Академический Документы
Профессиональный Документы
Культура Документы
Pain Case - SOAP Note (2011)
Загружено:
Alfie LeeИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pain Case - SOAP Note (2011)
Загружено:
Alfie LeeАвторское право:
Доступные форматы
PHAR 401 Pain Case (Tutorial #4)
Nov 14/11 @0945HRS ID Clinical Pharmacist Note MK is a 51-year-old previously healthy female librarian presenting to pain clinic for the first time with uncontrolled pain following a workplace injury after a metal shelving unit fell on her right arm 9 weeks ago. 1) Pain - c/o of shooting and stabbing pain which radiates up/down right arm; pulsates periodically; feels occasional numbness in right arm. Pain worsens when someone brushes up against arm. Pain limits patients ability to perform daily activities (e.g. putting clothes on, eating, perform job duties). - Has tried tramadol, ibuprofen, and naproxen with no improvement; denies current use of these medications. - Currently uses Tylenol #1 for pain; takes 8-9 tablets/dose and uses approximately 100 tablets every 3-4 days. Rates pain as 10/10 prior to and 9/10 after taking Tylenol #1. Patient acknowledges minimal relief with current regimen, but believes there are no other alternatives. - Patient denies any history of chemical dependency. 2) Mood - c/o depressed mood and fatigue. Has loss of interest in interacting with friends and family since the injury occurred. Patient reports suicidal thoughts, but does not have a plan. - Patient denies previous history of depression or psychiatric illness O - Patient is tearful with a sad facial expression; appears frustrated and defeated. - Patient guarding right arm/hand during interview. - Chart note from physical therapist indicates limited range of motion in right arm/hand. - Chart note from case manager indicates patient will not be able to return to work due to injury and will require re-training - All lab results and vitals WNL - Current meds are: 1) Escitalopram 10 mg daily (started 6 weeks ago) 2) Tylenol #1 (see dose as per patient above; started 4 weeks ago) - PharmaNet shows recent prescriptions filled for tramadol, ibuprofen and naproxen.
1) Neuropathic pain control - Patients symptoms consistent with neuropathic pain, and she has inadequate pain control on current regimen - Requires reassessment of current drug therapy in order to reduce pain to a tolerable level and improve function - 1st line options for neuropathic pain = pregabalin, gabapentin, tricyclic antidepressants (e.g. amitriptyline) - Pregabalin has official indication for neuropathic pain, convenient dosing regimen, no significant drug interactions, WorkSafe BC coverage; will need to monitor for sedation, weight gain, edema, dry mouth - Pregabalin side effects can be minimized by titrating dose slowly (q 3 days) 2) Tylenol #1 overuse - Opioid narcotics are not drug of choice for neuropathic pain and patient overusing Tylenol #1 (exceeding daily 4 g maximum for acetaminophen) - Currently uses ~30 Tylenol #1 tablets/day ( 240 mg codeine phosphate/day) - Need to slowly taper codeine dose to prevent withdrawal (i.e. reduce total daily codeine dose by 10-15% every 3-7 days), with eventual goal to discontinue codeine - Taper by switching from Tylenol #1 to an equivalent codeine dose given as longacting (i.e. Codeine Contin) + short-acting (i.e. codeine phosphate) combination to provide baseline + breakthrough pain control - Acetaminophen may have opioid-sparing effects, but total daily dose needs to be lowered to within safe range 3) Depression - Patients depressed mood and