Академический Документы
Профессиональный Документы
Культура Документы
Panosteitis
Загружено:
Umesh GopalanИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Panosteitis
Загружено:
Umesh GopalanАвторское право:
Доступные форматы
In: Textbook of Small Animal Orthopaedics, C. D. Newton and D. M. Nunamaker (Eds.) Publisher: International Veterinary Information Service (www.ivis.
org), Ithaca, New York, USA.
Canine Panosteitis ( 1-Jan-1985 )
T.M. Lenehan, D. C. Van Sickle and D. N. Biery
!
Clinical Presentation Radiographic Findings Etiology Pathobiology Treatment
Canine panosteitis is a spontaneously occurring, self-limiting disease of young, large breed dogs involving both the diaphyseal and metaphyseal areas of the tubular long bones. It is characterized by medullary fibrosis (enostosis), as well as by both endosteal and subperiosteal newbone deposition; affected animals are generally afflicted with an obscure, intermittent lameness affecting one or more limbs either simultaneously or sequentially.(l4) The disease was first described in the European veterinary literature in 1951 by Gratz(l9) and Bauman(2) as a chronic osteomyelitis (or eosinophilic panosteitis) of young German shepherd dogs. First described in the United States in 1960, the disease was soon noted epidemiologically to spread from New York through New England and into the Southeast,(1) probably as a result of a newly heightened practitioner awareness and unrelated to the spread of any etiologic agent. Originally believed to be a purulent hematogenous osteomyelitis caused by a streptococcus,(1-3,7,9,22) panosteitis was initially reported to be associated with tonsillitis and episodes of fever,(1,2,9,22,25) neither of which has been substantiated in subsequent investigations. The disease has been referred to in the veterinary literature as juvenile osteomyelitis,(2) enostosis,(5) eosinophilic panosteitis,(14) and canine panosteitis.(4) It appears to have no exact counterpart in humans.
CLINICAL PRESENTATION Canine panosteitis is a disease that affects only large or giant breeds, most often the German shepherd, although it has been reported in the bassett hound, Scottish terrier, Great Dane, St. Bernard, Doberman pinscher, German shorthaired pointer, Irish setter, Airedale, golden retriever, Labrador retriever, Samoyed, and miniature schnauzer.(1,4,9,10,12,14,17) Males are affected more commonly than females(1,5,10) (reported range 67%(6) to 84%(10)). The disease cycle in the long bones of males is more predictable and repeatable. The female usually has her first episode in association with her first estrus.(20) The average age at presentation is 5 to 12 months,(4-6,10,22,24) although German shepherds have been documented to have the disease as young as 2 months of age and as old as 5 years.(4) In one study, 20% of the animals were 18 months old at initial presentation.(4) The initial presenting complaint is usually an acute onset of lameness persisting for 2 to 14 days(1,4,20) with no current history of trauma. The disease begins in the bones of the forelegs, with the ulna being affected most often (42%), followed by the radius (25%), humerus (14%), femur (11%), and tibia (8%). The severity of these attacks becomes reduced and the interval between successive episodes increased with advancing age.(22) The degree of lameness usually increases during the first few days of an attack, remaining unaffected by either rest or exercise.(5) Periods of lameness are often accompanied by anorexia and lethargy. There may be a spontaneous regression of signs within 3 to 4 days with or without therapy,(22,23) however, more commonly the lameness is noted to shift from one limb to another every 2 to 3 weeks,(2,9,23) with occasional lapses of one month between episodes.4 In general, the pattern is from front limb to hind limb to recur again in the forelimb.
(20) Recurrence of the disease in a previously affected bone is seemingly rare;(2,22) however, in chronic cases the repeated occurrence of lesions can be found in the radius, followed by the ulna, with fewer repeats in the humerus and femur. The length of the cycle of disease is 90 days, but in some cases it extends to 160 to 190 days.(5,24) The interval between each skeletal cycle is 160 to 180 days. In one study, 53 of 100 dogs manifested multiple bone involvement, while 49 of 100 dogs showed multiple limb involvement on initial presentation.(4) As many as seven bones in various stages of disease have been observed to be affected during an episode in one dog. Clinical signs persist on an average of 2 to 9 months,(5,24) with the disease generally disappearing when the dog reaches 18 to 20 months of age. Physical examination is usually nonremarkable, since there is seldom an elevation in body temperature, muscle atrophy, or local hyperthermia. There is, however, pain upon firm palpation of the diaphyses of affected long bones; the pain is believed by some to be directly proportional to the amount of periosteal reaction present.(10) The degree of pain manifested clinically may range from slight to exquisite, with lameness being minimal to nonweight-bearing in severity. Since the pathologic bone formation occurs haphazardly in both time and location, multiple bones of the same limb or multiple limbs may be affected simultaneously; also, different phases of the disease may be occurring concurrently in any given animal.(4,11) Radiography is generally necessary to distinguish panosteitis from other disease conditions; however, the radiographic changes in early and late phases are subtle and far less distinct than those of mid-disease. It is generally rewarding to radiograph multiple long bones in an attempt to reveal more pronounced lesions.(4) It is important to realize, however, that generally there is no distinct relationship between the severity of radiologic changes, the amount of pain elicited on palpation, and the degree of lameness the animal manifests clinically (4,5,22)
RADIOGRAPHIC FINDINGS One or a combination of four radiographic abnormalities may be seen in panosteitis of the long tubular bones of the appendicular skeleton. The most common abnormality is an increased intramedullary radiopacity that may or may not have well-defined margins (Fig. 49-1). The increased opacity is usually hazy, demonstrating either a granular appearance or loss of the normal trabecular bony pattern. The increased medullary opacity usually is not prominent in the area of the nutrient canal of the bone. Additional radiographic findings that may be present with or without the medullary density include an endosteal bone thickening and a periosteal reaction. The periosteal new bone is usually smooth or laminar (Fig. 49-2). The least common radiographic finding is an increased radiolucency to the medullary portion of bone; this is the earliest radiographic abnormality that may be seen. FIG. 49-1 Medial-lateral radiographs of a humerus (A) and femur (B) demonstrate characteristic areas of increased medullary opacity.
