Академический Документы
Профессиональный Документы
Культура Документы
Practice Guidelines: Enteral Nutrition Delivery For The Adult Patient
Загружено:
damondouglasИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Practice Guidelines: Enteral Nutrition Delivery For The Adult Patient
Загружено:
damondouglasАвторское право:
Доступные форматы
Nutrition Care Subcommittee
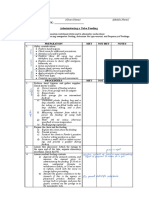
PRACTICE GUIDELINES: ENTERAL NUTRITION DELIVERY
FOR THE ADULT PATIENT
PURPOSE: To provide a “best practice” guideline for the management of enteral nutrition support in adult
patients based upon current research. To standardize practice throughout the organization.
I. Candidates for Enteral Nutrition
A. Who is a candidate for enteral feeds?
1. Functional GI tract and:
1. Neurological deficit prohibiting adequate intake
2. Mechanically ventilated
3. Increased nutrient needs unable to be met via p.o. intake
4. Oro-pharyngeal and esophageal deficits
B. Who is NOT a candidate for enteral feeds?
1. Bowel obstruction
2. Small bowel ileus
3. Intractable diarrhea
4. Massive intestinal hemorrhage
5. Low perfusion states
II. Feeding Tube Selection
A. Short Term
Selection criteria: for use in patients requiring nutrition support for < 6 weeks
1. NG Tube
2. OG Tube
3. Nasally-placed small bore feeding tube (gastric or post-pyloric placement)
B. Long Term/Permanent
Selection criteria: for use in patients requiring nutrition support for > 6 weeks
1. PEG
2. G-Tube
3. J-Tube
4. G-J Tube (e.g.: MICC)
III. Feeding Tube Placement and Care (Short Term)
A. Please refer to AACN Procedure Manual for Critical Care 4th Edition, Chapter 97, “Oro-gastric
and Naso-gastric Tube Insertion, Care, and Removal”, page 681
B. Please refer to UMMC Clinical Practice Council Practice Guideline: Procedure for Small-Bore
Feeding Tube Insertion (for post-pyloric placement)
IV. Long Term/Permanent Feeding Tube Care
A. Please refer to AACN Procedure Manual for Critical Care 4th Edition, Chapter 127,
“Gastrostomy or Jejunostomy Tube Care”, page 883
NutritionCare Subcommittee/Revised October 2007 1
V. Tube Identification
A. Refer to UMMC policy regarding labeling of tubes (Policy: Medication Administration Process
# Med-003 in Clinical Practice Manual)
B. Document clearly tip (end) position of feeding tube (ie: post-pyloric, naso-jejunal vs naso-
gastric)
VI. Formula Delivery
A. Clean Technique
• Wash hands prior to handling feedings and administration systems
• Inspect for dents and expired product
• Shake product to ensure proper mixing
• Rinse top of cans with water before opening
• Use clean technique
• Assemble feeding systems on a clean, dry, disinfected surface.
• Label feeding bag with patient name, product name, rate and
time/date hung. Limit hang time of feeding to 8 hours
• Note location of tube termination and document on flowsheet
(ie post-pyloric, naso-jejunal)
• Treat bag as a closed system (no additives without MD order)
• If additives placed in formula bag, hang time decreases to 4 hours
• Before adding additional tube feeding, let current formula
completely run out from bag. Flush any remaining feeding from
tubing. (coordinate with scheduled flush)
• Change entire administration set every 24 hours
• Discard all opened cans of formula that are not infused
VII. Method of Formula Delivery
A. Continuous Feeding Schedule
• Most appropriate feeding schedule for critically ill tube fed patients and only feeding
delivery method for small bowel feedings
• Formula infused continuously over ~ 24 hours via volumetric pump
• As a supplement to oral intake may be infused nocturnally over 10-12 hours
• Generally initiated at 20-40 ml/hour and advanced every 4-12 hours depending upon patient
tolerance to goal rate
• Fluid bolus usually provided every 4-6 hours to provide for additional fluid requirements
B. Intermittent Gravity Drip Feeding Schedule
• Intermittent feeding schedules are appropriate for non-critically ill patients and can only be
utilized in patients being fed gastrically. Jejunal/small bowel feedings should never be
delivered as intermittent gravity drip feeds. Patients who require long-term tube feedings
generally utilize this feeding regimen.
• Formula is infused intermittently throughout the day, often timed to mimic a meal schedule
(breakfast, lunch, dinner and HS snack)
• Formula is delivered via a feeding bag and tubing equipped with a roller clamp
NutritionCare Subcommittee/Revised October 2007 2
• Each feeding generally consists of 240- 480 ml formula infused via gravity drip over a
minimum of 30-60 minutes
• Patients should be positioned with head elevation at a minimum of 45 – 90 degrees during
and for 30 minutes following a feeding
• The feeding tube is flushed before and after each feeding. Additional free water can be
provided between meals.
• Gastric residual volumes (GRV) should be checked prior to each feeding (in patients with
gastric tubes) and if GRV is greater than 250 ml, the feeding should be delayed 1 hour and a
thorough GI assessment completed
C. Modular Components- DO NOT MIX MODULAR COMPONENTS INTO ENTERAL FEEDING
FORMULAS
• Prosource , No Carb - Single serving liquid protein supplement- 15 grams protein each
- Flush tube with 30 ml water
− Mix each packet Prosource with 30 ml tap water (subtract water from routine fluid
flush or bolus)
− Deliver Prosource bolus via syringe
− Flush tube with 30 ml water
• Arginaid
− Mix each packet Arginaid powder with 60 ml water in styrofoam cup with spoon, mix
until fully dissolved
− Flush feeding tube with 30 ml water
− Deliver Arginaid bolus via syringe
− Flush tube with 30 ml water
• GlutaSolve
− Flush feeding tube with 15 ml water
− Mix each packet GlutaSolve with 60 ml warm water for 20 seconds in a styrofoam cup
with spoon and infuse immediately via syringe
− Flush feeding tube with 15 ml water
D. Formula Delivery for Special Populations
1. Guidelines for all patients at UMMC and Shock Trauma undergoing HBO treatment and
receiving enteral nutrition support
A. Non Insulin Drip Requiring Enteral Nutrition Support Patient
a) All patients receiving tube feedings NOT on an insulin drip should be sent to the
HBO chamber with the tube feedings infusing
b) Prior to diving the tube feedings will be disconnected. (The tube feeding pole,
pump and formula will remain outside the diving chamber until the treatment is
complete due to pump incompatibility). Tube feeding infusion is restarted once
patient removed from the chamber.
