Академический Документы
Профессиональный Документы
Культура Документы
Dont Be Intimidated by Incident Reports
Загружено:
Cherie Boulware AkinИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Dont Be Intimidated by Incident Reports
Загружено:
Cherie Boulware AkinАвторское право:
Доступные форматы
Charting Checkup
Dont be intimidated by incident reports
By JoElla Hynes, MSN Clinical Nurse Educator Edward Hospital Naperville, Ill.
ANY TIME AN incident occurs at your facility, you must ll out an incident report. An incident report (also called an event report or occurrence report) is a formal report written by practitioners, nurses, or other staff members. It serves two purposes: to inform facility administrators of incidents that allow the risk management team to consider changes that might prevent similar incidents to alert administration and the facility insurance company of potential claims or need for further investigation. The forms used for incident reports are consistently being revised and updated, and some may be electronic (see What an incident report looks like). Most healthcare facilities provide guidelines for when incident reports must be completed. Dening an incident In general, an incident is any event that affects patient or employee safety. In most healthcare facilities, injuries, patient complaints, medication errors, equipment failure, adverse reactions to drugs or treatments, or errors in patient care must be reported. Data from incident reports are tracked for quality assurance and to allow the detection of emerging trends or problems. Incident reports bring problems to light in a nonblaming way and can provide a catalyst for changing the practice or procedure that contributed to the error. An incident report should be initiated only by someone who directly observes the incident or by the rst person to arrive at the site of the incident. Fill in the blanks When lling out an incident report, include the following information: the exact time and date the names of persons involved and any witnesses factual information about what happened other relevant facts, including your actions (such as notifying the healthcare provider) and any corrective actions taken. After completing the incident report, you must sign and date it. If your incident reports are led electronically, the form will require you to type in this information.
4 LPN2009
Follow your facilitys policy regarding the policies and procedures for how the incident report is to be followed up; this will determine whether the matter needs further investigation. If the incident directly involved a patient, notify the healthcare provider. Tips to get it right Here are some valuable tips for completing an incident report. Write objectively. Describe exactly what you saw. If you didnt see the patient fall, document that you found the patient lying on the oor. Then document your actions, such as assessment of the patient for injury, assisting the patient back to bed, and calling the healthcare provider. Incorporate patient and witness accounts of the event into the report. State their comments as direct quotes. Have the witnesses assist you in preparing the report and co-sign the nal report. Dont assign blame. Refrain from pointing your nger at a coworker or your facilitys administration. An incident report isnt an opportunity for you to point out inferior equipment or poor stafng. Just state the facts. Avoid hearsay and assumptions. If your patient is injured in another department, its up to the person who witnessed the incident in that department to write the incident report. Forward the report to the person designated by your facilitys policy. Ensure that only one copy of the report exists. If other departments or committees would like to see the report, the original may be forwarded to them in succession. Act quickly Because memories fade relatively quickly after an event occurs and critical components may be forgotten, its vital to document what happened right away. An incident report is factual and complete; it doesnt include excuses for behavior or actions. The incident report is not a part of the patients medical record. In most courts, the incident report is protected from discovery by the opposing attorneys. If you document the incident report in the patients medical record, youve lost that protection. In addition to lling out the incident report, you must document the facts of the event in the patients medical record. The medical record documentation, completed
Volume 5, Number 2
close to the time of the incident report, should contain only factual, objective, descriptive documentation relative to the patients condition and response to the incident. Never try to hide or cover up a mistake.
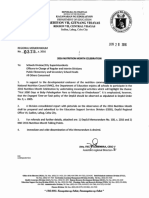
What an incident report looks like
When you witness or discover a reportable event, you must ll out an incident report. Forms vary, but most include the following information.