FIG. 49-2 Cranial-caudal radiograph of a femur demonstrates periosteal elevation, sometimes seen with panosteitis.
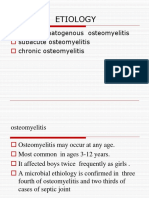
Panosteitis can often be seen concurrently with other disease processes. A differential diagnosis should include hypertrophic osteodystrophy, ununited anconeal/coronoid process, osteochondritis dissecans, hip dysplasia, trauma, osteomyelitis, nutritional secondary hyperparathyroidism, bicipital tenosynovitis, and olecranon bursitis. ETIOLOGY Although initially termed eosinophilic panosteitis by early authors(1,2,6,22) subsequent studies have failed to document consistent eosinophilias in affected animals during the acute phase of the disease (range 0%-50%).(1,4-6,9,10,15,20) Complete blood counts are generally within normal limits, as are levels of alkaline phosphatase, serum calcium, and serum phosphorus. Most dogs screened showed negative results when tested for intestinal parasites.
The few direct marrow and blood cultures that have been reported have uniformly been negative for aerobic and anaerobic bacteria, and histopathology has consistently failed to implicate any etiologic agent. The overall numbers of animals for whom these parameters have been published still remains low; however, such negative findings would seemingly be real in light of the usual absence of fever and normal white blood cell counts. The disease process and bony lesions have been believed by some to be indicative of an atypical viral osteomyelitis. One researcher stated that in preliminary studies, inocula had grown on bovine kidney cell culture. Other authors have purportedly accomplished artificial transmission of the disease via the intramedullary injection of both an unfiltered(10,22,24) and Seitz-filtered 10% suspension of affected bone marrow into young German shepherd dogs.(22,23) Controls were minimal, no generalized disease process reminiscent of canine panosteitis was produced, and only focal bone reactions resulted. More recently, an absence of cytopathic effect was noted when buffy coat and bone marrow inocula were taken from animals with active lesions and introduced into kidney cell lines; the same author also found an absence of second-degree intradermal delayed hypersensitivity reactions to the injection of biopsy material.(18)A genetic etiology would seem to be a factor since the German shepherd breed is disproportionately represented (86 of 100 animals in one study).(4,5,22) One investigator has reared German shepherd pups and English pointer pups together in the same pen, with only the German shepherds routinely manifesting the disease. He postulates a genetic predisposition with stress induction.(20) Other possible causes include transient vascular abnormalities,(l8)allergy,(8) a metabolic phenomenon (tubular long bones of growing males),(4,8) hyperestrinism(16), parasite migration, and possibly an autoimmune reaction following viral infection.(1)
PATHOBIOLOGY Canine panosteitis is a disease of the adipose bone marrow; it is often cyclic, and each episode is characterized by degeneration of medullary adipocytes followed by stromal cell proliferation, intramembranous ossification, removal of the medullary trabecular bone, and regeneration of the adipose bone marrow. While the etiology of the disease is unknown, stress can precipitate an episode of the disease. Radiographically, the lesion of canine panosteitis begins in the vicinity of the nutrient foramen of a long bone and is recognized by decreased medullary density (Fig. 49-3). FIG. 49-3 The radius and ulna of both forelimbs of a 5-month-old male German shepherd. The radius on the left is in the initial stages of panosteitis while the medullary cavity of the adjacent ulna is totally affected and the secondary periosteal reaction is evident on the caudal border. The medullary cavity of the right ulna appears to be clearing while the medullary cavity of the right radius is becoming increasingly radiodense and the periosteal reaction is evident.
