Академический Документы
Профессиональный Документы
Культура Документы
Cytotoxic Edema
Загружено:
Dinly JoyИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cytotoxic Edema
Загружено:
Dinly JoyАвторское право:
Доступные форматы
Cellular Injury During Ischemia
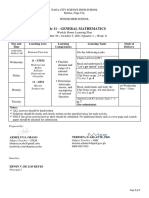
Edema Formation Ischemic brain edema is a combination of two major types of edema: cytotoxic (cellular) and vasogenic [Fishman RA. Cerebrospinal Fluid in Diseases in the Nervous System. 2nd Ed. Philadelphia, PA: W.B. Saunders Co; 1992:103-155]. Cytotoxic edema evolves over minutes to hours and may be reversible, while the vasogenic phase occurs over hours to days, and is considered an irreversibly damaging process. Cytotoxic edema is characterized by swelling of all the cellular elements of the brain (shown). In the presence of acute cerebral ischemia, neurons, glia (indicated by astrocytes), and endothelial cells swell within minutes of hypoxia due to failure of ATP-dependent ion (sodium and calcium) transport. With the rapid accumulation of sodium within cells, water follows to maintain osmotic equilibrium. Increased intracellular calcium activates phospholipases and the release of arachidonic acid, leading to the release of oxygen-derived free radicals and infarction. Vasogenic edema (not shown) is characterized by an increase in extracellular fluid volume due to increased permeability of brain capillary endothelial cells to macromolecular serum proteins (e.g., albumin). Normally, the entry of plasma protein-containing fluid into the extracellular space is limited by tight endothelial cell junctions, but in the presence of massive injury there is increased permeability of brain capillary endothelial cells to large molecules. Vasogenic edema can displace the brain hemisphere and, when severe, lead to cerebral herniation. Acute hypoxia initially causes cytotoxic edema, followed within the next hours to days by the development of vasogenic edema as infarction develops (Fishman, 1992). The delayed onset of vasogenic edema suggests that time is needed for the defects in endothelial cell function and permeability to develop.
Cellular Injury During Ischemia
Deterioration of Ion Gradients Inadequate energy supply leads to deterioration of ion gradients. Anoxic depolarization (equilibration of intracellular and extracellular ions) causes potassium to leave the cell and sodium, chloride, and calcium ions to enter. It also stimulates the massive release of the amino acids glutamate and aspartate, excitatory neurotransmitters in the brain. Glutamate further activates sodium and calcium ion channels in the neuron membrane. As sodium and calcium ions rapidly accumulate within the cells, accompanied by an inflow of water, cytotoxic edema causes rapid swelling of neurons and glia.
Activation of calcium channels results in further influx of calcium into the cell. One of the most intensely studied calcium channels is the N-methyl-D aspartate (NMDA) channel.
Consequences of Calcium Overload Entry of calcium through the NMDA (and similar channels) can be devastating. First, attempts to get rid of the excess calcium use up already scarce supplies of ATP. Second, excessive calcium influx causes the disordered activation of a wide range of enzyme systems (proteases, lipases, and nucleases). These enzymes and their metabolic products, such as oxygen free radicals, damage cell membranes, genetic material, and structural proteins in the neurons, ultimately leading to cell death. This sequence of events has been termed excitotoxicity because of the pivotal role of excitatory amino acids such as glutamate. Several agents are under investigation to block these steps.
The Ischemic Penumbra Within the ischemic cerebrovascular bed, there are two major zones of injury: the core ischemic zone and the "ischemic penumbra" (the term generally used to define ischemic but still viable cerebral tissue). In the core zone, which is an area of severe ischemia (blood flow below 10% to 25%), the loss of inadequate supply of oxygen and glucose results in rapid depletion of energy stores. Severe ischemia can result in necrosis of neurons and also of supporting cellular elements (glial cells) within the severely ischemic area.
Brain cells within the penumbra, a rim of mild to moderately ischemic tissue lying between tissue that is normally perfused and the area in which infarction is evolving, may remain viable for several hours. That is because the penumbral zone is supplied with blood by collateral arteries anastomosing with branches of the occluded vascular tree (see inset). However, even cells in this region will die if reperfusion is not established during the early hours since collateral circulation is inadequate to maintain the neuronal demand for oxygen and glucose indefinitely. In this example, the ischemic penumbra is shown as a rim of tissue surrounding the severely ischemic core lying within the vascular territory of the pre-Rolandic branch of the left middle cerebral artery. The Rolandic artery is occluded by a thromboembolus. The extent of the penumbra varies directly with the number and patency of collateral arteries. The penumbra is where pharmacologic interventions are most likely to be effective. However, it may also be possible to salvage cells within the severely ischemic core zone. Although severe ischemia kills selectively vulnerable neurons, glial cells may be spared if blood flow is restored early. Therefore, timely recanalization of the occluded vessel should theoretically restore perfusion in both the penumbra and in the severely ischemic core. Partial recanalization should markedly reduce the size of the penumbra as well.
