Академический Документы
Профессиональный Документы
Культура Документы
ANTIBIOTICS GUIDELINEهام جدا
Загружено:
Mohamad Samir0 оценок0% нашли этот документ полезным (0 голосов)
53 просмотров16 страницToo much or inappropriate use of antibiotics is leading to the occurrence of resistance and increased morbidity, mortality, increased use of health care resources. Antimicrobials account for up to one fifth of hospital drug budgets In Scotland. One of the key unintended consequences of such use is C. Difficile Associated Disease (CDAD) There are two core strategies, both proactive, that provide the foundation for an antimicrobial stewardship program.
Исходное описание:
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документToo much or inappropriate use of antibiotics is leading to the occurrence of resistance and increased morbidity, mortality, increased use of health care resources. Antimicrobials account for up to one fifth of hospital drug budgets In Scotland. One of the key unintended consequences of such use is C. Difficile Associated Disease (CDAD) There are two core strategies, both proactive, that provide the foundation for an antimicrobial stewardship program.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
53 просмотров16 страницANTIBIOTICS GUIDELINEهام جدا
Загружено:
Mohamad SamirToo much or inappropriate use of antibiotics is leading to the occurrence of resistance and increased morbidity, mortality, increased use of health care resources. Antimicrobials account for up to one fifth of hospital drug budgets In Scotland. One of the key unintended consequences of such use is C. Difficile Associated Disease (CDAD) There are two core strategies, both proactive, that provide the foundation for an antimicrobial stewardship program.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 16
Scottish Antimicrobial Prescribing Group
Guidance to Optimise Antimicrobial Use
and
Reduce Clostridium difficile Associated Disease
in Scottish Hospitals
Version 1
Produced July 2008
For Review July 2009
Guidance to optimise antibiotic use and reduce C. difficile associated
disease (CDAD) in Scottish hospitals
What is presently happening in Scotland?
Too much or inappropriate use of antibiotics is leading to the occurrence of resistance and
consequently increased morbidity, mortality, increased use of health care resources and
unintended consequences such as C. difficile infections.
In Scotland, antimicrobials account for up to one fifth of hospital drug budgets. Approximately
one third of all inpatient receive antibiotics during a period of hospitalisation and up to
50% of these prescriptions are deemed inappropriate for a variety of reasons, but primarily
due to unnecessary use of broad spectrum agents. One of the key unintended consequences
of such use is C. difficile associated disease (CDAD), of which significant increases have
been reported combined with evidence of more severe infection and greater attendant
complications and mortality.
What will help to reduce this?
The evidence base for the effectiveness of programmes or interventions restricting antibiotic use
and improving the quality of prescribing (antimicrobial stewardship programmes) combined with
key infection prevention measures is extensive.
The primary goal of antimicrobial stewardship is to optimize clinical outcomes while minimizing
unintended consequences of antimicrobial use including toxicity, the selection of pathogenic
organisms (such as C. difficile) and the emergence of resistance.
1
There are two core strategies, both proactive, that provide the foundation for an antimicrobial
stewardship program. These strategies are not mutually exclusive.
Prospective audit with intervention and feedback. This can result in reduced
inappropriate use of antimicrobials (I-A)*
Formulary restriction can lead to immediate and significant reductions in
antimicrobial use and cost ( II-A)
1
* See table for ranking recommendations in clinical guidelines page 7
- 2 -
What is the role of the Scottish Antimicrobial Prescribing Group (SAPG)?
The Scottish Antimicrobial Prescribing Group (SAPG), a national clinical forum, convened
by the Scottish Medicines Consortium (SMC), but supported by The Scottish Government
Health Directorate (SGHD) and Healthcare Associated Infection (HAI) Task Force was
launched in March 2008.
2
The SAPG is planning to undertake important pieces of work related
to antibiotic consumption and prescribing, resistance surveillance, organisational accountability
for antimicrobial stewardship, antimicrobial prescribing education for healthcare professionals
and infection management. One of its immediate concerns is to support the development,
implementation and evaluation of good practice guidance for antimicrobial use for common
infections and surgical prophylaxis. These should incorporate best evidence for patient
management as well as elements to limit the inappropriate use of antibiotics, including those
associated with development of CDAD and meticillin resistant Staphylococcus aureus (MRSA)
infection. Local implementation and evaluation of these measures should be undertaken by
Antimicrobial Management Teams (AMTs) recommended in the 2005, SGHD Health care
associated infection task force commissioned SMC paper Antimicrobial Prescribing Policy and
Practice (APP&P)
3
.
Unfortunately to date many of Scotlands NHS Boards do not have these
AMTs in place.
A Chief Executive Letter (CEL 30 2008 http://www.sehd.scot.nhs.uk/mels/CEL2008_30.pdf)
issued by the SGHD on the 8
th
July has confirmed the establishment of the SAPG. At its first
full meeting in June 2008 SAPG advised the SGHD that not every Board has an established
AMT as set out in APP&P and ScotMARAP
2
, and some of those which have been set up do not
cover primary care prescribing. As an immediate intervention to reduce the risks from C. difficile,
the SGHD has accepted SAPGs recommendation that all Boards should as a priority establish
an AMT which covers primary and secondary care prescribing activities.
SAPG Recommendations:
In response to increasing CDAD rates and invasive infections due to resistant bacteria such as
MRSA, awareness of the associated morbidity and mortality, and in order to ensure prudence in
antibiotic prescribing (including surgical prophylaxis) in Scottish hospitals, SAPG recommends
the following actions to complement current infection control measures;
1. As a minimum requirement each health board should have an AMT responsible at
board level, for the surveillance of antimicrobial usage, audit of local prescribing practice and
development and dissemination of infection management guidance. AMTs should be
- 3 -
supported by the local Area Drugs and Therapeutics Committee (ADTC) and or antibiotic
subcommittee.
The AMT should comprise a lead antimicrobial pharmacist, a lead clinician and a lead
microbiologist. All key members should have dedicated resource in keeping with the size of
the local organisation. The AMT should work closely with infection control teams to
implement changes in prescribing and to monitor changes in Healthcare Associated Infections,
antibiotic consumption and prescribing practice. The potential risks of antibiotic restriction
such as increased complications, readmissions, intensive care unit (ICU) admissions or
mortality from relevant infections and re-emergence of infections due to organisms that have
become uncommon during the antibiotic era should also be monitored. Resource should be
available to collect these data.