FIG. 49-4 (A) Passive hyperemia in the bone marrow of a 6-month-old male German shephers with panosteitis. Note the accompanying osteoclasis of the trabeculae. (H&E x 316) (B) The medullay edema and capillary distension that accompany the reaction in A are thought to cause the pain associated with panosteitis. (H&E x 316)
Initially the area of the lesion is extremely sensitive to digital pressure. Histologically, there is an eosinophilic granular degeneration in the cytoplasm of the medullary adipocyte with eventual loss of the cell, leaving the latticelike stroma (Fig. 49-4). Next, there is a proliferation of the stromal and adventitial cells of the bone marrow in which intramembranous ossification occurs. Radiographically, this is recognized as a nidus and occurs 10 to 14 days after the initial clinical signs. The nidus enlarges, becoming attached secondarily to the endosteal surface and subsequently extending toward each metaphysis. The leading or peripheral edge of the nidus is composed of proliferating stromal cells and a few vessels behind which fibrous bony trabeculae are forming, while the center of the nidus is composed of lamellar bone trabeculae. The cells of the bone marrow of the nidus disappear, and the vascularity appears to be only capillaries and large venous sinuses. The ossification spreads linearly along the central medullary artery and vein with outlying bony satellites becoming incorporated into the central nidus. A periosteal reaction of linear trabeculae arranged perpendicularly to the long axis of the cortex and enclosing a vascular connective tissue appears secondary to the medullary osseous reaction (Fig. 49-5). By 20 to 30 days, the medullary diaphyseal density has reached the metaphysis; it has never been observed to extend into the epiphysis. During the osteogenesis of the medullary density, the fibrous bony trabeculae are replaced by lamellar bone trabeculae, the vascularity of the bone marrow is reestablished, and the bone marrow becomes hemopoietic. The cortical bone becomes more callus of midshaft fractures is the reaction of the injured adipose bone marrow. Research on the regeneration of bone marrow
following complete removal(13) or irradiation,(19) shows a proliferation of stromal cells, trabecular bone formation, reestablishment of the medullary vasculature resulting in a periosteal bone formation and enlarging of the osteons, and restoration of the histology of the original bone marrow type. Not only is the tissue pattern the same as in panosteitis but the chronology (90 days) is similar. FIG. 49-5 (A) The normal periosteum of a young dog. Note the cellular or osteogenic layer adjacent to the cortical bone (H&E x 200) (B) The secondary periosteal reaction of canine panosteitis. The hyperplasia of the cellular layer of the periosteum is evident as well as the newly formed bone arranged perpendicularly to the cortex. By comparing the osteon of the cortex with one in A, its enlargement by cutting bones is readily evident. (H&E x 90) (Van Sickle DC: Panosteitis. In Selected Orthopedic Problems in the Growing Dog. American Animal Hospital Association, 1975) FIG. 49-6 (A) The intense osteonal remodeling of the cortex that accompanies panosteitis. Note that the outer 25% of the cortex (next to the periosteum) is fiber bone resulting from the periosteal addition while the inner 50% is a mixture of lamellar and woven bone and the deepest 25% is all lamellar bone. (H&E x115) (s) An enlargement of an osteonal canal from the cortex seen in A. The vessels are congested and form a canalicular pattern around the canal. This latter characteristic is evidence of osteocytic osteolysis occurring during the course of panosteitis.(H&E x416)(VanSickle DC: Panosteitis. In Selected Orthopedic Problems in the Growing Dog. American Animal Hospital Association, l975)
TREATMENT Therapeutic regimens comprising antibiotics, vitamin and mineral supplements, dietary changes, and irradiation of diseased bones and adrenal glands have all been tried with little success.(1-21) More commonly, analgesics or antiinflammitants such as salicylates or phenylbutazone remain the first line of defense against pain. When these fail, corticosteroids (prednisolone) seem to have a beneficial effect in relieving pain and decreasing lameness in a fair number of animals.
