Академический Документы
Профессиональный Документы
Культура Документы
Findings From The WHI Postmenopausal Hormone Therapy Trials
Загружено:
tharinduusИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Findings From The WHI Postmenopausal Hormone Therapy Trials
Загружено:
tharinduusАвторское право:
Доступные форматы
The National Institutes of Health (NIH) established the Women's Health Initiative (WHI) in 1991 to address the most
common causes of death, disability and impaired quality of life in postmenopausal women. The WHI addressed cardiovascular disease, cancer, and osteoporosis. The WHI was a 15 year multi-million dollar endeavor, and one of the largest U.S. prevention studies of its kind. The three major components of the WHI were: a randomized controlled clinical trial of promising but unproven approaches to prevention; an observational study to identify predictors of disease; a study of community approaches to developing healthful behaviors.
Findings from the WHI Postmenopausal Hormone Therapy Trials The WHI was launched in 1991 and consisted of a set of clinical trials and an observational study, which together involved 161,808 generally healthy postmenopausal women. The clinical trials were designed to test the effects of postmenopausal hormone therapy, diet modification, and calcium and vitamin D supplements on heart disease, fractures, and breast and colorectal cancer. The hormone trial had two studies: the estrogen-plus-progestin study of women with a uterus and the estrogenalone study of women without a uterus. (Women with a uterus were given progestin in combination with estrogen, a practice known to prevent endometrial cancer.) In both hormone therapy studies, women were randomly assigned to either the hormone medication being studied or to placebo. Those studies have now ended. The women in these studies are now participating in a follow-up phase, which will last until 2010. The Estrogen-Alone Study The Estrogen-Plus-Progestin Study Oral Contraceptives and Cardiovascular Disease
The Estrogen-Alone Study 1. Effects of Conjugated Equine Estrogens on Breast Cancer and Mammography in Postmenopausal Women with Hysterectomy
Findings from the E-Alone trial show that women with prior hysterectomy do NOT have an increased risk of breast cancer for at least 7 years after starting estrogen-alone (CEE). In contrast, findings from the E+P trial show that women with a uterus who used combined estrogen and progestin had an increased risk of breast cancer by 5 years. These findings suggest that CEE alone is safer in regard to breast cancer than combined estrogen plus progestin, at least in the short term for women who have a hysterectomy and, therefore, would not be prescribed a progestin. A womans individual decision about hormone therapy should take into account her risk profile for breast cancer and other diseases that might be affected by hormones (such as stroke, heart disease, blood clots, and hip fractures). 2. Estrogen Therapy and Coronary Artery Calcification
In summary, they have looked at the effect of estrogen on coronary artery calcium among women who were aged 50-59 when they joined the WHI estrogen-alone trial. After the trial was stopped, the calcium plaque build-up in the coronary arteries was lower in women randomized to estrogen compared to placebo. However, estrogen has complex biological effects and may affect a womans risk of heart disease and other health outcomes in many different ways.
