC treatment. Also, second generation antiandrogens such as MDV3100 offer another means to address persistent AR signaling in CRPC. Based on encouraging clinical results to date it seems likely that these new classes of agents will substantially change the treatment and clinical outlook in many men with CRPC, particularly those unwilling to accept or unable to tolerate cytotoxic chemotherapy.
CONCLUSIONS
A signicant proportion of CRPCs continue to rely on ligand mediated AR signaling for growth and
ACKNOWLEDGMENTS
Christine Gutheil and Karim Chamie assisted with the manuscript.
APPENDIX
Clinical development status of novel androgen synthesis inhibitors and second generation antiandrogens for CRPC Class/Agent Androgen biosynthesis inhibitors: Abiraterone acetete TOK-001 (formerly VN/124-1) TAK-700 Antiandrogens: MDV3100 BMS-641988 Target CYP17 (17- -hydroxylase/C17,20-lyase) CYP17 (17- -hydroxylase/C17,20-lyase), selective AR modulator CYP17 (C17,20-lyase) AR binding/nuclear translocation AR binding Phase Status III I/II I/II I/II I
REFERENCES
1. Lam JS, Leppert JT, Vemulapalli SN et al: Secondary hormonal therapy for advanced prostate cancer. J Urol 2006; 175: 27. 2. Tannock IF, de Wit R, Berry WR et al: Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 2004; 351: 1502. 3. Petrylak DP, Tangen CM, Hussain MH et al: Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med 2004; 351: 1513. 4. Berthold DR, Pond GR, Soban F et al: Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX327 study. J Clin Oncol 2008; 26: 242. 5. Pienta KJ and Bradley D: Mechanisms underlying the development of androgen-independent prostate cancer. Clin Cancer Res 2006; 12: 1665. 6. Scher HI and Sawyers CL: Biology of progressive, castration resistant prostate cancer: directed therapies targeting the androgen-receptor signaling axis. J Clin Oncol 2005; 23: 8253. 7. Bubley GJ, Carducci M, Dahut W et al: Eligibility and response guidelines for phase II clinical trials in androgen-independent prostate cancer: recommendations from the Prostate-Specic Antigen Working Group. J Clin Oncol 1999; 17: 3461. 8. Scher HI, Halabi S, Tannock I et al: Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 2008; 26: 1148. 9. Fossa SD, Slee PH, Brausi M et al: Flutamide versus prednisone in patients with prostate cancer symptomatically progressing after androgen-ablative therapy a phase III study of the European Organization for Research and Treatment of Cancer Genitourinary Group. J Clin Oncol 2001; 19: 62. 10. Small EJ, Halabi S, Dawson NA et al: Antiandrogen withdrawal alone or in combination with ketoconazole in androgen-independent prostate cancer patients: a phase III trial (CALGB 9583). J Clin Oncol 2004; 22: 1025. 11. Suzuki H, Okihara K, Miyake H et al: Alternative nonsteroidal antiandrogen therapy for advanced prostate cancer that relapsed after initial maximum androgen blockade. J Urol 2008; 180: 921. 12. Scher HI, Liebertz C, Kelly WK et al: Bicalutamide for advanced prostate cancer: the natural versus treated history of disease. J Clin Oncol 1997; 15: 2928. 13. Kassouf W, Tanguay S and Aprikian AG: Nilutamide as second line hormone therapy for prostate cancer after androgen ablation fails. J Urol 2003; 169: 1742. 14. Small EJ, Meyer M, Marshall ME et al: Suramin therapy for patients with symptomatic hormonerefractory prostate cancer results of a randomized phase III trial comparing suramin plus hydrocor-
794
NOVEL THERAPEUTIC STRATEGIES FOR CASTRATION RESISTANT PROSTATE CANCER