REFERENCES
1. Barrett RB, Schall WD, Lewis RE: Clinical and radiographic features of canine eosinophilic panosteitis. Anim Hosp 4:94, 1968 2. Baumann R. Pommer A: Die chronische Osteomyelitis der jungen Schaferhunde. Wien Tierarztl Monatsschr 38:670, 1951 3. Berta S. Lance E: Mit verinehrung der eosinophilen zeuin einhergehende Osteomyelitis junger Hunde. Academiae Scintorum Hungorical Acta Vet XI:367, 1961 4. Bohning R. Suter PF, Hohn RB et al: Clinical and radiologic survey of canine panosteitis. J Am Vet Med Assoc 156:870, 1970 5. Burt, JK, Wilson, GP: A study of eosinophilic panosteitis (enostosis) in German Shepherd dogs. Acta Radiol (suppl)319: 7, 1972 6. Cotter SM, Griffiths RC, Leav I: Enostosis of young dogs. J Am Vet Med Assoc 153:401, 1968 7. Evers WH: Enostosis in a dog. J Am Vet Med Assoc 154:799, 1969 8. Gartner K: Klinische Beobachtungen an der eosinophilen Panosteitis der Junghunde. Kleintier-Prax 1:71, 1956 9. Gratzl E: Die eosinophile Panosteitis der Junghunde (Osteomyelitis der jungen Schaferhunde). Wien Tierarztl Monatsschr 38:629, 1951 10. Hardy WD, Stockman WS: Clinicopathologic conference. J Am Vet Med Assoc 154:1600, 1969 11. Kaastrom H. Olsson S-E, Suter PF: Panosteitis in the dog. Acta Radiol (suppl) 319:15, 1972 12. LaCroix JA: Diagnosis of orthopedic problems peculiar to the growing dog. Vet Med 65:229, 1970 13. Pratt HM, Maloney MA: Reconstitution of bone marrow in a depleted medullary cavity. In Stohlman F Jr (ed): Hemopoietic Cellular Proliferation, pp 5666. New York, Grune & Stratton, 1970 14. Riedesel DH: Eosinophilic panosteitis of young dogs. Iowa St Univ Vet 31:29, 1969 15. Schalm O: Veterinary Hematology, 2nd ed. Philadelphia, Lea & Febiger, 1965
16. Sprinkle TA, Krook L: Hip dysplasia, elbow dysplasia, and eosinophilic panosteitis: Three clinical manifestations of hyperestrinism in the dog. Cornel1 Vet 60:476, 1970 17. Tandy J. Haywood S: A case of panosteitis. Vet Rec 100:287, 1977 18. Turnier JC, Silverman S: A case study of canine panosteitis: Comparison of radiographic and radioisotopic studies. Am J Vet Res 39:1550, 1978 19. Van Dyke K, Harris N: Bone marrow reaction to trauma. Blood 34:257, 1969 20. Van Sickle D: Canine panosteitis. In Selected Orthopedic Problems in the Growing Dog, pp 20-28. Monograph, South Bend, American Animal Hospital Association, 1975 21. Whorton S. Eosinophilic panosteitis in the dog. Am J Vet Clin Pathol 2:241, 1968 22. Zeskov B: A contribution to eosinophilic panosteitis in dogs. Zentralbl Vet Med 7:671, 1960 23. Zeskov B: A contribution to eosinophilic panosteitis in German Shepherd dogs. Vet Archiv 32: 146, 1962 24. Zeskov B: Prilog eozinofilnom panesititisu u. njemackih ovcara. Doctoral Thesis, Veterinarskiarhiv, Zagreb Kryiga XXXII, Svezak 4-6, 146-149, 1962 25. Zeskov B. Marzan: Kronicni osteomielitis mladih njemackih ovacava (eosinofilni panostitis mladih pasa). Vet Archiv 27:129, 1957 All rights reserved. This document is available on-line at www.ivis.org. Document No. B0050.0685.
Вам также может понравиться
- Humanism oДокумент9 страницHumanism oCielo GarОценок пока нет
- Jeffrey Dahmer Case Study ConclusionДокумент2 страницыJeffrey Dahmer Case Study ConclusionBrian TiangcoОценок пока нет
- Bear Neuroscience: Exploring The Brain Chap 12 SlidesДокумент58 страницBear Neuroscience: Exploring The Brain Chap 12 SlidesAdrienne NgoОценок пока нет
- Trastornos Neuropsiquiátricos Autoinmunes Asociados A Infección Estreptocócica en La Edad Pediátrica: PANDASДокумент13 страницTrastornos Neuropsiquiátricos Autoinmunes Asociados A Infección Estreptocócica en La Edad Pediátrica: PANDASLuis Ruelas SanchezОценок пока нет
- Schizophrenia Jim Van Os, Shitij KapurДокумент13 страницSchizophrenia Jim Van Os, Shitij KapurMina100% (1)
- Marital Satisfaction Scale analysis reliability validity Mexican supervisorsДокумент27 страницMarital Satisfaction Scale analysis reliability validity Mexican supervisorsSantiago BohórquezОценок пока нет
- El Uso de La Técnica de Reestructuración Racional Sistémica de Goldfried y Goldfried en Un Caso de Ansiedad de EvaluaciónДокумент2 страницыEl Uso de La Técnica de Reestructuración Racional Sistémica de Goldfried y Goldfried en Un Caso de Ansiedad de EvaluaciónRicardo NoyolaОценок пока нет
