Академический Документы
Профессиональный Документы
Культура Документы
Chapter 4c Emergency Medicine in The Podiatric Office
Загружено:
podmmgfИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Chapter 4c Emergency Medicine in The Podiatric Office
Загружено:
podmmgfАвторское право:
Доступные форматы
4.
Emergency Medicine in the Podiatric Office
Melvyn Grovit, DPM, MS, CNS
Emergencies occurring in the podiatric office setting require a focused history and physical examination to provide adequate assessment and effective management of the emergency condition. The guiding influence in virtually any emergency is the adherence to principles of the ABCs: Assess and clear the Airway; Assess and ensure Breathing; Assess and maintain Circulation. Emergency conditions therefore can generally be approached and managed by supporting respiration, cardiac function, and central nervous system equilibration. For the purpose of this review, we will classify the most common emergencies according to the system principally affected and provide for the specific management for those emergencies within a given system.
Initial Procedures
In all instances the patient should be placed in an appropriate position (Fowler, Semi-Fowler, Trendelenburg, Thorax flat, Legs elevated 30, Sit-up, or Coma) depending upon desired effects upon respiration and/or hemodymanics. EMS should be summoned immediately and it is the role of the podiatrist to ensure optimal patient care until the arrival of EMS personnel. I.V. access should be established early as profound hypotension, such as occurs in shock, may preclude finding a suitable vein. If pulmonary or cardiac arrest are established at any time, CPR must be initiated with all due haste.
Approach to the Patient with Respiratory Distress
Dyspnea
Clinical Features Dysphea may have multi-factorial origins and is a subjective feeling of difficult, labored, or uncomfortable breathing. The patient presents with tachypnea, tachycardia, stridor and use of assessory respiratory muscles (sternocleidomastoid, supraclavicular and intercostal). Other subjective and objective findings are inability to speak, agitation, or lethargy (due to hypoxia and paradoxical abdominal wall retraction upon inspiration). Management There is no single cause of dyspnea. Therefore, the primary management goal is to maintain a patent airway and provide appropriate oxygenation; in COPD, by nasal cannula at low flow (2L, 28% O2), in impending respiratory arrest, high flow (15L, 95% O2) by non-rebreathing mask in the conscious patient and bag-valve mask (15 L 100%) in the unconscious patient. Moderate degrees of dyspnea can be managed with varying flow rates and O2 percentages via nasal cannula, 1L = 24% O2. Each additional liter of O2 by nasal cannula delivers an additional 4% O2, 1 L = 24%, 2L = 28%, 4 L = 36%, etc.) In a spontaneously breathing patient, oxygen delivery by nasal cannula becomes less effective beyond 6-7L owing to the escape of oxygen into the atmosphere.
Medicine | Emergency Medicine in the Podiatric Office
277
Wheezing Secondary to Bronchospastic Disease (Asthma, COPD)
Clinical Features Dyspnea Chest tightness Wheezing Cough The wheezing presents as a prolonged expiratory component. An associated state of hypoxia is characterized by tachypnea, cyanosis, agitation and apprehensiveness, tachycardia and hypertension. It should be noted that patients with the most profound airway obstruction may not wheeze at all and their respiratory competence should then be evaluated by lung auscultation. Pulsus paradoxicus in excess of 20 mm/Hg. may be present. Diaphoresis and somnolence indicate hypercapnia and respiratory acidosis. The presence of cyanosis indicates tissue hypoxia. There are two levels of cyanosis: peripheral and central. In peripheral cyanosis the skin is reactive, and in central cyanosis the skin and mucous membrane areas are involved indicating more profound hypoxia. It may be difficult to establish a primary source of cyanosis as there may be an admix of mechanisms. Condition specific oxygen administration, at the appropriate flow and percentage, is advisable. Management Establish a patent airway; loosen collar, etc. Sit-up position Administer a Beta-agonist by inhalation, such as albuterol (1-2 inhalations) Administer underlying disorder - specific medications Pulmonary edema = furosemide 40-80 mg I.V. Severe asthma = epinephrine 1:1000, 0.3-0.5 ml. subcutaneously Oxygen 2-4L (28%-36%) by nasal cannula Transport the patient to the hospital
Approach to the Patient in Cardiovascular Compromise
Chest Pain
Clinical Features The pneumonic P, Q, R, S, T establishes the history of the event; Provocation, Quality, Radiation, Severity, Time of onset of pain. Associated findings, such as diaphoresis, nausea, or vomiting are of concern and indicate an increased likelihood of an ischemic event. Pain may be retrosternal or radiate to the left shoulder, arm, hand or jaw. The history of age above 40, male or postmenopausal female, hypertension, cigarette smoking, hypercholesterolemia, diabetes, truncal obesity, family history, and sedentary life style pose serious risk factors pointing to increased risk for an ischemic event. Differential diagnosis includes myocardial infarction, unstable angina, aortic dissection, pulmonary embolism, pneumothorax, and esophageal rupture. Palpitations further raise the index of suspicion of myocardial ischemia. Musculoskeletal origin of pain may be ruled out by movement, as movement will increase the pain.
