Академический Документы
Профессиональный Документы
Культура Документы
Antiviral Onward
Загружено:
Gene WinterwoodИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Antiviral Onward
Загружено:
Gene WinterwoodАвторское право:
Доступные форматы
ANTI - VIRAL More difficult to treat than bacterial infections because virus depends on
biochemical processor of the host cells for its replication
Drugs that interfere with virus may also damage cells MOA: inhibit viral replication by interfering viral nucleic acid synthesis in the cell
I. Agents for Influenza and Respiratory Viruses amantadine (Symmetrel) - PO oseltamivir (Tamiflu) - PO ribavirin (Virazole) aerosol inhalation rimantidine (Flumadine) - PO zanamivir (Relenza) inhaler CI: allergy, pregnancy & lactation,renal & liver disease AE: lightheadedness, dizziness, insomia, nausea, orthostatic hypotension, & urinary retention DI: with anti cholinergic drugs = increase atropine like effect Nursing Considerations: Start regimen as soon after the exposure to the virus as possible (achieve best effectiveness and decrease the risk of complications) Administer the full course of drug Provide safety measures ( protect patient from injury) II. Agents for Herpes Herpesviruses Herpes simplex virus type 1 HSV2 HSV3: Varicella- zoster (chickenpox or shingles) HSV 4: Epstein Barr virus CMV: cytomegalovirus
acyclovir (Zovirax) , famciclovir (Famvir), valacyclovir (Valtrex)- = herpes; PO cidofovir (Vistide) - IV= CMV in AIDS foscarnet (Foscavir) = both; IV ganciclovir (Cytovene) = long term treatment & prevention of CMV; IV
CI: CNS disorders, allergy, pregnancy & lactation, renal disease SE: N/V, HA, depression, rash, hair loss, inflammation & burning sensation at the site of injection and topical AE: renal dysfunction DI: + other nephrotoxic meds= inc toxicity + zidovudine= inc drowsiness TOPICAL ANTIVIRALS (HSV)
idoxuridine Penciclovir Trifluridine
Nursing Considerations: Extreme caution to children ( carcinogenic); foscarnet ( affect bone growth & development) Good hydration ( decrease toxic effects o the kidney) Administer as soon as possible, compliance
Wear protective gloves when applying the dug topically ( decrease risk of exposure to the drug and inadvertent absorption) Safety precautions = CNS effects( orientation, siderails, lighting, assistance) Warn that GI upset, N/V can occur (prevent undue anxiety, increase awareness of the importance of nutrition) Monitor renal function Avoid sexual intercourse if with genital herpes Avoid driving and hazardous tasks if with dizziness & drowsiness
Agents for HIV & AIDS Enzymes needed by viruses: Reverse transcriptase helps uncoat the virus; single stranded viral RNA is converted into DNA Integrase- helps viral DNA migrates into the nucleus of the cell, where I is spliced into the host DNA (provirus) => duplicated together with the cell genes every time the cell divides Protease- assists in the assemble of newly formed viral particles
ANTIRETROVIRAL THERAPY
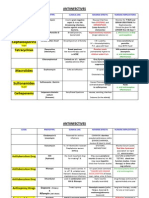
A. Reverse Transcriptase Inhibitors Nucleoside Analogues (NRTI) Nonnucleoside Analogues (NNRTI) B. Protease Inhibitors C. Entry Inhibitors A. Nucleoside/ Nucleotide Reverse Transcriptase Inhibitors (NRTIs) MOA: blocks the reverse transcriptase enzyme needed for viral replicaation zidovudine (Retrovir) didanosine (Videx) stavudine (Zerit) lamivudine (Epivir) abacavir (Ziagen) tenofovir (Viread) emtricitabine (Emtrive) Fixed dose: lamivudine/zidovudine (Combivir)
