Академический Документы
Профессиональный Документы
Культура Документы
83 29
Загружено:
hellsin666Исходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
83 29
Загружено:
hellsin666Авторское право:
Доступные форматы
Journal of Chinese Medicine Number 83 February 2007
Abdominal Acupuncture: A Practical Introduction
29
Abdominal Acupuncture: A Practical Introduction
Abstract
Abdominal acupuncture is a relatively new Chinese microsystem which is increasingly widely practised in China and the West. It involves the gentle, superficial needling of both standard and new acupoints on the abdomen and is thus indicated for cases of extreme sensitivity to needles and/or general weakness. By: Roger Lore Keywords: Abdominal acupuncture, acupuncture, pain, microsystem.
Background
icrosystems, in which a part of the body reects the whole, are a distinctive feature of traditional Chinese medicine (TCM). Whereas in ancient times the abdomen was used exclusively in diagnosis, the emphasis in modern abdominal acupuncture is on treatment. The system was developed approximately 20 years ago by Dr. Bo Zhiyun1 as part of the movement towards gentle acupuncture techniques which developed with the privatisation of acupuncture in China in the mid1980s. Dr. Bo appears to have been inuenced by Japanese traditions of diagnosis and treatment, which share with abdominal acupuncture a shallow depth of needle insertion and some of the zone correspondences. There are also similarities between abdominal acupuncture and the Chinese Daoist system of bodywork known as Qi Nei Zang.
Indications
Abdominal acupuncture is primarily indicated for pain and neurological disorders. It is particularly useful in the treatment of the sequelae of windstroke2, for which it is now used more often than scalp acupuncture in some clinics in China. It may also be helpful in treating cardiovascular and psychiatric disorders. Because the needling is supercial and there is only mild or no deqi obtained, abdominal acupuncture is indicated for any patients who are weak, or who are particularly sensitive to acupuncture. This includes the very young and the elderly. Point location Abdominal acupuncture is applied at three levels of needle penetration: supercial, middle and deep. Each level has its distinctive functions and therapeutic effects, but in this article I will discuss the supercial level only, since it is the one most commonly used. The supercial, or sky, level is situated subcutaneously between the skin and the fatty tissue. Dr. Bo refers to it as the congenital abdominal
meridian system since he maintains that it is present at the embryonic stage of foetal development and develops along with the embryo. Microsystems use representative imagery whenever possible to facilitate organisation and learning: in the case of Nogiers ear acupuncture, for example, an inverted foetus is depicted. Abdominal acupuncture at the supercial level uses the image of a turtle or tortoise, one of the benevolent animal spirits and a prominent symbol in Chinese literature, whose plastron is traditionally associated with the human abdomen. The tortoise is centred on the navel and its head lies on the epigastrium. It should be noted that abdominal acupuncture is two-dimensional, which means that the central line treats both the Conception and Governing vessels, for example, and the Kidney channel also treats the Bladder. Each area of the tortoises body reects a different part of the human body and corresponds to the following abdominal acupoints: The head is centred at Zhongwan REN-12, with the ears on the Kidney channel on either side of Zhongwan REN-12.