c) RD will adjust the tube feeding formula goal rate for diving as follows:
o QD treatments calculate feedings on 21-hours/day infusions.
NutritionCare Subcommittee/Revised October 2007 3
o BID treatments calculate feedings on 18-hours/day infusions.
o Monitor patient tolerance to increased infusion rates
o Discuss with service RD.
B. Insulin Drip Requiring Enteral Nutrition Support Patient
*Goal is to maintain glucose control as per unit protocol. (For additional information,
refer to Hyperglycemia Management Guidelines)
a) All patients receiving tube feedings and on an insulin drip should leave the unit
for HBO treatment with the tube feeding and insulin drip infusing.
b) In HBO prior to diving, decrease the insulin drip rate by 50%.
Disconnect the tube feeding (The tube feeding pole, pump, and formula
will remain outside the diving chamber until patient’s treatment is
complete due to pump incompatibility).
Check finger glucose mid way through the dive. (~45minutes) and at
completion of treatment
Document glucose on flow sheet and adjust insulin drip per insulin drip
guidelines.
Tube feeding should be restarted once patient removed from the chamber
prior to transfer back to the patient care unit.
Document all changes on flow sheets
c) Upon return to room, check finger stick, document on flow sheets,
adjust insulin drip per insulin drip guidelines.
2. Guidelines for all patients at UMMC and Shock Trauma undergoing Hemodialysis and
Enteral Nutrition Support
Continuous enteral feedings should continue during hemodialysis treatment unless
otherwise ordered by the physician
a) Transport patients to dialysis with pump, pole and adequate tube feeding product
for duration of treatment
b) Document enteral feeds infused on flow sheet during dialysis
c) Follow aspiration precaution guidelines
VIII. Monitoring, Complication Prevention/Management
A. General Monitoring:
1. Blood glucose
• Where applicable, follow Hyperglycemia Management Guidelines
• Goal glucose level: Per unit target
2. Weight
• Minimum twice weekly weight q Sunday and Wednesday
• Weigh patient in am
3. Intake/Output
4. Oral Care (Refer to CPC Practice Guidelines: Oral Care and Prevention of Aspiration
Pneumonia).
5. GI Exam
• To include evaluation of distention, tenderness, firmness, presence of bowel sound,
nausea, vomiting, flatus, stool (volume and characteristic)
NutritionCare Subcommittee/Revised October 2007 4
B. Monitoring Specific to Aspiration Prevention
1. Tube Position
• OGT/NGT placement should be confirmed
a. q shift
b. after severe coughing
c. after vomiting or retching
d. if mark at exit site of tube is in a different position or not visible
e. if a question exists regarding placement, feeding and medication delivery should
be held until placement confirmed
2. Head of bed elevation
• minimum 30 – 45 degrees for continuous feedings via gastric route
• 45 – 90 degrees during and 30 minutes after intermittent feedings
• Hold all tube feeding if HOB needs to be lower because of hemodynamic instability.
• Hold gastric feedings if HOB decreased for bedside procedures.
3. Frequent suctioning in ventilated patients.
4. Check gastric residuals (GRV)
• Do not check residuals in post pyloric feeding tubes or jejunal feeding tubes
• Check gastric residual volumes q 6 hrs (use 60 ml syringe w/Luer tip).
• Gastric residual volume should be checked in all gastrically fed patients regardless of
type of feeding tube (NGT, OGT, Gastric Corpak/Keofeed, PEG)
• All residual volumes must be documented on the flow sheet even if residual volume
is “0” ml
• If GRV < 250 ml- re-feed aspirate and continue tube feedings in patients without
other clinical changes
• If GRV 250 – 350 ml- re-feed aspirate in patients without clinical changes or change
in GI exam. Hold tube feedings for 1 hour and re-check residual volume.
• If GRV > 350 ml or patient experiences emesis- hold tube feeding, discard aspirate,
notify physician and document on flow sheets
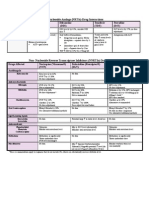
**Algorithm for residual volume management below
NutritionCare Subcommittee/Revised October 2007 5
Adult Check GRV every 6 hours if patient
Gastric receiving
gastric tube feeding (TF) and document
Residual
all
Volume
(GRV)
Algorithm
If GRV < 250 ml If GRV 250-350 ml IF
If GRV
GRV >> 350
350 ml,
ml, or
or
if patient has
if patient has
emesisemesis
•Return aspirate to patient, in the
•Refeed aspirate to absence of change in clinical
patient condition
•Continue TF or GI exam
•Hold TF 1 hour and recheck GRV
If GRV < 250 ml If GRV ≥ 250 ml
•Stop TF
•Discard
aspirate/emesis
•Notify MD
•Monitor clinical
condition(pressors,
hemodynamic instability)
•Monitor GI exam (firm,
distended,
N/V)
•Consider promotility agent
(e.g.metoclopramide)
•Verify tube placement & assess
Recheck GRV in 4
Nutritioncaresubcommittee/feb20 hours
04
NutritionCare Subcommittee/Revised October 2007 6
C. Complication Management
1. Tube occlusion
• Attach a 20 to 60 ml syringe to end of feeding tube and aspirate as much fluid as
possible. Fill syringe with warm water (Do not use carbonated beverages or fruit
juice). Instill using manual pressure for one minute; use a back-and-forth motion with
the plunger. Clamp the tube for 5 to 15 minutes. Try to aspirate or flush the tube.