Cerebral Infarction / Effects of Edema Shown is a brain slice viewed from the back following a stroke. Blood flow to the region on the left was interrupted due to a thrombus or embolus. The lack of blood flow resulted in severe damage (infarct) to some of the brain tissue. The infarcted tissue caused fluids to accumulate (edema) and result in swelling. The center of the brain is shifted to the right due to swelling from the left. The rigid container of the cranium allows limited room for expansion, and any condition that causes an increase in volume of one or more structures within this vault will cause an increase in intracranial pressure (ICP) or will shift one compartment of the brain, thereby compressing others. As the pressure increases, the brain shifts or is distorted, compressing neurons, nerve tracts, and cerebral arteries. A sustained increase in pressure causes persistent ischemia, irreversible damage to brain cells, and potentially death.
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- MATH3161 MATH5165 T1 2023 OutlineДокумент10 страницMATH3161 MATH5165 T1 2023 OutlineDouglusОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Noli Me Tangere CharactersДокумент4 страницыNoli Me Tangere CharactersDiemОценок пока нет
- Creativity and AestheticДокумент17 страницCreativity and AestheticSyahirah Erahzs100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Attitudes and Attitude ChangeДокумент19 страницAttitudes and Attitude Changeprajwal-athrey-3069Оценок пока нет
- STRUCTURAL CONVERSION Examples PDFДокумент5 страницSTRUCTURAL CONVERSION Examples PDFGerard Salmoral ParramonОценок пока нет
- (2016) The Role of Requirements in The Success or Failure of Software Projects-DikonversiДокумент11 страниц(2016) The Role of Requirements in The Success or Failure of Software Projects-DikonversiFajar HatmalОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Muslimah's Handbook of PurityДокумент60 страницMuslimah's Handbook of PurityMuadh KhanОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Chapter 1Документ13 страницChapter 1Jerard AnciroОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Draft Cavite MutinyДокумент1 страницаDraft Cavite MutinyaminoacidОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- MAT 120 NSU SyllabusДокумент5 страницMAT 120 NSU SyllabusChowdhury_Irad_2937100% (1)
- Spotify Strategig Possining and Product Life Cycle Four Basic Stages.Документ5 страницSpotify Strategig Possining and Product Life Cycle Four Basic Stages.Jorge YeshayahuОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Figures of Speech StylisticsДокумент11 страницFigures of Speech StylisticsCarmie Lactaotao DasallaОценок пока нет
- News StoryДокумент1 страницаNews StoryRic Anthony LayasanОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- CIR v. San Roque Power Corp., G.R. No. 187485, February 12, 2013Документ8 страницCIR v. San Roque Power Corp., G.R. No. 187485, February 12, 2013samaral bentesinkoОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Chairperson 2012 Bar Examinations Committee: Bar Exam Question 2012 Martin S. Villarama, JRДокумент73 страницыChairperson 2012 Bar Examinations Committee: Bar Exam Question 2012 Martin S. Villarama, JRsejinma0% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Per User Guide and Logbook2Документ76 страницPer User Guide and Logbook2Anthony LawОценок пока нет
- Prejudicial QuestionДокумент1 страницаPrejudicial QuestionlmafОценок пока нет
- General Mathematics - Module #3Документ7 страницGeneral Mathematics - Module #3Archie Artemis NoblezaОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- "Article Critique" Walden University Methods For Evidence-Based Practice, Nursing 8200 January 28, 2019Документ5 страниц"Article Critique" Walden University Methods For Evidence-Based Practice, Nursing 8200 January 28, 2019Elonna AnneОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- MIS Tutorial 4 AnswerДокумент8 страницMIS Tutorial 4 AnswerChia Kong Haw0% (1)
- Metric Schnorr Lock Washer SpecДокумент3 страницыMetric Schnorr Lock Washer SpecGatito FelinoОценок пока нет
- Thompson VarelaДокумент18 страницThompson VarelaGiannis NinosОценок пока нет
- Wulandari - Solihin (2016)Документ8 страницWulandari - Solihin (2016)kelvinprd9Оценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Code of Conduct of Dabur Company - 1Документ5 страницCode of Conduct of Dabur Company - 1Disha KothariОценок пока нет
- 4th Quarter Grade 9 ExamДокумент4 страницы4th Quarter Grade 9 ExamAnnie Estaris BoloОценок пока нет
- Reported Speech Rd1Документ3 страницыReported Speech Rd1Jose ChavezОценок пока нет
- TENSES ExerciseДокумент28 страницTENSES ExerciseKhanh PhamОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Birth and Growth of Semiotics: November 2020Документ9 страницBirth and Growth of Semiotics: November 2020Maria del Carmen Alvarado AcevedoОценок пока нет
- Slides - Simple Linear RegressionДокумент35 страницSlides - Simple Linear RegressionJarir AhmedОценок пока нет
- Beed 3a-Group 2 ResearchДокумент65 страницBeed 3a-Group 2 ResearchRose GilaОценок пока нет