abacavir/ lamivudine/ zidovudine (Trizivir) abacavir/ lamivudine (Epzicom) efavirenz/ emtricitabine/ tenofovir (Atripla) emtricitabine/ tenofovir (Truvasa)
SE (less tenofovir renal toxicity) GI: nausea, diarrhea, abdominal pain (transient 2 weeks) Mitochondrial toxicity: lactic acidosis, peripheral neuropathy, myopathy, pacreatitis, lipoatrophy (wasting of fats in face, buttocks and extemities)
Nursing Considerations: Should be taken with food except didanosine (60 min AC or 2 hours PC) Requires dosage adjustment except abacavir (creatinine clearance < 50mL/min) Fixed dose avoided if with renal insufficiency A. Non- nucleoside Reverse Transcriptase Inhibitors (NNRTIs) MOA: prevent viral replication by competing with binding of the revere transcriptase enzyme at the active site Used to reserve protease inhibitors (resistance) efavirenz (Sustiva) First-choice drug PC: D CNS toxicities: dizziness, sedation, nightmares, euphoria, loss of concentration Administered as a component of Atripla OD @ HS Empty stomach / low fat meal (prevent excessive drug absorption)
nevirapine ( Viramune) alternative: Pregnancy (1st tri) Planning to conceive Not using effective/ consistent contraception < risk: rash hepatotoxicity delavirdine (Rescriptor) Least potent antiviral activity Not recommended as part of regimen
B. Protease Inhibitors MOA: act at the end of the HIV cycle to inhibit the production of infectious HIV virus lopinavir/ ritonavir (first line) atazanivir fosamprenavir (second either boosted with retonavir or not) amprenavir tipranavir darunavir saquinavir indinavir ritonavir nelfinavir NOTE:
Ritonavir boosting mainstay of PI therapy (potent inhibitory effect) Take with food + didanosine = one hr before or two hours after ritonavir
C. Entry Inhibitors
MOA: prevents HIV cell entry (fusion of HIV and CD4) enfuvirtide the only agent approved Indicated in combination with 3-5 other anti- retroviral agents (for clients with limited tx option) Expensive. 90 mg Sub-Q. BID Injection site reaction: Suncutaneous nodules, redness Others: rash. Diarrhea, serous allergic reaction (anaphylaxis)
ANTIHELMINTICS
Helminthes are large organisms (parasitic worms) that feed through the host tissue Intestine, lymphatic system, blood vessel and liver MOA: act on metabolic pathways that are present in the invading worm but absent or significantly different from human host 4 groups: Cestodes ( tapeworms) Trematodes (flukes) Intestinal nematodes ( roundworm) tissue invading nematodes
pyrantel pamoate (Combatrin) Paralysis the intestinal tract of the worm Indication: giant roundworm, hookworm, pinworm mebendzole ( Antiox) Inhibits glucose and other nutrients of helminthes Indication: roundworm, pinworm, hookworm, whipworm thiabendazole (Mintozol) Interfere in parasitic metabolism Indication: roundworm, pinworm praziquantel (Biltrizide) Paralyzes the worm tapeworm SE: HA, dizziness, fever, chills and malaise, rash, pruritus, loss of hair NURSING CONSIDERATIONS: Take drug with food, small frequent feeding Avoid driving, change position slowly Take drug as prescribed Inform health care provider about OTC meds taking For intestinal infection, some measures that help prevent worm reinfection or help prevent spread to other family members: Vigorous use of soap and water after use of toilet Showering in the morning to wash away any ova deposited in the anal area during the night Changing and laundering undergarments, bed linens and pajama daily Disinfecting toilet & toilet seats, bathroom and bedroom floors periodically Proper handling of food and food preparation Control flies Avoid sexual intercourse or use condom in with vaginal infection
