Академический Документы
Профессиональный Документы
Культура Документы
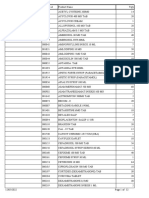
PM Drug List 2012
Загружено:
jrworthingtonАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
PM Drug List 2012
Загружено:
jrworthingtonАвторское право:
Доступные форматы
Drug Generic (Trade) adenosine (Adenocard)
Class antidysrhythmic
Indications stable PSVT, monomorphic VT, SVT
Adult Dosage/Route initial dose: 6 mg rapid IV push give over 1-2 seconds (may repeat 2 more times) repeat dose: 12 mg rapid IV push give over 1-2 seconds, repeat dose: 12 mg rapid IV push give over 1-2 seconds,
Pediatric Dose initial dose: 0.1 mg/kg rapid IV push (max 6mg) give over 1-2 seconds (may repeat 2 more times) repeat dose: 0.2 mg/kg IV push (max 12mg) give over 1-2 seconds, repeat dose: 0.2 mg/kg IV push (max 12mg) give over 12 seconds
albuterol 0.5% (Proventil, beta 2 adrenergic, Ventolin) bronchodilator
bronchospasm, asthma, reactive airway disease
2.5 mg/3cc saline via nebulizer
amiodarone (Cordarone) antiarrhythmic
cardiac arrest VF/ pulseless VT, VT with a pulse
0.15 mg/kg/3cc saline, up to 2.5 mg (2b protocol states for patients <1 year old 1.5 mg/3cc NS, for patients >1 year old 2.5 mg/3cc NS VF/VT arrest: 300 mg IV, may repeat 150 mg VF/VT arrest: 5 mg/kg IV once, IV after 3-5 minutes (max 2.2 grams in 24), VT max single dose 300 mg w/ pulse: 150mg slowly over 10 minutes administer vapors from crushed ampule for 30 administer vapors from crushed seconds, then administer oxygen 30 seconds, ampule for 30 seconds, then repeat continuously administer oxygen 30 seconds, repeat continuously
amyl nitrite
antidote
cyanide poisoning
aspirin (ASA)
NSAID analgesic, platelet inhibitor anticholinergic, parasympatholytic, antidote
chest pain suggestive of AMI
160 - 325 mg PO chewed
not indicated
atropine
symptomatic bradycardia, organophosphate or bradycardia 0.5 mg IV every 3 - 5 minutes, carbamate insecticide poisoning, premedication for(max 0.04 mg/kg or 3 mg), organophosphate RSI in children <10 years of age poisoning 2 - 5 mg IV until resolution of symptoms coma, hypoglycemia 1 gm/kg IV up to 25 grams, may repeat if glucose is <60 mg/dl (25 - 50 grams)
pediatric RSI dose: 0.02 mg/kg IV, minimum of 0.1 mg IV
dextrose 50%
carbohydrate
dextrose 25%
carbohydrate
coma, hypoglycemia
D50: 1-2 cc/kg , D25: 2-4cc/kg, D10: 5-10cc/kg
diazepam (Valium)
benzodiazepine, status epilepticus, sedation anticonvulsant, sedative
Status epilepticus 5 - 10 mg slow IV, Sedation 0.1 mg/kg IV up to 5mg every 25 - 15 mg slow IV 5 minutes, 0.2 mg/kg IN up to 10 mg every 2-5 minutes, 0.5 mg per rectum
diltiazem (Cardizem)
calcium channel blocker PSVT, rapid atrial fibrillation, atrial flutter (for rate 0.25 mg/kg IV slowly over 2 minutes (max 20 0.25 mg/kg IV slowly over 2 control) mg), if no affect in 15 mins., 0.35 mg/kg IV minutes (max 20 mg), if no slowly over 2 minutes (max 25 mg) affect in 15 mins., 0.35 mg/kg IV slowly over 2 minutes (max 25 mg), contact medical control prior to administration antihistamine, antidote allergies, anaphylaxis, acute dystonic reactions/ extrapyramidal symptoms - EPS shock, hypotension, bradycardia 25 - 50 mg IV, deep IM 1-2 mg/kg IV, up to 25 mg, deep IM
diphenhydramine (Benadryl) dopamine (Intropin)
sympathomimetic
2 - 20 mcg/kg/min titrate to effect, Renal dose 5-15 mcg/kg/min IV 2 - 5mcg/kg, Cardiac dose 5 - 10mcg/kg, Pressor dose 10 - 20mcg/kg
epineprine 1:10,000 (Adrenalin)
sympathomimetic
cardiac arrest, allergic reaction, anaphylaxis, severe asthma