The head is centred at Zhongwan REN-12 with the ears lying on the Kidney channel
The edge of the abdomen corresponds to Tianshu ST-25
The neck and throat lie on a line between Jianli REN-11 and Xiawan REN-10
30
Abdominal Acupuncture: A Practical Introduction
Journal of Chinese Medicine Number 83 February 2007
The elbow is situated 0.5 cun lateral & superior to the shoulder
The shoulder corresponds to Huaroumen ST-24
The wrist is situated 0.5 cun lateral and inferior to the elbow. The hand lies as a fist, just beyond the wrist, with the thumb up. The knee is situated 0.5 cun lateral and inferior to the hip
The neck and throat correspond to a line from Jianli REN-11 to Xiawan REN-10. The edge of the abdomen corresponds to Tianshu ST-25. The shoulder corresponds to Huaroumen ST-24. The elbow is situated 0.5 cun lateral and superior to the shoulder. The wrist is situated 0.5 cun lateral and inferior to the elbow. The upper limb forms an inverted V. The hand is represented as a st just beyond the wrist, with the thumb up. The lower border of the rst lumbar vertebra corresponds to Qihai REN-6, and Yaoyangguan DU-3 corresponds to Guanyuan REN-4. The coccyx corresponds to Zhongji REN-3. The hip corresponds to Wailing ST-26. The knee is situated 0.5 cun lateral and inferior to the hip. Note that a secondary knee point lies halfway between the primary one and Qihai REN-6. All three points lie on the same horizontal line The ankle is situated 0.5 cun inferior and lateral to the knee, and the foot is situated just beyond, with the toes 45-degrees inferior and medial to the foot.3 Treatment The rst point to note in treatment is that abdominal acupuncture at the supercial level, as is being discussed here, is usually either combined or alternated with conventional acupuncture. To treat anxiety or headache, for example, an abdominal acupuncture treatment may be combined with Fengchi GB-20 [angled inferiorly towards the feet4], or for leg pain, abdominal acupuncture may be combined with Yinshi ST-33.5 Treatment with abdominal acupuncture generally proceeds as follows: Step one Each treatment begins with a four needle protocol, using either i. Zhongwan REN-12, followed by Xiawan REN-10, Qihai REN-6 and Guanyuan REN-4, or ii. the diamond treatment consisting of Zhongwan REN-12, bilateral Tianshu ST-25, Qihai REN-6 or Guanyuan REN-4. These combinations of points promote the circulation of qi and blood in the abdomen and enhance the effects of any subsequent points needled. Step two Points corresponding to the site of pain or disease are then needled unilaterally on the aficted side. It is common when treating pain syndromes of the limbs to rst needle the shoulder point in order to promote the circulation of qi in the aficted upper limb, or the hip point to promote the circulation of qi in the lower limb. The point corresponding to the site of pain is then needled. For example, for right wrist pain, right Huaroumen ST-24 (i.e. the shoulder point) is needled rst, followed by the right wrist point. The needles are retained for 20-25 minutes and may be stimulated gently by hand every ten minutes as in a conventional treatment, although it is not necessary to obtain deqi. To increase the therapeutic effect a moxa pole or TDP infrared lamp may be placed over the navel for the duration of the session.
The hip corresponds to Wailing ST-26
The ankle is situated 0.5 cun lateral and inferior to the knee. The foot is situated just beyond the ankle, the toes 45 inferior and medial to the foot
Qihai REN-6 corresponds to the first lumbar vertebra
Guanyuan REN-4 corresponds to Yaoyangguan DU-3
The coccyx corresponds to Zhongji REN-3
Journal of Chinese Medicine Number 83 February 2007
Abdominal Acupuncture: A Practical Introduction
31
The four gates of abdominal acupuncture Another protocol which may be used on its own or in combination with the above two step treatment is the bilateral needling of the acupoints Huaroumen ST-24 and Wailing ST-26. These are known as the four gates of abdominal acupuncture and are used to promote the circulation of qi throughout the body in the same way that the four gates of conventional acupuncture, Hegu L.I.-4 and Taichong LIV-3 do. However it should be noted that when treating an aficted limb these same points are always used individually and on the affected side only.
Case histories
The following two case histories typify the use of abdominal acupuncture, the rst one in treating a sensitive patient with pain syndrome, and the second in a case of windstroke sequelae complicated by a psychiatric disorder. Case one A young woman presented in clinic with elbow pain. She was an acupuncturist herself, although she was extremely sensitive to needles and unable to bear conventional acupuncture treatment. She had been suffering from chronic elbow pain for eight months and had taken Chinese herbal medicine in patent form for several months with only minimal results. She described herself as hardworking and generally healthy, although her soft pulse, toothmarked tongue, tenderness on both the frontmu and back-shu points of the Spleen and noticeable worry about her pain clearly indicated Spleen deciency. Abdominal acupuncture was recommended to her for the gentleness of its technique and also its ability to address her Spleen qi deciency through its association with the navel, the centre of the abdominal acupuncture system. For the rst treatment she was given the routine four point protocol of Zhongwan REN-12, Xiawan REN-10, Qihai REN-6 and Guanyuan REN-4. Zhongwan REN-12 was needled at a depth of 0.5 cun, which increased progressively to a depth of 0.75 cun at Guanyuan REN-4. On insertion of the needles there was a visible pulsation associated with increased blood ow to the area, even though no deqi was experienced. Huaroumen ST-24 (the shoulder point) was then needled on the right side to promote the circulation of qi to the affected limb, followed by the elbow point (which is aptly also called Shang Feng Shi Dian, or upper wind-damp point). Both of these points were needled to a depth of 0.2-0.3 cun. As soon as the elbow point was inserted, the patient experienced a sensation of qi throughout her whole body which lasted for a few seconds, a phenomenon that the author has noted with other patients receiving abdominal acupuncture. Abdominal acupuncture was combined with conventional acupuncture at Zusanli ST-36, Sanyinjiao SP-6 and Quchi L.I.-11 at each treatment. After three treatments her pain was resolved.