Incident report
DATE OF INCIDENT TIME OF INCIDENT
Name of person involved Greta Manning Address
7 Worth Way, Boston, MA (617) 555-1122
3-20-09 4-Main, Rm. 447
TYPE OF INCIDENT (CHECK ONE ONLY) PATIENT
1442
Phone
EXACT LOCATION OF INCIDENT (Bldg, Floor, Room No, Area)
Medical record number (if patient)
VISITOR
EMPLOYEE
VOLUNTEER
OTHER (specify)
, Patient s wife found on floor next to bed. States, I was trying to put Just culture the siderail of the bed down and I fell down. To promote effective reporting FLOOR CONDITIONS OTHER FRAME OF BED LOW NIGHT LIGHT YES Patient and achieve quality CLEAN & SMOOTH SLIPPERY (WET) HIGH NO fall WERE BED RAILS PRESENT? OTHER RESTRAINTS (TYPE AND EXTENT) incidents care, facilities need N/A NO 1 UP 2 UP 3 UP 4 UP to adopt whats reAMBULATION PRIVILEGE UNLIMITED LIMITED WITH ASSISTANCE COMPLETE BEDREST OTHER ferred to as a just WERE NARCOTICS, ANALGESICS, HYPNOTICS, SEDATIVES, DIURETICS, ANTIHYPERTENSIVES, OR culture. The just ANTICONVULSANTS GIVEN DURING LAST 4 HOURS? culture recognizes YES NO DRUG AMOUNT TIME Patient PHYSICIAN NOTIFIED DATE TIME COMPLETE IF APPLICABLE that its rare for Name of Physician incidents J. Reynolds, MD 3-20-09 1445 any single nurse to JOB TITLE SOCIAL SECURITY # Employee DEPARTMENT incidents be the cause of an MARITAL STATUS incident; instead, NOTIFIED DATE TIME LOCATION WHERE TREATMENT WAS RENDERED All multiple system C. Jones, RN 3-20-09 1500 incidents factors often comNAME, ADDRESS, AND TELEPHONE NUMBERS OF WITNESS(ES) OR PERSONS FAMILIAR WITH INCIDENT - WITNESS OR NOT bine to create the Janet Adams (617) 555-0912 1 Main St., Boston, MA circumstances. The just culture SIGNATURE OF PERSON PREPARING REPORT TITLE DATE OF REPORT Connie Smith, LPN LPN 3-20-09 eliminates punitive PHYSICIANS REPORT To be completed for all cases involving injury or illness (DO NOT USE ABBREVIATIONS) action against the (Use back if necessary) DIAGNOSIS AND TREATMENT person ling out , Received patient in Emergency Department after reported fall in husband s room. 12 cm x the incident report 12 cm ecchymotic area noted on right hip. X-rays negative for fracture. Good range of motion, and encourages J. Reynolds, MD no c/o pain. VAS 0/10. Ice pack applied. looking beyond the DISPOSITION sent home, written instructions provided incident to deterPERSON NOTIFIED OTHER THAN HOSPITAL PERSONNEL DATE TIME mine other factors. NAME AND ADDRESS R. Manning (daughter), address same as pt 3-20-09 1500 These factors may PHYSICIANS SIGNATURE DATE include orientation J. Reynolds, MD 3-20-09 and training, stafng ratios, and Guido GW. Legal Issues in Nursing. 4th ed. Stanford, CA: Appleton and Lange; 2005. other issues inuencing patient safety. LPN Iedema R, Flabouris A, Granti S, Jorm C. Narrativizing errors of care: critical incident reporting in clinical practice. Soc Sci Med. 2006; 62(1):134-144.
DESCRIPTION OF THE INCIDENT (WHO, WHAT, WHEN, WHERE, HOW, WHY) (Use back of form if necessary)
Selected references
Chart Smart: The A to Z Guide to Better Nursing Documentation. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. Complete Guide to Documentation. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. Ditmer D. Risk Management Strategies for Health Care Providers. Eau Clair, WI: PESI Health Care Webinar; 2008.
Scott RW. Guide for the New Health Care Professional. Sudbury, MA: Jones & Bartlett Publications; 2006. Taylor JA, Brownstein D, Christakis DA, et al. Use of incident reports by physicians and nurses to document medical errors in pediatric patients. Pediatrics. 2004;114(3):729-735. Timby BK. Fundamental Nursing Skills and Concepts. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
March/April
LPN2009
Вам также может понравиться
- OET Part C Listening - Interview & PresentationДокумент6 страницOET Part C Listening - Interview & PresentationSudhakar PaulОценок пока нет
- COE WorksheetДокумент16 страницCOE WorksheetiloveraynaОценок пока нет
- History Taking FormДокумент2 страницыHistory Taking FormMaria Santiago100% (1)