The Estrogen-Plus-Progestin Study 1) Health Risks and Benefits 3 Years After Stopping Randomized Treatment With Estrogen and Progestin Based on the findings mentioned above, the studys global index that summarized risk and benefits was unchanged, showing that the health risks exceeded the health benefits from the beginning of the study through the end of this three year follow-up. The follow-up after stopping estrogen plus progestin confirms the studys main conclusion that combination hormone therapy (E+P) should not be used to prevent disease in healthy, postmenopausal women. The most important message to women who have stopped this hormone therapy is to continue seeing their physicians for rigorous prevention and screening activities for all important preventable health conditions 2) Estrogen plus Progestin Effects on Breast Cancer and Mammograms The increased risk of breast cancer due to E+P was eight additional cases of breast cancer for every 10,000 women over one year Overall, there was a 24% increase in the risk for breast cancer due to E+P The breast cancers in the E+P group had similar characteristics (looked the same under a microscope) to those in the placebo group. However, the tumors in the E+P group tended to be larger and more advanced (had spread to the lymph nodes or elsewhere in the body). A more advanced stage is usually associated with poorer outcome. At this time, no direct statements can be made about the prognosis of the breast cancer found in women taking E+P until more follow-up information is collected. After even one year, quite a few more women had abnormal mammograms in the E+P group (9.4%) compared to the placebo group (5.4%); this pattern continued until the study ended. An abnormal mammogram is a breast X-ray that results in a recommendation for additional medical evaluation (most often, a shorter time between mammograms, but sometimes, a breast biopsy or other tests). Although we have known from other studies that E+P use increases the density of breast tissue on mammograms, the increase in abnormal mammograms with E+P use seen in this study is a new finding. Further WHI studies are being done to learn what happens to breast cancer rates and mammograms after E+P use is stopped. 3) Estrogen plus Progestin Effects on Bone Density and the Risk of Fractures Overall, there was a 24% reduction in all fractures and a 33% reduction in hip fractures in women assigned to E+P. Hip bone density increased 3.7% after 3 years of taking E+P compared to 0.14% in the placebo group. E+P reduced the risk of fracture to a similar degree in women who were considered to be at high or low risk of fracture. In conclusion, treatment with E+P should not be recommended for the prevention and treatment of osteoporosis in women who dont have menopausal symptoms. Other medicines for osteoporosis should be considered. If E+P is prescribed to prevent osteoporosis, women need to be informed of the risks of taking E+P. 4) Estrogen plus Progestin Effects on Colorectal Cancer and its Diagnosis Because of E+P use, there were 6 fewer cases of colorectal cancer for every 10,000 women over one year. Overall, there was a 44% decrease in the risk for colorectal cancer due to E+P.
Colorectal cancer diagnosed in the E+P women were more advanced (regional/metastatic) in 76 percent of cases versus 49 percent on placebo 5) Estrogen plus Progestin and Risk of Coronary Heart Disease In final analyses, E+P use was associated with: A 24% overall increase in the risk of CHD (6 more heart attacks annually per 10,000 women using E+P) An 81% increased risk of CHD in the first year after starting E+P In conclusion, E+P does not protect the heart and may increase the risk of CHD among generally healthy postmenopausal women, especially during the first year after beginning hormones. E+P should not be started or continued to prevent heart disease 6) The Effects of Estrogen plus Progestin on Gynecologic Cancers and Associated Diagnostic Procedures A 19% decrease in endometrial cancer rates A 58% increase in ovarian cancer rates
Gynecologic cancers are rare diseases, so these estimates are not precise. Nevertheless, these results support current recommendations to use the lowest dose of E+P for the shortest duration needed to treat menopausal symptoms 7) Estrogen plus Progestin and Artery Diseases From the WHI data, E+P did not prevent blockage of the aorta (the large artery carrying blood from the heart to the rest of the body), the carotid arteries, or the arteries supplying the legs. This lack of effect of E+P was similar among women of different ages and among women with and without health problems like high blood pressure, diabetes, smoking, prior heart disease or PAD. Women in this trial were randomly assigned to either placebo or estrogen plus progestin (conjugated equine estrogens 0.625 mg and medroxyprogesterone acetate (2.5 mg), also known as Prempro). When the WHI study first began, this was the most commonly prescribed menopausal hormone therapy in the United States for women with the uterus. Because of the overall findings of health risks exceeding benefits, use of these hormones is now generally recommended only for short-term relief of menopausal symptoms. 8) Effects of Estrogen plus Progestin on Stroke in the Womens Health Initiative For every 10,000 women followed for 1 year, we would expect to see 31 strokes in women on E+P compared to 24 in women on placebo. The excess risk of stroke due to E+P was 7 strokes for every 10,000 women over one year. There is a 31% increase in the risk for stroke due to E+P. The increased risk of stroke due to E+P was seen in all groups of women studied, including those closest to the menopausal change and those with symptoms like hot flashes. The authors conclude that combined E+P should not be used to prevent cardiovascular diseases. The authors confirmed several risk factors for stroke that women can control: high blood pressure, smoking, and diabetes. They also suggest that exercise and taking vitamin C supplements reduce risk for stroke. Although the health benefits of exercise have been generally accepted, the benefits of vitamin C in reducing stroke risk will need to be confirmed by other randomized clinical trials.