Repeat as needed.
• If above fails, crush the Minimicrospheres from 1 capsule of Creon 10 or
formulary pancreatic enzymes with 1 (324 mg) tablet sodium bicarbonate. Dissolve in
5 mls warm water and inject into feeding tube. Cap tube and wait 5-15 minutes.
Uncap and attempt to flush tube. Repeat as needed.
2. Nausea/Vomiting
• Notify MD
• Hold gastric feedings for emesis
• Verify tube placement
• Assure head of bed elevation
• Assess for change in clinical status
• Evaluate changes in GI exam
− new onset distention
− constipation
• Medication profile review
• Evaluate possible etiology of symptoms
− Following suctioning
− Following medication administration
− Pain induced
− Too rapid feeding delivery
− Large volume fluid bolus
• Consider anti-emetics and/or promotility agents if other causes ruled out
• Discuss with R.D. if unresolved
3. Aspiration of feeding formula
• Immediate discontinuation of feeding and begin gastric decompression if able
• Notify MD
• Verify tube placement, HOB elevation
• Assess for changes in GI exam
• Discuss need for promotility agents and/or post pyloric feedings
4. Constipation- greater than 3 days without bowel movement
• Evaluate provision of enteral fluid boluses
• Evaluate need for bowel regimen
− Stool softener, laxatives, enemas
• Evaluate MAR for medications prone to decrease bowel motility (e.g.: Morphine)
NutritionCare Subcommittee/Revised October 2007 7
5. Acute/New-Onset Diarrhea- Greater than 5 liquid stools/day or a volume greater than
1500 ml/day
• Quantify stool output
• Notify MD for possible stool cultures (i.e. C. difficile )
• Evaluate medication profile (see medication section for high osmolality medication
list)
• Discuss with RD for further evaluation if above does not improve diarrhea
Blue dye is no longer recommended for routine use in enterally fed patients.
Case reports have associated negative patient outcomes caused by the systemic absorption of
blue dye in critically ill enterally fed patients.
Special Considerations with postpyloric and jejunal feeding tubes.
Due to their small diameter, additional diligence is required to prevent tube occlusion.
Feeding tubes should be flushed a minimum of 4 – 6 hours to maintain patency.
Do not obtain residual volumes from these tubes
Administer medications in liquid form whenever available
IX. Medications Delivery with Enteral Feedings
A. General considerations
• NO MEDICATION SHOULD BE MIXED DIRECTLY WITH FEEDING FORMULA.
• Identify where the tip of tube is prior to medication delivery as drug absorption can be affected by its
location.
• Flush tube with 15-30 ml tap water before and after administering medications and with 5 ml between
multiple doses being administered consecutively.
• If a medication is to be delivered on an empty stomach, check gastric residual before medication
delivery.
• Use only water to flush feeding tubes as other liquids not only significantly increase osmolality but also
may result in tube occlusion.
• When possible, the elixir, emulsion, solution, or suspension (except for ciprofloxacin and clarithromycin
suspensions) should be used. Notify the pharmacy that the medication is for delivery via feeding tube
and liquid medications can be sent, if available.
- medications available in liquid form include: acetaminophen, ibuprofen, ferrous sulfate, furosemide,
docusate, metoclopramide, diphenhydramine, multiple vitamins, valproic acid, potassium chloride,
digoxin, tacrolimus, sirolimus, and calcium carbonate.
• Administer medications as liquids. Many tablets can be crushed. Crush the tablet into a fine powder
and mix with 15-30 ml of room temperature tap water.
- Confirm with the pharmacy which medications can be crushed or opened. Certain medications such
as enteric coated, extended release, sustained release, or timed-release drugs should NOT be crushed
or opened to administer via feeding tube.
• Sublingual or buccal tablets should NOT be delivered via feeding tube.
NutritionCare Subcommittee/Revised October 2007 8
• Administer each medication separately and flush tube with 5 ml of water after each consecutively
administered medication.
• Liquid medications are easier to administer, but may be hypertonic and cause gastrointestinal distress.
Dilute hypertonic liquid medications with water.
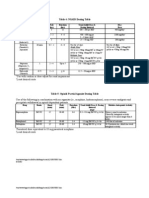
- Liquid medications can be up to 6000 mOsm whereas GI tract secretions are 300 mOsm (see below)
• *****Always flush tube between medications and Never mix medications together into “cocktails” as
these mixtures may cause precipitates, occlude feeding tubes or compromise patient safety because the
efficacy of the medication may be affected.
B. Preparation of Medication
1. Crushing Tablets
• Crush tablets as finely as possible. Mix powder with 15-60 ml tap water depending on tube diameter.
If tablet is uncovered, wrap in clean paper towel before crushing.
2. Thick Liquids
• Dilute with 15-30 ml of water. Very concentrated liquids should be diluted with 30-60 ml.
3. LIQUID-FILLED/SOFT GELATIN CAPSULES (e.g. Vit. E, calcitriol)
• Use one of 2 methods:
- A pinhole can be poked in one end of the capsule and the contents can be squeezed out and
reconstituted with 10-15 ml of tap water.
- Preferably, the entire capsule can be dissolved in 15-30 ml of warm tap water; it may take up to 1
hour for the capsule to dissolve.
4. Dilution
• Dilute medications that should be given with meals to avoid GI irritation.
• Dilute hypertonic or irritating medications with at least 15-30 ml of water to avoid GI irritation.