tisone to placebo plus hydrocortisone. J Clin Oncol 2000; 18: 1440. 15. Kantoff PW, Halabi S, Conaway M et al: Hydrocortisone with or without mitoxantrone in men with hormone-refractory prostate cancer: results of the cancer and leukemia group B 9182 study. J Clin Oncol 1999; 17: 2506. 16. Storlie JA, Buckner JC, Wiseman GA et al: Prostate specic antigen levels and clinical response to low dose dexamethasone for hormone-refractory metastatic prostate carcinoma. Cancer 1995; 76: 96. 17. Robertson CN, Roberson KM, Padilla GM et al: Induction of apoptosis by diethylstilbestrol in hormone-insensitive prostate cancer cells. J Natl Cancer Inst 1996; 88: 908. 18. Oh WK, Kantoff PW, Weinberg V et al: Prospective, multicenter, randomized phase II trial of the herbal supplement, PC-SPES, and diethylstilbestrol in patients with androgen-independent prostate cancer. J Clin Oncol 2004; 22: 3705. 19. Smith DC, Redman BG, Flaherty L et al: A phase II trial of oral diethylstilbestrol as a second-line hormonal agent in advanced prostate cancer. Urology 1998; 52: 257. 20. Kruit WH, Stoter G and Klijn JG: Effect of combination therapy with aminoglutethimide and hydrocortisone on prostate-specic antigen response in metastatic prostate cancer refractory to standard endocrine therapy. Anticancer Drugs 2004; 15: 843. 21. Figg WD, Liu Y, Arlen P et al: A randomized, phase II trial of ketoconazole plus aledronate versus ketoconazole alone in patients with androgen independent prostate cancer and bone metastases. J Urol 2005; 173: 790. 22. Small EJ, Baron A, Fippin L et al: Ketoconazole retains activity in advanced prostate cancer patients with progression despite utamide withdrawal. J Urol 1997; 157: 1204. 23. Holzbeierlein J, Lal P, LaTulippe E et al: Gene expression of human prostate carcinoma during hormonal therapy identies androgen-responsive genes and mechanisms of therapy resistance. Am J Pathol 2004; 164: 217. 24. Chen CD, Welsbie DS, Tran C et al: Molecular determinants of resistance to antiandrogen therapy. Nat Med 2004; 10: 33. 25. Linja MJ, Savinainen KJ, Saramki OR et al: Amplication and overexpression of androgen receptor gene in hormone-refractory prostate cancer. Cancer Res 2001; 61: 3550. 26. Stanbrough M, Bubley GJ, Ross K et al: Increased expression of genes converting adrenal andro-
gens to testosterone in androgen-independent prostate cancer. Cancer Res 2006; 66: 2815. 27. Gregory CW, Johnson RT, Mohler JL et al: Androgen receptor stabilization in recurrent prostate cancer is associated with hypersensitivity to low androgen. Cancer Res 2001; 61: 2892. 28. Hu R, Dunn TA, Wei S et al: Ligand-independent androgen receptor variants derived from splicing of cryptic exons signify hormone-refractory prostate cancer. Cancer Res 2009; 69: 16. 29. Puche C, Jose M, Cabero A et al: Expression and enzymatic activity of the P450c17 gene in human adipose tissue. Eur J Endocrinol 2002; 146: 223. 30. Montgomery RB, Mostaghel EA, Vessella R et al: Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castrationresistant tumor growth. Cancer Res 2008; 68: 4447. 31. Locke JA, Fazli L, Adomat H et al: Androgen levels increase by intrarumoral de novo steroidogenesis during progression of castration-resistant prostate cancer. Cancer Res 2008; 68: 6407. 32. Mohler JL, Gregory CW, Ford OH 3rd et al: The androgen axis in recurrent prostate cancer. Clin Cancer Res 2004; 10: 440. 33. Mostaghel EA, Page ST, Lin DW et al: Intraprostatic androgens and androgen-regulated gene expression persist after testosterone suppression: therapeutic implications for castration-resistant prostate cancer. Cancer Res 2007; 67: 5033. 34. Auchus RJ: The genetics, pathophysiology, and management of human deciencies of P450c17. Endocrinol Metab Clin North Am 2001; 30: 101. 35. Barrie SE, Potter GA, Goddard PM et al: Pharmacology of novel steroidal inhibitors of cytochrome P450 (17)alpha (17 alpha-hydroxylase/C17-20 lyase). J Steroid Biochem Mol Biol 1994; 50: 267. 36. Montgomery B, Mostaghel E, Nelson P et al: Abiraterone suppresses castration resistant human prostate cancer growth in the absence of testicular and adrenal androgens. Presented at American Association for Cancer Research Special Conference: Advances in Prostate Cancer Research, San Diego, California, January 2124, 2009. 37. ODonnell A, Judson I, Dowsett M et al: Hormonal impact of the 17alpha -hydroxylase/ C(17,20)-lyase inhibitor abiraterone acetate (CB7630) in patients with prostate cancer. Br J Cancer 2004; 90: 2317. 38. Attard G, Reid AHM, Yap TA et al: Phase I clinical trial of a selective inhibitor of CYP17, abiraterone acetate, conrms that castration-resistant prostate cancer commonly remains hormone driven. J Clin Oncol 2008; 28: 4563.