1 mg IV every 3 - 5 minutes - arrest; 0.3-0.5 mg for allergic reaction, anaphylaxis, severe asthma 0.3 - 0.5 mg (0.3 - 0.5 mL 1:1,000) IM or SQ
0.01 mg/kg IV
epinephrine 1:1,000 (Adrenalin)
sympathomimetic
allergic reactions, anaphylaxis, severe asthma
0.01 mg/kg (max 0.5 mg) IV
epinephrine drip
sympathomimetic
bradycardia after atropine and (TCP) pacing are ineffective, hypotension after fluid bolus
2-10 mcg/min, Mix 4 mg/500 mL for 8 mcg/mL 0.1-0.2 mcg/kg/min IV concentration
etomidate (Amidate)
sedative, hypnotic
sedation for RSI
0.3 mg/kg IV
0.3 mg/kg IV
fentanyl (Sublimaze)
narcotic analgesic
analgesia, chest pain
0.5-1.0 mcg/kg (50 - 100 mcg) IV, IM slow push, RSI: 2-5 mcg/kg
1-2 mcg/kg IV
furosemide (Lasix)
loop diuretic
CHF, pulmonary edema, edema
0.5-1 mg/kg (20-80 mg) IV slow push
0.5-1 mg/kg IV, IM, usual max: 20 mg
glucagon
hormone
hypoglycemia, beta-blocker overdose
hypoglycemia: 0.05-1 mg IM, calcium channel hypoglycemia: 0.5-0.1mg/kg IM or beta-blocker OD 3-10 mg IV up to 1 mg, Not recommended for calcium channel or betablocker overdose 1-1.5 mg/kg IV (max 3 mg/kg) 1-1.5 mg/kg IVP (max 3 mg/kg)
lidocane (Xylocaine)
antidysrythmic
cardiac arrest, VT w/ pulse, PVC's
lidocane (Xylocaine) Drip antidysrythmic
ROSC if lidocaine used during arrest, PVC's
1-4 mg/min ( 2 grams in 500 mL NS)
contact medical control
lorazepam (Ativan)
benzodiazepine, status epilepticus, anxiety, sedation anticonvulsant, sedative electrolyte cardiac arrest, torsades des pointes, eclampsia, hypomagnesemia analgesia
magnesium Sulfate
2-4 mg slow IV, IM, may repeat in 15 minutes to max dose of 8 mg, for sedation 0.05 mg/kg up to 4 mg IM 1 - 2 gm IV for Torsades, 2 - 4 grams Eclampsia 50 - 100 mg slow IV, IM, SQ
0.05-0.1 mg/kg IV up to 5 mg IV, IM, max dose 0.2 mg/kg 25-50 mg/kg IV, one time, over 10-20 minutes (max 2 gm) 1mg/kg IV, IM, SQ
meperidine (Demerol)
analgesic
midazolam (Versed)
sedative
seizures, sedation
0.1 mg/kg IV up to 5 mg, 0.2 mg/kg IN up to 10 mg
seizure activity: 0.1 mg/kg IV, 0.2 mg/kg IN, max dose 5 mg
morphine
narcotic analgesic
analgesia, pulmonary edema, chest pain
naloxone (Narcan)
competetive opioid antagonist
opiate overdose, coma
2-10 mg IV, IM, SQ (maximum dose is patient 0.1-0.2 mg/kg IV, IM, SQ, specific based on ability to protect airway, maintain respiratory drive and maintain blood pressure) 0.4-2 mg IN, IV, IM every 2-3 minutues 0.01 mg/kg IN, IV, IM, ETT dose: 0.1 mg/kg, max IV 2 mg/dose 0.3-0.4 mg/spray, 0.3-0.4 mg/tablet not indicated
nitroglycerin spray nitroglycerin tablets
vasodialator
angina, CHF, myocardial infarction, pulmonary edema, hypertension
ondansetron (Zofran) oxygen
antinauseant elemental gas
nausea/vomiting
4 mg slow IV, IM
0.1 mg/kg slow IVP, IM same as adult
hypoxia, ischemic chest pain, respiratory distress, Low concentration - 1 - 4 LPM via cannula, suspected carbon monoxide poisoning, traumatic High Concentration - 10 - 15 LPM via injuries, shock nonrereather mask
oxytocin (Pitocin)
hormone
postpartum hemorrhage
10 units IM after placenta delivers
not indicated
promethazine (Phenergan) rocuronium (Zemuron)
antiemetic, phenothiazine
nausea, vomiting, sedation
12.5-50 mg IV, deep IM every 4 hours
non-depolarizing paralytic sodim bicarbonate 8.4% electrolyte, alkalinizer succinylcholine (Anectine) vasopressin (Pitressin) depolarizing neuromuscular blocker vasopressor, hormone
paralysis to facilitate intubation tricyclic antidepressant overdose (TCA), hyperkalemia paralysis to facilitate intubation
0.6 - 1.2 mg/kg IV 1 mEq/kg 1 - 2 mg/kg IV
<2 years old - not indicated, 2 years old 6.25-12.5 mg IV, deep IM 1 mg/kg IV 0.5-1 mEq/kg IV 2 mg/kg IV