ANTI- FUNGALS ( anti- mycotics)
An infection caused by fungus mycosis
Fungi differ from bacteria in that the fungus has a rigid cell wall that is made up of chitin and various polysaccharides and a membrane that contains ergosterol ( makes them resistant to antibiotics) Treatment for systemic (candidiasis, histoplasmosis) and superficial (tinea pedis/ athletes foot
I. Polyenes A. amphotericin B (Fungizone) MOA: binding to the fungal cell membrane; forming open channels >> increase cell permeability and leakage of intracellular components. Very potent but with many unpleasant side effects (renal failure) DOC: severe systemic infection; IV SE/ AD: fever, N/V, dec BP, paresthesia, thrombophlebitis, nephrotoxicity, hypersensitivit, electrolyte imbalance (hypokalemia & hypomagnesemia)
B. nystatin ( Mycostatin) MOA: increases permeability of fungal cell membrane Oral preparation- intestinal candidiasis, poorly absorb in GIT Suspension mouth or throat fungal infection Oitment, suppository, cream- vaginal SE: fever, N/V, rash, diarrhea (large dose) ***** swish>> gargle>>swallow
II. Azole Group MOA: interfere with the formation of ergosterol (major sterol in fungal cell membrane) ketoconazole (Nizoral) First effective antifungal orally absorbed Used to treat same mycoses with amphotericin B (give with food; no antacid) Shampoo= dandruff SE: diziness, blurred vision AE: hepatomegaly ; photosensitivity itraconazole (Sporanox) Systemic fungal infection; also PO miconazole (Monistar) Oitment vaginitis; IV- fungal bladder infection fluconazole (Diflucan) Oropharyngeal and systemic; hepatotoxic; also PO Voriconazole Posaconazole *****NOTE: vaginal tablet, cream, ointment and solution (topical preparation to treat candidiasis and tinea infections)
III. Antimetabolite MOA: disrupts fungal DNA and RNA synthesis flucytosine (Ancoban)- combination therapy NURSING CONSIDERATIONS ( anti fungal): GS/CS, compliance, monitor IV sites, liver & renal function tests For topical: wash hands before & after application For athletes foot: wear cotton socks, change 2-3 times daily Jock itch worm: wear well fitting, non constrictive, ventilated clothing Intravaginal Read instructions carefully Insert high into the vagina Continue use through menstruation Wear a minipad to avoid staining clothing, do not use tampon Wash applicator with mild soap and rinse thoroughly after each use Avoid sexual intercourse while using the drug
ANTIMALARIAL Malaria- cause by protozoan parasites (plasmodium falciparum, malariae, vivax,
ovale)
Causes RBC deformity and increase fragility and decrease oxygen transport
Mx: fever, chills, sweating, anemia, spleenomegaly, hepatomegaly, malaise chloroquine HCL (Aralen) The mainstay of anti malarial therapy MOA: enters human RBC and changes the metabolic pathways necessary for the reproduction of plasmodium SE: GI upset, fatigue AE: blurring of vision, blindness, ototoxicity Other drugs: Quinine sulfate chloroquine resistant malaria Primaquine, mefloquine
