Академический Документы
Профессиональный Документы
Культура Документы
Reading - What Would Osler Do
Загружено:
SFLAccipiterИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Reading - What Would Osler Do
Загружено:
SFLAccipiterАвторское право:
Доступные форматы
PERS PE C T IV E BECOMING A PHYSICIAN
What Would Osler Do? Learning from Difficult Patients
What Would Osler Do? Learning from Difficult Patients
Michael W. Kahn, M.D. y intern cant stand Ms. Andrews and refuses to meet with her. He says Ill do all the communicating for the team and that I shouldnt be too nice to her so she wont split us. The attending says shes a classic borderline. So began a students presentation on Difficult Patient Rounds, my unofficial name for an exercise I started a few years ago with groups of four to five third-year students during their medicine clerkship. As a psychiatrist and card-carrying biopsychosocialist, I wanted to offer students some practical tips for working with patients who drove their caregivers to distraction. On this particular day, that description applied to Ms. Andrews, who was distressingly familiar to the medical service. Homeless and addicted to drugs and alcohol, she had terrible coping skills, a nasty temper, and a habit of leaving against medical advice after tormenting everyone for a few miserable days. Admitted yet again for pancreatitis, she was doing battle as usual over dilaudid and cigarettes. We spent half an hour trying to discover what made her tick. We structured the interviews for this exercise around two tasks. The first was to allow patients to vent about being in the hospital in Ms. Andrewss case, about everyones colossal incompetence and stupidity. The second was to find answers to the following questions: Where do you live and with whom? Who are the important people in your life? How do you spend your time? What gives you pleasure?
442
Ms. Andrews told us about having been physically, psychologically, and sexually abused by her drug-addicted parents and in serial foster homes; how teenage prostitution and crime had helped support her own habit; and how much she missed her two children, who had been taken away by the state. She explained why some people prefer living on the streets to staying in shelters, that cocaine helped her mood more than sertraline, and that she loved horror movies and Stephen King novels. She seemed glad to be able to talk without fighting. The students asked a few respectful questions that Ms. Andrews answered patiently. We thanked her and left to discuss the interview. The student who had presented her case commented that he hadnt realized that if Ms. Andrews was allowed to curse like a drill sergeant for 30 seconds or so, the wind would leave the sails of her hostility and she could actually have a sharp sense of humor. All the students seemed a bit shaken by the rather horrendous extent of her abuse history, but it clearly evoked compassion rather than revulsion. She seemed less the so-called classic borderline case than a person who came by her very difficult behavior honestly. One student asked whether all we had done was to get her to idealize us, as alleged borderlines are supposed to do. I didnt think she had idealized us so much as she had chosen not to fight with us a significant difference. Of course, we had the luxury of not having to negotiate
a cigarette break with her, but I think the students saw that successful negotiation begins with some basic understanding of the other sides position. I hoped they also saw that I had done nothing mysteriously psychiatric in the interview and that there was no reason why they couldnt do what I had done, given time and practice. Ms. Andrewss impossible behavior had become more intelligible, and the students learned that there were ways to begin collaborating with patients who have trouble doing so. We got some follow-up on Ms. Andrews at our meeting the next week. The medical student had informed the rest of the care team about the psychosocial background we had discovered, most of which had come as a surprise to them. Ms. Andrews had continued in her difficult ways but with much less intensity. Since she now knew that her caregivers knew something about the hell her life had been (and still was), she could afford to curb her antagonism and allow others to feel some sympathy for her. The intern still employed the student as the primary ambassador of medical care but with less worry that compassionate behavior on the students part would somehow undermine the teams purpose. Difficult Patient Rounds exposed students to the variety of settings in which clinicians feel like pulling out their hair. We found a more palatable side to the insufferably narcissistic patient and saw how the manipulative charm of the more sociopathic one could be leveraged
n engl j med 361;5
nejm.org
july 30, 2009
The New England Journal of Medicine Downloaded from nejm.org at FLAMEDLIB on August 26, 2011. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
PE R S PE C T IV E
What Would Osler Do? Learning from Difficult Patients
toward an alliance based less on lies and more on shared goals. When the students didnt have a behaviorally difficult patient on service, wed focus on one whose case exemplified what could be called the psychiatry of everyday medicine: those issues of competency, depression, suicidality, delirium, and so forth that are ubiquitous on every clinical service but are often seen as troublesome distractions in treatment. Such patients provided a reliable stream of teachable moments. Students found the exercise useful for at least three reasons: it allowed them to learn advanced tactical interviewing skills at the bedside, it demystified common psychiatric concepts, and it provided a more strategic perspective on engaging and better under-
standing a wide range of patients. Sometimes we would interview a patient who just seemed interesting: the homeless man with a large community of friends, the delusional woman with a number of outlandish convictions, the Holocaust survivor who still had a zest for living. In each case, we could discover the psychosocial equivalent of egophony or pulsus paradoxus: fascinating aspects of the patient, readily seen if you know how and where to look for them. Osler wrote long ago that it is much more important to know what sort of a patient has a disease than what sort of a disease a patient has. To modern ears, this assertion can unfortunately sound like irrelevant high-mind-
edness from a vanished era rather than a principle that can tangibly improve patient care and professional satisfaction. I dont know what Osler actually did to determine what sort of a patient has a disease, but holding rounds on behaviorally difficult patients is one way to show the usefulness of his principle. These rounds can demonstrate the immediate payoff of knowing even a little bit about a patients life. Lose that knowledge, and we risk becoming more technician than clinician.