Case two A 65 year old male patient was brought to the teaching clinic of OCOM (the Oregon College of Oriental Medicine), having suffered two successive strokes, 22 months earlier. The rst resulted in impairment of speech and paranoia, and the second in grand mal seizures and paralysis of both right limbs. His other symptoms included leg spasticity, outward hip rotation, drop foot and restricted shoulder movement, and although he was quick to smile and shake hands in greeting, his difculty in communicating and understanding indicated cognitive impairment. He was being given a complex mix of Western medications which included heart medication, psychoactive drugs for depression, mania and seizures, and botox injections every three months to relieve muscle spasms. His pulse was slippery, forceful and a little rapid, his tongue body was cracked and red/slightly purple (especially at the tip) and the coat was yellow and dry. He was diagnosed with wei (accidity) syndrome, deciency of yin, stagnation of qi and blood, internal wind and phlegm-heat obstructing the Heart. Initially he received scalp acupuncture from a visiting specialist in this system. The effects were immediate and so positive that the specialist recommended continuing with a two-month course of treatment, followed by one month of rest in order to avoid the sensitising effects that prolonged scalp treatment can have. Because his progress was so encouraging after two months, however, the instructions of the specialist were ignored and the patient ultimately received ve months of scalp acupuncture. At this point he started to become agitated and violent during and after treatments and the scalp acupuncture had to be stopped. Abdominal acupuncture was then proposed as an alternative. The patient was given the routine diamond treatment to promote the circulation of qi and blood, which consists of Zhongwan REN-12, Tianshu ST-25, Qihai REN-6 or Guanyuan REN-4. This was followed by Wailing ST-26 and Huaroumen ST-24 on the right side to activate qi and blood in the right hip and shoulder, respectively. He was then given conventional acupuncture to treat wei syndrome, using points such as Zusanli ST-36, Jiexi ST-41, Xuanzhong GB-39, Huantiao GB-30, Jianyu L.I.-15, Quchi L.I.-11, Hegu L.I.-4 and Waiguan SJ-5. Finally the ear points Aggression (Neurasthenia), Diaphragm, Shenmen and Sympathetic were chosen according to the authors experience of their successful use in calming violent patients. The patient was comfortable with the abdominal acupuncture and his condition continued to improve in all respects. After several more months of treatment his medical report concluded that he was at a new level of cognitive skills, with increased communication and understanding.
32
Abdominal Acupuncture: A Practical Introduction
Journal of Chinese Medicine Number 83 February 2007
Conclusion
Abdominal acupuncture has been described as the most powerful microsystem in acupuncture, more so than for the scalp or ear.6 It has also been noted, however, that the relatively quick effects it obtains are not necessarily sustained7 and this may be one reason that abdominal acupuncture is usually combined with conventional acupuncture. Results in China and elsewhere (such as Southern Europe) have been encouraging enough to warrant investigation in the English-speaking world. Abdominal acupuncture at all three levels takes longer to learn than many other microsystems of acupuncture (one source recommends three years to attain basic familiarity8). Despite this, practitioners may safely combine the treatment routines at the supercial level described in this article with conventional protocols, and then observe the results.
Dr. Roger Lore chairs the department of Acupuncture, Qigong & Bodywork at the Oregon College of Oriental Medicine. He teaches, practises and researches acupuncture and qigong at OCOM, and is currently enrolled in the Research Scholar Program funded by the National Institute of Health. Roger is also engaged in acupuncture research and practice at Oregon Health & Science University.
