Академический Документы
Профессиональный Документы
Культура Документы
Limitations of Pulse Oximetry
Загружено:
Suresh KumarАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Limitations of Pulse Oximetry
Загружено:
Suresh KumarАвторское право:
Доступные форматы
Anesth Prog 39:194-196 1992
Limitations
of Pulse Ox
netry
George Mardirossian,
DMD, and Ronald E. Schneider, DDS Department of Oral and Maxillofacial Surgery, New Jersey Dental School, Newark, New Jersey
Pulse oximetry is a noninvasive, accurate, and safe method for the measurement of oxygen saturation during intravenous sedation or general anesthesia. Several factors should be considered with its use, since these variables will either alter the accuracy of the readings or may cause harm to the patient. These factors include changes in the strength of the arterial pulse, body movements, dyshemoglobinemias, plasma lipids and bilirubin, color interferences, venous pulsations, and several physical factors. Awareness of these variations will help the clinician become more knowledgeable in the use of the pulse oximeter.
to the patient. The clinician must be aware of the limitations of this technique and understand the conditions that alter its proper function.
BASIS OF PULSE OXIMETRY
The pulse oximeter functions by positioning a pulsating arterial vascular bed between a two-wavelength lightemitting diode and a detector (photodiode). One wavelength is 660 nm (red) and the other is 940 nm (infrared). Oxygenated hemoglobin (O2Hb) will absorb more of the 940 nm wavelength than reduced hemoglobin (RHb); conversely, RHb will absorb ten times more of the 660 nm wavelength than O2Hb.9 The pulse oximeter isolates readings of the pulsatile-dependent portion of the total light absorption, which is presumably arterial in nature. The percent saturation reading results from a ratio of oxygenated hemoglobin to the total hemoglobin content. In most situations, the total hemoglobin is essentially the sum of O2Hb and RHb (functional Hb Saturation); however, methemoglobin (MetHb) and carboxyhemoglobin (COHb) also absorb these wavelengths and, when increased in concentrations, will interfere with accurate SPO2 readings. This example is but one of many sources of error.
pulse oximetry has become a useful adjunct for monitoring the arterial oxygen saturation of hemoglobin. This method of continuous monitoring has been shown to detect early hypoxic changes in sedated or anesthetized patients. 1 Spectrophotoelectric oximetry is a noninvasive, accurate, and safe technique for measuring oxygen saturation and has become standard practice for specific clinical situations, such as intravenous conscious sedation, deep sedation, and general anesthesia.2 The pulse oximeter sensor is usually attached to a patient's digit and monitors early changes in arterial hemoglobin oxygen saturation (SpO2) in the peripheral tissues. Many publications have justly lauded the advent of the pulse oximeter. 1-4 However, the literature also reports several conditions when the use of this instrument has either harmed the patient or has given incorrect data.5-8 In most of these cases, these problems can be circumvented by thoroughly reviewing the medical history and physical findings and by proper application of this device
Received January 10, 1992; accepted for publication December 28, 1992. Address correspondence to Dr. George Mardirossian, Department of Oral and Maxillofacial Surgery, New Jersey Dental School, 110 Bergen Steet, Newark, NJ 07103-2400. 1992 by the American Dental Society of Anesthesiology
SOURCES FOR ERROR
Factors that can adversely influence the pulse oximeter reading include changes in the strength of the arterial pulse, body movements, dyshemoglobinemias, plasma lipids and bilirubin, color interferences, venous pulsations, and various physical factors. These factors are summarized in Table 1.
