Академический Документы
Профессиональный Документы
Культура Документы
Untitled
Загружено:
Cismaru Mirela VeronicaИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Untitled
Загружено:
Cismaru Mirela VeronicaАвторское право:
Доступные форматы
1274 Anatomic Characteristics of the Left Atrial Isthmus in Patients with Atrial Fibrillation: Lessons from Computed Tomographic
Images SHUO-JU CHIANG, M.D., HSUAN-MING TSAO, M.D., MEI-HAN WU, M.D., CHING-TAI TAI, M.D., SHIH-LIN CHANG, M.D., WANWARANG WONGCHAROEN, M.D., YENN-JIANG LIN, M.D., LI-WEI LO, M.D., YI-JEN CHEN, M.D., MING-HUEI SHEU, M.D., CHENG-YEN CHANG, M.D., and SHIH-ANN CHEN, M.D. From the Division of Cardiology and Cardiovascular Research Center, Radiology, Sch ool of Medicine, National Yang-Ming University, and Taipei Veterans General Hospital and I-Lan Hos pital, Taiwan Anatomic Characteristics of the Left Atrial Isthmus. Introduction: Left atrial ( LA) isthmus ablation was reported to improve the success rate of catheter ablation of paroxy smal atrial fibrillation (AF). LA isthmus ablation could also cure a subset of LA flutter. Therefore, understan ding the anatomy of the LA isthmus is important for performing the ablation effectively. Methods and Results: Group I included 45 patients (40 male, mean age=5013 years) with paroxysmal AF who underwent catheter ablation. Group II included 45 patients (37 male, mean age = 54 10 years) without a history of AF. They underwent a 16-slice multidetector computed tomogr aphy (MDCT) scan to delineate the LA structures before the ablation procedure. The average length of the LA isthmus was longer in group I than in group II (lateral isthmus: 3.30 0.68 vs 2.71 0.60 cm, P < 0.0 01; medial isthmus: 5.12 0.94 vs 4.45 0.63 cm, P < 0.001), and morphological patterns of lateral and medial isthmus were similar between groups. In addition, the average depth of lateral isthmus w as similar between groups (0.62 0.32 vs 0.55 0.33 cm, P = 0.41), but the average depth of medial isthmus w as larger in group I than in group II (0.60 0.32 vs 0.44 0.25 cm, P = 0.01). The medial isthmus had more ridges, as compared to the lateral isthmus (13% vs 0%, P = 0.026). Furthermore, the distanc es between esophagus and lateral isthmus were longer in group I than in group II (at the middle of is thmus and mitral annulus level: 21.0 4.8 vs 18.4 6.0 mm, P < 0.001; and 37.1 5.7 vs 29.6 8.1 mm, P < 0.00 1, respectively). Conclusion: The LA isthmus was longer in the AF patients. The morphology of the isthmus was variable. Compared with the lateral isthmus, the medial isthmus was longer and had more ri dges. A peculiar configuration of the isthmus provided by CT images could influence the ablation strategy. (J Cardiovasc Electrophysiol, Vol. 17, pp. 1274-1278, December 2006) atrial fibrillation, isthmus, computed tomography Introduction Catheter ablation to isolate the triggers of pulmonary veins (PV) from the left atrium was established to effectively treat paroxysmal atrial fibrillation (AF).1,2 However, the recurrence of AF was noted in about 2040% of the patients in the follow-up period. To improve the long-term success of AF ablation, the application of linear lesions in addition to the PV isolation was advocated to creating substrate modification and preventing AF recurrence.3-6 The lateral LA isthmus
defined as the area from the ostium of the left inferior PV (LIPV) to the lateral mitral annulus is the most frequently encountered linear lesion made.7 In addition, the area between This work was supported in part by grants from the Taipei Veterans General Hospital (VGH94-204, V95S27-005) and National Science Council (NSC94-2314-B-010-053, 056), Taiwan. Address for correspondence: Hsuan-Ming Tsao, M.D., Division of Cardiology, I-Lan Hospital, 152, Shin-Min Road, I-Lan City, Taiwan. Fax: 886-22873-5656; E-mail: hmtsao.pohai@msa.hinet.net Manuscript received 11 May 2006; Revised manuscript received 10 August 2006; Accepted for publication 14 August 2006. doi: 10.1111/j.1540-8167.2006.00645.x the right inferior PV to the mitral annulus, which is referred to as medial isthmus, was occasionally involved in part of the circuit of LA flutter.8,9 From the experience gained from the cavotricuspid isthmus ablation of typical atrial flutter, it is known that the peculiar structures of the isthmus encountered