References
1 Bo Z, Fu Zhen Liao Fa, Beijing: S c i e n c e & Te c h n o l o g y Publishing Press, 1999. Chinese language edition. ISBN 7-5046-2771-2. A c u p u n c t u r e To d a y, An Interview with Zhiyun Bo, Inventor of Abdominal A c u p u n c t u re ( F u Z h e n ) . DAlberto A, Kim E. August 2005. Vol. 6, Issue 8. http:// w w w. a c u p u n c t u re t o d a y. com/archives2005/aug/ 08dalbertokim.html - last accessed 5 Nov 05. Poster chart, Abdominal Hologram. Beijing Science & Technology Press. ISBN 75304-2952-3. Website: www. bkjpress.com [in Chinese], last accessed 8 Jan 2006. Bensky D et al [translator]. Acupuncture: A Comprehensive Text, Shanghai College of Traditional Medicine, Seattle: Eastland Press, 1984, p.492. Dr. Han Yan. From a lecture on Abdominal Acupuncture at Nanjing University of TCM to clinical doctoral students
from the Oregon College of Oriental Medicine in May, 2004. Dr. Han is a specialist in this type of acupuncture, and practises at the Jiangsu Provincial Hospital. 6 Dr. Li Yutang of Nanjing University of TCM, during a lecture at Oregon College of Oriental Medicine (OCOM) doctoral program in Portland, Oregon, 19 Sep 2003. Dr. Ou Jianwen of Nanjing Municipal TCM Hospital. Clinical internship: 7-28 May 2005. Dr.Han, ibid.
Вам также может понравиться
- Managing Pain: And Other Medically Proven Uses of AcupunctureОт EverandManaging Pain: And Other Medically Proven Uses of AcupunctureОценок пока нет
- The Acupuncture Prescription:: A Holistic Approach to HealthОт EverandThe Acupuncture Prescription:: A Holistic Approach to HealthОценок пока нет
- A Study of The Sa-Ahm Five Element Acupuncture Theory: December 2009Документ13 страницA Study of The Sa-Ahm Five Element Acupuncture Theory: December 2009dtncorreoОценок пока нет
- Why Pulse DiagnosisДокумент7 страницWhy Pulse DiagnosisRanganathan100% (1)
- Bleeding Peripheral Points. An Acupuncture TechniqueДокумент6 страницBleeding Peripheral Points. An Acupuncture TechniqueSanjay PatilОценок пока нет
- Acupoint Stimulation For AcneДокумент22 страницыAcupoint Stimulation For AcneCristian SauraОценок пока нет
- Adv Acu Tech 1 - Class 2 - Jiao's Scalp AcupunctureДокумент4 страницыAdv Acu Tech 1 - Class 2 - Jiao's Scalp Acupunctureg23164100% (1)
- Balance Method RevBalance Method Revolutionizes Acupunctureolutionizes AcupunctureДокумент3 страницыBalance Method RevBalance Method Revolutionizes Acupunctureolutionizes Acupuncturedrtommy75Оценок пока нет
- Acupuncture Pulse Diagnosis and the Constitutional Conditional ParadigmОт EverandAcupuncture Pulse Diagnosis and the Constitutional Conditional ParadigmОценок пока нет
- Acupuncture As A FasciaДокумент5 страницAcupuncture As A Fasciacelliastt100% (1)
- World's Largest Science, Technology & Medicine Open Access Book PublisherДокумент18 страницWorld's Largest Science, Technology & Medicine Open Access Book PublisherAndik SH100% (1)
- Other Acupuncture Reflection 1Документ11 страницOther Acupuncture Reflection 1Indra SyafriОценок пока нет
- Treatment of Female Infertility A New Approach in Chinese MedicineДокумент23 страницыTreatment of Female Infertility A New Approach in Chinese Medicinean ssiОценок пока нет
- Microsystem NoteДокумент18 страницMicrosystem Noteyayanica100% (1)
- Toni (Zhu Scalp Acup)Документ4 страницыToni (Zhu Scalp Acup)AngelaОценок пока нет
- JCM Ashi Points ArticleДокумент8 страницJCM Ashi Points ArticleCarleta StanОценок пока нет