Strength of the Arterial Pulse The pulse oximeter is designed to measure changes in light absorbance produced during arterial pulsations. In this manner, absorbance changes due to surrounding tissue are eliminated. Any factor that reduces vascular pulsations will reduce the ability of the instrument to detect
ISSN 0003-3006/92/$6.00
194
Anesth Prog 39:194-196 1992
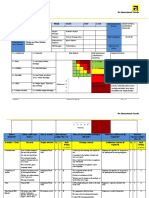
Table 1. Sources of Errors Error Source Hypotension
Vasoconstriction (Reduction of blood flow to arterial bed) Hypothermia (Reduction of blood flow; seen in Pts. w/Raynaud's disease) Shivering/muscle twitching
Mardirossian and Schneider 195
Effects on SpO2
Possible loss of signal
Possible loss of signal, reduction of SPO2 Possible loss of signal, reduction of SpO2
Response Correct underlying problem (eg, give fluid challenge, lighten anesthesia), vasopressors Change to more central site
Keep patient and extremities
warm
Carboxyhemoglobinemia
Methemoglobinemia
Venous pulsations Blood pressure cuff on monitored arm Arterial lines on monitored arm
Changes in pulse size, possible loss of signal Falsely high SPO2 reading
Falsely low readings approaching 85% Falsely low SP02 readings Loss of signal decreases SP02
Loss of signal decreases SP02
Warm and/or sedate patient Increase ventilation, eliminate rebreathing Administer methylene blue
Change site Change site
Avoid use of arteries in monitored arm Avoid exposure of photodiode to light
Intense bright light (eg, fiberoptic fluorescent lights)
Lower SP02 readings
and analyze the signal and, therefore, to calculate the arterial oxygen saturation. Hypothermia, hypotension (mean arterial blood pressure under 50 mm Hg), and the use of vasopressors that act to decrease the arterial pulsation in the finger or toe used for pulse oximetry may contribute to inaccurate readings. Most manufacturers warn that the instrument will not register a reading if there is inadequate perfusion. However, the clinician must still be aware that inaccurate reading may result from decreasing tissue perfusion. Body Movements Since pulse oximeters rely on the pulsatile stage of arterial blood flow to determine SP02, any extraneous movements that cause intermittent changes in absorbance can affect the reading. Shivering and muscle twitching may influence both the pulse rate display and saturation reading. Most instruments can tolerate small amounts of movement, but exaggerated movements have been shown to effect the accuracy of this method of monitoring.
push the saturation reading toward 85%, which will be falsely low at high SP02 states and falsely high at SP02 states below 85%. Methylene blue, which is used to treat methemoglobinemia will in itself cause a drop in SP02 to 65% for several minutes.9 Careful review of the medical history and physical examination will help to identify these patients.
Lipids and Bilirubin High blood lipid concentrations, hyperalimentation, and hyperbilirubinemia can interfere with pulse oximeter readings. Increased concentrations of bilirubin tend to overestimate the measured oxygen saturation. The Lambert-Beer Law states that the concentration of solute in suspension is inversely related to the intensity of light transmitted through the solution.10 Although the pulse oximeter is designed to measure two specific wavelengths, it is apparent that other elements of the blood can interfere with the overall transmission of light, including these two wavelengths.
Color Interferences Skin color is not a limiting factor in pulse oximetry, since the measurements use the arterial pulsatile component of blood flow, and the surround tissue is basically factored out by the microcomputer. In general, the instrument will accommodate a wide range of tissue thickness and skin pigmentation. However, artificial nails or opaque nail finishes may interfere with the transmission of the light
Dyshemoglobinemias
Dyshemoglobinemias due to methemoglobin, carboxyhemoglobin, and sulfhemoglobin may lead to inaccurate pulse oximeter readings due to absorbance of one or both wavelengths. Carboxyhemoglobin may absorb as much of the 660-nm wavelength as O2Hb. Methemoglobin will absorb as much of the 660-nm light as RHb, but absorbs the 940-nm light to even a greater degree. This effect will
196 Limitations of Pulse Oximetry
Anesth Prog 39:194-196 1992
source. Intravenous dyes, such as methylene blue, indigocarmine, and indocyanine green cause varying changes in pulse oximetry readings.
CONCLUSION
The pulse oximeter has proven efficacy in clinical practice. A vigilant and knowledgeable clinician, however, must be aware of its proper use and limitations. Only then can it be considered a useful adjunct to the care of the patient.