- This formula can be used to calculate the exact amount of water needed to bring the osmolality
of the hypertonic liquid medication down to isotonic levels:
- Final volume = volume of liquid med x mOsm of liquid med
desired mOsm (300-500)
- Example: a dilution with 30 ml of water can reduce a 10 ml amount of medication with an
osmolality of 2000 mOsm/kg to 500 mOsm/kg.
DRUG (Average) mOsm/kg
Acetaminophen elixir 5,400
Aminophylline liquid 450
Digoxin elixir 1,350
Diphenoxylate suspension 8,800
Ferrous sulfate liquid 4,700
Furosemide solution 2,050
Metoclopramide 8,350
Multivitamin liquid ~5,700
Phenytoin sodium suspension 1,500-2,000
Potassium chloride liquid 3,000-4,350
NutritionCare Subcommittee/Revised October 2007 9
Theophylline elixir 6,550
C. Specific Medication considerations:
1. Liquid Antacids
• Administer into feeding tubes with the tip placed in the stomach only.
• Avoid giving via feeding tubes < 10 french in size.
• Aluminum containing antacids (e.g. Amphogel/ aluminum hydroxide, Maalox, Mylanta)
should be given 15 minutes after all other medications have been administered.
• Preferably, give the antacid following a feed (bolus or intermittently fed patients) and flush the tube
with 10-15 ml of warm water prior to administration.
2. Bulk-forming Medications- (methylcellulose, polycarbophil Metamucil, psyllium, cholestyramine)
• Avoid giving via tube, especially small bore feeding tubes, as they clog easily.
3. Antibiotic Agents
• Clarithromycin and ciprofloxacin suspensions should NOT be administered via feeding tubes as they
clog easily. Used crushed ciprofloxacin tablets for medication administration via feeding tubes.
4. Gastrointestinal Agents
• Esomeprazole may be administered by opening and mixing the contents of the capsule with 25-50
ml of water or apple juice and giving immediately. Then flush the tube with 15 ml of water.
• Sucralfate should be administered into feeding tubes with the tip placed in the stomach only.
• Pancreatic enzymes (Creon, pancretin, Pancrease, pancrelipase) should be administered by
opening and mixing the contents of the capsule with 10-15 ml of apple or cranberry juice and given
immediately followed by flushing the tube with the juice. Then flush the tube with 15 ml of water.
5. Carbamazepine
• This suspension should NOT be given along with other medications or diluted with other liquids.
6. Phenytoin
• Hold tube feeds 1 hour before and 1 hour after dosing.
• Dilute phenytoin suspension with 30ml of water.
• Monitor blood levels of phenytoin.
• Phenytoin can not be delivered via J tube.
7. Ciprofloxacin
• Hold tube feeds for 1 hour before and 2 hours after dose is administered.
8. Moxifloxacin
• Hold tube feeds for 2 hours before and 2 hours after dose is administered.
NutritionCare Subcommittee/Revised October 2007 10
X: Documentation Requirements:
A. Patient/Family Education
1. Explain procedure for enteral nutrition
2. If possible, teach patient to report signs/symptoms of intolerance such as nausea, abdominal
cramping, abdominal fullness
3. Discuss patient’s need for long term nutrition support if appropriate
B. Aspiration Precautions
1. HOB Elevation
2. Gastric Residual Volumes (GRV)/frequency/times/appearance
C. Fluid bolus (fluid and volume)
D. Weight
E. Feeding prescription
F. Feeding formula, rate, total volume delivered over 24 hours
G. Feeding hold with reason
H. Tube insertion
I. Confirmation of tube placement minimum of q shift (naso-gastric)
J. Feeding tube type and tip placement
K. GI exam including bowel sounds, tenderness, distention, flatus, nausea, vomiting, stooling (character,
volume, frequency)
XI: Where To Document Each-
Nursing Flowsheet- Floor:
• Patient/Family Education- Computer charting or on paper form
• Aspiration Precautions- HOB elevation- Last Line under Nutrition Section (page 2)
• Gastric Residual Volumes/Appearance- Designated area in Nutrition Section (page 2)
• Feeding Prescription and Fluid bolus volume and frequency- (page 2) In “Diet” line under Nutrition
Section
• Actual Tube Feeding formula, rate and fluid bolus delivered- (page 6) Intake Section
• Tube Feeding holds/Reason- (page 1) Additional Notes section
• Tube insertion- (page 1) Additional notes section
• Feeding tube type and tip placement- (page 2) Nutrition Section “GI Access/Care”
• Confirmation of tube placement (NGT)- (page 2) Nutrition Section “GI Access/Care”
• GI Exam- (page 4) Assessment Section “GI”
• Weight- (page 6) Designated area
Nursing Flowsheet –ICU:
• Patient/Family Education- Computer charting
• Aspiration Precautions- HOB elevation- (page 1) Designated area
• Gastric Residual Volumes/Appearance- (page 4) “Tube feeding residual”
• Feeding Prescription and Fluid bolus volume and frequency- (page 4) “Meal assistance”
NutritionCare Subcommittee/Revised October 2007 11
• Actual Tube Feeding formula, rate and fluid bolus delivered- (page 3) Intake Section
• Tube Feeding holds/Reason- (page 6) “GI”
• Tube insertion- (page 6) “GI” or (page 8)
• Feeding tube type and tip placement- (page 6) “GI- Feeding tube Type/Location”
• Confirmation of tube placement (NGT)- (page 6) “GI- Feeding tube Type/Location”
• GI Exam- (page 6) Assessment Section “GI”
• Weight- (page 3) Designated area
Nursing Flowsheet- Trauma:
• Pt/Family Education Documentation-Complete the Pt/Family Education Documentation Form
• Aspiration Precautions-HOB (page 7)“GI” section
• Gastric Residual Volume: (page 3) “output” section above or on “OGT/NGT” line
• Feeding Bag Label: (page 8) under “care documentation”
• Fluid Bolus (page3) “intake” section below “PO/Enteral”
• Weight: (page 1) “Weight” box
• Feeding Prescription: (page 1) “Nutrition” box
• Feeding Formula, rate, and total: (page 3) “intake” section with “PO/Enteral” line
• Confirmation of tube placement and insertion: (page 7) “GI” section
• Feeding tube type and tip location: (page 5) “Label” section
• GI exam: (page 7) “GI” section
NutritionCare Subcommittee/Revised October 2007 12
Enteral Practice Guideline Reference List
Au Yeung S, Ensom M. Phenytoin and enteral feedings: does the evidence support an interaction? Ann
Pharmacother 34(7-8):896-905 Jul-Aug, 2000.