VF/VT cardiac arrest, (use in place of 1st or 2nd dose dose of epinephrine 1:10,000) paralysis to facilitate intubation
40 units IV (replaces 1st or 2nd dose of epinephrine in cardiac arrest) 0.1 mg/kg IV (up to 10 mg)
not indicated
vecuronium (Norcuron)
non-depolarizing paralytic
0.1 mg/kg IV
Contraindications (applies to all - sensitivity to drug) 2 or 3 AV block, sinus node disease, i.e. sicksinus syndrome, polymorphic ventricular tachycardia
Side effects CNS: headache, lightheadedness, dizziness, tingling in arms, numbness, apprehension, and blurred vision CV: brief asystole, facial flushing, bradycardia palpitations, chest pressure, hypotension Resp: dyspnea, hyperventilation, shortness of breath, bronchospasm GI: nausea, metallic taste, throat tighness, inform patient of feeling they will feel when adenosine is administered
Notes/Onset/Duration onset immediate, half-life 10-12 seconds, administer into the medication port closest to the IV site followed by rapid flush of 20 mL saline, theophyllines and caffiene may block effects, dipyridamole and carbamazepine may potentiate effects.
tachydysrythmias
CNS: tremors, headache, nervousness, anxiety onset immediate, half-life unknown, effect may CV: palpitations Resp: bronchospasm GI: be decreased in patients on beta blockers. nausea/vomiting
none in prehospital cardiac arrest, cardiogenic shock, bradycardia, 2 or 3 AV block, idioventricular rhythm, sinus node dysfunction, none prehospital
CV: bradycardia, hypotension, vasodilation, AV block, increases. QTc, hepatotoxicity
onset 1-3 minutes, duration/half-life up to 40 days, do not administer with other QT prolonging drugs such as procainamide
CV: hypotension, headache, methemoglobinemia administer as soon as possible after exposure GI: nausea
allergy to ASA, patients with "factor" deficiencies, use caution with asthma, ulcers or other bleeding disorders presence of acute MI, narrow angle glaucoma
intracranial hemorrhage
CV: prolonged bleeding time Resp: onset 35-40 minutes, duration and peak effect bronchospasm, angioedema GI: nausea, vary by patient vomiting, CNS: dilated pupils, headache CV: , tachycardia, use as premedication for RSI in children <10 dry mouth, flushed hot dry skin, years, or before second dose of Succinylcholine tachydysrhythmias, usually does not work in the in adults presence of beta-blocker or calcium channel blocker overdose CNS: hyperglycemia CV: possible hypokalemia, onset immediate, duration is dependent on leve tissue necrosis if extravasation occurs, venous of hypoglycemia, best if given through central irritation at insertion point line or large venous catheter
intracranial hemorrhage
CNS: hyperglycemia CV: possible hypokalemia, onset immediate, duration is dependent on leve tissue necrosis if extravasation occurs, venous of hypoglycemia, may cause hypokalemia irritation at insertion point onset 1-5 min, duration 20-60 minutes
head Injury, decreased BP, acute narrow angle CNS: drowsiness CV: hypotension, venous glaucoma, renal failure - lorazepam, midazolam, irritation Resp: decreased respirations hepatic failure - lorazepam
2 or 3 AV block, hypotension, sick sinus CNS: headache, dizziness, weaknes CV: syndrome, WPW or short PR syndrome with atrial hypotension, bradycardia, flushing, diaphoresis fibrillation or atrial flutter, do not give with oral GI: nausea, vomiting, diltiazem will increase beta blockers, do not give with IV furosemide in serum digoxin levels the same line
onset 2-3 min, duration 1-3 hours, use