can significantly influence the procedure time and outcome of the ablation.10-13 Thus, understanding the morphological characteristics of the mitral isthmus is crucial to achieve a more efficient and successful ablation of AF. The purpose of this study was to characterize the morphology of the left atrial isthmus in AF patients using the 16-slice multidetector computed tomography (MDCT). Methods Patient Selection Group I included 45 consecutive patients who were referred for an electrophysiological study and catheter ablation because of frequent episodes of AF (more than one episode per week) and who were refractory to more than one antiarrhythmic drug. Group II included 45 control subjects with age and sex matched with group I. They had no history of AF. All 90 patients underwentMDCTto perform the morphology survey of the LA and PVs. Chiang et al. Anatomic Characteristics of the Left Atrial Isthmus 1275 MDCT The LA and PVs were evaluated with an ECG-gated, 16slice multidectorCTscanner (Siemens Sensation 16, Siemens Medical Solutions, Forchheim, Germany). All patients underwent the CT scan during sinus rhythm. A nonionic contrast medium, iohexol (350 mg of iodine per milliliter [Omnipaque, Amersham Health, Amersham, UK]), was given in a test dose to determine the moment of the peak left atrium filling, and subsequently followed by 80 mL of contrast medium and then chased with 60 mL of saline through the antecubital vein with the use of a power injector at a rate of 3.5 mL/second, after which the scanning was initiated. The image acquisition was performed from the base of the lungs to the apices during a single breathhold. The table speed and pitch were heart rate dependent because the image acquisition was ECG gated. The acquisition time was 2025 seconds. The lateral isthmus was demonstrated by a plane including the ostium of the left inferior PV, LA, and lateral mitral annulus. The medial isthmus was demonstrated by a plane that included the ostium of the right inferior PV, LA, and medial mitral annulus. The isthmus morphologywas analyzed in this plane. The isthmus lengthwas obtained by measuring the endocardial surface from the bottom of inferior PV ostium to the mitral annulus. In patients with left common trunk or large antrums, the length was obtained from the inferior border
of the common trunk or antrum to the mitral annulus. The distance was obtained by measuring the straight length of the isthmus in the same plane. The isthmus depth was measured from that straight line to the deepest point of a perpendicular line to the surface of the isthmus in all patients. If the depth was < 2 mm, it was defined as straight; if >2 mm, it was defined as concave. If the contour of the isthmus bulged over the straight line and formed a narrow band on the surface, it was defined as a ridge. If the morphology was composed of a vestibule and recess, it was defined as a pouch. These morphological patterns were evaluated with virtual endoscopic viewat the same time for confirmation. The image was sent to theworkstation (Advantage windows, version 4.0, General Electric Medical Systems, Milwankee, WI, USA). Endoscopic view analysis was performed with commercially available CT navigator software (Voxtool 3.0.51f, General Electric Medical Systems). The software allows voxel elimination on the basis of a user-defined threshold density value, which in the case of the left atrium is usually between 160 and 300 Housefield units depending on the enhanced density of contrast. It was possible to examine the area of interest as if the operator had a scope looking inside the left atrium; the operator could also move freely inside the cardiac cavity and into the PV. To evaluate the relationship between the esophagus and lateral isthmus, the distance was measured at three levels: (1) the junction of LIPV ostium and upper end of isthmus, (2) the mid-point of lateral isthmus, and (3) the mitral annulus (lower end of isthmus). Furthermore, the LA dimensions were obtained by measuring the maximal transverse diameter of theLAin a coronal section (LA1), and the maximal anteroposterior (LA2) and superoinferior (LA3) diameters of the LA in a sagittal section. Statistical Analysis All quantitative data are expressed as the mean SD. A chi-square test withYates correctionwas used for categorical