suicidal thoughts suggest that current antidepressant regimen is ineffective - Requires reassessment of drug therapy to achieve remission, restore patient optimal functioning, and prevent suicide - Escitalopram is an appropriate 1st line drug choice, however current dose (10 mg/day) is subtherapeutic, and there is room to increase dose - Patient denies any side effects from escitalopram, therefore reasonable to continue for now (and not switch to another drug) 1) Discontinue Tylenol #1 2) Start new pain medication regimen today: - Tylenol Arthritis 650 mg ii PO Q8H at 7am, 3pm, 11pm - Codeine Contin 50 mg PO Q8H at 7am, 3pm, 11pm - Codeine phosphate 15 mg PO BID PRN breakthrough pain 3) Increase escitalopram to 20 mg PO OD 4) Give patient a 7-day supply of all medications; patient to return to clinic in 7 days for follow-up appointment 5) At next follow-up appointment, will plan to start pregabalin 25 mg PO OD x 3 days (with plan to titrate dose up by 25 mg/day every 3 days) 6) Will monitor for efficacy (reduced pain, improved mood, reduced fatigue, improved ability to participate in rehabilitation) and toxicity (drowsiness, constipation, GI upset, reduced sexual interest) 7) Will continue to re-assess pain management and codeine use at each follow-up, with eventual goal to discontinue codeine use
K.Seto
K. Seto, PharmD Pager #: 604-555-5555
Вам также может понравиться
- Soap Note Week 1 Sep7Документ3 страницыSoap Note Week 1 Sep7dondavis77Оценок пока нет
- Dermatitis SOAP NOTEДокумент10 страницDermatitis SOAP NOTEHugs100% (2)
- Chapter 3 SOAP NoteДокумент2 страницыChapter 3 SOAP NoteKatrina Litzko50% (2)
- Final Check Off Soap NoteДокумент4 страницыFinal Check Off Soap Notesana100% (1)
- SoapДокумент5 страницSoapallele940% (1)
- Create SOAP Notes Using Medical TerminologyДокумент4 страницыCreate SOAP Notes Using Medical TerminologyLatora Gardner Boswell100% (3)
- Headache H&P SOAPДокумент3 страницыHeadache H&P SOAPRauf Ab67% (3)
- SOAP NoteДокумент8 страницSOAP NoteAnonymous p0y5mmLQОценок пока нет
- Nsg6435 Soap Note 2Документ7 страницNsg6435 Soap Note 2Hephzibah Beulah100% (1)
- Soap Note 1Документ3 страницыSoap Note 1Heather CunninghamОценок пока нет
- Soap Note 3 FinalДокумент9 страницSoap Note 3 Finalapi-272656243Оценок пока нет
- Physical Exam ChecklistДокумент2 страницыPhysical Exam ChecklistRaisah Bint Abdullah100% (5)
- Soap Note 3 DominguezДокумент6 страницSoap Note 3 Dominguezapi-320062911Оценок пока нет
- ICM SOAP Note 11:3Документ4 страницыICM SOAP Note 11:3Warren G Lawless67% (3)
- Soap Note1 - Gyn ComplaintДокумент6 страницSoap Note1 - Gyn Complaintapi-482726932100% (3)
- Soap 1Документ7 страницSoap 1api-248360288Оценок пока нет
- Primary Care Case: Sore ThroatДокумент9 страницPrimary Care Case: Sore Throatarunateja100% (2)
- Soap NotesДокумент1 страницаSoap Notesjcfx2100% (1)
- Final Practicum - Soap Note 3Документ17 страницFinal Practicum - Soap Note 3api-494643478100% (2)
- Chronic SOAP Note for 51 Year Old Female with HyperlipidemiaДокумент3 страницыChronic SOAP Note for 51 Year Old Female with HyperlipidemiaJeffrey ViernesОценок пока нет
- Red eye with dischargeДокумент4 страницыRed eye with dischargeเด็กชายท็อปปิ้ง ชอบกลิ้งเข้าคณะเภสัชศาสตร์Оценок пока нет
- SOAP Note Cheat Sheet - Complete H&PДокумент2 страницыSOAP Note Cheat Sheet - Complete H&PAdeline N. Omene95% (19)
- SOAP Sample 1Документ6 страницSOAP Sample 1AyeshaArif100% (1)
- Soap Note 2 Dominguez 2015Документ5 страницSoap Note 2 Dominguez 2015api-320062911Оценок пока нет
- Peds - Soap Note 5Документ3 страницыPeds - Soap Note 5api-546259691Оценок пока нет