- Mr. Jones Bipolar Disorder Case StudyДокумент3 страницыMr. Jones Bipolar Disorder Case StudyCamille SindayОценок пока нет
- Amnanesis JanyДокумент19 страницAmnanesis JanyJosé Manuel Guerrero Barboza100% (2)
- PanosteitisДокумент5 страницPanosteitisElEffe100% (1)
- Enfermedad de Desarrollo 2Документ25 страницEnfermedad de Desarrollo 2Andi Dytha Pramitha SamОценок пока нет
- Glander-Farcy - Reemerging Disease - Eq. Vet. Edu. 2009Документ2 страницыGlander-Farcy - Reemerging Disease - Eq. Vet. Edu. 2009Muhammad SaqibОценок пока нет
- Calvarial Tuberculosis: A Rare Form of Tuberculous OsteitisДокумент2 страницыCalvarial Tuberculosis: A Rare Form of Tuberculous Osteitiskbianca26Оценок пока нет
- Signs and Symptoms: Pott's Disease Is A Presentation of ExtrapulmonaryДокумент48 страницSigns and Symptoms: Pott's Disease Is A Presentation of ExtrapulmonaryNem AkoОценок пока нет
- Diagnosticimagingof Discospondylitis: Catherine M. Ruoff,, Sharon C. Kerwin,, Amanda R. TaylorДокумент10 страницDiagnosticimagingof Discospondylitis: Catherine M. Ruoff,, Sharon C. Kerwin,, Amanda R. TaylorIngrid MachadoОценок пока нет
- CANINE-Hypertrophic Osteodystrophy and Calvarial HyperostosisДокумент7 страницCANINE-Hypertrophic Osteodystrophy and Calvarial Hyperostosistaner_soysurenОценок пока нет
- Bartonella henselae infection causes abscess-forming lymphadenopathy and osteomyelitis in childrenДокумент7 страницBartonella henselae infection causes abscess-forming lymphadenopathy and osteomyelitis in childrenJosé RojasОценок пока нет
- Pathologyofdiseasesof Geriatricexoticmammals: Drury R. Reavill,, Denise M. ImaiДокумент34 страницыPathologyofdiseasesof Geriatricexoticmammals: Drury R. Reavill,, Denise M. ImaiRaquel MotaОценок пока нет
- Pott'S Disease: Partial Fulfilment in Orthopaedic Nursing de Ramos, Mary Grace L. Bsn-Iii March 08, 2013Документ6 страницPott'S Disease: Partial Fulfilment in Orthopaedic Nursing de Ramos, Mary Grace L. Bsn-Iii March 08, 2013Mary Grace de RamosОценок пока нет
- Descricion ofДокумент5 страницDescricion ofLlrss AdnОценок пока нет
- Bedin 2007Документ3 страницыBedin 2007erzebeth bathoryОценок пока нет
- Case ReportДокумент4 страницыCase ReportbejoОценок пока нет
- Canine Choroid Plexus Tumor With Intracranial Dissemination Presenting As Multiple Cystic LesionsДокумент5 страницCanine Choroid Plexus Tumor With Intracranial Dissemination Presenting As Multiple Cystic LesionsMihai SavescuОценок пока нет
- JZWM Jan 2010Документ7 страницJZWM Jan 2010llcoffeeОценок пока нет
- Hasan2004 PDFДокумент2 страницыHasan2004 PDFspin_echoОценок пока нет
- Infectious Agents Identified With Multifocal Interstitial Nephritis at SlaughterДокумент6 страницInfectious Agents Identified With Multifocal Interstitial Nephritis at SlaughterNicolas Carrillo GodoyОценок пока нет
- The Skeletal Effects of Congenital Syphilis: The Case of Parrot 'S BonesДокумент11 страницThe Skeletal Effects of Congenital Syphilis: The Case of Parrot 'S Boneslink_wolfloboОценок пока нет
- Pott Disease (Tuberculous Spondylitis) : FrequencyДокумент9 страницPott Disease (Tuberculous Spondylitis) : FrequencyChris EdenОценок пока нет
- Vaccination-Savage1995 Cotton Top Tamarin PDFДокумент5 страницVaccination-Savage1995 Cotton Top Tamarin PDFToha PutraОценок пока нет
- Ehrlichiosis in DogsДокумент3 страницыEhrlichiosis in DogsMarisol AsakuraОценок пока нет
- Pott's Disease Is A Presentation of ExtrapulmonaryДокумент13 страницPott's Disease Is A Presentation of ExtrapulmonaryJc HarharОценок пока нет
- Brucellosis in horses causes fistulous withers and poll evilДокумент6 страницBrucellosis in horses causes fistulous withers and poll evilMaceface JimenezОценок пока нет
- Huxsoll 1976Документ12 страницHuxsoll 1976Paula Andrea Castro MartinezОценок пока нет
- Spinal Epidural Abscess in Two CalvesДокумент8 страницSpinal Epidural Abscess in Two CalvesRachel AutranОценок пока нет
- CoccocidiopsisДокумент10 страницCoccocidiopsisMoises PinedaОценок пока нет
- Arthritis in Cats-Diagnosis, Relevance and TratmentДокумент3 страницыArthritis in Cats-Diagnosis, Relevance and TratmentLaura Carolina Moreno RestrepoОценок пока нет
- Pott Disease (TB Spondylitis) (Emed)Документ7 страницPott Disease (TB Spondylitis) (Emed)Ali Al.JuffairiОценок пока нет