9) Hormone Therapy and Risk of Venous Thrombosis in the Womens Health Initiative Trial of Estrogen Plus Progestin Hormone treatment added to the known risks associated with age, being overweight/obese, and having factor V Leiden*. Based on these findings, careful consideration of the use of E + P in women with these added risk factors is advised. While thinner and younger women (ages 50-59) were at lower risk of VT while using E + P, their risk was still two-fold higher with E + P compared to placebo. In another finding from this paper, regular use of aspirin did not protect women from developing E + P-related venous blood clots. Compared with the placebo, estrogen plus progestin resulted in: Increased risk of heart attack Increased risk of stroke Increased risk of blood clots Increased risk of breast cancer Reduced risk of colorectal cancer Fewer fractures No protection against mild cognitive impairment and increased risk of dementia (study included only women 65 and older)
Overall health risks exceeded benefits from use of combined estrogen plus progestin for an average 5.2-year follow-up among healthy postmenopausal US women. All-cause mortality was not affected during the trial. The risk-benefit profile found in this trial is not consistent with the requirements for a viable intervention for primary prevention of chronic diseases, and the results indicate that this regimen should not be initiated or continued for primary prevention of CHD.
Compared with the placebo, estrogen alone resulted in: No difference in risk for heart attack Increased risk of stroke Increased risk of blood clots Uncertain effect for breast cancer No difference in risk for colorectal cancer Reduced risk of fracture (Findings about memory and cognitive function are not yet available.) Statement on Oral Contraceptive Study from Barbara Alving, M.D., Director of the Womens Health Initiative and Acting Director of the National Heart, Lung, and Blood Institute Research conducted in the past to answer specific questions about OCs and breast cancer has shown an increased risk of breast cancer in women who have recently used OCs. Past research has also shown a decreased risk of ovarian cancer and a slight decreased risk of endometrial (uterine) cancer in women who use some types of Ocs 1. What are the benefits of menopausal hormone therapy? Research from the WHI Estrogen-plus-Progestin study has shown that women taking combined hormone therapy had the following benefits:
One-third fewer hip and vertebral fractures than women taking the placebo. In absolute terms, this meant 10 fractures per 10,000 women per year who took hormone therapy compared with 15 fractures per 10,000 women per year who took the placebo. One-third lower risk of colorectal cancer than women taking the placebo. In absolute terms, this meant 10 cases of colorectal cancer per 10,000 women per year who took hormone therapy compared with 16 cases of colorectal cancer per 10,000 women per year who took the placebo.
However, a follow-up study found that neither benefit persisted after the study participants stopped taking combined hormone therapy medication. Women taking estrogen alone experienced the following benefits: o One-third lower risk for hip and vertebral fractures than women taking the placebo. In absolute terms, this meant 11 hip and 11 vertebral fractures per 10,000 women per year who took estrogen compared with 17 hip and 17 vertebral fractures per 10,000 women per year who took the placebo. A 23 percent reduced risk of breast cancer than women taking the placebo. In absolute terms, this meant 26 cases of invasive breast cancer per 10,000 women per year who took estrogen compared with 33 cases of invasive breast cancer per 10,000 women per year who took the placebo.
After 10.7 years of follow-up, however, the risk of hip fractures was slightly higher in the estrogen-alone group, but the risk of breast cancer remained lower than that among women who took the placebo. 2. What are the health risks of MHT? Before the WHI studies began, it was known that MHT with estrogen alone increased the risk of endometrial cancer in women with an intact uterus. It was for this reason that, in the WHI trials, women randomly assigned to receive hormone therapy took estrogen plus progestin if they had a uterus and estrogen alone if they didnt have one. Research from the WHI studies has shown that MHT is associated with the following harms: o o o Urinary incontinence. Use of estrogen plus progestin increased the risk of urinary incontinence. Dementia. Use of estrogen plus progestin doubled the risk of developing dementia among postmenopausal women age 65 and older. Stroke, blood clots, and heart attack. Women who took either combined hormone therapy or estrogen alone had an increased risk of stroke, blood clots, and heart attack. For women in both groups, however, this risk returned to normal levels after they stopped taking the medication. Breast cancer. Women who took estrogen plus progestin were more likely to be diagnosed with breast cancer . The breast cancers in these women were larger and more likely to have spread to the lymph nodes by the time they were diagnosed. The number of breast cancers in this group of women increased with the length of time that they took the hormones and decreased after they stopped taking the hormones. These studies also showed that both combination and estrogen-alone hormone use made mammography less effective for the early detection of breast cancer. Women taking hormones had more repeat mammograms to check on abnormalities found in a screening mammogram and more breast biopsies to determine whether abnormalities detected in mammograms were cancer.