Venous Pulsations Arteriovenous anastamoses and glomuses are unusual features of the cutaneous circulation, particularly in the fingers and toes. Arterial blood is shunted into a vein, which also becomes pulsatile, causing falsely low readings.8 Physical Factors Many physical factors should be considered when using the pulse oximeter. The following are common-sense precautions. The clinician should avoid using the grounding pad of the electrocautery near the pulse oximeter sensor. The blood pressure cuff should not be placed on the arm that is being used for the sensor. Arterial lines or sticks should not be placed or performed on extremities used for oximetry. The pulse oximeter should not be plugged into the same power source as the electrocautery unit. In addition, the clinician should avoid interference of the sensor with high intensity light sources such as fiberoptic units. Finally, it must be made sure that the light-emitting diode is facing the nail bed and the photodiode is securely positioned on the opposite side of the digit.
ACKNOWLEDGMENT We wish to acknowledge the expertise contributed by Karen Taylor in the preparation of this review.
REFERENCES
1. Hovagim AR, Vitkum SA, Manecke GR, Reiner R: Arterial desaturation in adults receiving conscious sedation. J Oral Maxillofac Surg 1989;47:936-939. 2. Yelderman M, New W: Evaluation of pulse oximetry. Anesthesiology 1983;59:349-352. 3. Lopert H: The pulse oximeter in dental surgery. Anesth Prog 1989;36:146-147. 4. Anderson JA, Lambert DM, Kater ER, Dolan P: Pulse oximetry: evaluation of accuracy during outpatient general anesthesia for oral surgery. Anesth Prog 1988;35:53-60. 5. Chemello PD, Nelson SR, Wolford LM: Finger injury from pulse oximeter probe during orthognathic surgery. Oral Surg Oral Med Oral Pathol 1990;69:161-163. 6. Brunel W, Cohen NH: Evaluation of the accuracy of pulse oximetry in critically ill patients. Crit Care Med 1988; 16: 432. 7. Swedlow DB, Runnin V, Feaster S: In reply to: Ambient light affects pulse oximeters. Anesthesiology 1987;67:865. 8. Kim JM, Mathewson HS: Venous congestion affects arterial hemoglobin saturation measured by a pulse oximeter. Anesthesiology 1985;63:A174. 9. Tremper KK, Barker SJ: Pulse oximetry. Anesthesiology 1989;70:98-108. 10. Barash P, Cullen BF, Stoelting RK: Clinical Anesthesia. Philadelphia, JB Lippincott Co., 1989;116-121. 11. Nellcor Inc: Product Information. Hayward, CA, Nellcor Inc. 12. Novametrix Co: Product Information. Wallingford, CT, Novametrix Medical Systems.
MORBIDITY Although the pulse oximeter is noninvasive and considered safe, morbidity has been associated with its use. Finger ischemia and necrosis have been reported with use of nondisposable sensors. The duration of application of the pulse oximeter sensor, the amount of pressure exerted (which may depend on the size of the digit), and the amount of hypotension or vasoconstriction during the procedure have been implicated in this type of injury.5 Thermal injuries also have been reported due to faulty sensors. Manufacturers warn that these instruments are not designed to be used with explosive anesthetic gases. 11,12
Вам также может понравиться
- Spinal Anesthesia For Caeserian Section: Comparison of 5.0% Lignocaine and 0.5% BupivacaineДокумент4 страницыSpinal Anesthesia For Caeserian Section: Comparison of 5.0% Lignocaine and 0.5% BupivacaineSuresh KumarОценок пока нет
- Ventilator Associated Pneumonia (Vap)Документ11 страницVentilator Associated Pneumonia (Vap)Suresh KumarОценок пока нет
- Cerebral Protection What Is New ?Документ11 страницCerebral Protection What Is New ?Suresh Kumar100% (1)