ANTIPARASITC (DERMA) Eg; Pediculosis lice infection (head, body, pubic) Scabies caused by sarcopte scabie, characterized by: eruptive lesion from
burrowing of the female parasite, transmitted through direct contact with skin, clothing and bedding lindane ( Kwell) MOA: unknown, thought to stimulate the parasites CNS leading to seizure and death SE: local skin irritation AE: hypersensitivity NURSING CONSIDERATIONS: Administer twice ( 1st immediately after dx; 2nd one week after the initial) Administer to all household members Wear gloves to remove nits by using fine- tooth comd with vinegar Apply to all body area except face
ANTIPROTOZOAL Use to treat:
amebiasis (E. histolytica) N/V, diarrhea, abdominal cramping and weakness trichomoniasis (T. vaginalis)- reddened inflamed vaginal mucosa, burning itching and yellowish- green discharge
metronidazole (Flagyl) MOA: inhibits DNA synthesis, bactericidal USES: DOC for intestinal and systemic amebiasis; prophylaxis fro abdominal and colorectal surgery, H. pylori and trichomoniasis SE: N/V, diarrhea, unpleasant taste AE: HA, dizziness, ataxia, superinfection NURSING CONSIDERATIONS: Avoid alcohol (disulfiram like reaction = nausea, flushing, tachycardia, increase vomiting Protected sex, proper hygeine, proper foOD preparation
ANTITUBERCULOSIS
A. Isoniazid (INH) MOA: affects the mycolic acid coating the bacterium Hepatic enzyme elevation, peripheral neuropathy (as it competes with absorption of Vitamin B6 or pyridoxine) Take AC 10-50mg pyridoxine as prophylaxis, 50-100mg as treatment B. Rifampicin MOA: alters DNA and RNA activity in the bacterium Orange discoloration of secretion and urine Best taken empty stomach but causes gastric irritation hence should be taken with food (also at bedtime) Protect drug from light C. Pyrazinamide (PZA) Both bactericidal & bacteriostatic Hepatotoxic, ototoxic, nephrotoxic, GI upset May lead to hyperuricemia, arthralgia Protect drug from light D. Ethambutol (Myobutol) MOA: inhibits cellular metabolism Lead to optic neuritis (affect the red green discrimination), skin rash Not given to children 6 years or younger because cannot reliably monitor vision Nursing Considerations Refer the following: Jaundice (ALL) Visual impairment (ethambutol) Tinnitus & hearing impairment (streptomycin) Oliguria & albuminuria (streptomycin & rifampicin) Psychosis & convulsion (INH) Thrombocytopenia & anemia (rifampicin) DRUGS FOR URINARY TRACT DISEASE Urinary Tract Antiseptics / anti infectives Urinary analgesics Urinary stimulants Urinary antispasmodics
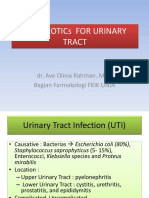
I. Urinary Tract Antiseptics/ Anti-infectives
nitrofurantoin (Macrodantin) MOA: interferes with CHON metabolism, bactericidal (high doses) Spectrum: Broad esp E- coli Uses: acute & chronic UTI CI: hypersensitivity, renal dse, pregnant, lactating DI: dec absorption if with antacid SE: NAVDA Dizziness ( institute safety measures) Rust/brown urine (harmless/ inc OFI) Staining of teeth ( do not crush tablets, dilute suspension, rinse mouth) AE: peripheral neuropathy, agranulocytosis, hemolytic anemia, superinfection, hepatotoxicity
methanamine (Hiprex) MOA: in the presence of acidic urine (pH < 5.5) converted to formaldehyde = bactericidal Uses: chronic UTI DI: inc crystalluria if taken with sulfonamides Dec if taken with NaHCO3
SE: NAVDA, dizziness AE: allergic reaction to dye, Crystalluria; HA. Nervousness, confusion