variables; unpaired Students t-test was used for continuous variables between the two groups. A value of P < 0.05 was considered significant. Results Patient Characteristics The clinical characteristics, including age (50 13 vs 54 10 years, P = 0.12), gender (M/F: 40/5 vs 37/8, P = 0.55), hypertensive cardiovascular diseases, diabetes mellitus, chronic obstructive pulmonary disease, congestive heart failure, and coronary artery disease were similar between the two groups (Table 1). CT Findings Comparison of the structure of the LA isthmus between AF patients and controls The average length and straight distance of the lateral isthmus in the AF patients were longer than that in the controls (length: 3.30 0.68 vs 2.71 0.60 cm, P < 0.001; distance: 2.74 0.50 vs 2.32 0.43 cm, P < 0.001). The average length and straight distance of the medial isthmus in the AF patients were also longer than those in the controls (length: 5.12 0.94 vs 4.45 0.63 cm, P < 0.001; distance: 4.72 0.79 vs 4.15 0.55 cm, P < 0.001). In addition, the average depth of the lateral isthmus was similar between the two groups (0.62 0.32 vs 0.55 0.33 cm, P = 0.41). However, the average depth of the medial isthmus was larger
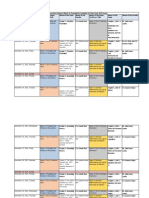
in group I than in group II (0.60 0.32 vs 0.44 0.25 cm, P=0.01). The morphology of the LA isthmuswas variable in TABLE 1 Patients Clinical and Computed Tomographic Parameters AF (n = 45) Control (n = 45) P Value Age (years) 50 13 54 10 0.12 Sex (male, %) 89 82 0.55 Hypertension (number) 8 8 >0.99 Diabetes 2 3 >0.99 COPD 1 2 >0.99 CHF 2 3 >0.99 CAD 3 2 >0.99 Lateral isthmus Length (cm) 3.30 0.68 2.71 0.60 <0.001 Distance (cm) 2.74 0.50 2.32 0.43 <0.001 Morphology Concave 37 35 Straight 6 8 Pouch 2 2 0.91 Depth (cm) 0.62 0.32 0.55 0.33 0.41 Medial isthmus Length (cm) 5.12 0.94 4.45 0.63 <0.001 Distance (cm) 4.72 0.79 4.15 0.55 <0.001 Morphology Concave 33 31 Straight 4 9 Pouch 2 2 Ridge 6 3 0.40 Depth (cm) 0.60 0.32 0.44 0.25 0.01 LA dimension (cm) LA1 6.10 0.62 5.37 0.59 <0.001 LA2 3.64 0.58 3.38 0.54 0.03 LA3 6.19 0.72 5.68 0.61 <0.001 CAD = coronary artery disease; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; LA = left atrium. 1276 Journal of Cardiovascular Electrophysiology Vol. 17, No. 12, December 2006 Figure 1. The different morphologies of the mitral isthmus demonstrated by multidetector computed tomography. A: Concave. B: Straight. C: Pouch. The corresponding virtual endoscopic views in the same patient are demonstrated from D to F (concave, straight, and pouch). LAPW = left atrial posterior wall; LIPV = left inferior pulmonary vein; LSPV = left superior pulmonary vein; MA = mitral annulus; MI = mitral isthmus; MV = mitral valve. both groups. The computed tomographic morphologies of the lateral isthmus in the AF patients included concave (82%), straight (13%), and pouch (5%) types (Fig. 1AF), which were similar to those of the controls (P = 0.91). The CT morphology of the medial isthmus in the AF included concave (73%), straight (9%), pouch (5%), and ridge (13%) (Fig. 2) types, which were similar to those of the controls (P = 0.40). Comparison of the lateral and medial isthmuses in AF patients The mean length (5.12 0.94 vs 3.30 0.68 cm, P < 0.001) and distance (4.72 0.79 vs 2.74 0.50 cm, P < 0.001) of the medial isthmus were significantly longer than that of the lateral isthmus. The depth of the medial isthmus was similar to lateral isthmus (0.60 0.28 vs 0.62 0.36 cm, P = 0.67). However, the morphologies of the medial isthmus were complex and consisted of more ridges in this area, as compared with the lateral isthmus (13% vs 0%, P = 0.026). Comparison of the left atrial dimension between the AF