- NU 665 Pediatric Gastrointestinal Case Study - Michelle - StewardДокумент10 страницNU 665 Pediatric Gastrointestinal Case Study - Michelle - StewardMichelle StewardОценок пока нет
- Sample Soap NoteДокумент12 страницSample Soap NoteSedaka Donaldson0% (1)
- Nurs 5018 - Soap Note Chronic IllnessДокумент5 страницNurs 5018 - Soap Note Chronic Illnessapi-308904543Оценок пока нет
- SOAP NoteДокумент3 страницыSOAP NoteMagdala D'autruche100% (1)
- Focused Soap NoteДокумент4 страницыFocused Soap Noteapi-24735887592% (13)
- Adult Health - Soap Note 5Документ3 страницыAdult Health - Soap Note 5api-546259691100% (3)
- SOAP 2 - KhanДокумент11 страницSOAP 2 - KhanMohammad KhanОценок пока нет
- Soap Note - Musculoskeletal and Nervous SystemsДокумент2 страницыSoap Note - Musculoskeletal and Nervous SystemsSummer Keller88% (8)
- Danny Rivera SOAPДокумент4 страницыDanny Rivera SOAPariel sparkman100% (1)
- Contraception SOAP Note ReviewДокумент7 страницContraception SOAP Note ReviewAnnah AnnОценок пока нет
- Abdominal Pain Diagnosis and Treatment PlanДокумент2 страницыAbdominal Pain Diagnosis and Treatment PlanSandhya Rubens67% (9)
- Soap NotesДокумент2 страницыSoap Notesapi-380833341100% (1)
- 11 - Dot Phrase Templates HMC ED June 2017 - Rev 9.6.17Документ13 страниц11 - Dot Phrase Templates HMC ED June 2017 - Rev 9.6.17M100% (1)
- SOAP Annual PhysicalДокумент11 страницSOAP Annual Physicalniknshell100% (1)
- H&P For ScriptДокумент12 страницH&P For ScriptAlina KievskyОценок пока нет
- Nurs 5023 - Soap 5Документ5 страницNurs 5023 - Soap 5api-308904543100% (2)
- Nursing NoteДокумент6 страницNursing Noteshiller0% (1)
- Sample Soap NoteДокумент7 страницSample Soap Notesedaka260% (1)
- Soap NoteДокумент4 страницыSoap Noteapi-252633788100% (7)
- Acute Cholecystitis ER AdmissionДокумент6 страницAcute Cholecystitis ER Admissionjessica100% (5)
- Soap Well Women S KellyДокумент6 страницSoap Well Women S Kellyapi-415083061Оценок пока нет
- Adult - Case StudyДокумент14 страницAdult - Case Studyapi-494643478100% (2)
- SOAP Note AdviceДокумент5 страницSOAP Note AdviceNico AvellanaОценок пока нет
- Patient History and Presentation SkillsДокумент4 страницыPatient History and Presentation Skillsbnarnold100% (2)
- Peds 4 Soap Note S Kelly 5023 100 From KellyДокумент12 страницPeds 4 Soap Note S Kelly 5023 100 From Kellyapi-415083061Оценок пока нет
- SOAP For Upper Respiratory Infection #4Документ3 страницыSOAP For Upper Respiratory Infection #4carlos fernandezОценок пока нет
- Soap 5 - Geriatric 65Документ13 страницSoap 5 - Geriatric 65api-482726932Оценок пока нет
- Esther Park - SOAP NOTE - Abdominal PainДокумент4 страницыEsther Park - SOAP NOTE - Abdominal PainMallory ZaborОценок пока нет
- TB Soap NoteДокумент1 страницаTB Soap NoteNumerator0% (1)
- Textbook of Urgent Care Management: Chapter 17, Physician Extenders in the Urgent Care CenterОт EverandTextbook of Urgent Care Management: Chapter 17, Physician Extenders in the Urgent Care CenterОценок пока нет
- The Nurse Practitioner in UrologyОт EverandThe Nurse Practitioner in UrologyMichelle LajinessОценок пока нет
- Back to Zero: FNP Board Review NotesОт EverandBack to Zero: FNP Board Review NotesРейтинг: 5 из 5 звезд5/5 (2)
- FAMILY NURSE PRACTITIONER: Passbooks Study GuideОт EverandFAMILY NURSE PRACTITIONER: Passbooks Study GuideОценок пока нет
- Herbal Antibiotics: A Review: October 2020Документ8 страницHerbal Antibiotics: A Review: October 2020srikanth PosaОценок пока нет
- Psychiatry MCQ-Answer-Book PDFДокумент12 страницPsychiatry MCQ-Answer-Book PDFWorku Kifle100% (2)