Nursing Considerations: GS/CS before therapy Take with food Comply compliance Increase OFI; UO and SG. Report dec UO Acidify urine ( cranberry juice, vitamin C/ ascorbic acid) Avoid alkaline foods ( milk, vegetables, antacids, NaHCO3) Dont use clinitest for glucose testing In additon women should: Avoid bubble baths, pantiliners, scented tissue Wipe from front to back Void after coitus, void whenever with urge
II. Urinary Analgesics
phenazopyridine HCL (Pyridium) An azo dye excreted in the urine MOA: provides a topical analgesic effect to the urinary tract within 30 mins Uses: releives mx of UTI ( pain, burning sensation, frequency & urgency of urination) SE: red- orange urine (harmless); NAVDA; vertigo, rash AE: hemolytic anemia; thrombocytopenia; leukopenia; hepato/ nephrotoxicity Nursing Considerations: Check the underlying cause of pain Caution that reddish orange urine may occur, permanently stain clothing, tears will stain contact lenses Take with food / milk to decrease gastric distress Stop drug if sclera turn yellow (a sign of drug accumulation) Treatment should not exceed 2-3 days ( inc toxic effects) Can alter glucose urine test
III. Urinary Stimulants
Used when bladder function is decreased or lost as a result of: Neurogenic bladder ( dysfunction caused by lesion of nerve) Spinal cord injury Severe head injury ===== urinary retention DOC: bethanecol chloride (Urecholine) MOA: direct acting parasympathomimetic (cholinomimetic) L/T contraction of detrusor muscle and relaxation of sphincter L/T urination May stimulate gastric motility
SE: flushing of skin & headache ( vasodilation) AE: flushing, increase sweating, colicky pain, abdominal cramps, diarrhea, increase salivation, involuntary defecation, bradycardia, hypotension, cardiac arrest ANTIDOTE: atropine sulfate
Nursing Considerations: Monitor VS, ECG Administer on an empty stomach to decrease N/V, bathroom facilities stay in cool environment, use lightweight clothing (flushing & sweating)
IV. URINARY ANTISPASMODICS
AKA: antimuscarinics MOA: blocks parasympathetic activity L/T relaxing the detrusor muscle Uses: relief urinary tract spasm d/t UTI / trauma
CI: obstructive urinary tract problem, glaucoma, myasthenia gravis, acute hemorrhagic / GI obstruction SE: N/V, dry mouth, constipation, dizziness, nervousness, visual changes, Increase BP, tachycardia, increase IOP AE: urinary retention, hepato/ nephrotoxicity, photosensitivity
propantheline bromide (Pro- banthine) oxybutynin (Ditropan)- increase bladder capacity and decreases frequency of voiding in neurogenic bladder tolterodine (Detrol) inhibits bladder contraction, decreases detrusor muscle pressure, delays the urge to void flavoxate (Uripas)- counteract spasm in smooth muscle dimethylsulfoxide (DMSO)
Nursing Considerations Arrange for the treatment of the underlying cause Arrange for an opthalmological examination, institute safety measures Monitor and manage constipation, dry mouth, Assess changes in VS
Вам также может понравиться
- Anti - Viral: Topical Antivirals (HSV)Документ2 страницыAnti - Viral: Topical Antivirals (HSV)Charlie AbagonОценок пока нет
- Antimicrobials BPN: CH 46Документ11 страницAntimicrobials BPN: CH 46Shawn McMahonОценок пока нет
- Topic 2.1: Antibiotics: Unit 2: Anti-Infective MedicationsДокумент50 страницTopic 2.1: Antibiotics: Unit 2: Anti-Infective MedicationsNirali ParmarОценок пока нет