Bankhead R, Fang J. Enteral Access Devices IN The ASPEN Nutrition Support Core Curriculum: A Case Based
Approach/The Adult Patient. Gottschlich, MM (ed): ASPEN, Silver Spring, Maryland, 2007.
Carvalho MLR, Morais TA, Amaral DF, Sigulem DM. Hazard analysis and critical control point system
approach in the evaluation of environmental and procedural sources of contamination of enteral feeding in three
hospitals. JPEN 24:296-303, 2000.
Drugdex Drug Evaluations. Levodopa. Resource on world wide web: http://micromedex.com, June 2003.
Drugdex Drug Evaluations. Levothyroxine. Resource on world wide web: http://micromedex.com, July 2003.
Engle K, Hannawa T. Techniques for administering oral medications to critical care patients receiving
continuous enteral nutrition. Am J Health-Syst Pharm 56:1441-4, 1999.
FDA Public Health Advisory: Reports of blue discoloration and death in patients receiving enteral feedings
tinted with the dye, FD&C Blue No. 1. http://www.cfsan.fda.gov.
FDA website for USDA/NACMCF: HACCP; http://vm.cfsan.fda.gov/~comm/nacmcfp.html .
Heyland DK, Khaliwal R, Drover JW, et al. Canadian clinical practice guidelines for nutrition support in
mechanically ventilated, critically ill patients. JPEN 27:5:255-73, 2003.
Johnson D, Roach A. Esomeprazole pellets are stable following in vitro suspension in common beverages. Am
J Gastroenterol. 97(9 suppl):S20 Abstract 59, 2002.
Koch K. Improving Pharmaceutical Care: Active Monitoring of Phenytoin and Tube Feedings to Reduce
ADR’s. P&T, Aug 1995 520-31.
Kreymann KG, Berger MM, Deutz NEP, et al. ESPEN guidelines on enteral nutrition: intensive care.
Clinical Nutrition 25:210-33, 2006.
NutritionCare Subcommittee/Revised October 2007 13
Lacy C, Armstrong L, et al. Drug Information Handbook 2003-2004, 11th edition, Lexi-Comp INC. Hudson
(Cleveland) 2003.
Lefton J. Management of common gastrointestinal complications in tube-fed patients. Support Line 24(1): 19-
24, 2002
Levindale Geriatric Home & Hospital, Dept of Food and Nutrition HACCP Plan for Enteral Feeding and
Administration 11/99.
Lin HC, Van Citters GW. Stopping enteral feeding for arbitrary gastric residual volume may not be
physiologically sound: results of a computer simulation model. JPEN 21:286 - 289, 1997.
McClave SA, DeMeo MT, DeLegge MH et al. North American summit on aspiration in the critically ill patient:
concensus statement. JPEN Nov-Dec 26(6 Suppl):S80-5, 2002.
McClave SA, Snider HL. Clinical use of gastric residual volumes as a monitor for patients on enteral tube
feedings. JPEN 26:S43 - S50, 2002.
McClave SA, Snider HL, Lowen CC, et al. Use of residual volume as marker for enteral feeding intolerance:
prospective blinded comparison with physical examination and radiographic findings. JPEN 16:99 - 105, 1992.
Malone A, Seres D, Lord L. Complications of Enteral Nutrition IN The ASPEN Nutrition Support Core
Curriculum: A Case Based Approach/The Adult Patient. Gottschlich, MM (ed): ASPEN, Silver Spring,
Maryland, 2007.
Maloney, JP, Ryan TA, Brasel KJ et al. Food dye use in enteral feedings: a review and a call for a moratorium.
NCP 17: 168-181, 2002.
Marion M, McGiness C. Overview of Enteral Nutrition IN The ASPEN Nutrition Support Core Curriculum: A
Case Based Approach/The Adult Patient. Gottschlich, MM (ed): ASPEN, Silver Spring, Maryland, 2007.
Mentec H, Dupont H, Bocchetti M, Cani P, Ponche F, Bleichner G. Upper digestive intolerance during enteral
nutrition in critically ill patients: frequency, risk factors and complications. Crit Care Med 29(10):1955-1961,
2001.
Mitchell J. Oral dosage forms that should not be crushed: 2000 update. Hospital Pharmacy 35(5):553-7, 2000.
Montejo J. Enteral nutrition-related gastrointestinal complications in critically ill patients: A multicenter study.
Crit Care Med 27(8): 1447-1453, 1999.
Nestle Clinical Nutrition: The Seven Steps of HACCP, 2000.
Oliveira MR, Batista CRV, Aidoo KE. Application of hazard analysis critical control points system to enteral
tube feeding in hospital. The British Dietetic Association J Hum Nutr Dietet 14:397-403, 2001.
Parrish, CR. Enteral feeding: the art and science. NCP18: 76-85, 2003.