patients and control The LA diameters, including LA1, LA2, and LA3, were significantly longer in group I (LA1: 6.10 0.62 vs 5.37 0.59 cm, P < 0.01; LA2: 3.64 0.58 vs 3.38 0.54 cm, P = 0.03, LA3: 6.19 0.70 vs 5.68 0.61 cm, P < 0.001). However, no significant difference could be demonstrated for the corrected isthmus length (lateral isthmus/LA1: 0.53 0.09 vs 0.53 0.13, P = 0.97; lateral isthmus/LA2: 0.92 0.22 vs 0.86 0.22, P = 0.32, lateral isthmus/LA3: 0.52 0.09 vs 0.51 0.13, P = 0.72) between the two groups. Comparison of the distance between the esophagus and lateral isthmus The distances between the esophagus and lateral isthmus at three levels were compared between the AF and control groups (at the junction of LIPV and lateral isthmus: 3.5 3.1 vs 4.1 3.3 mm, P=0.22; at the level of the middle of lateral isthmus 21.0 4.8 vs 18.4 6.0 mm, P < 0.001; at the level of mitral annulus: 37.1 5.7 vs 29.6 8.1 mm, P < 0.001, respectively). The esophaguswas in the closest vicinity of the upper end of the lateral isthmus at the junction of the LIPV ostium, with a mean distance of 3.5mmbetween them. Direct contact of esophagus with the upper end of isthmus could be noted in 51% (46/90) cases. As the esophagus descended, it became more separated from the isthmus toward the level of the mitral annulus (Fig. 3). The mean distance between the esophagus and the upper end of the lateral isthmuswas similar between the two groups, but the mean distance between the esophagus and the lateral mitral isthmus was greater in the AF patients. Discussion Major Findings Several important findings were observed in this study. First, the lateral and medial LA isthmuses were significantly longer in the AF patients than in the controls. Second, although the majority of the morphologies of the LA isthmus were concave, variable configurations of the isthmus, including the pouch, ridge, and straight types, were demonstrated in the AF patients. Third, the medial isthmus was longer and consisted of more ridges than the lateral isthmus. Fourth, the esophaguswas usually in close proximity to the upper portion of lateral isthmus. Anatomic Features of the LA Isthmus and LA Chamber Previous postmortem studies demonstrated considerable variations in the length and thickness of the LA isthmus in human hearts without AF.14,15 Becker reported that the mean length between the LIPV and mitral valve annulus was 34.6 mm (range 1552 mm). Schwartzman et al. used the CT scan to demonstrate that the distances between the inferior PVs and mitral annulus were longer in AF patients than those in non-AF patients.16 In the present study, the mean length of the lateral isthmus obtained by CT images was 2.74 cm in the control group (1.753.85 cm) and was longer with a mean length of 3.30 cm (2.105.53 cm) in the AF patients. In addition, the medial isthmus was also longer in AF patients and showed a considerable variation (3.146.53 cm) in the length. The longer isthmuses in AF patients might be one Chiang et al. Anatomic Characteristics of the Left Atrial Isthmus 1277 Figure 2. The ridge (arrows) between the right inferior pulmonary vein and mitral annulus was demonstrated by 2D (panel A) and
virtual endoscopic view (panel B). RIPV = right inferior pulmonary vein. local expression of the LA enlargement, rather than a specific feature of AF. More importantly, we demonstrated the different morphologies of endocardial aspect of the LA isthmus in AF patients by virtual endoscopic viewofMDCT. The configurations of the LA isthmuses were complex, including a concave shape, flat surface, and presence of a pouch in the lateral isthmuses. The configurations of the medial isthmus were more variable and included more ridges, as compared to the lateral isthmus. These features may result from the anatomic characteristics of this area and reflect the complexity of the ablation attempts. The ridge shown by the endoscopic view might be formed from the prominent muscle bundle first described by Papez.17 This bundle may correspond to the left leaf of the septum secundum. Furthermore, the mean depth of medial isthmus was significantly greater in AF patients, as compared with controls, but the mean depth of the lateral isthmus was similar between AF and controls. This observation could be explained by the regional difference of orientation and thickness of myocardial fibers between the structures of LA. We also measured the LA dimensions at the same time and observed a significantly dilated LA in the AF patients. Furthermore, the difference in the corrected isthmus length of LA1, LA2, and LA3 was nonsignificant between the two groups. In a previous study, we demonstrated the simultaneous dilatation of PVs and LA due to atrial stretch.18 It is plausible that isthmus elongation resulting from LA dilatation could occur in patients with AF. Figure 3. A: Axial view of MDCT showed the direct contact between the bottom of left inferior (LI) PV and esophagus (red circle). B: Sagittal view