2. Regional networking should be established in order to share best practice and harness
best use of resources and expertise.
3. Each AMT should develop, actively implement and audit compliance with an Infection
management guideline for commonly encountered infections in hospitals. Guidance should
incorporate the following elements;
Specific guidance for the management of pneumonia, infective exacerbations of
chronic obstructive pulmonary disease (COPD), urinary tract infection, skin and soft
tissue infection, intra-abdominal infection, bone and joint infection, central nervous
system infection, infection of unknown source and clinical management of CDAD
(see point 5 below). Examples of existing policies within Scotland are available in
appendix 1. Any policy needs to be linked to local infection and antimicrobial
resistance patterns
Clear recommendations on duration of therapy for each antibiotic indication.
Clear recommendations on when to use intravenous (IV) or oral antibiotic therapy,
when to switch from IV to oral therapy and the key components of documenting in
case notes antibiotic treatment review. There is considerable evidence in the literature
covering this area. Although there is as yet no formal care bundle developed for
antimicrobial prescribing core elements for monitoring prescribing have been
identified.
4
- 4 -
Within local guidance there should be clear demonstration of restrictions of
antibiotics associated with CDAD. An example of how this might be done can be
found in appendix 2.
Specific recommendations on good antibiotic stewardship to limit the spread
of C. difficile are
o Stop any (non-Clostridium difficile) antimicrobial treatment in
patients with CDAD as soon as possible (IA)
o As part of good antibiotic stewardship review frequency, duration,
dose and type of antimicrobial used and avoid the use of high-risk
agents in patients at risk. Use these agents only when medically
needed. (IB)
High-risk antimicrobial agents:
3
rd
generation cephalosporins (ceftriaxone, cefotaxime, ceftazidime)
Broad spectrum penicillins (including amoxicillin-clavulanic acid)
Clindamycin
Fluoroquinolones
There is evidence that concurrent implementation of key infection control
measures and antimicrobial stewardship can lead to a reduction in CDAD
incidence
4. Each board is responsible for ensuring compliance with SIGN guidance on surgical antibiotic
prophylaxis
5
. In particular antibiotic prophylaxis should not be continued beyond 24
hours following an operative procedure. AMTs should audit administration of surgical
prophylaxis. Recording of compliance with this recommendation should be
undertaken as part of the routine data collection for mandatory surgical site infection
surveillance.
- 5 -
5. Each board should have in place individual patient management guidelines for when a patient
is diagnosed with CDAD. These should incorporate the following;
Patients with CDAD should have concomitant antibiotic therapy stopped or
simplified.
Patients with CDAD should have concomitant gastric acid suppressive therapy
stopped whenever possible.
Patients with CDAD should undergo severity assessment. Severe infections are
defined as those with one or more of the following criteria;
Temperature > 38.5 C
Patient has major risk factors (hospitalisation in ICU, immuno-supression)
Hypotension (Systolic blood pressures <90 mm/Hg),
White cell count >15/ mm
3
,
Serum albumin <25 mg/l,
Serum creatinine >1.5 xs base line
Suspicion of PMC, toxic megacolon, ileus
Colonic dilatation in CT scan >6 cm on abdominal X ray
Treatment of CDAD should be initiated based on assessment of symptoms and
severity of disease while taking into account individual risk factors of the patient.
Patients with non-severe CDAD should receive oral metronidazole 400mg 8 hourly
for 10 days.
Patients with non-severe CDAD who have not improved after 5 days or patients
with severe CDAD should switch to oral vancomycin 125mg 6 hourly for 10 days.
Patients with severe CDAD with hypotension or ileus should receive IV
metronidazole 400mg 8 hourly in addition to oral vancomycin 250-500mg qds. If
there is evidence of peritonitis secondary to colonic perforation additional anti-
bacterial cover against coliforms would be necessary. In these situations urgent
surgical review with a view to considering colectomy should be sought.
For further information for CDAD treatment refer to Owens RG, Valeti AJ. IDCP 2007;
15(5):299-315.
SCOTTISH ANTIMICROBIAL PRESCRIBING GROUP (SAPG)
July 2008
Review July 2009
- 6 -
Grading system for ranking recommendations in clinical guidelines
1
Category , grade Definition
Strength of recommendation
A Good evidence to support a recommendation for use
B Moderate evidence to support a recommendation for use
C Poor evidence to support a recommendation for use
Quality of evidence
I Evidence from > 1 properly randomised controlled trial
II Evidence from > 1 well designed clinical trial, without
randomisation; from cohort or case-controlled analytic
studies (preferably from >1 centre); from multiple time series;
or from dramatic results from uncontrolled experiments
III Evidence from opinions of respected authorities, based on
clinical experience, descriptive studies, or reports of expert
committees.
- 7 -
References
1. T.H. Dellit et al Infectious diseases society of America and the society for healthcare
epidemiology of America Guidelines for developing an institutional program to enhance
antimicrobial stewardship. CID 2007:44 159-177
2. The Scottish Management of Antimicrobial Resistance Action Plan (ScotMARAP) 2008
http://www.scotland.gov.uk/Publications/2008/03/12153030/0 Accessed 25
th
June
2008
3. Antimicrobial Prescribing Policy and Practice in Scotland: Recommendations for Good
Antimicrobial Practice in Acute Hospitals
http://www.scotland.gov.uk/Publications/2005/09/02132609/26099 Accessed 25
th
June 2008
4. C.Pulcinin et al Design of a day 3 bundle to improve the reassessment of inpatient
empirical antibiotic prescriptions , JAC 2008: 61, 1384-1388
5. Antibiotic prophylaxis in surgery. A national clinical guideline. Scottish Intercollegiate
guidelines network July 2008
http://www.sign.ac.uk/pdf/sign104.pdf
- 8 -
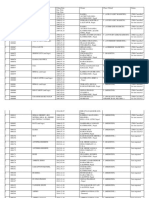
Appendix 1
Infection Management Guideline: Empirical Antibiotic Therapy NHS Greater
Glasgow & Clyde.
(Note this was designed to be printed A3 in size, if printing it A4 in size please
ensure that in the print menu shrink to printable area is selected for the Page
Scaling setting.)