- How The Strategy of The 12 Magic Points Makes A Tiger With A Pair of Wings 1294072199Документ3 страницыHow The Strategy of The 12 Magic Points Makes A Tiger With A Pair of Wings 1294072199kahuna_ronbo3313Оценок пока нет
- Japanese AcupunctureДокумент2 страницыJapanese AcupunctureRachel GreeneОценок пока нет
- Web - The Eight Principles of Diagnosis in Traditional Chinese MedicineДокумент8 страницWeb - The Eight Principles of Diagnosis in Traditional Chinese MedicineJing CruzОценок пока нет
- Introduction To Neijing Classical Acupuncture Part II: Clinical TheoryДокумент14 страницIntroduction To Neijing Classical Acupuncture Part II: Clinical TheoryElanghovan ArumugamОценок пока нет
- AJACM 2011 6 1 Wang Juyi Interview Part 2 of 2 - LiuДокумент4 страницыAJACM 2011 6 1 Wang Juyi Interview Part 2 of 2 - LiuYagtaliОценок пока нет
- Tran MentalactivityДокумент33 страницыTran MentalactivityKiran JoshiОценок пока нет
- Pulse Diagnosis: © 2004 William R. Morris, Omd, Msed, LacДокумент5 страницPulse Diagnosis: © 2004 William R. Morris, Omd, Msed, LacAndik SH100% (1)
- Lesson03thinkific 1511875031903Документ10 страницLesson03thinkific 1511875031903Rocío JMОценок пока нет
- The Spark in The MachineДокумент53 страницыThe Spark in The MachineElanghovan Arumugam100% (1)
- Immortalizing Emotions: A Chinese Medicine perspective of TattoosОт EverandImmortalizing Emotions: A Chinese Medicine perspective of TattoosОценок пока нет
- 1996 Root and Branch Clinical ApplicationsДокумент9 страниц1996 Root and Branch Clinical Applicationsdoktormin106Оценок пока нет
- Acupuncture Imaging 31 40 PDFДокумент10 страницAcupuncture Imaging 31 40 PDFmamun31Оценок пока нет
- Qualities of A Great AcupuncturistДокумент6 страницQualities of A Great AcupuncturistKim HaslamОценок пока нет
- Acupuncture For Disorders of ConsciousneswsДокумент27 страницAcupuncture For Disorders of ConsciousneswsGabriel Navarro100% (1)
- UseofDr tansChineseBalanceAcupuncture Medicalacupuncture04 16Документ10 страницUseofDr tansChineseBalanceAcupuncture Medicalacupuncture04 16Marlon ManaliliОценок пока нет
- 05 Brechtje SebregtsДокумент6 страниц05 Brechtje Sebregtstigerstyle1Оценок пока нет
- Treating Pain With Master Tung PointsДокумент4 страницыTreating Pain With Master Tung PointsJose Gregorio Parra100% (2)
- Acup 123 For Back Pain BlurbДокумент5 страницAcup 123 For Back Pain Blurbhihi12100% (1)
- Pain Control With Acupuncture - Class 2Документ46 страницPain Control With Acupuncture - Class 2Hector Rojas100% (1)
- A Skeptical Look at The AcuGraphДокумент4 страницыA Skeptical Look at The AcuGraphhjsassoОценок пока нет
- Carpal Tunnel Syndrome - Kiiko Matsumoto Japanese StyleДокумент3 страницыCarpal Tunnel Syndrome - Kiiko Matsumoto Japanese StyleAWEDIOHEADОценок пока нет
- Lecture-4 (Meridian and Acupuncture)Документ78 страницLecture-4 (Meridian and Acupuncture)DS EОценок пока нет
- Mastering Tung AcupunctureДокумент16 страницMastering Tung AcupunctureMustafa Ali0% (1)
- Qigong AcupunctureДокумент244 страницыQigong Acupuncturewerottydesluiz100% (1)
- Bleeding Peripheral PointsДокумент28 страницBleeding Peripheral PointsChetna Kanchan BhagatОценок пока нет
- Adv Acu Tech 1 - The Second Metacarpal Bone TherapyДокумент24 страницыAdv Acu Tech 1 - The Second Metacarpal Bone Therapysuperser123465100% (2)
- Syllabus Master Tung PDFДокумент25 страницSyllabus Master Tung PDFkamran ahmadОценок пока нет
- Limb MicrosystemsДокумент1 страницаLimb Microsystemsdrprasant100% (1)
- Acupuncture 3-Points For AutismДокумент3 страницыAcupuncture 3-Points For AutismHaryono zhu100% (1)