- GBTPP PHKДокумент59 страницGBTPP PHKSyahrul Tuba Al FatihОценок пока нет
- 04-05-2020 - Non Compartment AnalysisДокумент3 страницы04-05-2020 - Non Compartment AnalysisTHE SMURFSОценок пока нет
- Ayahuasca 2022Документ17 страницAyahuasca 2022Doctor LeoОценок пока нет
- Hemodynamic Management Pocket Card PDFДокумент8 страницHemodynamic Management Pocket Card PDFjenn1722Оценок пока нет
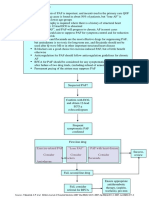
- Pathway DIAGNOSIS OF PAF FTRДокумент1 страницаPathway DIAGNOSIS OF PAF FTRYoan Eka Putra PalilingОценок пока нет
- The Neurobiology of AutismДокумент15 страницThe Neurobiology of AutismArif KurniawanОценок пока нет
- DM Type 2Документ9 страницDM Type 2Gates FebriОценок пока нет
- Naloxone HydrochlorideДокумент3 страницыNaloxone HydrochlorideDanish MaqboolОценок пока нет
- Solved Suppose That in The Repeated Bertrand Model Discussed in SectionДокумент1 страницаSolved Suppose That in The Repeated Bertrand Model Discussed in SectionM Bilal SaleemОценок пока нет
- Article WJPR 1513745964Документ12 страницArticle WJPR 1513745964Sivakumar LakshminarayananОценок пока нет
- A Milestone in Codifying The Wisdom of Traditional Oriental Medicine: TCM, Kampo, TKM, TVM-WHO International Standard Terminologies On Traditional Medicine in The Western Pacific RegionДокумент3 страницыA Milestone in Codifying The Wisdom of Traditional Oriental Medicine: TCM, Kampo, TKM, TVM-WHO International Standard Terminologies On Traditional Medicine in The Western Pacific RegionDimas RfОценок пока нет
- Pcol Cover To CoverДокумент214 страницPcol Cover To CoverJec OcampoОценок пока нет
- 85beb4c0-49be-4351-b700-ee2fc36a7ab6Документ90 страниц85beb4c0-49be-4351-b700-ee2fc36a7ab6imgamer.msОценок пока нет
- Zinc Oxide USP 31Документ5 страницZinc Oxide USP 31Gracelyn GatusОценок пока нет
- Validate Cleaning Method for Flunixin Meglumine ResidueДокумент14 страницValidate Cleaning Method for Flunixin Meglumine ResiduePatricia Joyce Malabanan SunglaoОценок пока нет
- Chapter 1 Dispensing Labelling MeДокумент10 страницChapter 1 Dispensing Labelling MeQasim Jalali NanotiОценок пока нет
- Drug Metabolism - Phase IIДокумент26 страницDrug Metabolism - Phase IIalexpharmОценок пока нет
- Chewing Guava L-WPS Office YasДокумент5 страницChewing Guava L-WPS Office Yasmady everardОценок пока нет
- Character, Onset, Location, Duration, Severity, Pattern and Associated - FactorsДокумент1 страницаCharacter, Onset, Location, Duration, Severity, Pattern and Associated - FactorsJohn CuencoОценок пока нет
- NYSTATIN-nys Tatin S Us Pens Ion Morton Grove Pharmaceuticals, IncДокумент5 страницNYSTATIN-nys Tatin S Us Pens Ion Morton Grove Pharmaceuticals, IncZeyad A AbdullahОценок пока нет
- Post-Stroke Depression - A ReviewДокумент20 страницPost-Stroke Depression - A Reviewkenth nathanОценок пока нет
- Workshop 8. Badac Plan of ActionДокумент1 страницаWorkshop 8. Badac Plan of Actionjudy mar delacruzОценок пока нет
- Transdermal Drug Delivery System ReviewДокумент8 страницTransdermal Drug Delivery System ReviewParth SahniОценок пока нет
- Malarone JuniorДокумент5 страницMalarone Juniorhannah.g.pavОценок пока нет
- A Drug Study On EpinephrineДокумент7 страницA Drug Study On EpinephrineMaesy Garcia LorenaОценок пока нет
- Mehlmanmedical Hy Neuro Part IДокумент18 страницMehlmanmedical Hy Neuro Part IAzlan OmarОценок пока нет
- Anesthesia in Dentistry and Extraction of Tooth by Pratyasha ParipurnaДокумент42 страницыAnesthesia in Dentistry and Extraction of Tooth by Pratyasha ParipurnapariОценок пока нет
- Basetext SingleДокумент129 страницBasetext SingleJiHyun ParkОценок пока нет