The rate of death from breast cancer among those taking estrogen plus progestin was 2.6 per 10,000 women per year, compared with 1.3 per 10,000 women per year among those taking the placebo. The rate of death from any cause after a diagnosis of breast cancer was 5.3 per 10,000 women per year among women taking combined hormone therapy, compared with 3.4 per 10,000 women per year among those taking the placebo. Lung cancer. Women who took combined hormone therapy had the same risk of lung cancer as women who took the placebo. However, among those who were diagnosed with lung cancer, women who took estrogen plus progestin were more likely to die of the disease than those who took the placebo. There were no differences in the number of cases or the number of deaths from lung cancer among women who took estrogen alone compared with those among women who took the placebo . Colorectal cancer. In the initial study report, women taking combined hormone therapy had a lower risk of colorectal cancer than women who took the placebo. However, the colorectal tumors that arose in the combined hormone therapy group were more advanced at detection than those in the placebo group. There was no difference in either the risk of colorectal cancer or the stage of disease at diagnosis between women who took estrogen alone and those who took the placebo. However, a subsequent analysis of the WHI trials found no strong evidence that either estrogen alone or estrogen plus progestin had any effect on the risk of colorectal cancer, tumor stage at diagnosis, or death from colorectal cancer
Вам также может понравиться
- IndianJEndocrMetab17745-8531231 234152Документ5 страницIndianJEndocrMetab17745-8531231 234152Sri HariОценок пока нет
- Menopausia Cancer de MamaДокумент9 страницMenopausia Cancer de MamaGabriela Zavaleta CamachoОценок пока нет
- Rethinking Postmenopausal Hormone TherapyДокумент2 страницыRethinking Postmenopausal Hormone TherapyDanielle Moon100% (1)
- JURDING Hormon TherapyДокумент24 страницыJURDING Hormon TherapyAgustinus Darmawan HОценок пока нет
- Sismondi - HRT and Cancer 1999Документ9 страницSismondi - HRT and Cancer 1999yunxiangsgh4321Оценок пока нет
- Int. J. Epidemiol. 2001 Barrett Connor 423 6Документ4 страницыInt. J. Epidemiol. 2001 Barrett Connor 423 6SISОценок пока нет
- Oxford Journals Medicine & Health International Journal of Epidemiology Volume 30, Issue 3Документ9 страницOxford Journals Medicine & Health International Journal of Epidemiology Volume 30, Issue 3nindyaayuuОценок пока нет
- Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal WomenДокумент13 страницRisks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal WomenEric Xuan LiuОценок пока нет
- Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal WomenДокумент13 страницRisks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal WomenJosé Luis OjedaОценок пока нет
- Oral Contraceptive Cancer RisksДокумент3 страницыOral Contraceptive Cancer RisksJamie Paola SevillaОценок пока нет
- Menopause Dan Myoma UteriДокумент7 страницMenopause Dan Myoma UteriFellixeby ElninothetorresОценок пока нет
- Breast Cancer Research PaperДокумент13 страницBreast Cancer Research PapershaunОценок пока нет
- JAMA 1998 Hulley 605 13Документ9 страницJAMA 1998 Hulley 605 13ajflca20034Оценок пока нет
- Oral Contraceptives and Cancer Risk: Questions and Answers: Key PointsДокумент21 страницаOral Contraceptives and Cancer Risk: Questions and Answers: Key PointsTyan Caery QueОценок пока нет