- MTMP Beg1 TC FinalДокумент28 страницMTMP Beg1 TC FinalAdriana GL100% (1)
- Stop Suffering from Arthritis: Tcm Can Help YouОт EverandStop Suffering from Arthritis: Tcm Can Help YouОценок пока нет
- Scalp Acupuncture ASDДокумент7 страницScalp Acupuncture ASDHaryono zhuОценок пока нет
- Class 9 and 10 - Wrist and Ankle AcupunctureДокумент13 страницClass 9 and 10 - Wrist and Ankle Acupunctureg23164100% (4)
- Jprot Tungbmpain LNДокумент48 страницJprot Tungbmpain LNJoan MoralesОценок пока нет
- Sinew Channels by J Yuen002Документ81 страницаSinew Channels by J Yuen002Jonathan100% (1)
- Persuasive Essay - Final DraftДокумент10 страницPersuasive Essay - Final DraftEmily LongОценок пока нет
- Teacher Guide To Good PrescribingДокумент106 страницTeacher Guide To Good PrescribingJosep Maria Castel100% (1)
- G6PD Deficiency Food To AvoidДокумент9 страницG6PD Deficiency Food To AvoidJason Tiongco100% (7)
- MBRДокумент9 страницMBRAuspicious MuthuОценок пока нет
- Lesson Plan On Electroconvulsive TherapyДокумент13 страницLesson Plan On Electroconvulsive Therapysimranjeet kaurОценок пока нет
- M-FUN Assessment ReviewДокумент4 страницыM-FUN Assessment ReviewKishan RamtohulОценок пока нет
- Head InjuryДокумент22 страницыHead InjuryNguyễn Ly100% (1)
- Nursing Care Plan Mobility SampleДокумент6 страницNursing Care Plan Mobility Samplen2biologyОценок пока нет
- The Process of Pinioning Involves The Cutting of One Wing at The Carpel JointДокумент23 страницыThe Process of Pinioning Involves The Cutting of One Wing at The Carpel JointNanda FinisaОценок пока нет
- Nausea and Vomiting (Algorithm) PDFДокумент2 страницыNausea and Vomiting (Algorithm) PDFAnggie Anggriyana0% (1)
- Veris TOHДокумент35 страницVeris TOHtofssbiОценок пока нет
- 02 IV TherapyДокумент3 страницы02 IV Therapybunso padillaОценок пока нет
- 02-HK Products AllДокумент154 страницы02-HK Products AllHari SetiawanОценок пока нет
- cs2 NCPДокумент1 страницаcs2 NCPapi-251084195Оценок пока нет
- Daftar PustakaДокумент3 страницыDaftar PustakaEKAОценок пока нет
- Everyone Knows That Joining A Gym Is A QuoteДокумент2 страницыEveryone Knows That Joining A Gym Is A Quotejigar shahОценок пока нет
- CNS Stimulants 2010Документ38 страницCNS Stimulants 2010Neal KirkОценок пока нет
- Modul UrologyДокумент49 страницModul UrologysonyОценок пока нет
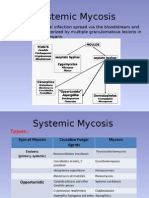
- MycosisДокумент5 страницMycosisMaiWahidGaberОценок пока нет
- Drug Study For Mini Case PRESДокумент11 страницDrug Study For Mini Case PRESKevin AliasasОценок пока нет
- Quality by Design For ANDAs - MR TabletsДокумент161 страницаQuality by Design For ANDAs - MR TabletsShilpa Kotian100% (1)
- Behavior Therapy: Mr. Jayesh PatidarДокумент21 страницаBehavior Therapy: Mr. Jayesh PatidarDr. Jayesh Patidar100% (2)
- Giraud2013 Obesity and MigraineДокумент6 страницGiraud2013 Obesity and MigraineEcaterina PozdircăОценок пока нет
- Types of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisДокумент4 страницыTypes of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDaisy MellaОценок пока нет
- Case No 1:-Bio DataДокумент8 страницCase No 1:-Bio DataSarah Saqib Ahmad100% (1)
- ABSTRACT PROF. DR. Dr. ZAKIUDIN MUNASIR SpAKДокумент1 страницаABSTRACT PROF. DR. Dr. ZAKIUDIN MUNASIR SpAKTimothy Eduard A. SupitОценок пока нет
- Obsessive Compulsive DisorderДокумент2 страницыObsessive Compulsive DisorderMargaretDeniseDelRosarioОценок пока нет
- Contrast MediaДокумент94 страницыContrast MediaJustin JoseОценок пока нет
- MagnetoterapieДокумент10 страницMagnetoterapieHelena PatraОценок пока нет