use with caution in elderly patients, use caution with asthma patients, acute narrow angle glaucoma hypovolemic shock, pheochromocytoma, tachyarrhythmias, decrease dose for patient's on MAOIs
CNS: dizziness, sedation, blurred vision, onset 15-30 min, peak affect 1 hour, duration anticholinergic affects Resp: thickens bronchial 12 hours secretions CNS: headache CV: tachydysrhythmia, VT, VF, onset 1-4 minutes, peak afffect 5-10 minutes, hypertension, cardiac ishemia/infarct, incresed mix 800 mg/500 mL for 1600 mcg/mL, ensure myocardial oxygen demand, extravasation causes patient is on supplemental oxygen during tissue necrosis GI: nausea, vomiting administration
none in cardiac arrest, tachydysrhtmias
CNS: anxiety CV: peripheral vasoconstriction, onset immediate, duration 5-10 minutes, do not hypertension, tachycardia, arrhythmias, increasedmix with sodium bicarbonate myocardial oxygen consumption
tachydysrhythmias
CNS: anxiety CV:peripheral vasoconstriction, onset immediate, duration 5-10 minutes, do not hypertension, tachycardia, arrhythmias, increasedmix with sodium bicarbonate myocardial oxygen consumption
tachydysrhythmias, hypovolemia
CNS: anxiety CV: peripheral vasoconstriction, onset immediate, duration 5-10 minutes, using hypertension, tachycardia, arrhythmias, increaseda 60 gtts set - 15 gtts/min = 2 mcg/min, 30 myocardial oxygen consumption gtts/min = 4 mcg/min, 45 gtts/min = 6 mcg/min, 60 gtts/min = 8 mcg/min, 75 gtts/min = 10 mcg/min adrenal insufficiency, use caution in septic shock CNS: transient suppression of corticosteroid onset 30-60 seconds, peak 1-3 minutes, production (after repeated doses), sedation CV: duration 4-10 minutes bradycardia, hypotension Resp: apnea GI: nausea, vomiting MAOI use, asthma, myasthenia gravis CNS: confusion, sedation, headache CV: onset 1-2 minutes, peak 3-5 minutes, duration hypotension, bradycardia Resp: apnea, GI: 20-60 minutes, decrease doses with elderly nausea, vomiting Side effects in pediatrics: chest patients wall rigidity CNS: tinnitus, dizziness CV: hypokalemia, onset 5 minutes, peak effect 20-60 minutes, hypovolemia, hepatic coma duration 2 hours IV, administer through separate IV line than other medications if possible GI: nausea, vomiting onset 5-10 minutes IM, peak effect within 30 minutes, duration 1-2 hours, depletes storage of glycogen patient may become hypoglycemic again if patient does not eat or receive glucose CNS: slurred speech, altered mental status CV: onset 30-90 seconds IV, 10-20 minutes bradycardia duration
hypokalemia, hypovolemia, hepatic coma, hypersensitivity to sulfonamides, anuria
pheocromocytoma
2nd or 3rd degree AV block, wide complex ventricular escape beats with bradycardia, use caution in patients with liver disease or renal disease 2nd or 3rd degree AV block, wide complex ventricular escape beats with bradycardia, use caution in patients with liver disease or renal disease
CNS: slurred speech, altered mental status CV: RSI premedication dose 1.0-1.5mg/kg to help bradycardia control ICP
acute narrow-angle glaucoma, use caution in renal CNS: dizziness, sedation, vertigo failure