Pinilla JC, Samphire J, Arnold C, Liu L, Thiessen B. Comparison of gastrointestinal tolerance to two enteral
feeding protocols in critically ill patients: a prospective, randomized controlled trial. JPEN 25:81 - 86, 2001
NutritionCare Subcommittee/Revised October 2007 14
Robinson D, Higginson I, Macklin B, et al. Influence of protein containing meals on the pharmacokinetics of
levodopa in healthy volunteers. Br J Clin Pharmac 31: 413-7, 1991.
Schmidt L, Dalhoff K. Food-Drug Interactions. Drugs 62(10):1481-1502, 2002.
Smith Becker D, Ashley J. HACCP, Implications for enteral feeding .Today's Dietitian, October 2002.
Sostek M, Blychert E, et al. An in vitro study of the administration of esomeprazole enteric-coated pellets
through naso-gastric and gastrostomy tubes. Am J Gastroenterol 97(9 suppl):S3-4 Abstract 9, 2002.
Tube Feeding: Practical Guidelines and Nursing Protocols. Guenter, P and Silkroski, M (eds): ASPEN
Publication, Gaithersburg, Maryland, 2001.
University of Maryland Medical Center Formulary, 2007.
Van Den Bernt PMLA, Cusell MBI, Overbeeke PW et al. Quality improvement of oral medication
administration in patients with enteral feeding tubes. Qual Safe Health Care 15:44-7, 2007.
Williams T, Leslie G. A review of the nursing care of enteral feeding tubes in critically ill adults: part II.
Intensive and Critical Care Nursing 21:5-15, 2005.
NutritionCare Subcommittee/Revised October 2007 15
Вам также может понравиться
- HenyaДокумент6 страницHenyaKunnithi Sameunjai100% (1)
- Return Residual Fluid To Stomach Via Tube and Proceed To FeedingДокумент7 страницReturn Residual Fluid To Stomach Via Tube and Proceed To FeedingMhae De GuzmanОценок пока нет
- NGT Enteral Feeding CareДокумент8 страницNGT Enteral Feeding CareSheng GosepОценок пока нет
- Rounded Scoodie Bobwilson123 PDFДокумент3 страницыRounded Scoodie Bobwilson123 PDFStefania MoldoveanuОценок пока нет
- Assess, Check, Monitor Enteral FeedingДокумент3 страницыAssess, Check, Monitor Enteral Feedingchristina lidaОценок пока нет
- Maintaining Nutritional Status with Enteral FeedingДокумент22 страницыMaintaining Nutritional Status with Enteral FeedinganuОценок пока нет
- Gastrostomy and Jejunostomy Feeding Tube CareДокумент43 страницыGastrostomy and Jejunostomy Feeding Tube CareLeslie Anne Alcibar TababaОценок пока нет
- NG FeedingДокумент56 страницNG FeedingMae DacerОценок пока нет
- Biology Mapping GuideДокумент28 страницBiology Mapping GuideGazar100% (1)
- Case StudyДокумент2 страницыCase StudyBunga Larangan73% (11)
- Nasogastric Tube FeedingДокумент6 страницNasogastric Tube Feedingmarie100% (5)
- Enteral FeedingДокумент16 страницEnteral FeedingShane KasabovОценок пока нет
- Protocal Followed For Enteral FeedingДокумент4 страницыProtocal Followed For Enteral FeedingK Jayakumar KandasamyОценок пока нет
- Nasogastric Tube FeedingДокумент7 страницNasogastric Tube FeedingVina Empiales100% (1)
- Nutrition in Critically Ill PatientsДокумент34 страницыNutrition in Critically Ill PatientsBindiya MangarОценок пока нет
- NGT Feeding and Meds Administration Via NGTДокумент25 страницNGT Feeding and Meds Administration Via NGTPaul Michael BaguhinОценок пока нет
- Quantification of Dell S Competitive AdvantageДокумент3 страницыQuantification of Dell S Competitive AdvantageSandeep Yadav50% (2)
- Enteral Nutrition Support Assignment 72618Документ8 страницEnteral Nutrition Support Assignment 72618api-341835458100% (1)
- Enteral FeedingДокумент10 страницEnteral Feedingkitsilc100% (2)
- Antimicrobial Renal DosingДокумент5 страницAntimicrobial Renal DosingdamondouglasОценок пока нет
- Postgraduate Notes in OrthodonticsДокумент257 страницPostgraduate Notes in OrthodonticsSabrina Nitulescu100% (4)
- BDA guidance on enteral feeding in prone positionДокумент6 страницBDA guidance on enteral feeding in prone positionMahtosurup GodavarthyОценок пока нет
- Enteral Nutrition TherapyДокумент5 страницEnteral Nutrition TherapyJAMES ROD MARINDUQUEОценок пока нет
- Controlling Bleeding4AGastricGavage PDFДокумент25 страницControlling Bleeding4AGastricGavage PDFSam VeraОценок пока нет
- Icu Enteral Feeding GuidelinesДокумент12 страницIcu Enteral Feeding GuidelinesNofilia Citra CandraОценок пока нет
- NCM LabДокумент22 страницыNCM LabRico Delgado of WorldbexОценок пока нет
- Nasogastric/Enteric Tubes/Feedings - Page 1 Nursing Policy: T-58Документ10 страницNasogastric/Enteric Tubes/Feedings - Page 1 Nursing Policy: T-58Deology JuaninoОценок пока нет
- Nasogastric Tube InsertionДокумент12 страницNasogastric Tube Insertionmemon_bilqeesОценок пока нет
- FOND 231 Enteral and Parenteral Nutrition - 092140Документ36 страницFOND 231 Enteral and Parenteral Nutrition - 092140Keabetswe MosweuОценок пока нет
- NGT Feeding RemovingДокумент2 страницыNGT Feeding RemovingMaria Carmela RoblesОценок пока нет