- Tuberculosis Spondylitis IIДокумент40 страницTuberculosis Spondylitis IICendraiin MinangkabauОценок пока нет
- A Retrospective Histopathological Survey On Canine and Feline Liver Diseases at The University of Tokyo Between 2006 and 2012Документ6 страницA Retrospective Histopathological Survey On Canine and Feline Liver Diseases at The University of Tokyo Between 2006 and 2012Flaviu TabaranОценок пока нет
- USPancreas DR GomaaДокумент14 страницUSPancreas DR GomaaFlavio RibeiroОценок пока нет
- Bone Infection in The Bovine Appendicular Skeleton: A Clinical, Radiographic, and Experimental StudyДокумент11 страницBone Infection in The Bovine Appendicular Skeleton: A Clinical, Radiographic, and Experimental Studymari combsОценок пока нет
- Ajr 127 5 789Документ4 страницыAjr 127 5 789Egi Patnialdi Firda PermanaОценок пока нет
- SJS (Jurnal)Документ6 страницSJS (Jurnal)FerryRoferdiОценок пока нет
- Van Buchem DiseaseДокумент9 страницVan Buchem DiseaseZehra UrunОценок пока нет
- Petton 2021 Frontiers Pacific MANUSCRIT2Документ26 страницPetton 2021 Frontiers Pacific MANUSCRIT2AmadorRevillaОценок пока нет
- cmo-ebookДокумент5 страницcmo-ebookDiana Rahmayani PutriОценок пока нет
- Elderly:: Tuberculous Spondylitis A Potential Diagnostic PitfaliДокумент2 страницыElderly:: Tuberculous Spondylitis A Potential Diagnostic PitfaliKristian Lihardo GirsangОценок пока нет
- Etiology: Acute Hematogenous Osteomyelitis Subacute Osteomyelitis Chronic OsteomyelitisДокумент42 страницыEtiology: Acute Hematogenous Osteomyelitis Subacute Osteomyelitis Chronic OsteomyelitisNoe-pal DynmОценок пока нет
- POTT's DiseaseДокумент3 страницыPOTT's DiseaseFema Jill AtrejenioОценок пока нет
- Penyakit Pada IkanДокумент16 страницPenyakit Pada IkanKoleta Tresi RosariОценок пока нет
- Linguatula Serrata Tongue Worm in Human Eye, Austria: Emerging Infectious Diseases May 2011Документ4 страницыLinguatula Serrata Tongue Worm in Human Eye, Austria: Emerging Infectious Diseases May 2011Nona Hidayati MaghfirahОценок пока нет
- Intoxicación Por VoriconazolДокумент2 страницыIntoxicación Por VoriconazolMariana fotos FotosОценок пока нет
- A Rare Case of Papillon-Lefevre Syndrome: A Case ReportДокумент4 страницыA Rare Case of Papillon-Lefevre Syndrome: A Case ReportIJAR JOURNALОценок пока нет
- Echinococcosis Review: Causes, Symptoms, and TreatmentДокумент9 страницEchinococcosis Review: Causes, Symptoms, and TreatmentAmalia Nur LatifahОценок пока нет
- Universa MedicaДокумент11 страницUniversa Medicarido eledОценок пока нет
- Clinical Microbiology and Infection: A. Mailles, J.-P. Stahl, K.C. BlochДокумент7 страницClinical Microbiology and Infection: A. Mailles, J.-P. Stahl, K.C. BlochgugicevdzoceОценок пока нет
- Review FIP 1963-2022 Final Version April 2022 - 0Документ41 страницаReview FIP 1963-2022 Final Version April 2022 - 0Weiwei CierraОценок пока нет
- CANINE-CAnine Systemic Lupus Erythematosus - Part IДокумент7 страницCANINE-CAnine Systemic Lupus Erythematosus - Part Itaner_soysurenОценок пока нет
- Leptospirosis:: A Waterborne Zoonotic Disease of Global ImportanceДокумент4 страницыLeptospirosis:: A Waterborne Zoonotic Disease of Global ImportanceMuhFarizaAudiОценок пока нет
- 1 s2.0 S8756328221003938 MainДокумент10 страниц1 s2.0 S8756328221003938 MainPoramate PITAK-ARNNOPОценок пока нет
- Identification of Three Novel Mycoplasma Species From Ostriches in South AfricaДокумент11 страницIdentification of Three Novel Mycoplasma Species From Ostriches in South AfricaUmesh GopalanОценок пока нет
- Pathophysiology of DMДокумент1 страницаPathophysiology of DMUmesh GopalanОценок пока нет
- General Systemic StatesДокумент16 страницGeneral Systemic StatesUmesh GopalanОценок пока нет
- Brachycephalic Syndrome in DogsДокумент7 страницBrachycephalic Syndrome in DogsUmesh GopalanОценок пока нет
- Ultrasound of Urogenital TractДокумент9 страницUltrasound of Urogenital TractUmesh GopalanОценок пока нет
- Polioencephalomalacia in GoatsДокумент20 страницPolioencephalomalacia in GoatsUmesh GopalanОценок пока нет
- Pv0212 Mace CeДокумент0 страницPv0212 Mace CeCarlos Ruben BlancoОценок пока нет
- Emergency Fluid Therapy in Companion Animals - PPitneyДокумент9 страницEmergency Fluid Therapy in Companion Animals - PPitneyUmesh GopalanОценок пока нет