- Hormone Replacement Therapy and Quality of LifeДокумент2 страницыHormone Replacement Therapy and Quality of Liferizqi_cepiОценок пока нет
- Oral ContrasepsiДокумент16 страницOral Contrasepsidokter wawanОценок пока нет
- Progyluton-26 1DДокумент16 страницProgyluton-26 1DUsma aliОценок пока нет
- 1 s2.0 S0378512213002545 MainДокумент8 страниц1 s2.0 S0378512213002545 Mainrys239Оценок пока нет
- Breast Cancer and ObesityДокумент24 страницыBreast Cancer and ObesityHenry Ogbonna100% (1)
- Final PortfolioДокумент10 страницFinal Portfolioapi-272608990Оценок пока нет
- Serum Levels of Sex Steroids in Benign and Malignant Disorders of Breast in Libyan Women Full ModelДокумент1 страницаSerum Levels of Sex Steroids in Benign and Malignant Disorders of Breast in Libyan Women Full ModelJagannadha Rao PeelaОценок пока нет
- Gyne - Obs-Relation Between OCPs and CancerДокумент16 страницGyne - Obs-Relation Between OCPs and CancerOstazОценок пока нет
- Use of SERMs in MenopauseДокумент3 страницыUse of SERMs in MenopausePoonguzhali PratОценок пока нет
- What's New in The Other Journals?: Screening For Ovarian Cancer Bilateral Salpingo-Oophorectomy at Hysterectomy or Not?Документ2 страницыWhat's New in The Other Journals?: Screening For Ovarian Cancer Bilateral Salpingo-Oophorectomy at Hysterectomy or Not?Gladstone AsadОценок пока нет
- Am. J. Epidemiol. 2009 Prentice 12 23Документ12 страницAm. J. Epidemiol. 2009 Prentice 12 23Nanda Rizky FathiyaОценок пока нет
- Evidence From Randomised Trials On The Long-Term Effects of Hormone Replacement TherapyДокумент3 страницыEvidence From Randomised Trials On The Long-Term Effects of Hormone Replacement TherapyAnurudh SinghОценок пока нет
- Menopausal Hormone Therapy and The Risk of Breast Cancer - UpToDateДокумент20 страницMenopausal Hormone Therapy and The Risk of Breast Cancer - UpToDateAnonymous EMqrRpnoОценок пока нет
- Atkins Writ159a Assignment3Документ5 страницAtkins Writ159a Assignment3api-553023922Оценок пока нет
- Kapoor 2018Документ8 страницKapoor 2018angela_karenina_1Оценок пока нет
- Breast CAДокумент8 страницBreast CAjchowkingОценок пока нет
- Menopausal Hormone Therapy and Cardiovascular RiskДокумент32 страницыMenopausal Hormone Therapy and Cardiovascular RiskAnonymous EMqrRpnoОценок пока нет
- 168 Essentials of Gerontological Nursing: CancerДокумент3 страницы168 Essentials of Gerontological Nursing: CancerNeoGellinОценок пока нет
- Hulley 1998Документ9 страницHulley 1998junta.propietarios.1456Оценок пока нет
- Aquifer Case - Summary - FamilyMedicine17 - 55-YДокумент9 страницAquifer Case - Summary - FamilyMedicine17 - 55-YHyunsoo EllisОценок пока нет
- Conditions/menopause/in Depth/hormone Therapy/art 20046372?pg 2Документ5 страницConditions/menopause/in Depth/hormone Therapy/art 20046372?pg 2nindyaayuuОценок пока нет
- Uterine Fibroids Natural Treatment by CurcuminДокумент6 страницUterine Fibroids Natural Treatment by CurcuminRay CrashОценок пока нет
- MR 15 27184Документ4 страницыMR 15 27184Arif RSОценок пока нет
- Lifestyle-Related Breast Cancer Risk Factors: Drinking AlcoholДокумент15 страницLifestyle-Related Breast Cancer Risk Factors: Drinking AlcoholGhina AdilaОценок пока нет
- P ('t':'3', 'I':'3054211587') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Документ5 страницP ('t':'3', 'I':'3054211587') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ni Wayan Ana PsОценок пока нет