- Anaesthetic Management of Blunt Chest TraumaДокумент11 страницAnaesthetic Management of Blunt Chest TraumaSuresh KumarОценок пока нет
- Medico-Legal Issues in AnaesthesiaДокумент2 страницыMedico-Legal Issues in AnaesthesiaSuresh KumarОценок пока нет
- Local Anaesthetic AgentsДокумент21 страницаLocal Anaesthetic AgentsSuresh KumarОценок пока нет
- GO S For Tamilnadu DoctorsДокумент160 страницGO S For Tamilnadu DoctorsSuresh KumarОценок пока нет
- Day Care AnesthesiaДокумент4 страницыDay Care AnesthesiaSuresh KumarОценок пока нет
- Alleviating Cancer PainДокумент9 страницAlleviating Cancer PainSuresh KumarОценок пока нет
- Perioperative Management of A Patient With Left Ventricular FailureДокумент6 страницPerioperative Management of A Patient With Left Ventricular FailureSuresh KumarОценок пока нет
- Controversial Issues in NeuroanaesthesiaДокумент12 страницControversial Issues in NeuroanaesthesiaSuresh KumarОценок пока нет
- Anaesthesia in The Gastrointestinal Endoscopy SuiteДокумент3 страницыAnaesthesia in The Gastrointestinal Endoscopy SuiteSuresh KumarОценок пока нет
- Anaesthesia Care Beyond Operating Rooms: Newer Opportunities & Challenges.Документ8 страницAnaesthesia Care Beyond Operating Rooms: Newer Opportunities & Challenges.Suresh Kumar100% (1)
- Role of The Anaesthesiologists in The Management of BurnsДокумент12 страницRole of The Anaesthesiologists in The Management of BurnsSuresh KumarОценок пока нет
- Depth of Anesthesia & MonitoringДокумент2 страницыDepth of Anesthesia & MonitoringSuresh KumarОценок пока нет
- Surgical Patients at Risk For Renal FailureДокумент35 страницSurgical Patients at Risk For Renal FailureSuresh KumarОценок пока нет
- Labour Analgesia - Recent ConceptsДокумент18 страницLabour Analgesia - Recent ConceptsSuresh KumarОценок пока нет
- Anaesthetic Management of Bleeding Obstetric PatientДокумент10 страницAnaesthetic Management of Bleeding Obstetric PatientSuresh KumarОценок пока нет
- Anaesthesia For Bleeding TonsilДокумент6 страницAnaesthesia For Bleeding TonsilSave MedicalEducation Save HealthCareОценок пока нет
- Anesthesia For Fetal SurgeryДокумент8 страницAnesthesia For Fetal SurgerySuresh KumarОценок пока нет
- Muscle Relaxants in Current PracticeДокумент6 страницMuscle Relaxants in Current PracticeSuresh KumarОценок пока нет
- Preoperative Anaesthetic Risk Assessment and Risk Reduction Before SurgeryДокумент17 страницPreoperative Anaesthetic Risk Assessment and Risk Reduction Before SurgerySuresh KumarОценок пока нет
- Pre-Operative Cardio-Pulmonary Exercise Testing (Cpet)Документ14 страницPre-Operative Cardio-Pulmonary Exercise Testing (Cpet)Suresh KumarОценок пока нет
- Anaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Документ16 страницAnaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Suresh KumarОценок пока нет
- Fluid Resuscitation in TraumaДокумент17 страницFluid Resuscitation in TraumaSuresh Kumar100% (1)
- Basic Physics Applied To AnaesthesiologyДокумент10 страницBasic Physics Applied To AnaesthesiologySuresh KumarОценок пока нет
- Analysis of Arterial Blood GasesДокумент17 страницAnalysis of Arterial Blood GasesSuresh KumarОценок пока нет
- Anaesthetic Management of Ihd Patients For Non Cardiac SurgeryДокумент18 страницAnaesthetic Management of Ihd Patients For Non Cardiac SurgerySuresh KumarОценок пока нет
- Anaesthesia Breathing SystemsДокумент15 страницAnaesthesia Breathing SystemsSuresh KumarОценок пока нет
- Pulmonary Function Test in Pre Anaesthetic EvaluationДокумент10 страницPulmonary Function Test in Pre Anaesthetic EvaluationSuresh KumarОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Slave and The Lion: (Time - 3.18)Документ1 страницаThe Slave and The Lion: (Time - 3.18)Mohammad AwaisОценок пока нет