- Improving Healthcare Through Advocacy: A Guide for the Health and Helping ProfessionsОт EverandImproving Healthcare Through Advocacy: A Guide for the Health and Helping ProfessionsОценок пока нет
- AHA ACLS Provider Manual $45Документ2 страницыAHA ACLS Provider Manual $45Jigar GandhiОценок пока нет
- Ien Application Package: Type Text HereДокумент23 страницыIen Application Package: Type Text Herejyselle domingoОценок пока нет
- Nnas Applicant Handbook EnglishДокумент17 страницNnas Applicant Handbook EnglishCharlemagne C. Marban IVОценок пока нет
- Nurse InterviewДокумент1 страницаNurse InterviewTiarnida NababanОценок пока нет
- Writing Task 2Документ18 страницWriting Task 2May ThuaungОценок пока нет
- Patient Satisfaction With The Health CareДокумент15 страницPatient Satisfaction With The Health CareEmna MahjoubiОценок пока нет
- Jahshan Listening OET Collection IRS LT1Документ11 страницJahshan Listening OET Collection IRS LT1P.K.Оценок пока нет
- Nursing Job Cover Letter ExamplesДокумент8 страницNursing Job Cover Letter Examplesafmrgjwjcowaov100% (1)
- Practice Test 2 Reading Part BДокумент5 страницPractice Test 2 Reading Part BkholiooОценок пока нет
- (Osborn) Chapter 73 Learning Outcomes (Number and Title)Документ16 страниц(Osborn) Chapter 73 Learning Outcomes (Number and Title)KittiesОценок пока нет
- Anking Interview Questions You Will Be AskedДокумент6 страницAnking Interview Questions You Will Be AskedKevanОценок пока нет
- StressДокумент3 страницыStressabydlОценок пока нет
- The Oet Letter - TipsДокумент1 страницаThe Oet Letter - Tipsapi-179604969Оценок пока нет
- Oet Test SampleДокумент9 страницOet Test SampleOana Maria GrigoreОценок пока нет
- Skin Cancer Part A Nursing Oet General NoteДокумент394 страницыSkin Cancer Part A Nursing Oet General Noteiffat hanifОценок пока нет
- Veritas Mock Interview Dos Donts HandoutДокумент6 страницVeritas Mock Interview Dos Donts HandoutSanОценок пока нет
- Template of Referral Letter (Sample 1) : HistoryДокумент1 страницаTemplate of Referral Letter (Sample 1) : HistoryWYОценок пока нет
- Work Abroad 200 STAFF NURSES W - IELTS - OET Jobs in United KingdomДокумент6 страницWork Abroad 200 STAFF NURSES W - IELTS - OET Jobs in United Kingdomnoel anthony badajosОценок пока нет
- Celban Tips: LISTENING - What To Expect During The Listening TestДокумент1 страницаCelban Tips: LISTENING - What To Expect During The Listening TestJyselle DomingoОценок пока нет
- OetДокумент15 страницOetAchwani Santosh0% (1)
- LP130100171 Final Report 1 November 2017Документ41 страницаLP130100171 Final Report 1 November 2017Prasoon PremrajОценок пока нет
- OET Seeks Nursing Experts for Sub-Test CreationДокумент1 страницаOET Seeks Nursing Experts for Sub-Test Creationbaljinder4uОценок пока нет
- Role Play Nursing Care To Diare PatientДокумент7 страницRole Play Nursing Care To Diare Patientleny cahyani putriОценок пока нет
- Brought To You by Sam Agency: To Join Us Click Here Facebook or TelegramДокумент4 страницыBrought To You by Sam Agency: To Join Us Click Here Facebook or TelegramJoan Manabat BugnaОценок пока нет
- List of Programs - IM - Early DraftДокумент285 страницList of Programs - IM - Early DraftAbs Sarry100% (1)
- Sample Personal Letter Ophthalmology 1Документ1 страницаSample Personal Letter Ophthalmology 1John Christian Mirasol RnОценок пока нет
- Task 3: Authors: Cécile Viboud & Lone Simonsen Source: Public Library of ScienceДокумент7 страницTask 3: Authors: Cécile Viboud & Lone Simonsen Source: Public Library of Sciencefernanda1rondelliОценок пока нет
- OET 2 Reading Test 17 Part AДокумент6 страницOET 2 Reading Test 17 Part AAlice ChirilaОценок пока нет
- GrammarBoosterPreview PDFДокумент4 страницыGrammarBoosterPreview PDFMikeОценок пока нет
- Oet ReadingДокумент7 страницOet ReadingAditi ParmarОценок пока нет
- 19 - OET Online Test 6Документ20 страниц19 - OET Online Test 6Abdullah Mohammad Ibne HaiderОценок пока нет
- OET Reading Test Preparation: Question Types and FormatsДокумент6 страницOET Reading Test Preparation: Question Types and FormatsNimraj PatelОценок пока нет