showed the esophagus (between red lines) was in contact with upper part of lateral isthmus (between the arrows) and was separated from the lateral isthmus gradually when it went down toward the mitral annulus (MA). A = anterior; Ao = aorta; CS = coronary sinus; L = left; LA = left atrium; LV = left ventricle; P = posterior; R = right; S = spine. Relationship Between the Esophagus and the Lateral Isthmus The atrio-esophageal fistula is a potentially serious drawback following radiofrequency ablations within LA. Delineating the relationship of the esophagus and posterior LA provides useful information to prevent this complication by avoiding energy applications over esophagus.19-21 Our results demonstrated that the esophagus was in very close vicinity of the upper end of isthmus at the level of inferior PVs. Direct contact of esophagus with the upper end of isthmus could be noted in50% cases. In these patients, care needs to be taken when deploying energies over the junction of LIPV and lateral isthmus to avoid repeated ablation and overheating. The esophagus was separated from the lateral isthmus gradually when it went down. The distance between the esophagus and lateral mitral annulus was more than 3 cm in our patients. Thus, it was less likely to cause esophageal injury during
ablation over the lower half of lateral isthmus. Clinical Implications Various approaches aimed at achieving complete block of the LA isthmus have been developed to improve the success rate of AF ablation. From the clinical experience gained from typical atrial flutter ablation, we reasonably postulate that the peculiar anatomy of the LA isthmus may influence the efficiency and safety of AF ablation. Wittkampf et al. showed that there are some cavities existing in the mitral isthmus and they might entrap the ablation catheter.15 Thus, if CT 1278 Journal of Cardiovascular Electrophysiology Vol. 17, No. 12, December 2006 images demonstrate a longer length and greater curvature of the isthmus, or a pouch is observed before the ablation, careful planning of the ablation strategy to avoid entrapment of catheter tip and decrease in gap formation should be undertaken. However, the ablation catheter may not follow the line with the shortest distance between inferior PVs and mitral annulus. This is a limitation in application of the CT images for AF ablation. Although the clinical study to evaluate the effectiveness of medial isthmus ablation was lacking, delivering radiofrequency energies between the right inferior PV and atrial septum or septum primum to mitral annuluswas effective to cure the left septal atrial flutter.22 It is crucial to increase the success rate ofAFablation if we can eliminate theLAflutter with circuit involving this area. Recognizing the details of medial isthmus anatomy can overcome the technical difficulty and improve the outcome. Conclusion TheLAisthmuses were longer in patients with paroxysmal AF. The morphologies of lateral and medial isthmus were complex, and a particular configuration of the isthmus shown by the CT images might influence the ablation results. In addition, close proximity of the esophagus and upper end of lateral isthmuswas demonstrated. Knowledge of the anatomy and the adjacent structure of the LA isthmus is important for rationalizing the ablation strategy and contributing to a successful outcome. References 1. Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Metayer P, Clementy J: Spontaneous initiation of atrial fibrillation by ectopic beats originating from pulmonary veins. New Engl J Med 1998;339:659-666. 2. Chen SA, Hsieh MH, Tai CT, Tsai CF, Prakash VS, Yu WC, Hsu TL, Ding YA, Chang MS: Initiation of atrial fibrillation by ectopic beats originating from the pulmonary veins: Electrophysiologic characteristics, pharmacologic response and effects of radiofrequency ablation. Circulation 1999;100:1879-1886. 3. Pappone C, Oreto G, Rosanio S, Vicedomini G, Tocchi M, Gugliotta F, Salvati A, Dicandia C, Calabro MP, Mazzone P, Ficarra E, Di Gioia C, Gulletta S, Nardi S, Santinelli V, Benussi S, Alfieri O: Atrial electroanatomic remodeling after circumferential radiofrequency pulmonary vein ablation: Efficacy of an anatomic approach in a large cohort of patients with atrial fibrillation. Circulation 2001;104:25392344. 4. Oral H, Scharf C, Chugh A, Hall B, Cheung P, Good E, Veerareddy S, Pelosi F Jr, Morady F: Catheter ablation for paroxysmal atrial fibrillation: Segmental pulmonary vein ostial ablation versus left atrial ablation. Circulation 2003;108:2355-2360. 5. Haissaguerre M, Sanders P, Hocini M, Hsu LF, Shah DC, Scavee