- Urinary Germicides PharmaДокумент11 страницUrinary Germicides PharmaMaria Pina Barbado PonceОценок пока нет
- Common Antibiotics Master List: Rodney Paullus Dewight Cowley Izzy Winestone Ben BowmanДокумент20 страницCommon Antibiotics Master List: Rodney Paullus Dewight Cowley Izzy Winestone Ben BowmanMahendra VermaОценок пока нет
- Immunologic DrugsДокумент12 страницImmunologic DrugsPamela Ria HensonОценок пока нет
- Farmakologi AntiparasitДокумент119 страницFarmakologi AntiparasitFitri Sri WulandariОценок пока нет
- 1 AntibioticsДокумент144 страницы1 AntibioticsRhomizal MazaliОценок пока нет
- Agents For Influenza A and Respiratory VirusesДокумент10 страницAgents For Influenza A and Respiratory VirusesTrixia RodulfaОценок пока нет
- Anti-Infectives Part 1Документ9 страницAnti-Infectives Part 1edle maeОценок пока нет
- AntibioticsДокумент31 страницаAntibioticsAkash SrivastavaОценок пока нет
- Antiviral: Anggelia Puspasari, MD Dept. Pharmacology and Therapeutic Medical Faculty University of JambiДокумент27 страницAntiviral: Anggelia Puspasari, MD Dept. Pharmacology and Therapeutic Medical Faculty University of JambiLiana Ika SuwandyОценок пока нет
- Antibiotics 11.05.19Документ18 страницAntibiotics 11.05.19dahiphale1Оценок пока нет
- Anthelmintic - Antiviral & Antiprotozoal Drugs Anthelmintic - Antiviral & Antiprotozoal DrugsДокумент39 страницAnthelmintic - Antiviral & Antiprotozoal Drugs Anthelmintic - Antiviral & Antiprotozoal DrugsAhmed AmgedОценок пока нет
- Pharmacology of Antiparasit DrugsДокумент40 страницPharmacology of Antiparasit Drugsakun scribОценок пока нет
- Farmakologi Obat Kusta Dan Antiparasit 2015Документ84 страницыFarmakologi Obat Kusta Dan Antiparasit 2015Alex FerdinandОценок пока нет
- AntibioticsДокумент30 страницAntibioticsRoza RahbeniОценок пока нет
- Nnrtis: Nonnucleoside Reverse Trancriptase InhibitorsДокумент12 страницNnrtis: Nonnucleoside Reverse Trancriptase InhibitorsMalueth AnguiОценок пока нет
- Unit 9 Drugs To Know: Penicillin (Amoxicillin), Cephalosporin, Macrolides (Azithromycin), AminoglycosidesДокумент8 страницUnit 9 Drugs To Know: Penicillin (Amoxicillin), Cephalosporin, Macrolides (Azithromycin), AminoglycosidestriciaОценок пока нет
- Modes of TransmissionДокумент5 страницModes of TransmissionMaheen IdreesОценок пока нет
- Pharma Finals Part 1Документ11 страницPharma Finals Part 1zyyw.abello.uiОценок пока нет
- FTX Infeksi JamurДокумент64 страницыFTX Infeksi JamurNafisah SofiaОценок пока нет
- Antiinfectives Drug TableДокумент5 страницAntiinfectives Drug Tablecdp1587100% (3)
- Anti Fungal Drugs: Example: CandidiasisДокумент4 страницыAnti Fungal Drugs: Example: Candidiasiskaren carpioОценок пока нет
- A Drug Study On: Monaliza J. Lee, RN, MNДокумент6 страницA Drug Study On: Monaliza J. Lee, RN, MNJeah Bearl AbellarОценок пока нет
- Acquired Immunodeficiency Syndrome (Aids) : Etiology: Human Immunodeficiency Virus (HIV) InfectionДокумент38 страницAcquired Immunodeficiency Syndrome (Aids) : Etiology: Human Immunodeficiency Virus (HIV) InfectionDhian HidayatОценок пока нет
- Antibiotics Antiviral Antifungal Antimalarial Antiseptic & Disinfectant Agents Antiinflammatory & AntirheumaticДокумент69 страницAntibiotics Antiviral Antifungal Antimalarial Antiseptic & Disinfectant Agents Antiinflammatory & AntirheumaticNop PiromОценок пока нет
- Antivirus: Wening Sari, DR., M, KesДокумент39 страницAntivirus: Wening Sari, DR., M, KesruuweelscribdОценок пока нет