- Selección de Resúmenes de Menopausia Semana Del 10 Al 21 de Septiembre de 2014Документ5 страницSelección de Resúmenes de Menopausia Semana Del 10 Al 21 de Septiembre de 2014rocksurОценок пока нет
- Lower Risk of Hip Fracture with Higher Fruit and Vegetable IntakeДокумент4 страницыLower Risk of Hip Fracture with Higher Fruit and Vegetable IntakerocksurОценок пока нет
- Ni Hms 574605Документ17 страницNi Hms 574605circe5690Оценок пока нет
- Could Estrogen Protect YoungerДокумент3 страницыCould Estrogen Protect YoungerAmy NilifdaОценок пока нет
- Tibolone and The Promise of Ideal Hormone-Replacement TherapyДокумент3 страницыTibolone and The Promise of Ideal Hormone-Replacement TherapyLeydi Laura QuirozОценок пока нет
- Estradiol 1mg + Norethisterone Acetate 0.5mg (Activelle)Документ12 страницEstradiol 1mg + Norethisterone Acetate 0.5mg (Activelle)asdwasdОценок пока нет
- CEU Nursing pharmacology antineoplastic drugsДокумент3 страницыCEU Nursing pharmacology antineoplastic drugsAlmarie PasaoaОценок пока нет
- Hiperplasia DX y ManejoДокумент10 страницHiperplasia DX y ManejoFinka InaraeОценок пока нет
- Symptoms of Ovarian CancerДокумент3 страницыSymptoms of Ovarian Cancerwwe_jhoОценок пока нет
- Menopause and The Cardiovascular System: Pamela Ouyang, M.DДокумент3 страницыMenopause and The Cardiovascular System: Pamela Ouyang, M.DYofa SukmawatiОценок пока нет
- Med Term JounralДокумент6 страницMed Term JounralKaroline FarleyОценок пока нет
- Hormone Replacement Therapy (HRT) Evidence-Based Guidelines: DR Mahdy El-Mazzahy Damietta General HospitalДокумент38 страницHormone Replacement Therapy (HRT) Evidence-Based Guidelines: DR Mahdy El-Mazzahy Damietta General Hospitalhossam626Оценок пока нет
- Endometrial Hyperplasia - Gyn ReviewДокумент18 страницEndometrial Hyperplasia - Gyn ReviewFedrik Monte Kristo LimbongОценок пока нет
- Selección de Resúmenes de Menopausia Semana Del 6 Al 12 de Agosto de 2014Документ5 страницSelección de Resúmenes de Menopausia Semana Del 6 Al 12 de Agosto de 2014rocksurОценок пока нет
- Journal 6Документ7 страницJournal 6Muflih AlghifaryОценок пока нет
- Medication and Lifestyle May Lower Breast Cancer Risk: by Jane E. BrodyДокумент3 страницыMedication and Lifestyle May Lower Breast Cancer Risk: by Jane E. BrodySabirОценок пока нет
- Estradiol Valerate 2mg + Nongestrel 0.5mg (PROGYLUTON)Документ12 страницEstradiol Valerate 2mg + Nongestrel 0.5mg (PROGYLUTON)ddandan_2Оценок пока нет
- OC Use & Cardiovascular RiskДокумент3 страницыOC Use & Cardiovascular RiskzaplarОценок пока нет
- BACKGROUNDДокумент8 страницBACKGROUNDAhmad Althof Malihul AdiОценок пока нет
- Clinical Internal Medicine Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2От EverandClinical Internal Medicine Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Оценок пока нет
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyОт EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyОценок пока нет
- Introduction to Prosthodontics and Complete DenturesДокумент86 страницIntroduction to Prosthodontics and Complete DenturesKamal NidaОценок пока нет
- Vital Signs GuideДокумент4 страницыVital Signs GuideellithОценок пока нет
- Jurnal Case Report Carcinoma Maxillaris PDFДокумент3 страницыJurnal Case Report Carcinoma Maxillaris PDFEnvhy WinaОценок пока нет
- Mhos PedsfДокумент29 страницMhos PedsfshashiОценок пока нет