- NutriLab Handout on Enteral Feeding Routes and MethodsДокумент9 страницNutriLab Handout on Enteral Feeding Routes and MethodsJudea PagedpedОценок пока нет
- Administration of Nasogastric Tube FeedingДокумент4 страницыAdministration of Nasogastric Tube FeedingLian James MataОценок пока нет
- Nutrition SupportДокумент15 страницNutrition SupportuSE yOUR hEADОценок пока нет
- Administering Tube FeedingДокумент2 страницыAdministering Tube FeedingAlecsandra CabridoОценок пока нет
- Gastrointestinal Treatment Modalties 1Документ28 страницGastrointestinal Treatment Modalties 1AndreОценок пока нет
- Guide to Tube and Parenteral FeedingДокумент4 страницыGuide to Tube and Parenteral FeedingMariaОценок пока нет
- Administering Tube FeedingsДокумент48 страницAdministering Tube FeedingsJan Federick BantayОценок пока нет
- DieteticsДокумент51 страницаDieteticsKainat RiazОценок пока нет
- CASE STUDY (Gastro)Документ3 страницыCASE STUDY (Gastro)Jake Yvan DizonОценок пока нет
- Medical Nutrition Therapy Classification of Modified DietsДокумент7 страницMedical Nutrition Therapy Classification of Modified DietsSOLIVEN KING JAMESОценок пока нет
- NUTR - Feeding PatientsДокумент38 страницNUTR - Feeding PatientsYorlenie JuárezОценок пока нет
- Clinical Topic # 5: Gastric Tubes Student GuideДокумент3 страницыClinical Topic # 5: Gastric Tubes Student Guidetripj33Оценок пока нет
- ICU Guide Enteral NutritionДокумент11 страницICU Guide Enteral NutritionPablo CauichОценок пока нет
- NGT NCM-116 ChecklistДокумент9 страницNGT NCM-116 ChecklistclaribelleОценок пока нет
- Gastrostomy Feeding Guideline: RationaleДокумент5 страницGastrostomy Feeding Guideline: RationaleRakaОценок пока нет
- Gastric GavageДокумент3 страницыGastric GavageRico Delgado of WorldbexОценок пока нет
- ParenteralДокумент10 страницParenteralDennis SantosОценок пока нет
- Nutritional SupportДокумент33 страницыNutritional SupportAlex WagnerОценок пока нет
- Nasogastric Tube Feeding GuideДокумент19 страницNasogastric Tube Feeding GuideMicah Alexis CandelarioОценок пока нет
- Specialized Nutrition Support: Enteral & Parenteral NutritionДокумент122 страницыSpecialized Nutrition Support: Enteral & Parenteral Nutrition천사자Оценок пока нет
- Gastric Gavage and LavageДокумент5 страницGastric Gavage and LavageEgielyn PainandosОценок пока нет
- Assignment 2Документ3 страницыAssignment 2Mays OthmanОценок пока нет
- Gastrostomy Feeding ProcedureДокумент5 страницGastrostomy Feeding ProcedureRohini RaiОценок пока нет
- RLE Nutritional Support NGT FeedingДокумент41 страницаRLE Nutritional Support NGT FeedingRoiniel AntonioОценок пока нет
- Fundamental Part II: Nutrition and MetabolismДокумент91 страницаFundamental Part II: Nutrition and MetabolismSeud BehruОценок пока нет
- Administering A Tube Feeding Preparation 1. Assess:: University of Eastern PhilippinesДокумент4 страницыAdministering A Tube Feeding Preparation 1. Assess:: University of Eastern PhilippinesJerika Shane MañosoОценок пока нет
- 17 Enteral and Parenteral NutritionДокумент47 страниц17 Enteral and Parenteral NutritionKathleen AngОценок пока нет
- NUTRI LEC CalaraДокумент6 страницNUTRI LEC CalaracalarasheanОценок пока нет
- TPN Care Guide Explains Parenteral NutritionДокумент5 страницTPN Care Guide Explains Parenteral NutritionkhalidicuОценок пока нет
- Nutritional support through feeding tubesДокумент76 страницNutritional support through feeding tubesKryzza LeizellОценок пока нет
- Caring For Your Jejunostomy Feeding Tube - Feb22Документ6 страницCaring For Your Jejunostomy Feeding Tube - Feb22Buvana VigneshОценок пока нет
- Gastrostomy FeedingДокумент8 страницGastrostomy FeedingAwol AregaОценок пока нет
- Tube Feeding PolicyДокумент3 страницыTube Feeding Policyaudrey.r.bedwellОценок пока нет
- Amit Enteral Feeding PresentationДокумент89 страницAmit Enteral Feeding PresentationAmit KochetaОценок пока нет
- Read The Case Study Then Answer The Following QuestionsДокумент1 страницаRead The Case Study Then Answer The Following QuestionsMays OthmanОценок пока нет
- Nutrition: A Handbook for NursesОт EverandNutrition: A Handbook for NursesCarolyn BestОценок пока нет
- IV PO Conversion P&P.V2Документ3 страницыIV PO Conversion P&P.V2damondouglasОценок пока нет
- Sodium Content of Inject Able AntibioticsДокумент1 страницаSodium Content of Inject Able AntibioticsdamondouglasОценок пока нет
- PIs Drug InteractionДокумент1 страницаPIs Drug InteractiondamondouglasОценок пока нет
- NRTI NNRTI Drug Interact TBLДокумент1 страницаNRTI NNRTI Drug Interact TBLdamondouglasОценок пока нет
- Sedation Pain AlgorithmДокумент1 страницаSedation Pain Algorithmdamondouglas100% (2)
- Restricted AntimicrobialsДокумент1 страницаRestricted AntimicrobialsdamondouglasОценок пока нет