Adult IV to Oral Antibiotic Switch Therapy Guidelines NHS Dumfries & Galloway.
Antibiotic Prescribing Protocol Antibiotic Traffic Light System Dumfries &
Galloway Royal Infirmary and Galloway Community Hospital, NHS Dumfries &
Galloway.
- 9 -
Oral therapy usually recOmmended
IndIcatIOns FOr IV rOute
1. Sepsis or severe sepsis or deteriorating clinical condition
2. Febrile with neutropenia/ immunosuppression
3. Specifc indications: endocarditis, deep abscess,
meningitis, bone/joint infection
4. Skin and soft tissue infection: IV therapy when heat, erythema and induration
+/- sepsis
5. Oral route compromised: nil by mouth, reduced absorption, mechanical swal-
lowing disorder, unconscious, no oral formulation, vomiting
sImplIFy, sWItch, stOp and state duration!
sImplIFy Use narrow spectrum agents whenever possible.
sWItch In the absence of +ve microbiology and specifc situations (see above)
switch to oral therapy when signs of sepsis are resolving and oral route is not
compromised.
stOp Please observe indicated duration of therapy and stop if alternative non-infectious
diagnosis is made.
recOrd IndIcatIOn FOr antIbIOtIc In case nOtes
deFInItIOn OF sepsIs - please recOrd In case nOtes
Clinical symptoms of infection (sweats, chills, rigors etc) plus 2 of the following:
Temp >38 or <36, HR >90bpm, RR >20/min and WCC <4 or >12
severe sepsis: Sepsis + Organ dysfunction/ hypoperfusion (eg. oliguria, confusion, acidosis or hypotension)
NB. Sepsis may be masked in immunosuppression, the elderly and in the presence of anti-infammatory drugs and beta-blockers.
culture blood (8-10mls each bottle) and appropriate area ie. Urine, sputum, CSF, wound or venous access site
Clostridium diffcile infection is associated with prescribing of; Cephalosporins, Co-amoxiclav, Clindamycin and Quinolones (Ciprofoxacin,
Levofoxacin, Moxifoxacin, Ofoxacin). These agents must be restricted to reduce selection pressure. Stop gastric acid suppressive therapy if possible.
lower respiratory tract skin / soft tissue Gastro-intestinal urinary tract cns infection severe systemic
infection? source
eXac of cOpd
Antibiotics if purulent sputum.
Oral therapy usually.
Use 1st line antibiotic unless
recent hospitalisation or recent
antibiotic.
severe / complicated /
infective eXac of cOpd
Use IV therapy as for frst or
second line if indication for IV
route (see above) or ventilation
or sepsis.
Duration 7 days
NB. Doxycycline not available IV.
staphylococcal pneumonia suspected
add IV Flucloxacillin 2g 6hrly
aspiration pneumonia
IV Amoxicillin 1g 8hrly
+ Metronidazole 500mg 8hrly
( + Gentamicin** if hospital acquired)
pneumonia
CURB 65 score:
Confusion (new onset), urea
>7, RR>30, diast BP<60 or syst
BP<90,
age >65 yrs
Additional features:
hypoxia (PO
2
<8Kpa) or multilobe
changes.
limited soft tissue
infection
Flucloxacillin 1g 6hrly
or if true penicillin allergy
Clarithromycin 500mg 12hrly
Duration 7 days
severe cap
CURB 65 score: 3 or 2 with one
additional feature
or CAP plus sepsis syndrome:
IV Coamoxiclav 1.2g 8hrly
and Clarithromycin 500mg 12hrly
or if true penicillin allergy use
IV Clarithromycin 500mg 12hrly
+/- Vancomycin
Total duration (IV plus oral thera-
py) 7 days (Pneumococcal) to 21
days (confrmed Legionella)
moderate to severe
cellulitis / erysipelas
Flucloxacillin 1-2g 6hrly IV
+ / -
Benzylpenicillin 1.2g 6hrly IV
+ / -
Gentamicin**
or if true penicillin allergy
Vancomycin**
+ / -
Gentamicin**
Gastroenteritis
No antibiotic usually required
lower utI/cystitis
Antibiotics if; urinary symptoms
+ positive urinalysis (leucocytes
+ nitrites in clean catch urine).
Obtain urine culture. Consider
delaying antibiotic therapy pend-
ing culture. Catheter specimen
of urine is unreliable.
Trimethoprim 200mg 12hrly
or
Nitrofurantoin 50mg 6hrly
(avoid if renal impairment)
Duration 3 days
urgent IV therapy
meningitis
IV Ceftriaxone 2g 12hrly +
Dexamethasone 10mg 6hrly
If age >55 or immunosuppression
or pregnancy add Amoxicillin 2g
4hrly
If penicillin resistant, pneumo-
coccus suspected
ADD Vancomycin**
Duration 7 days (meningococcal),
14 days (pneumococcal), 21 days
(listeria).
Dexamethasone for 4 days.
possible encephalitis
Aciclovir 10mg/kg 8hrly (see
prescribing guidance for dosage
alteration in renal impairment)
Duration 10-14 days
**Gentamicin/Vancomycin**
see prescribing guidance
pyelonephritis
Oral Ciprofoxacin 500mg 12hrly
( 750mg if Pseudomonas
suspected)
or
IV Amoxicillin 1g 8hrly
+ Gentamicin**
Total duration (IV/oral) 10 days
Intra-abdominal /
hepatobiliary / pelvic
sepsis
IV Amoxicillin 1g 8hrly
+ Metronidazole 500mg 8hrly
+ Gentamicin**
or
If true penicillin allergy
Vancomycin** plus Metronidazole
500mg 8hrly plus Gentamicin**
NB. Pancreatitis does not require
antibiotic therapy unless compli-
cated by gallstones
Total duration (IV/oral) 7-10 days
Further adVIce Can be obtained from the Duty Microbiologist or Clinical Pharmacist or the ID Unit (Brownlee Centre), Gartnavel General Hospital,
or your local Respiratory Unit (for pneumonia). Infection Control advice may be given by the duty microbiologist.
Greater Glasgow & Cyde Antimicrobial Utilisation Committee, ADTC. 10th July 2008. Review updates on .www.ggcformulary.scot.nhs.uk/Guidelines MIS 165760/a.