39. Ryan CJ, Smith MR, Fong L et al: Phase I clinical trial of the CYP17 inhibitor abiraterone acetate demonstrating clinical activity in patients with castration-resistant prostate cancer who received prior ketoconazole. J Clin Oncol 2010; 28: 1481. 40. Attard G, Reid AHM, AHern R et al: Selective inhibition of CYP17 with abiraterone acetate is highly active in the treatment of castration-resistant prostate cancer. J Clin Oncol 2009; 27: 3742. 41. Ryan C, Efstathiou E, Smith M et al: Phase II multicenter study of chemotherapy (chemo)-nave castration resistant prostate cancer (CRPC) not exposed to ketoconazole (keto), treated with abiraterone acetate (AA) plus prednisone. J Clin Oncol, suppl., 2009; 27: 15s, abstract 5046. 42. Reid AH, Attard D, Danila D et al: Signicant and sustained antitumor activity in post-docetaxel, castration-resistant prostate cancer with the CYP17 inhibitor abiraterone acetate. J Clin Oncol 2010; 28: 1489. 43. Danila DC, Morris MJ, de Bono J et al: Phase II multicenter study of abiraterone acetate plus prednisone in patients in patients with docetaxeltreated castration-resistant prostate cancer. J Clin Oncol 2010; 28: 1486. 44. Logothetis CJ, Wen S, Molina A et al: Identication of an androgen withdrawal responsive phenotype in castrate resistant prostate cancer (CRPC) patients (pts) treated with abiraterone acetate (AA). J Clin Oncol, suppl., 2008; 26: abstract 5017. 45. Dreicer R, Agus DB, MacVicar GR et al: Safety, pharmacokinetics, and efcacy of TAK-700 in castration-resistant metastatic prostate cancer: a phase I/II open label study. Genitourin Cancer Symp Proc 2010; 89: abstract 103. 46. Vasaitis T, Belosay A, Schayowitz A et al: Androgen receptor inactivation ncontributes to antitumor efcacy of 17 -hydroxylase/17,20-lyase inhibitor 3 hydroxy-17-(1H-benzimidazole-1-yl)androsta-5,16-diene in prostate cancer. Mol Cancer Ther 2008; 7: 2348. 47. Tran C, Ouk Sm Clegg NJ et al: Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science 2009; 324: 787. 48. Scher HI, Beer TM, Higano CS et al: Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1-2 study. Lancet 2010; 375: 1437. 49. Attar RM, Jure-Kunkel M, Balog A et al: Discovery of BMS-641988: a novel and potent inhibitor of androgen receptor signaling for the treatment of prostate cancer. Cancer Res 2009; 69: 6522
Вам также может понравиться
- EAU Guidelines On Urinary Incontinence 2019 PDFДокумент100 страницEAU Guidelines On Urinary Incontinence 2019 PDFTina RОценок пока нет
- EVMS Critical Care COVID-19 ProtocolДокумент49 страницEVMS Critical Care COVID-19 ProtocoljarganОценок пока нет
- Essm Newsletter: Highlights From The EditionДокумент24 страницыEssm Newsletter: Highlights From The EditionRazvan BardanОценок пока нет
- NCCN Testicular CancerДокумент78 страницNCCN Testicular CancerRazvan BardanОценок пока нет
- ShockPulse-SE Brochure en 20150312Документ3 страницыShockPulse-SE Brochure en 20150312Razvan BardanОценок пока нет
- Balkan Endemic NephropathyДокумент11 страницBalkan Endemic NephropathyRazvan BardanОценок пока нет
- Meniu Bucatarie Stadio Oct 2018 en SiteДокумент2 страницыMeniu Bucatarie Stadio Oct 2018 en SiteRazvan BardanОценок пока нет
- 7th INUM 2019 ProgrammeДокумент36 страниц7th INUM 2019 ProgrammeRazvan BardanОценок пока нет
- Cruiser ManualДокумент491 страницаCruiser ManualChristian HauganОценок пока нет
- Abstracte Razvan - PerforanteДокумент3 страницыAbstracte Razvan - PerforanteRazvan BardanОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Androgen and AntiandrogenДокумент18 страницAndrogen and AntiandrogenIrma MarianyОценок пока нет