onset 1-5 minutes IV, 15-30 minutes IM, duration 12-24 hours, note: overdose may be reversed by flumazenil none in cardiac arrest, renal disease, heart block CNS: CNS depression muscle hyporeflexia CV: antidote is calcium chloride hypotension, asystole, cardiac arrest Resp: repiratory paralysis patients receiving MAOI CNS: sedation, increased ICP CV: apnea, onset 1 minute, peak effect 5-7 minutes, hypotension, tachycardia Resp: nausea, vomiting duration 2-4 hours acute narrow angle glaucoma, shock, renal failureCNS: decreased level of consciousness CV: hypotension, bradycardia Resp: respiratory depression, apnea GI: nausea, vomiting, may be reversed with flumazenil head injury, COPD, hypotension, LOC CNS: dizziness, decreased level of consciousness CV: hypotension, syncope Resp: respiratory depression, apnea GI: nausea,vomiting use caution using with newborns of heroin CNS: withdrawal effects CV: hyper/hypotension, addicted mothers, may be better to use BVM, use arrhythmias/VF caution in chronic opiod user hypotension (systolic below 90), hypovolemia, intracranial bleeding, aortic stenosis, right ventricle infarction, severe bradycardia, or tachycardia, tamponade, recent use of Viagra, Cialis, or Levitra hypersensitivity
onset 1-5 min, durration dose related usually <2 hours
onset 1-3 minutes, peak 20 minutes, 4-5 hours, use caution in elderly, ALOC, patients in renal failure, and inferior MI
onset 1-2 min, duration 1-4 minutes, depending on overdose, will outlast heroin overdose, may not outlast longer acting narcotics
CNS: dizziness, headache CV: syncope, onset 1-2 minutes IV, 2-5 minutes SL, duration hypotension, tachycardia, rebound hypertension 3-5 minutes IV, duration 30-60 minutes SL, decreases preload - use caution in inferior MI, ask patient if using ED medications CNS: headache dizziness
effect is greater if patient has not vomited prior to administration known paraquat poisoning (paraquat is a commonCNS: high concetrations may cause a decreased onset immediate herbicide) level of consciousness and respiratory depression in patients with chronic carbon dioxide retention or chronic lung disease rule out multiple fetuses before administration CV: hypertension, dysrhythmias vasoconstrictors can cause major complications, onset - 3-5 minutes, duration up to 1 hour onset IV 5 minutes, duration is 2-8 hours, sedation effect may be potentiated by alcohol/CNS depressent use onset 30-60 seconds IV, duration 30-60 minutes, use with caution in children <2 onset is immediate, duration is 1-2 hours onset 30-60 seconds, duration 3-5 minutes, give sedation agent prior to administration of paralytic use in caution with patients with epilepsy
asthma, allergy to antihistamines, allergy to CNS: CNS depression, dizziness, drowsiness, phenothiazines, lactating females, MAOI use, sedation Resp: thickens bronchial secretions pregnancy, COPD, HTN caution if impaired hepatic or respiratory function, CV: dysrhythmias, hypotension Resp: or if severe obesity bronchospasm, apnea for 30-60 minutes alkalosis CV: metabolic alkalosis, hypokalemia, fluid overload glaucoma, eye injury, burns 24-48 hours old, CNS: hyperthermia CV: dysrhythmias, crush injury, muscular distrophy bradycardia, hypotension, hyperkalemia Resp:apnea for 3-5 minutes chronic nephritis, migraine, epilepsy, CHF, PG CNS: confusion CV: angina, IV pain GI: stomach cramps, nausea, vomiting, diarrhea, do not use on newborn, myasthenia gravis CV: dysrhythmias, hypotension Resp: bronchospasm, apnea for 20-45 minutes
onset <1min, duration 20-45 minutes, give sedation agent prior to administration of paralytic
Вам также может понравиться
- CH 03Документ71 страницаCH 03jrworthingtonОценок пока нет
- Vol1 Ch08 IbДокумент34 страницыVol1 Ch08 IbjrworthingtonОценок пока нет
- CH 10 AДокумент57 страницCH 10 AjrworthingtonОценок пока нет
- CH 06Документ71 страницаCH 06jrworthingtonОценок пока нет
- Spinal SeatedДокумент1 страницаSpinal Seatedcptjimmy15Оценок пока нет
- Curriculum-PM 2012Документ16 страницCurriculum-PM 2012jrworthingtonОценок пока нет