Infection Management Guideline: Empirical Antibiotic Therapy
hospital-acquired pneumonia
(occurring >48hrs post-admission or within
10 days of discharge)
As for CAP and consider adding IV Gentamicin
Vancomycin
non-severe community-
acquired pneumonia (cap)
CURB 65 score: 2
Amoxicillin 500mg 8hrly
or if true penicillin allergy or
atypical suspected
Clarithromycin 500mg 12hrly
or
Doxycycline 100mg 12hrly
Duration 7 (10 days if atypical)
1st line hospital therapy
Amoxicillin 500mg 8hrly or
Clarithromycin 500mg 12hrly or
Doxycyline 200mg stat then
100mg daily
Duration 5 days
IV therapy to be administered
URGeNTLy on arrival at
hospital and after blood cultures.
CT scan before LP if age >60,
seizures, reduced GCS, CNS
signs or immunosuppression.
Seek ID / microbiology advice.
consider mrsa infection
healthcare associated sepsis,
recent hospital discharge, post-
operative wound or line-related
sepsis or sepsis in previous or
current MRSA carrier.
consider severe streptococcal
sepsis e.g. pharyngitis, erythro-
derma, hypotension.
consider infective
endocarditis e.g. IVDU, line-
related sepsis, recent dental
extraction.
source unknown
IV Amoxicillin 1g 6hrly
+ Flucloxacillin 2g 6hrly (Vanco-
mycin if true penicillin allergy)
and Gentamicin**
possible mrsa infection
IV Vancomycin**
+ Gentamicin**
possible infective
endocarditis
Seek senior specialist advice.
Ben Pen 2.4g 6hrly + Flucloxacil-
lin 2g 4hrly + Gentamicin**
or if true penicillin allergy / sus-
pected resistance
Vancomycin** + Gentamicin**
possible streptococcal
sepsis (?source)
ADD Clindamycin 900mg 8hrly
(up to 1200mg 6hrly) to above
and seek ID/microbiology advice
2nd line hospital therapy
Doxycyline 200mg stat then
100mg daily
Duration 5 days
bone / joint infection
septic arthritis / osteomyelitis
- Underlying metal work
- Recent surgery
Consider orthopaedic referral
septic arthritis /
osteomyelitis
Flucloxacillin 2g 6hrly IV +
Benzyl penicillin 1.8g 6hrly IV
+ / -
Gentamicin**
or if true penicillin allergy or
MRSA suspected
Vancomycin**
+ / -
Gentamicin**
diabetic foot sepsis
as above + / -
Metronidazole 400mg 8hrly po
Total duration (IV/oral) depend-
ent on surgical intervention.
Discuss with microbiology/ID.
Usually 6 weeks.
Obtain synovial fuid / deep tissue
as appropriate when possible
IV therapy usually
spontaneous bacteria peri-
tonitis
Chronic liver disease with ascites:
send peritoneal aspirate in both
blood culture bottles and universal
container to microbiology.
If peritoneal white cell count >
500/mm
3
or >250 neutrophils/mm
3
Co- amoxiclav 1.2g 8hrly
Total duration (IV/oral) 7-10 days
Immunocompromised
patient
Sepsis syndrome
No defnable site of infection
Immunocompromised plus
sepsis
Piperacillin - Tazobactam 4.5g
6hrly + Gentamicin**
Consider Staphylococcal infec-
tion (e.g. line-related sepsis or
soft tissue infection)
ADD IV Vancomycin**
N.B. If haematology/oncology
patient discuss with appropriate
specialist and seek ID / microbi-
ology advice.
Guidance for initial hospital therapy in adults.
specialist units may have separate policies.
ratIOnalIse antIbIOtIc therapy when microbiology results become available or clinical condition changes.
Review IV therapy daily and remember IV-Oral sWItch
catheter-related utI
Remove/replace catheter and
culture urine. Give single dose
IV agent as per pyelonephritis.
Further antibiotic treatment may
not be required. However:
- If cystitis, treat as above.
- If sepsis or deterioration treat
as for pyelonephritis as below.
human or animal infected
bite
Co-amoxiclav 625mg 8hrly
or if true penicillin allergy
seek Microbiology / ID advice
Duration 7 days
seVere InFectIOns or InFectIOns Where IV therapy Is usually recOmmended
severe human or animal
infected bite or peri-anal
infection
Co-amoxiclav 1.2g 8hrly
or if true penicillin allergy
seek Microbiology / ID advice
Total duration (IV/oral) 10-14 days
diabetic foot sepsis
- Ulcer, probes to bone?
- Neuropathy?
- Peripheral vascular disease?
- MRSA risk?
For outpatient therapy consult
diabetic clinic guidelines
review all anatomical systems
Hospital vs community-acquired
infection? eColi, Staph aureus
and Pneumococcus are com-
monest community blood culture
isolates
Which patient?
Chemotherapy within 3 weeks,
high-dose steroids (>15mg/day
for >2 weeks), other immunosup-
pressive agents (e.g. anti-TNF,
cyclophosphamide), neutrophil
<0.5 or < 1.0 and falling, primary
immunodefciency.
NB. For patients with HIV infec-
tion please discuss with the IDU,
Brownlee Centre.
Clostridium diffcile
associated diarrhoea :
Stop / simplify concomitant
antibiotics and gastric acid sup-
pressive therapy if possible.
severe if; colonic dilatation
>6cm or white cell count >15 or
Creatinine >1.5 xs baseline or
albumin 25
non-severe; oral metronida-
zole 400mg 8hrly
severe or no improvement
after 5 days of metronidazole
or recurrence ; oral vanco-
mycin 125mg 6 hrly (add IV
Metronidazole 500mg 8hrly if
ileus or hypotension)
Total duration 10-14 days
suspected necrotising fasciitis or severe or
rapidly progressive infection in IVdu
Flucloxacillin 2 g 4 hrly + Benzylpenicillin 1.8g 4 hrly +
Gentamicin**
AND Clindamycin 900mg 8hrly IV (up to 1200mg 6hrly) AND
CONSIDeR eARLy DeBRIDeMeNT/ exPLORATION .
review antibiotic therapy daIly: stop? simplify? switch?
stOp and thInK beFOre yOu GIVe antIbIOtIc therapy! Antibiotics are overused in the elderly (particularly patients with urinary catheters or suspected UTIs) and in patients with viral or non-infective exacerbations of COPD.