- Your Dog's Lab Tests DecodedДокумент3 страницыYour Dog's Lab Tests DecodedUmesh GopalanОценок пока нет
- ColapsoДокумент10 страницColapsoRoberta ResendeОценок пока нет
- Understanding Labwork ValuesДокумент3 страницыUnderstanding Labwork ValuesUmesh GopalanОценок пока нет
- Canine GlomerulonephritisДокумент10 страницCanine GlomerulonephritisUmesh GopalanОценок пока нет
- Cyanide PoisonsДокумент22 страницыCyanide PoisonsUmesh Gopalan0% (1)
- Heat StrokeДокумент5 страницHeat StrokeUmesh GopalanОценок пока нет
- Anesthesia Guidelines For Dogs and CatsДокумент9 страницAnesthesia Guidelines For Dogs and CatsNatalie KingОценок пока нет
- Peritoneal Dialysis in CatsДокумент6 страницPeritoneal Dialysis in CatsUmesh GopalanОценок пока нет
- Cytology of The LiverДокумент3 страницыCytology of The LiverUmesh GopalanОценок пока нет
- CANINE-Pathophysiology and Management of Canine Colonic DiseasesДокумент14 страницCANINE-Pathophysiology and Management of Canine Colonic Diseasestaner_soysuren100% (1)
- Feline Idiopathic CystitisДокумент4 страницыFeline Idiopathic CystitisUmesh GopalanОценок пока нет
- Albumin in Health and Disease: Protein Metabolism and FunctionДокумент7 страницAlbumin in Health and Disease: Protein Metabolism and FunctionAlexis AvendañoОценок пока нет
- Lodha GroupДокумент2 страницыLodha Groupmanish_ggiОценок пока нет
- Fisher - Techincal Monograph 42 - Understanding DecibelsДокумент8 страницFisher - Techincal Monograph 42 - Understanding Decibelsleslie.lp2003Оценок пока нет
- Deviser TV Analyser S7000: Bagian 1: Fungsi AnalyzerДокумент15 страницDeviser TV Analyser S7000: Bagian 1: Fungsi AnalyzerAlexander WieseОценок пока нет
- CP302 Example 01 OKДокумент5 страницCP302 Example 01 OKAw Yeong Pei Yee100% (1)
- Unit 5 EstándarДокумент2 страницыUnit 5 EstándardechillbroОценок пока нет
- Grab E-Receipt for 15,000 RP Ride on March 30Документ1 страницаGrab E-Receipt for 15,000 RP Ride on March 30WellyОценок пока нет
- Map Project Rubric 2018Документ2 страницыMap Project Rubric 2018api-292774341Оценок пока нет
- A Review of The Management of Cerebral Vasospasm After Aneurysmal Subarachnoid HemorrhageДокумент15 страницA Review of The Management of Cerebral Vasospasm After Aneurysmal Subarachnoid HemorrhageAlanОценок пока нет
- Bahasa Inggris Kelas XIIДокумент2 страницыBahasa Inggris Kelas XIIMuhammad ImadudinОценок пока нет
- Syllabus PTSV3Документ21 страницаSyllabus PTSV3Pablito Quispe RuizОценок пока нет
- 02 1 Cohen Sutherland PDFДокумент3 страницы02 1 Cohen Sutherland PDFSarra AnitaОценок пока нет
- F FS1 Activity 3 EditedДокумент15 страницF FS1 Activity 3 EditedRayshane Estrada100% (1)
- Henoch Schönlein PurpuraДокумент12 страницHenoch Schönlein PurpuraRavania Rahadian Putri100% (1)
- FIL M 216 2nd Yer Panitikan NG PilipinasДокумент10 страницFIL M 216 2nd Yer Panitikan NG PilipinasJunas LopezОценок пока нет
- Assessmentof Safety Cultureand Maturityin Mining Environments Caseof Njuli QuarryДокумент12 страницAssessmentof Safety Cultureand Maturityin Mining Environments Caseof Njuli QuarryAbdurrohman AabОценок пока нет
- USP FriabilityДокумент2 страницыUSP Friabilityshdph100% (1)
- The Manning EquationДокумент10 страницThe Manning EquationFederico LeonОценок пока нет
- Inna Phos Diammonium Phosphate MSDSДокумент9 страницInna Phos Diammonium Phosphate MSDSjosephОценок пока нет
- Atlas Ci30002Tier-PropanДокумент3 страницыAtlas Ci30002Tier-PropanMarkus JeremiaОценок пока нет
- Mercury Poisoning Symptoms and TreatmentsДокумент1 страницаMercury Poisoning Symptoms and TreatmentsRakheeb BashaОценок пока нет
- Altered Ventilatory Function Assessment at Pamantasan ng CabuyaoДокумент27 страницAltered Ventilatory Function Assessment at Pamantasan ng Cabuyaomirai desuОценок пока нет
- Computer ViruesДокумент19 страницComputer ViruesMuhammad Adeel AnsariОценок пока нет
- Rolls-Royce M250 FIRST Network: 2015 Customer Support DirectoryДокумент76 страницRolls-Royce M250 FIRST Network: 2015 Customer Support Directoryale11vigarОценок пока нет
- Armv8-A Instruction Set ArchitectureДокумент39 страницArmv8-A Instruction Set ArchitectureraygarnerОценок пока нет
- FacebookH Cking 1 3 (SFILEДокумент10 страницFacebookH Cking 1 3 (SFILEFitra AkbarОценок пока нет
- BOOK-Deva-Oracle MaterialДокумент177 страницBOOK-Deva-Oracle MaterialPAVANN TОценок пока нет