(The patients name and identifying details have been changed to protect her privacy.) No potential conflict of interest relevant to this article was reported. From the Beth Israel Deaconess Medical Center and Harvard Medical School both in Boston.
Copyright 2009 Massachusetts Medical Society.
n engl j med 361;5
nejm.org
july 30, 2009
443
The New England Journal of Medicine Downloaded from nejm.org at FLAMEDLIB on August 26, 2011. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- SHCДокумент81 страницаSHCEng Mostafa ElsayedОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- 05 x05 Standard Costing & Variance AnalysisДокумент27 страниц05 x05 Standard Costing & Variance AnalysisMary April MasbangОценок пока нет
- Pavement Design1Документ57 страницPavement Design1Mobin AhmadОценок пока нет
- Career Level Diagram - V5Документ1 страницаCareer Level Diagram - V5Shivani RaikwarОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Dtu Placement BrouchureДокумент25 страницDtu Placement BrouchureAbhishek KumarОценок пока нет
- Chemistry: Crash Course For JEE Main 2020Документ18 страницChemistry: Crash Course For JEE Main 2020Sanjeeb KumarОценок пока нет
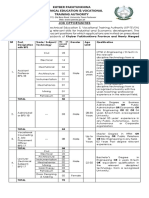
- KP Tevta Advertisement 16-09-2019Документ4 страницыKP Tevta Advertisement 16-09-2019Ishaq AminОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Chapter3 Elasticity and ForecastingДокумент25 страницChapter3 Elasticity and ForecastingGee JoeОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Anatomy Anal CanalДокумент14 страницAnatomy Anal CanalBela Ronaldoe100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- 1.technical Specifications (Piling)Документ15 страниц1.technical Specifications (Piling)Kunal Panchal100% (2)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Negotiating Skills Negotiating Skills: To Provide You With The Skills To Plan & Implement Successful NegotiationДокумент32 страницыNegotiating Skills Negotiating Skills: To Provide You With The Skills To Plan & Implement Successful NegotiationKanimozhi.SОценок пока нет
- Thermally Curable Polystyrene Via Click ChemistryДокумент4 страницыThermally Curable Polystyrene Via Click ChemistryDanesh AzОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Origami Oso HormigueroДокумент9 страницOrigami Oso HormigueroRogelio CerdaОценок пока нет
- WEB DESIGN WITH AUSTINE-converted-1Документ9 страницWEB DESIGN WITH AUSTINE-converted-1JayjayОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Monergism Vs SynsergismДокумент11 страницMonergism Vs SynsergismPam AgtotoОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Jesus Prayer-JoinerДокумент13 страницJesus Prayer-Joinersleepknot_maggotОценок пока нет
- AnticyclonesДокумент5 страницAnticyclonescicileanaОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Mantel Colonized Nation Somalia 10 PDFДокумент5 страницThe Mantel Colonized Nation Somalia 10 PDFAhmad AbrahamОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- 2009 2011 DS Manual - Club Car (001-061)Документ61 страница2009 2011 DS Manual - Club Car (001-061)misaОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Agnes de MilleДокумент3 страницыAgnes de MilleMarie-Maxence De RouckОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Turning PointsДокумент2 страницыTurning Pointsapi-223780825Оценок пока нет
- Hdfs Default XML ParametersДокумент14 страницHdfs Default XML ParametersVinod BihalОценок пока нет
- Tribal Banditry in Ottoman Ayntab (1690-1730)Документ191 страницаTribal Banditry in Ottoman Ayntab (1690-1730)Mahir DemirОценок пока нет
- Working With Difficult People Online WorksheetДокумент4 страницыWorking With Difficult People Online WorksheetHugh Fox IIIОценок пока нет
- A Case Study Puga Geothermal System,: OF IndiaДокумент7 страницA Case Study Puga Geothermal System,: OF IndiaPERIKALA TARUNОценок пока нет
- DarcДокумент9 страницDarcJunior BermudezОценок пока нет
- Snapdragon 435 Processor Product Brief PDFДокумент2 страницыSnapdragon 435 Processor Product Brief PDFrichardtao89Оценок пока нет
- Business Plan 3.3Документ2 страницыBusiness Plan 3.3Rojin TingabngabОценок пока нет
- Functions in C++Документ23 страницыFunctions in C++Abhishek ModiОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Post Appraisal InterviewДокумент3 страницыPost Appraisal InterviewNidhi D100% (1)