278 The 2005 Podiatry Study Guide
Office Emergency Management: Activate EMS. Fowler position Administer oxygen 4L, 36% by nasal cannula. If COPD is present, administer 2L, 28% by nasal cannula Maintenance of appropriate oxygenation is determined by frequent monitoring of the patients condition Establish I.V. access with 5% dextrose in water Administer underlying disorder- specific medications Angina sublingual nitroglycerin 1/150 gr. sublingual q 5 minutes up to 3 doses or until relief of symptoms Myocardial Infarction sublingual nitroglycerin as above. Morphine sulfate I.V. 2-4 mg, if available, will relieve pain and reduce preload, 325mg ASA p.o. for inhibition of platelet aggregation
Cardiac Arrest
Basic life support, EMS transports the patient to the hospital. The hospital evaluation of an acute myocardial infarction will begin with an immediate EKG to establish the indication for thrombolytic therapy.
Approach to the Patient with CNS Disturbance
A rapid assessment of the nervous system in the podiatric office can be accomplished by evaluation of mental status, speech process and content, sensation, coordination, reflexes, motor control including gait with associated movements. differential diagnosis of conditions involving the CNS in some manner are remembered by the following pneumonic: TIPS = Trauma, Infection, Psychiatric, Space occupying lesions. AEIOU = alcohol (and drugs), endocrine, insulin, oxygen, uremia. The goal of the assessment is to differentiate structural focal CNS conditions from diffuse metabolic processes. There are three conditions representative of the more common conditions altering mental status: vasovagal syncope, hypoglycemia, and seizure disorders. Clinical Features Vasovagal Syncope: Prodromal subjective complaints include blurring of vision, dizziness, pallor, nausea and diaphoresis occurring in the setting of environmental stimuli, such as fear, pain, and/or excessive heat. Management Have a high index of suspicion of more life-threatening processes, such as cardiac events, CVA, and drug reactions. Placing the patient in a position supporting increased cerebral circulation (Trendelenburg, Thorax flat, Legs elevated 30) is usually sufficient.
Hypoglycemia
Patients with hypoglycemia have a wide array of presenting signs and symptoms based upon the neuroglycopenic and compensatory sympathomimetic effects. Since the principal fuel in the brain is glucose, it is not surprising to find CNS dysfunction associated with glucose levels < 50 mg./dL. The patient experiences lethargy, confusion, combativeness, agitation, and unresponsiveness. More extreme manifestations are the development of seizures and focal neurologic deficits. When the counter-regulatory hormones epinephrine and norepinephrine are stimulated, the patient experiences anxiety, nervousness, irritability, nausea, vomiting, palpitations and tremor.
Medicine | Emergency Medicine in the Podiatric Office
279
Management Fowler position (low), or supine, or Trendelenburg Finger stick glucose. Result <50 mg/dL IV 50% dextrose in water followed by another ampule of 50% dextrose in water if the finger glucose does not return to a normal range (>100 mg/dL) If IV route of dextrose administration is unobtainable give 1 mg of glucagon IM, followed by oral glucose when the patient is conscious. Glucagon activates the release of glycogen as glucose and therefore the effect may be short-lived if additional glucose is not available when liver glycogen is depleted. Comorbid conditions such as cardiac disorders dictate activating EMS and transporting the patient to the hospital
Seizure Disorders
Seizure disorders may be categorized as focal, generalized, and focal with secondary generalization. A focal seizure affects only a defined area of the body. A generalized seizure involves the entire body. Focal with secondary generalization begins in a localized area of the brain and then spreads to involve the entire brain resulting in generalized seizure activity. Clinical Features Abrupt onset and termination Lack of recall Purposeless or inappropriate movement A postictal period of confusion and lethargy Loss of continence Management Status epilepticus is defined as either seizure activity lasting 30 minutes or more or two or more seizures that occur without full recovery of consciousness between attacks. Status epilepticus requires urgent treatment. EMS should be activated. The patient should be protected from trauma. Start an IV with normal saline or lactated Ringers solution. Lorezapam 2 mg or diazepam 5mg IV is administered, slowly so as to guard against respiratory arrest. The maximum dose of diazepam is 20mg. Oxygenation can be accomplished by nasal cannula, 46 L/min., 36%-44%. It should be appreciated that benzodiazapines can induce respiratory arrest, which would necessitate immediate endotracheal intubation. The patient should be transported to the hospital as soon as possible. Many seizures of limited duration require no emergency treatment other than careful monitoring of vital signs, proper positioning (coma position) to prevent aspiration. In all circumstances, the patients physician should be notified.