Always obtain cultures and consider delay in therapy unless there is a clear anatomical site of infection with high probality of bacterial aetiology, if sepsis syndrome is present or if there is clinical deterioration.
- 10 -
NHS DUMFRIES & GALLOWAY
ADULT IV to ORAL ANTIBIOTIC SWITCH THERAPY GUIDELINES
0eveloped by AntImIcrobIal Team July 2008.
FevIew 0ate July 2009.
7ersIon 2.
This policy aims to:
1. Reduce hospital acquired infections by promoting early removal of IV cannulae
2. Reduce adverse events associated with parenteral antibiotic therapy
3. Improve use of resources
Patients receiving IV antibiotics MUST be considered for a switch to oral WITHIN THE FIRST 48 hours and every
24 hours thereafter IF the following inclusion criteria are MET and NONE of the specific exclusion criteria apply.
The need for IV therapy should be reviewed after 24 hours however 48 hours will be usually be required to
observe a pattern of improvement assuming the use of IV antibiotic has been appropriate initially.
SpecIfIc excIusIon crIterIa
Dral route compromIsed:
o 7omItIng/nIl by mouth
o UnconscIous wIthout enteral feed tubes
o |echanIcal swallowIng dIsorder
o Dral fluIds not tolerated
AbsorptIon problem: dIarrhoea/steatorrhea
ContInuIng severe sepsIs
2 or more from:
- Temp J8`C or J6`C
- Heart beat 90bpm
- FespIratory rate 20/mInute
- WorsenIng WCC and/or CFP
FebrIle wIth neutropenIa - neutrophIls 1
SpecIfIc IndIcatIons:
o menIngItIs/encephalItIs
o endocardItIs
o ImmunosuppressIon
o osteomyelItIs
o septIc arthrItIs
o deep abscess
o cystIc fIbrosIs
o severe soft tIssue InfectIons such as group A
streptococcal InfectIons
o HIckman (central) lIne InfectIon
No oral formulatIon of the drug or specIfIed alternatIve
avaIlable
CeneraI IncIusIon crIterIa
o Able to swallow and tolerate
oral fluIds
o ClInIcal Improvement
o Temperature J6`C J8`C for
at least 48 hours
o Heart rate 90 bpm for
prevIous 12 hours
o Dral formulatIon or
alternatIve avaIlable
SuItable for swItch:
Yes
SwItch to oral therapy (usually for 5 to
7 days)
o Check contraIndIcatIons, A0Fs
and potentIal drug
InteractIons In 8NF
o Change on drug kardex
o Femove 7 cannula If not
requIred
No
ContInue to revIew
the need for 7
antIbIotIcs every 24
hours.
|onItor venflon sIte
daIly every tIme vItal
sIgn observatIons are
made.
The rationale to
continue IV therapy
must be clearly
documented in
medical notes
Be guided by culture
and sensitivities.
If in doubt contact
consultant
microbiologist
- 11 -
NHS DUMFRIES & GALLOWAY
ADULT IV to ORAL ANTIBIOTIC SWITCH THERAPY GUIDELINES
0eveloped by AntImIcrobIal Team July 2008.
FevIew 0ate July 2009.
7ersIon 2.
IV agent DraI agent wIth dose suggestIons** LIquId and rectaI formuIatIons avaIIabIe
AmoxIcIllIn AmoxIcIllIn 500mg 8 hourly AmoxIcIllIn suspensIon 125mg/5mls E
250mg/5ml
8enzylpenIcIllIn PenIcIllIn 7
1
500mg1g 6 hourly
DP AmoxIcIllIn
1
500mg T0S
PenIcIllIn 7 oral solutIon 125mg/5mls E
250mg/5mls
AmoxIcIllIn suspensIon 125mg/5mls E
250mg/5ml
CefuroxIme / CeftrIaxone /
CefotaxIme
CoamoxIclav 625mg 8 hourly or J75mg 8 hourly (dependent on
possIble sIde effects)
CoamoxIclav dIspersIble tabs (+ AmoxIcIllIn
suspensIon for hIgher dose)
CIprofloxacIn CIprofloxacIn
2
500-750mg 12 hourly (If pseudomonas suspected
Increase to cIprofloxacIn 750mg 12 hourly
CIprofloxacIn suspensIon 250mg/5mls
ClarIthromycIn ClarIthromycIn 500mg 12 hourly ClarIthromycIn suspensIon 125mg/5mls E
250mg/5mls
ClIndamycIn ClIndamycIn 60kg J00mg 6 hourly
60kg 450mg 6 hourly
No lIquId formulatIon avaIlable
CoamoxIclav CoamoxIclav 625mg 8 hourly or J75mg 8 hourly (dependent on
possIble sIde effects)
CoamoxIclav dIspersIble tabs (+ AmoxIcIllIn
suspensIon for hIgher dose)
FlucloxacIllIn FlucloxacIllIn 500mg 1g 6 hourly FlucloxacIllIn oral solutIon 125mg/5mls E
250mg/5mls
CentamIcIn CIprofloxacIn 500mg bd or 750mg bd If pseudomonas suspected
2
CIprofloxacIn suspensIon 250mg/5mls
|etronIdazole |etronIdazole 400mg 8 hourly |etronIdazole suspensIon 200mg/5mls and
500mg supposItorIes
FIfampIcIn FIfampIcIn 0.6 1.2g daIly In 2 - 4 dIvIded doses FIfampIcIn syrup 100mg/5ml
TazocIn CoamoxIclav 625mg tId CoamoxIclav dIspersIble tabs (+ AmoxIcIllIn
suspensIon for hIgher dose)
1. Amoxicillin has slightly better tissue penetration than Penicillin V, and is better for deep seated infections.
2. Oral ciprofloxacin has excellent bioavailability, good tissue and pus penetration and is active against pseudomonas.
The tabIe above appIIes onIy to patIents wIth normaI renaI functIon. 0oses shouId be adjusted accordIng to severIty of InfectIon.
- 12 -
Version 1
N.B Some medicines listed in the antibiotic guidelines have been placed in the amber category as additional care is required
in the decision to prescribe.