- UPSR Model EssayДокумент22 страницыUPSR Model EssayKevin Suresh De CostaОценок пока нет
- Kate Hill - Rediscovering ThorДокумент172 страницыKate Hill - Rediscovering ThorsweetautumntearsОценок пока нет
- Lm2120e Lm2120e-Sp - Ego 56v Lawn Mower - ManualДокумент284 страницыLm2120e Lm2120e-Sp - Ego 56v Lawn Mower - ManualjОценок пока нет
- M-140075 ManualДокумент16 страницM-140075 ManualvovobossОценок пока нет
- Syncope ShockДокумент39 страницSyncope ShockBunga Erlita RosaliaОценок пока нет
- HSE Presentation TemplateДокумент10 страницHSE Presentation TemplatejeffreyОценок пока нет
- Cerebral Protection & NeuroresuscitationДокумент19 страницCerebral Protection & NeuroresuscitationImad El SadekОценок пока нет
- MCQ Introduction of Anatomy 2013-2014 by Dr. Noura PDFДокумент3 страницыMCQ Introduction of Anatomy 2013-2014 by Dr. Noura PDFFaddy Oraha75% (24)
- Case DigestДокумент3 страницыCase DigestRuss TuazonОценок пока нет
- Parotidectomy: H.Shameer AhamedДокумент47 страницParotidectomy: H.Shameer AhamedAndreas RendraОценок пока нет
- Safety Training Hydrojetting of Exchangers GeneralДокумент15 страницSafety Training Hydrojetting of Exchangers GeneralandinumailОценок пока нет
- Risk Assessment - Window and Glass Partition InstallationДокумент4 страницыRisk Assessment - Window and Glass Partition Installationburak80% (5)
- IHCD First Person On Scene - v4Документ3 страницыIHCD First Person On Scene - v4Blas de LezoОценок пока нет
- Report of Traffic Accident Occurring in California: Read Important Information On BackДокумент3 страницыReport of Traffic Accident Occurring in California: Read Important Information On BackThebomb3Оценок пока нет
- Frog AtlasДокумент26 страницFrog AtlasAlelie Ayen100% (2)
- Section D Pressure Relief Valves and Relief Valve Manifolds: LP-Gas & Anhydrous Ammonia EquipmentДокумент20 страницSection D Pressure Relief Valves and Relief Valve Manifolds: LP-Gas & Anhydrous Ammonia EquipmentHamza NoumanОценок пока нет
- Anatomy of Plexus Branchialis PDFДокумент24 страницыAnatomy of Plexus Branchialis PDFGemantri veyonda ZikryОценок пока нет
- 6-1 Warm Up and StretchingДокумент7 страниц6-1 Warm Up and StretchingRam SyistОценок пока нет
- Omsite 2004 PDFДокумент196 страницOmsite 2004 PDFJulieОценок пока нет
- Final Examination in Legal MedicineДокумент21 страницаFinal Examination in Legal MedicineFrances Angelie NacepoОценок пока нет
- Dman Spa 2014 Rev 1Документ40 страницDman Spa 2014 Rev 1osha911Оценок пока нет
- Test/Sign Procedure (+) INDДокумент8 страницTest/Sign Procedure (+) INDDesi SmithОценок пока нет
- 1986 Design of Pervious Pressure Tunnels Schleiss PDFДокумент8 страниц1986 Design of Pervious Pressure Tunnels Schleiss PDFgerardo manuel canto barreraОценок пока нет
- Nursing Care Plan Priorities: Risk For InjuryДокумент6 страницNursing Care Plan Priorities: Risk For InjuryPauling FrezОценок пока нет
- Reaction Paper About First AidДокумент3 страницыReaction Paper About First AidJerome DiassanОценок пока нет
- Stephanix BRS Basic Radiological System - User ManualДокумент34 страницыStephanix BRS Basic Radiological System - User ManualNassima BELILОценок пока нет
- NACM Welded Chain SpecificationsДокумент12 страницNACM Welded Chain SpecificationsAmpera marzelaОценок пока нет
- Ear Correctiono R E J AДокумент52 страницыEar Correctiono R E J AMiller Gonzalez100% (1)
- BA DL Brustbeinsaege EFA 57 en 02.2020Документ34 страницыBA DL Brustbeinsaege EFA 57 en 02.2020Enrique MurgiaОценок пока нет