- Assam Tea Gardens Cachar, Burtoll T.E. Commissionerate of Labour, Government of Assam Plantation Association name: TAIBVBДокумент4 страницыAssam Tea Gardens Cachar, Burtoll T.E. Commissionerate of Labour, Government of Assam Plantation Association name: TAIBVBAvijitSinharoyОценок пока нет
- Spotlight On Cardiac DrugsДокумент2 страницыSpotlight On Cardiac Drugspauerish100% (2)
- Nursing Ethics: Raymund Christopher R. Dela Peña, RN, RMДокумент23 страницыNursing Ethics: Raymund Christopher R. Dela Peña, RN, RMrnrmmanphd100% (1)
- Family Nursing Care Plan Proper Cigarette Smoking As Health ThreatДокумент2 страницыFamily Nursing Care Plan Proper Cigarette Smoking As Health ThreatWishley Ann PiñedaОценок пока нет
- The Elements of Success:: 21 Customer Stories On Achieving Autonomous TransformationДокумент34 страницыThe Elements of Success:: 21 Customer Stories On Achieving Autonomous TransformationValenОценок пока нет
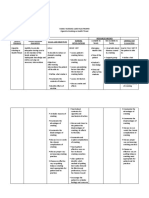
- Nursing Care Plan Impaired AdjustmentДокумент1 страницаNursing Care Plan Impaired Adjustmentderic100% (2)
- Tugas Bahasa Inggris Nama: Sastia Saromeng NIM: Kelas: A/Ners LanjutanДокумент3 страницыTugas Bahasa Inggris Nama: Sastia Saromeng NIM: Kelas: A/Ners LanjutanRiri LangoyОценок пока нет
- Case Studies - NeurologyДокумент12 страницCase Studies - NeurologyNick MorettinОценок пока нет
- Pediatric Dosage Calculation TutorialДокумент34 страницыPediatric Dosage Calculation TutorialnickyboreОценок пока нет
- Tsr-Backpain Ebook FinalДокумент24 страницыTsr-Backpain Ebook FinalRodrigo LimaОценок пока нет
- Typhoid fever: A bacterial infection spread through contaminated food or waterДокумент6 страницTyphoid fever: A bacterial infection spread through contaminated food or waterJohn Ervin AgenaОценок пока нет
- The Role of Orlistat in Treatment of ObesityДокумент12 страницThe Role of Orlistat in Treatment of ObesityNoor786110Оценок пока нет
- Case Scenario 2Документ1 страницаCase Scenario 2Sophia LaurieОценок пока нет
- Neuromuscular QuestionsДокумент9 страницNeuromuscular QuestionsLily JenОценок пока нет
- International Journal of Psychophysiology: Helen Beuzeron-Mangina, Constantine A. ManginaДокумент6 страницInternational Journal of Psychophysiology: Helen Beuzeron-Mangina, Constantine A. ManginaIcaroОценок пока нет
- Nclex Hema and CardioДокумент9 страницNclex Hema and CardioDefensor Pison GringgoОценок пока нет
- DM Type 2 With GangreneДокумент28 страницDM Type 2 With GangreneAgustania PrihantoОценок пока нет
- Yin Yang MedicineДокумент78 страницYin Yang Medicineashutosh2501100% (2)
- CASE 7 Somatic Symptom DisorderДокумент11 страницCASE 7 Somatic Symptom DisorderApril AstilloОценок пока нет
- Wellington ICU Drug Manual 2013Документ444 страницыWellington ICU Drug Manual 2013khangsiean89Оценок пока нет
- Payment Agreement PDFДокумент1 страницаPayment Agreement PDFLisa HalajkoОценок пока нет
- Toxic alcohols review highlights methanol, ethylene glycol dangersДокумент8 страницToxic alcohols review highlights methanol, ethylene glycol dangersSyukron FadillahОценок пока нет
- Chapter 66 - ShockДокумент9 страницChapter 66 - ShockCrysta Venice Tapoc100% (1)
- KMBH CardiacДокумент9 страницKMBH CardiacPutra SimaОценок пока нет
- Cranial Nerve Exam TechniquesДокумент19 страницCranial Nerve Exam Techniquesifer_018Оценок пока нет
- Opini-Can Hemoglobin-Hematocrit Relationship Be Used To Assess Hydration StatusДокумент4 страницыOpini-Can Hemoglobin-Hematocrit Relationship Be Used To Assess Hydration StatusBoby ShéОценок пока нет