Issued January 2008
Review March 2009
Developed by the Antimicrobial Management Team
1
Dumfries and Galloway Royal Infirmary and
Galloway Community Hospital
ANTIBIOTIC PRESCRIBING PROTOCOL
ANTIBIOTIC TRAFFIC LIGHT SYSTEM
This system, in conjunction with the
antibiotic guidelines, aims to ensure that
antibiotics are prescribed appropriately.
The aim is to ensure patients receive
optimum therapy, reduce the risk of side
effects and slow down the emergence of
resistance.
The traffic light system has THREE groups
of antibiotics:
GREEN --- Available for all
prescribers in line with current
antibiotic prescribing guidelines.
AMBER --- Prescription
restricted to approval by
consultant. Consultant approval
must be documented in the
medical notes.
RED --- Available only after
discussion with consultant
microbiologists or infectious
diseases consultant.
GREEN
(Available to all prescribers in line with current antibiotic
prescribing guidelines)
ANTIBACTERIAL AGENTS
Amoxicillin IV/PO
Ampicillin IV (For listeria meningitis only)
Azithromycin PO
Benzylpenicillin IV
Cefixime PO
Cefotaxime IV
Ciprofloxacin PO
Clarithromycin PO/IV
Clindamycin PO/IV
Co-amoxiclav (Augmentin) PO/IV
Doxycycline PO
Flucloxacillin IV/PO
Gentamicin IV - once daily regime unless directed otherwise
by microbiologists
Levofloxacin PO/IV
Metronidazole IV/PO
Phenoxymethylpenicillin (penicillin V) PO
Tazocin IV
Trimethoprim PO
Vancomycin PO - for antibiotic associated
diarrhoea/pseudomembranous colitis only
ANTIFUNGAL AGENTS
Fluconazole PO
Nystatin suspension
Terbinafine PO
ANTIVIRAL AGENTS
Aciclovir PO/IV
Valaciclovir PO
- 13 -
Version 1
N.B Some medicines listed in the antibiotic guidelines have been placed in the amber category as additional care is required
in the decision to prescribe.
Issued January 2008
Review March 2009
Developed by the Antimicrobial Management Team
2
AMBER
(Only available if approved by consultant. Consultant
approval should be documented in medical notes.)
ANTIBACTERIAL AGENTS
Liposomal
Amphotericin
(Ambisome)
For febrile neutropenics only
Ceftazidime IV Paediatrics only
Cefalexin PO Paediatrics and out of hours only
Ceftriaxone IV
Cefuroxime IV/PO Except Surgical Prophylaxis
Ciprofloxacin IV
Colistin Neb/IV
Erythromycin PO/IV
Ethambutol PO
Isoniazid PO
Itraconazole PO
Nitrofurantoin PO
Ofloxacin PO
Rifampicin PO/IV Do not use as single agent
Rifater PO
Rifinah PO
Sodium Fusidate PO
Vancomycin IV
Tobramycin IV
Penicillin Allergy
Patients with a history of anaphylaxis or
urticaria or rash occurring immediately after
penicillin therapy are at increased risk of
immediate hypersensitivity to penicillins and
should not receive beta-lactam antibiotics. This
includes co-amoxiclav, cephalosporins, tazocin
and meropenem
Patients with a history of rash occurring
more than 72 hours after administration
of penicillin are probably not allergic to
penicillin.
RED
(These will NOT be supplied by Pharmacy unless
approved by Consultant Microbiologist/ ID physician)
ANTIBACTERIAL AGENTS
Aztreonam IV
Chloramphenicol IV/PO
Co-trimoxazole (Septrin) PO/IV
Dapsone PO
Daptomycin IV
Ertapenem IV
Linezolid IV/PO
Meropenem IV
Moxifloxacin PO
Pentamidine Nebulised
Pivmecillinam PO
Sodium Fusidate IV
Synercid IV
Teicoplanin IV
Tigecycline IV
ANTIFUNGAL AGENTS
Caspofungin IV
Fluconazole IV
Itraconazole IV
Lipsomal amphotericin (Ambisome) IV
Posaconazole PO
Voriconazole IV/PO
ANTIVIRAL AGENTS
Famciclovir PO
Zanamivir (Inhalation)
NB Agents listed in the amber/red restricted list (shaded
entries) may not be stocked in pharmacy but if requested
by the consultant Microbiologist/ Infectious Diseases
would be available within 24 hours.
A request for an antibiotic not listed here will follow non
formulary process.
- 14 -
Appendix 2
Antibiotic Guidance for Hospital Inpatients NHS Greater Glasgow & Clyde.
(Note this was designed to be printed A3 in size, if printing it A4 in size please
ensure that in the print menu shrink to printable area is selected for the Page
Scaling setting.)
- 15 -
To contact a microbiologist:
Western 52246orpage3085 Royal 24640/1orpage3702 Gartnavel page4129
Victoria 65601/2/4orpage6137/8 Southern 61702orpage7077 Inverclyde 64492(01475504492)
Stobhill 13015(orphoneRoyal) RoyalAlexandra/ValeofLeven 46172
TocontactanIDphysicianphone2113000(GartnavelSwitchboard)andaskfortheIDconsultant/SpecialistRegistraroncall.
ANTIBIOTIC GUIDANCE FOR HOSPITAL INPATIENTS
Site of Infection:
Non-severe pneumonia or Exacerbation of COPD
a. Amoxicillin or Clarithromycin or Doxycycline
b. IV therapy if sepsis criteria present or oral route not available
Severe pneumonia; (CURB-65) score
d. Co-amoxiclav + Clarithromycin
e. Clarithromycin +/- Vancomycin (if beta-lactam allergy)
Skin and Soft tissue infection
f. Flucloxacillin or Clarithromycin (if beta lactam allergy)
g. Add Gentamicin if severe
h. Vancomycin + Gentamicin if severe + beta-lactam allergy
Lower Urinary Tract Infection
i. Trimethoprim or Nitrofurantoin
j. Exchange catheter if present
k. Add Gentamicin if severe
Pyelonephritis
l. Ciprofoxacin(oral)
m. Amoxicillin + Gentamicin if severe
Intra-abdominal / Pelvic sepsis
n. Amoxicillin + Metronidazole + Gentamicin
o. Vancomycin (if betalactam allergy) + Metronidazole
+ Gentamicin
Severe sepsis and source not known
p. Amoxicillin + Flucloxacillin + Gentamicin
q. Vancomycin + Gentamicin (if MRSA suspected
or beta-lactam allergy)
Bacterial meningitis
r. Ceftriaxone + Dexamethasone
Clostridium diffcile infection
Stop or simplify concomitant antibiotic therapy. Consider stopping
gastric acid suppressive therapy
s. Metrondiazole (oral)
t. Vancomycin (oral) for recurrent episode or if severe
u. Vancomycin (oral) + IV Metronidazole if ileus or hypotension
Additional features; Hypoxaemia Sa02 <92% or PO2 < 8kPa
or bilateral or multilobe involvement on chest X ray or Sepsis syn-
drome
If CURB-65 score on admission is
3or2criteriawithoneadditionalfeaturethepatienthas
severe CAP and IV co-amoxiclav + oral/IV clarithromycin is
appropriate.