- The 3 stages of falling in love: lust, attraction and attachmentДокумент3 страницыThe 3 stages of falling in love: lust, attraction and attachmentRenalyne Andres BannitОценок пока нет
- Hormone Levels in LoveДокумент3 страницыHormone Levels in LoveMădălina PopОценок пока нет
- Drugs Used in Disorders of Endocrine System Ppt. Book (Lectures 1-6)Документ467 страницDrugs Used in Disorders of Endocrine System Ppt. Book (Lectures 1-6)Marc Imhotep Cray, M.D.Оценок пока нет
- 3pags Nutrient TimingДокумент5 страниц3pags Nutrient TimingLucas CalleriОценок пока нет
- Big Promotion Steroids & Oil & HGH & Peptide & PillДокумент8 страницBig Promotion Steroids & Oil & HGH & Peptide & PillLeonardoAdrianPerezОценок пока нет
- Neutering in Dogs and CatsДокумент11 страницNeutering in Dogs and CatsEdgar MorenoОценок пока нет
- Hypopituitarism Deficiency GuideДокумент83 страницыHypopituitarism Deficiency GuideEdward Eid0% (1)
- Wolstenholme Et Al. (2011)Документ10 страницWolstenholme Et Al. (2011)DaBid Lopez RodriguezОценок пока нет
- Aggression - Biological Factors Agresi - Faktor BiologisДокумент11 страницAggression - Biological Factors Agresi - Faktor BiologisArio TuwondilaОценок пока нет
- Males With Androgen DeficiencyДокумент28 страницMales With Androgen DeficiencyVicki NottОценок пока нет
- Effects of Steroid Hormones On Brain: GlossaryДокумент6 страницEffects of Steroid Hormones On Brain: GlossaryAnonymous droqJBqu6Оценок пока нет
- Natural Penis Enlargement Volume 2Документ143 страницыNatural Penis Enlargement Volume 2MJ0% (1)
- Anabolic Steroids - Cynthia KuhnДокумент25 страницAnabolic Steroids - Cynthia KuhnX-ON FITNESSОценок пока нет
- Anabolic Peptide Beta EbookДокумент226 страницAnabolic Peptide Beta EbookMatei Cipri80% (5)
- Advanced Prostate FormulaДокумент16 страницAdvanced Prostate FormulaDean Sole50% (2)
- Gonadal Hormones and InhibitorsДокумент10 страницGonadal Hormones and InhibitorsCarlos NiñoОценок пока нет
- The Ultimate Sex StackДокумент15 страницThe Ultimate Sex StackAngelo100% (1)
- Dr. Syafrizal Syafei Basic Principle and Administration of Hormonal and Intgreated Therapy in CancerДокумент28 страницDr. Syafrizal Syafei Basic Principle and Administration of Hormonal and Intgreated Therapy in CancerWilliamRayCassidyОценок пока нет
- Hormones of The GonadsДокумент17 страницHormones of The GonadsSophia AgenyiОценок пока нет
- Spironolactone-Induced Unilateral GynecomastiaДокумент3 страницыSpironolactone-Induced Unilateral GynecomastiaLabontu IustinaОценок пока нет
- Drjockers Com Best Aromatase Inhibiting FoodsДокумент29 страницDrjockers Com Best Aromatase Inhibiting FoodsgareththomasnzОценок пока нет
- Greatest SexДокумент94 страницыGreatest SexPaulo Marcondes50% (12)
- Bao Swaab 2011Документ13 страницBao Swaab 2011BeatrizCamposОценок пока нет
- A Guide To Testosterone: Boost Levels Through Diet And SupplementsДокумент5 страницA Guide To Testosterone: Boost Levels Through Diet And SupplementsNick Graham TrinhОценок пока нет
- The Anabolic Handbook - 1st EditionДокумент489 страницThe Anabolic Handbook - 1st EditionNguyễn Bảo MinhОценок пока нет
- JSM 19 1 144Документ14 страницJSM 19 1 144Amo Bogotano DuroОценок пока нет
- Hormone Diet PlanДокумент21 страницаHormone Diet Plancarlos100% (2)
- Digit Ratio (2D-4D) Profile of Varsity Rugby Players (Mohd Zulkhairi Mohd Azam) PP 103-107Документ5 страницDigit Ratio (2D-4D) Profile of Varsity Rugby Players (Mohd Zulkhairi Mohd Azam) PP 103-107upenapahangОценок пока нет
- The+TOT+Bible+Email 1520807089087 PDFДокумент598 страницThe+TOT+Bible+Email 1520807089087 PDFluiszertucheОценок пока нет