Approach to the Patient with Anaphylaxis
Anaphylaxis is the most severe form of systemic allergy, which results in profound respiratory and cardiovascular decompensation. Perhaps the most common cause of anaphylaxis in the podiatric office may be related to the paraben preservatives in local anesthetics. The most commonly used local anesthetic, lidocaine, enjoys an excellent record of safety. In some atopic individuals, however, an untoward reaction may occur.
Clinical Features
The clinical presentation generally occurs rapidly after an exposure to the allergen. It begins with pruritis, cutaneous flushing and urticaria, which then proceeds to feelings of fullness in the throat, chest tightness, dyspnea, lightheadedness, and subsequent loss of consciousness.
280 The 2005 Podiatry Study Guide
Office Emergency Management
Note time of onset of reaction Exposure to the causative agent should be terminated EMS should be activated Semi-Fowler position and adjust according to assessment Establish airway patency Assist breathing as required with high flow oxygen, 15 L/min, 100% Establish IV access with large bore angiocatheter Administer medications according to assessment Epinephrine 1:1000, 0.3 0.5 ml subq. For adults. This is important to administer ASAP in order to counter the systemic effects of released histamine. It may be advisable to administer the subq. epinephrine prior to establishing IV access as difficulty with IV access may cause a serious delay in desired pharmacological response. Patients on beta-blockers may be epinephrine resistant and glucagon, 1mg IV q 5 min. may also be used to advantage Diphenhydramine 50 mg IM to counter subsequent histamine release. If reaction is more severe, IV diphenhydramine 50 100 mg may be administered. Hydrocortisone 250 mg1000 mg IV or methylprednisolone 125 mg-250mg IV may be administered. It should be noted, however, that steroids have an onset of action of 4-6 hours and will have limited benefit in the acute attack. The patient should be transported to the hospital with a record of the time of onset and time and doses of medications administered
References
1. Greenberg MR, Greenberg GS, Preparing for and Managing the Podiatric Office Emergency. Lower Extremity 2, 1995 2. Markovchick VJ, Pons PT, Wolfe, RE, Emergency Medicine Secrets, Hanley & Belfus, Inc.1993. 3. Tintinalli JE, Kelen, GD, Stapczynski, JS. Emergency Medicine, A Comprehensive Study Guide, 5th edition. McGraw-Hill, 1999. 4. Tintinalli, JE, Kelen, GD, Stapczynski, JS. Emergency Medicine, A Comprehensive Study Guide, Companion Handbook, 5th edition, McGraw-Hill, 2000.
Medicine | Emergency Medicine in the Podiatric Office
281
282 The 2005 Podiatry Study Guide
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Chapter 6b Digital SurgeryДокумент18 страницChapter 6b Digital SurgerypodmmgfОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Chapter 4e Internal MedicineДокумент19 страницChapter 4e Internal MedicinepodmmgfОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Chapter 5 Pediatric PodiatryДокумент88 страницChapter 5 Pediatric Podiatrypodmmgf100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Chapter 4d Podiatric Infectious DiseasesДокумент20 страницChapter 4d Podiatric Infectious DiseasespodmmgfОценок пока нет
- Chapter 4 and 4a Introduction To Medicine and DermatologyДокумент16 страницChapter 4 and 4a Introduction To Medicine and DermatologypodmmgfОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Chapter 3g Physical MedicineДокумент20 страницChapter 3g Physical MedicinepodmmgfОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- PathoMechanics PDFДокумент36 страницPathoMechanics PDFMagnus SigaarssonОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Chapter 3e Pathological GaitДокумент8 страницChapter 3e Pathological GaitpodmmgfОценок пока нет
- Care of Clients With Physiologic and Psychosocial AlterationsДокумент34 страницыCare of Clients With Physiologic and Psychosocial AlterationsChloie Marie RosalejosОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Med Surg Respiratory SystemДокумент173 страницыMed Surg Respiratory Systembamfalcon100% (4)