- Community HelpersДокумент3 страницыCommunity Helpersapi-252790280100% (1)
- Ed Brown CatalogДокумент44 страницыEd Brown CatalogssnvetОценок пока нет
- Inner Unit EstimateДокумент35 страницInner Unit EstimateMir MoОценок пока нет
- BC Sample Paper-3Документ4 страницыBC Sample Paper-3Roshini AОценок пока нет
- Roxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueОт EverandRoxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueРейтинг: 5 из 5 звезд5/5 (3)
- Roxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueОт EverandRoxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueРейтинг: 5 из 5 звезд5/5 (21)
- Inside of a Dog: What Dogs See, Smell, and KnowОт EverandInside of a Dog: What Dogs See, Smell, and KnowРейтинг: 4 из 5 звезд4/5 (390)
- Will's Red Coat: The Story of One Old Dog Who Chose to Live AgainОт EverandWill's Red Coat: The Story of One Old Dog Who Chose to Live AgainРейтинг: 4.5 из 5 звезд4.5/5 (18)
- Show Dog: The Charmed Life and Trying Times of a Near-Perfect PurebredОт EverandShow Dog: The Charmed Life and Trying Times of a Near-Perfect PurebredРейтинг: 3.5 из 5 звезд3.5/5 (13)
- An Eagle Named Freedom: My True Story of a Remarkable FriendshipОт EverandAn Eagle Named Freedom: My True Story of a Remarkable FriendshipОценок пока нет
- Alex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessОт EverandAlex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessОценок пока нет
- Dogland: Passion, Glory, and Lots of Slobber at the Westminster Dog ShowОт EverandDogland: Passion, Glory, and Lots of Slobber at the Westminster Dog ShowОценок пока нет
- How To Speak Dog: Mastering the Art of Dog-Human CommunicationОт EverandHow To Speak Dog: Mastering the Art of Dog-Human CommunicationРейтинг: 4 из 5 звезд4/5 (66)
- The Dog Who Couldn't Stop Loving: How Dogs Have Captured Our Hearts for Thousands of YearsОт EverandThe Dog Who Couldn't Stop Loving: How Dogs Have Captured Our Hearts for Thousands of YearsОценок пока нет
- The Other End of the Leash: Why We Do What We Do Around DogsОт EverandThe Other End of the Leash: Why We Do What We Do Around DogsРейтинг: 5 из 5 звезд5/5 (64)
- The Dog Listener: Learn How to Communicate with Your Dog for Willing CooperationОт EverandThe Dog Listener: Learn How to Communicate with Your Dog for Willing CooperationРейтинг: 4 из 5 звезд4/5 (37)
- Come Back, Como: Winning the Heart of a Reluctant DogОт EverandCome Back, Como: Winning the Heart of a Reluctant DogРейтинг: 3.5 из 5 звезд3.5/5 (10)
- Talking to Animals: How You Can Understand Animals and They Can Understand YouОт EverandTalking to Animals: How You Can Understand Animals and They Can Understand YouРейтинг: 4.5 из 5 звезд4.5/5 (18)
- Meet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorОт EverandMeet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorРейтинг: 5 из 5 звезд5/5 (34)
- Arthur: The Dog Who Crossed the Jungle to Find a HomeОт EverandArthur: The Dog Who Crossed the Jungle to Find a HomeРейтинг: 4.5 из 5 звезд4.5/5 (19)
- Your Dog Is Your Mirror: The Emotional Capacity of Our Dogs and OurselvesОт EverandYour Dog Is Your Mirror: The Emotional Capacity of Our Dogs and OurselvesРейтинг: 4 из 5 звезд4/5 (31)
- Puppy Training 101: How to Train a Puppy, Training Your Own Psychiatric Service Dog, A Step-By-Step Program so your Pup Will Understand You!От EverandPuppy Training 101: How to Train a Puppy, Training Your Own Psychiatric Service Dog, A Step-By-Step Program so your Pup Will Understand You!Рейтинг: 5 из 5 звезд5/5 (85)
- The Wrong Dog: An Unlikely Tale of Unconditional LoveОт EverandThe Wrong Dog: An Unlikely Tale of Unconditional LoveРейтинг: 4.5 из 5 звезд4.5/5 (26)
- Lessons from Tara: Life Advice from the World's Most Brilliant DogОт EverandLessons from Tara: Life Advice from the World's Most Brilliant DogРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Meet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorОт EverandMeet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorРейтинг: 5 из 5 звезд5/5 (1)
- Arthur: The Dog who Crossed the Jungle to Find a HomeОт EverandArthur: The Dog who Crossed the Jungle to Find a HomeРейтинг: 4.5 из 5 звезд4.5/5 (16)
- Edward's Menagerie: Dogs: 50 canine crochet patternsОт EverandEdward's Menagerie: Dogs: 50 canine crochet patternsРейтинг: 3 из 5 звезд3/5 (5)