- CAP Order Form Admission Final VerДокумент1 страницаCAP Order Form Admission Final VerdamondouglasОценок пока нет
- IV PO Conversion CAPДокумент3 страницыIV PO Conversion CAPdamondouglasОценок пока нет
- University of Maryland Medical Center Fluconazole (Diflucan®)Документ6 страницUniversity of Maryland Medical Center Fluconazole (Diflucan®)damondouglasОценок пока нет
- 3.E.2-Caspofungin Guideline 2003Документ3 страницы3.E.2-Caspofungin Guideline 2003damondouglasОценок пока нет
- CAP AlgorithmДокумент1 страницаCAP AlgorithmdamondouglasОценок пока нет
- Perioperative Antibiotics For Surgical ProphylaxisДокумент1 страницаPerioperative Antibiotics For Surgical ProphylaxisdamondouglasОценок пока нет
- CAP Guidelines For UseДокумент11 страницCAP Guidelines For Usedamondouglas100% (1)
- In B Deoxycholate Shortage Alternative TherapiesДокумент2 страницыIn B Deoxycholate Shortage Alternative TherapiesdamondouglasОценок пока нет
- Antibiogram 07Документ1 страницаAntibiogram 07damondouglas100% (1)
- NSAID Agonist Antagonist TableДокумент1 страницаNSAID Agonist Antagonist TabledamondouglasОценок пока нет
- UMMC Argatroban Protocol Revised 4-2008Документ2 страницыUMMC Argatroban Protocol Revised 4-2008damondouglas100% (1)
- ICU Neuromuscular BlockadeДокумент7 страницICU Neuromuscular BlockadedamondouglasОценок пока нет
- Opioid Equianalgesic ChartДокумент1 страницаOpioid Equianalgesic Chartdamondouglas100% (7)
- Pediatric Antimicrobial DosingДокумент3 страницыPediatric Antimicrobial Dosingdamondouglas100% (2)
- PONV GuidelinesДокумент3 страницыPONV GuidelinesdamondouglasОценок пока нет
- Pain Guidelines & Range DosingДокумент3 страницыPain Guidelines & Range Dosingdamondouglas100% (1)
- IV Insulin - FinalДокумент18 страницIV Insulin - Finaldamondouglas100% (2)
- IV PO Conversion CAPДокумент3 страницыIV PO Conversion CAPdamondouglasОценок пока нет
- IV PO ConversionsДокумент1 страницаIV PO Conversionsdamondouglas100% (1)
- Hyperglycemia Algorithm 2Документ1 страницаHyperglycemia Algorithm 2damondouglasОценок пока нет
- Guideline For The Prevention of CINДокумент2 страницыGuideline For The Prevention of CINdamondouglasОценок пока нет
- Hypertensive Urgency EmergencyДокумент5 страницHypertensive Urgency Emergencydamondouglas100% (3)
- HIT ProtocolДокумент1 страницаHIT ProtocoldamondouglasОценок пока нет
- MID TERM Question Paper SETTLEMENT PLANNING - SEC CДокумент1 страницаMID TERM Question Paper SETTLEMENT PLANNING - SEC CSHASHWAT GUPTAОценок пока нет
- AsiaSat 7 at 105Документ14 страницAsiaSat 7 at 105rahman200387Оценок пока нет
- UAPPДокумент91 страницаUAPPMassimiliano de StellaОценок пока нет
- Write UpДокумент5 страницWrite Upmourad baОценок пока нет
- Last Clean ExceptionДокумент24 страницыLast Clean Exceptionbeom choiОценок пока нет
- Ancient Greek Divination by Birthmarks and MolesДокумент8 страницAncient Greek Divination by Birthmarks and MolessheaniОценок пока нет
- STAT100 Fall19 Test 2 ANSWERS Practice Problems PDFДокумент23 страницыSTAT100 Fall19 Test 2 ANSWERS Practice Problems PDFabutiОценок пока нет
- Rishte ki baat SMS messages collectionДокумент108 страницRishte ki baat SMS messages collectionTushar AggarwalОценок пока нет
- Lecture02 NoteДокумент23 страницыLecture02 NoteJibril JundiОценок пока нет
- Nokia MMS Java Library v1.1Документ14 страницNokia MMS Java Library v1.1nadrian1153848Оценок пока нет
- Final Thesis Report YacobДокумент114 страницFinal Thesis Report YacobAddis GetahunОценок пока нет
- Electronics Ecommerce Website: 1) Background/ Problem StatementДокумент7 страницElectronics Ecommerce Website: 1) Background/ Problem StatementdesalegnОценок пока нет
- 5511Документ29 страниц5511Ckaal74Оценок пока нет
- Federal Complaint of Molotov Cocktail Construction at Austin ProtestДокумент8 страницFederal Complaint of Molotov Cocktail Construction at Austin ProtestAnonymous Pb39klJОценок пока нет
- UTP3-SW04-TP60 Datasheet VER2.0Документ2 страницыUTP3-SW04-TP60 Datasheet VER2.0Ricardo TitoОценок пока нет
- تاااتتاااДокумент14 страницتاااتتاااMegdam Sameeh TarawnehОценок пока нет
- Tigo Pesa Account StatementДокумент7 страницTigo Pesa Account StatementPeter Ngicur Carthemi100% (1)
- How Psychology Has Changed Over TimeДокумент2 страницыHow Psychology Has Changed Over TimeMaedot HaddisОценок пока нет
- Tension field beams: Aircraft wing spar analysisДокумент19 страницTension field beams: Aircraft wing spar analysisPrajeesh RajОценок пока нет
- Additional Help With OSCOLA Style GuidelinesДокумент26 страницAdditional Help With OSCOLA Style GuidelinesThabooОценок пока нет
- ServiceДокумент47 страницServiceMarko KoširОценок пока нет
- Zelev 1Документ2 страницыZelev 1evansparrowОценок пока нет
- Pom Final On Rice MillДокумент21 страницаPom Final On Rice MillKashif AliОценок пока нет