C, Takahashi Y, Rotter M, Pasquie JL, Garrigue S, Clementy J, Jais P: Changes in atrial fibrillation cycle length and inducibility during catheter ablation and their relation to outcome. Circulation 2004;109:3007-3013. 6. Oral H, Chugh A, Lemola K, Cheung P, Hall B, Good E, Han J, Tamirisa K, Bogun F, Pelosi F Jr, Morady F: Noninducibility of atrial fibrillation as an end point of left atrial circumferential ablation for paroxysmal atrial fibrillation: A randomized study. Circulation 2004;110:27972801. 7. Jais P, Hocini M, Hsu LF, Sanders P, Scavee C,Weerasooriya R, Macle L, Raybaud F, Garrigue S, Shah DC, Le Metayer P, Clementy J, Haissaguerre M: Technique and results of linear ablation at the mitral isthmus. Circulation 2004;110:2996-3002. 8. Marrouche NF, Natale A, Wazni OM, Cheng J, Yang Y, Pollack H, Verma A, Ursell P, Scheinman MM: Left septal atrial flutter: Electrophysiology, anatomy, and results of ablation. Circulation 2004;109:2440-2447. 9. Ouyang F, Ernst S, Vogtmann T, Goya M, Volkmer M, Schaumann A, Bansch D, Antz M, Kuck KH: Characterization of reentrant circuits in left atrial macroreentrant tachycardia: Critical isthmus block can prevent atrial tachycardia recurrence. Circulation 2002;105:1934-1942. 10. Da Costa A, Faure E, Thevenin J, Messier M, Bernard S, Abdel K, Robin C, Romeyer C, Isaaz K: Effect of isthmus anatomy and ablation catheter on radiofrequency catheter ablation of the cavotricuspid isthmus. Circulation 2004;110:1030-1035. 11. Cabrera JA, Sanchez-Quintana D, Ho SY, Medina A, Wanguemert F, Gross E, Grillo J, Hernandez E, Anderson RH: Angiographic anatomy of the inferior right atrial isthmus in patients with and without history of common atrial flutter. Circulation 1999;99:3017-3023. 12. Heidbuchel H, Willems R, Van Rensburg H, Adams J, Ector H, Van de Werf F: Right atrial angiographic evaluation of the posterior isthmus: Relevance for ablation of typical atrial flutter. Circulation 2000;101:2178-2184. 13. Cabrera JA, Sanchez-Quintana D, Farre J, Rubio JM, Ho SY: The inferior right atrial isthmus: Further architectural insights for current and coming ablation technologies. J Cardiovasc Electrophysiol 2005;16:402-408. 14. Becker AE: Left atrial isthmus: Anatomic aspects relevant for linear catheter ablation procedures in humans. J Cardiovasc Electrophysiol 2004;15:809-812. 15. Wittkampf FH, Van Oosterhout MF, Loh P, Derksen R, Vonken EJ, Slootweg PJ, Ho SY: Where to draw the mitral isthmus line in catheter ablation of atrial fibrillation: Histological analysis. Eur Heart J 2005;26:689-695. 16. Schwartzman D, Lacomis J, Wigginton WG: Characterization of left atrium and distal pulmonary vein morphology using multidimensional computed tomography. J Am Coll Cardiol 2003;41:1349-1357. 17. Papez J: Heart musculature of the atria. Am J Anat 1920;27:255-285. 18. Tsao HM, Yu WC, Cheng HC, Wu MH, Tai CT, Lin WS, Ding YA, Chang MS, Chen SA: Pulmonary vein dilation in patients with atrial fibrillation: Detection by magnetic resonance imaging. J Cardiovasc Electrophysiol 2001;12:809-813. 19. Lemola K, Sneider M, Desjardins B, Case I, Han J, Good E, Tamirisa K, Tsemo A, Chugh A, Bogun F, Pelosi F Jr, Kazerooni E, Morady F, Oral H: Computed tomographic analysis of the anatomy of the left atrium and the esophagus: Implications for left atrial catheter ablation. Circulation 2004;110:3655-3660. 20. Kottkamp H, Piorkowski C, Tanner H, Kobza R, Dorszewski A, Schirdewahn P, Gerds-Li JH, Hindricks G: Topographic variability of the esophageal left atrial relation influencing ablation lines in patients with
atrial fibrillation. J Cardiovasc Electrophysiol 2005;16:146-150. 21. Tsao HM,Wu MH, Higa S, Lee KT, Tai CT, Hsu NW, Chang CY, Chen SA: Anatomic relationship of the esophagus and left atrium: Implication for catheter ablation of atrial fibrillation. Chest 2005;128:2581-2587. 22. Marrouche NF, Natale A, Wazni OM, Cheng J, Yang Y, Pollack H, Verma A, Ursell P, Scheinman MM: Left septal atrial flutter: Electrophysiology, anatomy, and results of ablation. Circulation 2004;109:2440-2447.