- Antiviral: Anggelia Puspasari, MD Dept. Pharmacology and Therapeutic Medical Faculty University of JambiДокумент30 страницAntiviral: Anggelia Puspasari, MD Dept. Pharmacology and Therapeutic Medical Faculty University of JambieldiОценок пока нет
- Antifungaldrugs 150519204813 Lva1 App6892Документ54 страницыAntifungaldrugs 150519204813 Lva1 App6892Jennifer S ZiegenОценок пока нет
- Ampicillin:: Treatment of The Following Infections: Skin and Skin Structure Infections, Soft-TissueДокумент1 страницаAmpicillin:: Treatment of The Following Infections: Skin and Skin Structure Infections, Soft-TissueGeorge FogОценок пока нет
- AntibioticsДокумент56 страницAntibioticstintinОценок пока нет
- Leptospirosis Case Study (Short)Документ16 страницLeptospirosis Case Study (Short)Liryc Ernest CuerboОценок пока нет
- Acute Infectious Diarrheal Diseases and Bacterial Food PoisoningДокумент32 страницыAcute Infectious Diarrheal Diseases and Bacterial Food PoisoningVenkatesh GarikapatiОценок пока нет
- PharmaДокумент16 страницPharmaPaula Grace MorfeОценок пока нет
- Ciprofloxacin Drug StudyДокумент2 страницыCiprofloxacin Drug StudyRosalie Delfin89% (9)
- Chapter - Iii Antimalarial, Antiprotozoal and Anthelmintic DrugsДокумент28 страницChapter - Iii Antimalarial, Antiprotozoal and Anthelmintic DrugsNEHA DIXITОценок пока нет
- RocephinДокумент2 страницыRocephinianecunar100% (2)
- Pharmacology Final ExamДокумент71 страницаPharmacology Final ExamSavanna ChambersОценок пока нет
- 2021 BSN PHARMA Antivirals Antimalarials AnthelminticsДокумент150 страниц2021 BSN PHARMA Antivirals Antimalarials AnthelminticsKarl EstradaОценок пока нет
- Antiviral DrugsДокумент75 страницAntiviral DrugsluamsmarinsОценок пока нет
- Compilation of Antiviral Drug Leaflets: Project in PharmacologyДокумент32 страницыCompilation of Antiviral Drug Leaflets: Project in PharmacologydaleascabanoОценок пока нет
- Bousquet-Melou Metaphylaxis Aavm 2010Документ32 страницыBousquet-Melou Metaphylaxis Aavm 2010vindhyОценок пока нет
- Invanz (Ertapenem)Документ2 страницыInvanz (Ertapenem)E100% (1)
- Czarina Drug Study JuneДокумент20 страницCzarina Drug Study JuneNicoh AvilaОценок пока нет
- Anthelmentics Version 2Документ21 страницаAnthelmentics Version 2N Gv FcОценок пока нет
- Antifungal Drugs 3Документ54 страницыAntifungal Drugs 3Mikee MeladОценок пока нет
- DR - Saleh-26 March 2013-Farmakologi (Anti Jamur, Anti Virus, Anti Parasit, DLL)Документ72 страницыDR - Saleh-26 March 2013-Farmakologi (Anti Jamur, Anti Virus, Anti Parasit, DLL)jeinpratpong100% (4)
- Lac 10&11 PPTДокумент16 страницLac 10&11 PPTRaghdaОценок пока нет
- Antibiotics EssayДокумент5 страницAntibiotics EssayIshwarya JonathanОценок пока нет
- Neisseria Gonorrhoeae, Sometimes Called The: I. DefinitionДокумент16 страницNeisseria Gonorrhoeae, Sometimes Called The: I. DefinitionBerle Joy VillanuevaОценок пока нет
- Antibiotics and Antibacterial DrugsДокумент69 страницAntibiotics and Antibacterial DrugsJames PerianayagamОценок пока нет
- CiprofloxacinДокумент1 страницаCiprofloxacinEОценок пока нет
- Pharm MnemonicsДокумент47 страницPharm MnemonicsMina RacadioОценок пока нет
- Antibiotik Dan Antiseptik Saluran KemihДокумент29 страницAntibiotik Dan Antiseptik Saluran KemihPutri Sari SeptirianiОценок пока нет
- Introduction To Antimicrobial/Anti-Infective DrugsДокумент17 страницIntroduction To Antimicrobial/Anti-Infective DrugsMaria Pina Barbado PonceОценок пока нет