- Oral Station ScenarioДокумент3 страницыOral Station ScenariojrworthingtonОценок пока нет
- Bleeding ControlДокумент1 страницаBleeding ControlRashad SabreeОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Therapeutic Monoclonal Antibodies Approved by FDA in 2019 (Mini Review)Документ2 страницыTherapeutic Monoclonal Antibodies Approved by FDA in 2019 (Mini Review)asclepiuspdfsОценок пока нет
- Transfer LetterДокумент4 страницыTransfer LetterSarena GillОценок пока нет
- H2 Receptor Antagonists and LidocaineДокумент14 страницH2 Receptor Antagonists and LidocaineJoharaОценок пока нет
- Medication ModuleДокумент53 страницыMedication Modulefarhana100% (1)
- Drug Development ProcessДокумент14 страницDrug Development Processsnaren76100% (1)
- TDM Request Form Provides Drug MonitoringДокумент3 страницыTDM Request Form Provides Drug MonitoringWildan Setyo RayandiОценок пока нет
- PDF 0OIutGciNYy1qLCkgEMFДокумент2 страницыPDF 0OIutGciNYy1qLCkgEMFSusanta MohapatraОценок пока нет
- AMAZEO (Amisulpride)Документ14 страницAMAZEO (Amisulpride)Konark DinkarОценок пока нет
- PERFORMANCE EVALUATION CHECKLISTДокумент7 страницPERFORMANCE EVALUATION CHECKLISTJerika Shane MañosoОценок пока нет
- List Harga Obat Plazamedis Desember 2021Документ78 страницList Harga Obat Plazamedis Desember 2021Rusma YanaОценок пока нет
- Puskesmas Sidomulyo Reports Medicine Usage and RequestДокумент6 страницPuskesmas Sidomulyo Reports Medicine Usage and RequestJumaidin TvОценок пока нет
- Pharmacology of HypertensionДокумент23 страницыPharmacology of HypertensionNandraj123100% (1)
- Bioequivalence Comparison Between Two Different Formulations of Alverine AriqДокумент5 страницBioequivalence Comparison Between Two Different Formulations of Alverine AriqHendri WijayaОценок пока нет
- O Bat April 2022Документ32 страницыO Bat April 2022asd 123Оценок пока нет
- School Deworming Report FormДокумент1 страницаSchool Deworming Report FormErika Yahmila De LizoОценок пока нет
- Drugs Approving AuthoritiesДокумент38 страницDrugs Approving AuthoritiesTariq HaqueОценок пока нет
- Amikacin Drug StudyДокумент4 страницыAmikacin Drug StudyMark Angelo LorzanoОценок пока нет
- List of Substandard Drugs2006Документ8 страницList of Substandard Drugs2006Mohammad Shahbaz AlamОценок пока нет
- Cephalosphorins 3rd Gen 4rt GenДокумент24 страницыCephalosphorins 3rd Gen 4rt GenshaitabliganОценок пока нет
- Drug List FinalsДокумент2 страницыDrug List FinalsMyzhel InumerableОценок пока нет
- R GCVP V2 2.15Документ3 страницыR GCVP V2 2.15GabrielОценок пока нет
- Topic 13 - Post Marketing SurveillanceДокумент46 страницTopic 13 - Post Marketing SurveillanceTerepe CrimsonОценок пока нет
- Substance Use DisorderДокумент28 страницSubstance Use Disorderv.s rawatОценок пока нет
- Morphine & PhenobarbitalДокумент6 страницMorphine & PhenobarbitalfitriaОценок пока нет
- APPGP MFG OC G4 PD UNIT DOSE AND BATCH FORMULATIONДокумент5 страницAPPGP MFG OC G4 PD UNIT DOSE AND BATCH FORMULATIONIsabel PeraltaОценок пока нет
- 3-4 Epinephrine & LidocaineДокумент3 страницы3-4 Epinephrine & LidocaineNasrah N. MusaОценок пока нет
- Drug StudyДокумент5 страницDrug StudyKathleen Joy PingenОценок пока нет
- Deferasirox-An Oral Agent For Chronic Iron Overload: New Drug DevelopmentsДокумент8 страницDeferasirox-An Oral Agent For Chronic Iron Overload: New Drug DevelopmentsTriska Maharani Manoppo100% (1)
- TrisДокумент48 страницTrisisgaydioОценок пока нет
- Biowaiver Assessment for AcetazolamideДокумент9 страницBiowaiver Assessment for Acetazolamideمحمد فضل Fadhol RomdhoniОценок пока нет