Nonsevereif2;
2 Admit and oral therapy (IV if Sepsis)
1maybetreatedathome.
Sepsis criteria;
SignsofinfectionPLUS2ormoreoffollowing:
Infective Exacerbation of COPD
Antibiotic Rx if Purulent sputum
DonotgivedualantibiotictherapyfrstlineforCOPDexacerbations.
Lower Urinary tract Antibioticsif;urinarysymptoms+postivive
urinalysis (leucocytes + nitrites in clean catch urine). Obtain urine
culture. Consider delaying antibiotic therapy pending culture. Cath-
eterspecimenofurineisunreliable.Discusswithmicrobiology.
Clostridium diffcile severity
SevereifColonicdilatation>6cmORWCC>15
ORCreatinine>1.5xbaselineORAlbumin25
Length of therapy Guide
IncludingIVandoraltherapy,annotatetheKardexwiththeappropri-
ate duration
Pneumonia
Nonseverepneumonia(microbiologyundefned) 7days
Severepneumonia,(microbiologyundefned) 10days
Atypicalpneumonia 14-21days
Exacerbation of COPD 5 days
Uncomplicated UTI 3 days
Pyelonephritis 10 days
Cellulitis 10 days
When should IV Therapy be used? Sepsis or oral route
compromised or severe CAP or Bone/Joint sepsis or Endocarditis
ormeningitisorskin/softtissueinfection(withheat,erythemaand
induration) or oral formulation of drug not available Review IV
therapy daily!
Note:
Severity Assessment for Pneumonia
Check initial CURB-65 score
Confusion(newonset)
Urea>7.0mmol/L
Respiratoryrate30/min
BPsystolic<90mmHg/diastolic60mmHg
Age65years
Temp>38or<36
Respiratory rate > 20 /min
Pulse > 90 beats per min
WCC<4or>12
Clostridium diffcile infection is associated with prescribing of; Cephalosporins,Co-amoxiclav, Clindamycin and Quinolones
(eg Ciprofoxacin, Levofoxacin and Moxifoxacin). These agents must be restricted
See; Infection Management Guideline for detailed guidance. Discuss complex infections with microbiology or ID (see below)
Oral switch if these criteria are not present (or resolve)
Always use narrow spectrum agents when possible!
Stop therapy if bacterial infection unlikely!
STOP AND THINK BEFORE YOU GIVE ANTIBIOTIC THERAPY! Antibioticsareoverusedintheelderly(particularlypatientswith
urinarycathetersorsuspectedUTIs)andinpatientswithviralornon-infectiveexacerbationsofCOPD.Alwaysobtainculturesand consider
delay in therapy unlessthereisaclearanatomicalsiteofinfectionwithhighprobalityofbacterialaetiology,ifsepsissyndromeispresentorif
there is clinical deterioration.
GreaterGlasgow&CydeAntimicrobialUtilisationCommittee,ADTC.20thJune2008.Reviewupdateson.www.ggcformulary.scot.nhs.uk/Guidelines.MIS177136
- 16 -
Вам также может понравиться
- Angina New PDFДокумент27 страницAngina New PDFMohamad SamirОценок пока нет
- Tpnlabmonitoring PDFДокумент5 страницTpnlabmonitoring PDFMohamad SamirОценок пока нет
- Neonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualДокумент7 страницNeonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualNugraha SultanОценок пока нет
- Here are the answers to the questions:1. a2. b 3. c4. d5. a6. b7. a8. c 9. a10. b11. c12. a13. c14. d15. a16. c17. b18. a19. c20. a21. b22. c23. a 24. d25. b26. cДокумент29 страницHere are the answers to the questions:1. a2. b 3. c4. d5. a6. b7. a8. c 9. a10. b11. c12. a13. c14. d15. a16. c17. b18. a19. c20. a21. b22. c23. a 24. d25. b26. cDr-Usman Khan100% (9)
- TPN in Neonatal PDFДокумент12 страницTPN in Neonatal PDFMohamad SamirОценок пока нет
- Pharmacology SummaryДокумент16 страницPharmacology Summarysechzhen96% (46)
- Total Parenteral Nutrition (TPN) PDFДокумент8 страницTotal Parenteral Nutrition (TPN) PDFMohamad SamirОценок пока нет
- EC1 Salicyclic Acid PDFДокумент1 страницаEC1 Salicyclic Acid PDFMohamad SamirОценок пока нет
- TPN Policy PDFДокумент12 страницTPN Policy PDFMohamad Samir100% (1)
- ABC of DermatologyДокумент149 страницABC of DermatologyAndreea Alexandru100% (15)
- Pharmacology Charts PDFДокумент88 страницPharmacology Charts PDFMohamad Samir90% (10)
- BMT Total Parenteral NutritionДокумент5 страницBMT Total Parenteral NutritionDuwii CinutОценок пока нет
- DrugInteractions 2 PDFДокумент23 страницыDrugInteractions 2 PDFMohamad SamirОценок пока нет
- أدوية الطوارىءДокумент162 страницыأدوية الطوارىءManar22Оценок пока нет
- Androgen PharmacologyДокумент10 страницAndrogen PharmacologySri Nurliana BasryОценок пока нет
- Cardiovascular EmergenciesДокумент401 страницаCardiovascular EmergenciesNeslihan Avcı100% (1)
- أدوية الطوارىءДокумент162 страницыأدوية الطوارىءManar22Оценок пока нет
- Parenteral Nutrition CalculationsДокумент62 страницыParenteral Nutrition CalculationsMohamad Samir100% (1)
- Icu&Er DrugsДокумент168 страницIcu&Er DrugsMohamad SamirОценок пока нет
- Usp 797 Primer PDFДокумент20 страницUsp 797 Primer PDFMohamad SamirОценок пока нет
- Hypertension. Management PDFДокумент5 страницHypertension. Management PDFMohamad SamirОценок пока нет