Вам также может понравиться
- ICS Technical College Prospectus 2024 Edition 1Документ36 страницICS Technical College Prospectus 2024 Edition 1samuel287kalumeОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- SRT95 Engine Power TakeoffДокумент20 страницSRT95 Engine Power TakeoffoktopusОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- KOREAДокумент124 страницыKOREAchilla himmudОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- A Strategic Management PaperДокумент7 страницA Strategic Management PaperKarll Brendon SalubreОценок пока нет
- Chapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsДокумент10 страницChapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsALANKRIT TRIPATHIОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Analysis I - SyllabusДокумент3 страницыAnalysis I - SyllabusJUan GAbrielОценок пока нет
- Vee 2003Документ14 страницVee 2003Syed faizan Ali zaidiОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Communication & Collaboration: Lucy Borrego Leidy Hinojosa Scarlett DragustinovisДокумент44 страницыCommunication & Collaboration: Lucy Borrego Leidy Hinojosa Scarlett DragustinovisTeacherlucy BorregoОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Main: Exploded ViewДокумент30 страницMain: Exploded ViewamokssantiagoОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Database Case Study Mountain View HospitalДокумент6 страницDatabase Case Study Mountain View HospitalNicole Tulagan57% (7)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- RRC Igc1Документ6 страницRRC Igc1kabirОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Theravada BuddhismДокумент21 страницаTheravada BuddhismClarence John G. BelzaОценок пока нет
- Salt Analysis-Ferric ChlorideДокумент3 страницыSalt Analysis-Ferric ChlorideVandana0% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Iso 696 1975Документ8 страницIso 696 1975Ganciarov MihaelaОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Curriculum Vitae: Name: Bhupal Shrestha Address: Kamalamai Municipality-12, Sindhuli, Nepal. Email: ObjectiveДокумент1 страницаCurriculum Vitae: Name: Bhupal Shrestha Address: Kamalamai Municipality-12, Sindhuli, Nepal. Email: Objectivebhupal shresthaОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- German BasicДокумент60 страницGerman BasicchahirОценок пока нет
- IT Technician CVДокумент3 страницыIT Technician CVRavi KumarОценок пока нет
- Gizmotchy 3 Element Complete Assembly InstructionsДокумент5 страницGizmotchy 3 Element Complete Assembly InstructionsEuropaОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Working Capital Management (2015)Документ62 страницыWorking Capital Management (2015)AJОценок пока нет
- American Literature TimelineДокумент2 страницыAmerican Literature TimelineJoanna Dandasan100% (1)
- Armitage Tutorial for Cyber Attack ManagementДокумент54 страницыArmitage Tutorial for Cyber Attack Managementworkmumbai3870Оценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Viscosity IA - CHEMДокумент4 страницыViscosity IA - CHEMMatthew Cole50% (2)
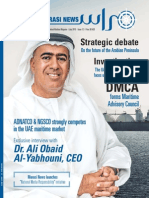
- MarasiNews Issue 12Документ47 страницMarasiNews Issue 12Sunil Kumar P GОценок пока нет
- Quality of Good TeacherДокумент5 страницQuality of Good TeacherRandyОценок пока нет
- Biology 11th Edition Mader Test BankДокумент25 страницBiology 11th Edition Mader Test BankAnthonyWeaveracey100% (44)
- Mafia Bride by CD Reiss (Reiss, CD)Документ200 страницMafia Bride by CD Reiss (Reiss, CD)Aurniaa InaraaОценок пока нет
- Year 2 - Push and Pull FPDДокумент18 страницYear 2 - Push and Pull FPDRebecca LОценок пока нет
- Chair Locker Provides Storage and Space SavingsДокумент32 страницыChair Locker Provides Storage and Space SavingsElza S. GapuzОценок пока нет
- Atomic Structure - One Shot by Sakshi Mam #BounceBackДокумент231 страницаAtomic Structure - One Shot by Sakshi Mam #BounceBackchansiray7870Оценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Jensen-English I SyllabusДокумент6 страницJensen-English I Syllabusapi-284900455Оценок пока нет