- Week 5 LecturesДокумент18 страницWeek 5 LecturesJana-Tae KerrОценок пока нет
- Antiviral Drugs Group 3 FinalДокумент10 страницAntiviral Drugs Group 3 FinalSpeed SamОценок пока нет
- Female Urinary Tract Infections in Clinical PracticeОт EverandFemale Urinary Tract Infections in Clinical PracticeBob YangОценок пока нет
- Pneumococcal Vaccine Timing For AdultsДокумент4 страницыPneumococcal Vaccine Timing For AdultsNur Farhanah Zulkifli100% (1)
- Hepatitis B PDFДокумент15 страницHepatitis B PDFAvicenna_MSCОценок пока нет
- Liver CirrhosisДокумент83 страницыLiver CirrhosisRusiana NasilahОценок пока нет
- Daftar PustakaДокумент7 страницDaftar PustakaJonesius Eden ManoppoОценок пока нет
- CANCERДокумент11 страницCANCERMuhammed IbrahimОценок пока нет
- 1st PagesДокумент10 страниц1st PagesNhcpsОценок пока нет
- Biohazard Cabinet Operation Manual NSF 49-92-030714Документ37 страницBiohazard Cabinet Operation Manual NSF 49-92-030714Kaherul KaherОценок пока нет
- Rhizoctonia BulletinДокумент6 страницRhizoctonia BulletinMarlene RosalesОценок пока нет
- Amit Kumar Tyagi PHDДокумент40 страницAmit Kumar Tyagi PHDrohitОценок пока нет
- Molecular Mechanisms of B-Lymphocyte TransformationДокумент5 страницMolecular Mechanisms of B-Lymphocyte Transformationkiedd_04Оценок пока нет
- Communicable Diseases Handouts)Документ15 страницCommunicable Diseases Handouts)snpjavierОценок пока нет
- TetraximДокумент5 страницTetraximkemalahmadОценок пока нет
- MAPEH 8 Health - LAS 1 Communicable DiseasesДокумент1 страницаMAPEH 8 Health - LAS 1 Communicable DiseasesYanzy JilhanoОценок пока нет
- Immediate Care of The NewbornДокумент3 страницыImmediate Care of The NewbornAngelee OngchuaОценок пока нет
- Dsa 281Документ319 страницDsa 281Nabil ChoukОценок пока нет
- Spooky2rifefrequencylist PDFДокумент17 страницSpooky2rifefrequencylist PDFKevin100% (2)
- Ebola Health Education CHNДокумент23 страницыEbola Health Education CHNBrijesh YadavОценок пока нет
- Book Club Pack: Angel of Death: The Story of Smallpox by Gareth WilliamsДокумент2 страницыBook Club Pack: Angel of Death: The Story of Smallpox by Gareth WilliamsWellcome TrustОценок пока нет
- West Nile Virus Fact SheetДокумент2 страницыWest Nile Virus Fact SheetWSETОценок пока нет
- Project Coc (Cleanliness On Comfort Rooms)Документ6 страницProject Coc (Cleanliness On Comfort Rooms)Dhivinne PerezОценок пока нет
- IMCIДокумент3 страницыIMCIwordlife360Оценок пока нет
- Case Studies DetailsДокумент36 страницCase Studies Detailssiachen26100% (1)
- Case PresentationДокумент29 страницCase PresentationLeezhaj VargasОценок пока нет
- ETAs etaWEBREPORT PDFДокумент111 страницETAs etaWEBREPORT PDFjoelОценок пока нет
- Systemic Lupus Erythematosus Disease Activity Index SELENA ModificationДокумент4 страницыSystemic Lupus Erythematosus Disease Activity Index SELENA ModificationaminahrahimiОценок пока нет
- Lecture 01 - Introduction To ParasitologyДокумент38 страницLecture 01 - Introduction To ParasitologyGiorgos Doukas KaranasiosОценок пока нет
- Molecular Biology of The Gene: Figures 10.1 - 10.5Документ75 страницMolecular Biology of The Gene: Figures 10.1 - 10.5Arif MulyantoОценок пока нет
- RememberedДокумент12 страницRememberedLorenzini GrantОценок пока нет
- Epidemiologic Mass Treatment 2014Документ11 страницEpidemiologic Mass Treatment 2014TivHa Cii Mpuzz MandjaОценок пока нет