- Session 3 Pathophysiology of COPD and AsthmaДокумент40 страницSession 3 Pathophysiology of COPD and AsthmaOsamaMazhariОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Pulm HTN WilcoxДокумент11 страницPulm HTN WilcoxyersiniapestismorОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- GINA 2017 Teaching Slide Set FullДокумент17 страницGINA 2017 Teaching Slide Set FullLorenzoVasquezDatul100% (3)
- NCP GunshotДокумент13 страницNCP GunshotMichael John F. Natividad0% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Formic Acid C BASF Medguidelines E036Документ4 страницыFormic Acid C BASF Medguidelines E036varrsinneОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Case Study For DiscussionДокумент3 страницыCase Study For DiscussionSiti nur Kholifatus samsiyahОценок пока нет
- Chapter 2 Respiratory AssessmentДокумент9 страницChapter 2 Respiratory AssessmentKathleen Dela CruzОценок пока нет
- Respiratory Distress Syndrome of The Newborn JCG0086 v3Документ17 страницRespiratory Distress Syndrome of The Newborn JCG0086 v3meutia salsabilaОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- An Essay On "Covid-19 Pandemic" by Prof. Dr. Mustafa Asim SafakДокумент9 страницAn Essay On "Covid-19 Pandemic" by Prof. Dr. Mustafa Asim Safakkasmakiprawi72Оценок пока нет
- NCP For BronchitisДокумент2 страницыNCP For BronchitisJefherrson Nericua Jemilo50% (2)
- Assessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale Evaluation Subjective: Short Term: Independent: IndependentДокумент4 страницыAssessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale Evaluation Subjective: Short Term: Independent: IndependentAlyssa Marie SantosОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- NURS FPX 6021 Assessment 1 Concept MapДокумент7 страницNURS FPX 6021 Assessment 1 Concept MapCarolyn HarkerОценок пока нет
- Gregori Graboboi - Quick Code ListДокумент20 страницGregori Graboboi - Quick Code Listondasdeforma93% (29)
- International Emergency NursingДокумент6 страницInternational Emergency NursingAtika AlfiaОценок пока нет
- Assessment Diagnosis Background Knowledge Plan of Care Nursing Intervention S Rationale EvaluationДокумент3 страницыAssessment Diagnosis Background Knowledge Plan of Care Nursing Intervention S Rationale Evaluationtin911Оценок пока нет
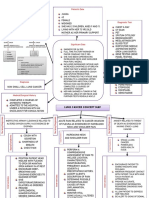
- Lung Cancer Concept Map-Group 2Документ2 страницыLung Cancer Concept Map-Group 2Maria Cristina100% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Anaphylaxis Clinical PresentationДокумент9 страницAnaphylaxis Clinical Presentationilhampaneja_x3Оценок пока нет
- The Thorax and Lungs - BATESДокумент4 страницыThe Thorax and Lungs - BATESsitalcoolk100% (2)
- CC-Concept Map 2Документ5 страницCC-Concept Map 2MDCITY50% (2)
- Reexpansion Pulmonary Edema : UpdateДокумент6 страницReexpansion Pulmonary Edema : UpdateWenny EudensiaОценок пока нет
- MCQ About Pulmonary-DiseaseДокумент31 страницаMCQ About Pulmonary-Diseaseمجتبى عليОценок пока нет
- Abdominal Aortic AneurysmДокумент10 страницAbdominal Aortic AneurysmPrince K. TaileyОценок пока нет
- RLE - Reviewer - OxygenationДокумент14 страницRLE - Reviewer - OxygenationVinzii DrtОценок пока нет
- HSNS264 Case StudyДокумент8 страницHSNS264 Case StudySophie AndersonОценок пока нет
- Clinical Manifestations and Assessment of Respiratory Disease 5th Edition Jardins Test BankДокумент36 страницClinical Manifestations and Assessment of Respiratory Disease 5th Edition Jardins Test Bankgeincupola.06zi100% (23)
- Antibiotics For Treatment and Prevention of Exacerbations of Chronic Obstructive Pulmonary DiseaseДокумент19 страницAntibiotics For Treatment and Prevention of Exacerbations of Chronic Obstructive Pulmonary DiseaseAvila CulenОценок пока нет
- Respiratory System: Study: Pulmonology Physician: Pulmonologist Function: Exchange of GasesДокумент5 страницRespiratory System: Study: Pulmonology Physician: Pulmonologist Function: Exchange of GasesSakshi BishnoiОценок пока нет
- BisinosisДокумент4 страницыBisinosisMaría IgnaciaОценок пока нет