- TPN in Neonatal PDFДокумент12 страницTPN in Neonatal PDFMohamad SamirОценок пока нет
- AntibioticsДокумент10 страницAntibioticsJulián David Ríos ZuluagaОценок пока нет
- Hypertension TreatmentДокумент84 страницыHypertension TreatmentMohamad SamirОценок пока нет
- Amidarone HCL SuspДокумент2 страницыAmidarone HCL SuspMohamad SamirОценок пока нет
- Amlodipine SuspДокумент2 страницыAmlodipine SuspMohamad SamirОценок пока нет
- Actazolamide SuspДокумент2 страницыActazolamide SuspMohamad SamirОценок пока нет
- Antiarrythmic DrugsДокумент25 страницAntiarrythmic DrugsMohamad SamirОценок пока нет
- FPGEE Review Guide ContentДокумент6 страницFPGEE Review Guide ContentMohamad Samir0% (3)
- Antimicrobial DrugsДокумент63 страницыAntimicrobial DrugsMohamad SamirОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- SUSPENSIONДокумент11 страницSUSPENSIONAnoosha FarooquiОценок пока нет
- 334 RegistrationДокумент220 страниц334 RegistrationMuhammad ImranОценок пока нет
- Drogueria Clinica Medica, C.A: RIF. J-31112669-4Документ3 страницыDrogueria Clinica Medica, C.A: RIF. J-31112669-4W.J A.GОценок пока нет
- Hope Hospital Self Assessment ToolkitДокумент120 страницHope Hospital Self Assessment Toolkitcxz4321Оценок пока нет
- Kerbala University Lab Booklet for Pharmaceutical CalculationsДокумент9 страницKerbala University Lab Booklet for Pharmaceutical Calculationssultan100% (1)
- 3 3 2 A Med History 3 2Документ2 страницы3 3 2 A Med History 3 2api-263196423Оценок пока нет
- Drug Stores - VirarДокумент6 страницDrug Stores - VirarTal subuОценок пока нет
- StreptokinaseДокумент8 страницStreptokinaseemman_abzОценок пока нет
- Cannabinoids and Cancer - Abrams and GuzmanДокумент8 страницCannabinoids and Cancer - Abrams and GuzmanprojectcbdОценок пока нет
- Eu Guide To Good Manufacturing Practice PDFДокумент2 страницыEu Guide To Good Manufacturing Practice PDFAmandaОценок пока нет
- MilleniumДокумент2 страницыMilleniumrahul_dua111100% (1)
- Class 5Документ430 страницClass 5Subash NeupaneОценок пока нет
- Data Collection Form RetrospectiveДокумент3 страницыData Collection Form Retrospectivejamilah AlnahdiОценок пока нет
- Classic Hallucinogens: LSD (D-Lysergic Acid Diethylamide) - Also Known As Acid, Blotter, Doses, HitsДокумент3 страницыClassic Hallucinogens: LSD (D-Lysergic Acid Diethylamide) - Also Known As Acid, Blotter, Doses, HitsName ToomОценок пока нет
- Citizens For Responsibility and Ethics in Washington: by First Class Mail and E-Mail (Mallen@osmre - Gov)Документ7 страницCitizens For Responsibility and Ethics in Washington: by First Class Mail and E-Mail (Mallen@osmre - Gov)CREWОценок пока нет
- Jujube FruitДокумент5 страницJujube FruitnasmiОценок пока нет
- Cough N Cold Medicine List PDFДокумент7 страницCough N Cold Medicine List PDFDonna DominnoОценок пока нет
- Drugs Powerpoint MidtermДокумент24 страницыDrugs Powerpoint MidtermRicka Racquel Dugan BravanteОценок пока нет
- Italian Folk HerbsДокумент12 страницItalian Folk HerbsMelissa Farruggio McNairОценок пока нет
- Veramita Augusta Arisandy&Team - EDAWA - Full PaperДокумент6 страницVeramita Augusta Arisandy&Team - EDAWA - Full PaperveramitaugustaОценок пока нет
- Antibiotics: Review of Ceftazidime-Avibactam For The Treatment of Infections Caused by Pseudomonas AeruginosaДокумент24 страницыAntibiotics: Review of Ceftazidime-Avibactam For The Treatment of Infections Caused by Pseudomonas AeruginosaVictor Hugo SilveiraОценок пока нет
- Narayana Dental Journal Vol I Issue 1.pdf Final 1 PDFДокумент58 страницNarayana Dental Journal Vol I Issue 1.pdf Final 1 PDFsivaram_12213443Оценок пока нет
- Approved DrugsДокумент165 страницApproved DrugsHelenОценок пока нет
- Drugs and Poison InformationДокумент7 страницDrugs and Poison Informationnoor nizamiОценок пока нет
- Equipment Cleaning ValidationДокумент11 страницEquipment Cleaning Validationhabibshaikh0973% (11)
- Calculate Health Insurance Costs and Savings with Sample Medical ExpensesДокумент2 страницыCalculate Health Insurance Costs and Savings with Sample Medical ExpensesKathleen0% (1)
- Advertising of Nonprescription Medicines To The Public: A Significant Contributor To HealthcareДокумент32 страницыAdvertising of Nonprescription Medicines To The Public: A Significant Contributor To HealthcareSherif Adel EmamОценок пока нет
- Link e Katalog Obat CTM Per 10 Juli 23Документ175 страницLink e Katalog Obat CTM Per 10 Juli 23SarjanaMudaОценок пока нет
- Antifungal Breakpoints V 9.0 180212Документ5 страницAntifungal Breakpoints V 9.0 180212hergoОценок пока нет
- Plant Molecular Farming For Recombinant Therapeutic ProteinsДокумент61 страницаPlant Molecular Farming For Recombinant Therapeutic Proteinsnitin_star2010Оценок пока нет