- Test Format: Listening General Training Reading Academic Writing General Training Writing SpeakingДокумент4 страницыTest Format: Listening General Training Reading Academic Writing General Training Writing Speakingpaulo de carvalhoОценок пока нет
- Reading Sub-Test - Question Paper: Part CДокумент10 страницReading Sub-Test - Question Paper: Part CSarah Jane PetalioОценок пока нет
- CLINICAL DIPRESSION PDFДокумент15 страницCLINICAL DIPRESSION PDFSunitha Sunitha kОценок пока нет
- Common OET Grammar Mistakes in Writings Infinitives (Special Verbs)Документ16 страницCommon OET Grammar Mistakes in Writings Infinitives (Special Verbs)Chinonso Nelse NwadeОценок пока нет
- Oet Speaking Tips007Документ12 страницOet Speaking Tips007aiswarya georgeОценок пока нет
- Oet Speaking Guide: Always Start The ConversationДокумент3 страницыOet Speaking Guide: Always Start The ConversationAnaKristineBalbuenaAnobaОценок пока нет
- Pain: Onset Provocation Quality Radiation Severity Mental Status Airway Skin Moisture Pulse Color TempДокумент5 страницPain: Onset Provocation Quality Radiation Severity Mental Status Airway Skin Moisture Pulse Color TempAlvarez StevenОценок пока нет
- Reading 01Документ1 страницаReading 01Carl JardelezaОценок пока нет
- Part B 29 ImmunizationДокумент15 страницPart B 29 Immunizationfernanda1rondelliОценок пока нет
- Regular 20 Regular 30 Regular 50 Urgent 20 Urgent 30 Urgent 50Документ2 страницыRegular 20 Regular 30 Regular 50 Urgent 20 Urgent 30 Urgent 50Arwa AlgezeriОценок пока нет
- 18 - OET Online Test 4Документ22 страницы18 - OET Online Test 4DHARA MODIОценок пока нет
- Therapeutic CommunicationДокумент7 страницTherapeutic CommunicationJanineОценок пока нет
- Oet Online Test 5 Jahshan Collection Oet Listening Task ScriptДокумент21 страницаOet Online Test 5 Jahshan Collection Oet Listening Task ScriptTed DoyleОценок пока нет
- Breast Reconstraction - OET - 005 - Practice - Role - Play - by - PASS - OET PDFДокумент2 страницыBreast Reconstraction - OET - 005 - Practice - Role - Play - by - PASS - OET PDFJismy FregyОценок пока нет
- Speaking Sub-Test - Test InformationДокумент5 страницSpeaking Sub-Test - Test InformationAli Ghahreman50% (2)
- Role-play interview skills for medical professionalsДокумент5 страницRole-play interview skills for medical professionalsMaine GosimОценок пока нет
- Speaking in OETДокумент42 страницыSpeaking in OETMUHAMMED SHINOS THAIKKADANОценок пока нет
- Communication SkillsДокумент5 страницCommunication SkillssanthoshОценок пока нет
- What Is Expected in OET Speaking SubtestДокумент4 страницыWhat Is Expected in OET Speaking SubtestAmi Barnes100% (1)
- Patient Registration FormДокумент5 страницPatient Registration FormCari WithrowОценок пока нет
- The British Institute For Learning Found ThatДокумент9 страницThe British Institute For Learning Found ThatnouriiОценок пока нет
- Essential Reading Strategies Part B PDFДокумент7 страницEssential Reading Strategies Part B PDFMaster SeventhreeoneОценок пока нет
- OET2 Reading Test 1 Part AДокумент6 страницOET2 Reading Test 1 Part ATavi NicolaeОценок пока нет
- Writing Nursing Sample Test 1 2010Документ4 страницыWriting Nursing Sample Test 1 2010LOTSOFTESTSОценок пока нет
- Leaping the Hurdles: The Essential Companion Guide for International Medical Graduates on their Australian JourneyОт EverandLeaping the Hurdles: The Essential Companion Guide for International Medical Graduates on their Australian JourneyОценок пока нет
- Cataract: Presented By: HomipalДокумент12 страницCataract: Presented By: Homipalankita singhОценок пока нет
- Pharmaceutical ExipientДокумент14 страницPharmaceutical ExipientShekhar SinghОценок пока нет
- Valium drug guide for nursesДокумент2 страницыValium drug guide for nursesRhea Liza Comendador-TjernmoenОценок пока нет
- Negative Affect Erasing MethodДокумент2 страницыNegative Affect Erasing MethodmirkjhaelОценок пока нет
- Motion SicknessДокумент5 страницMotion SicknessIbrahim AbdullahОценок пока нет
- Pap SmearДокумент17 страницPap SmearMaisarah IsmailОценок пока нет
- Konversi Kode Prosedure INACBGs Ke Kode ICD 9-CMДокумент349 страницKonversi Kode Prosedure INACBGs Ke Kode ICD 9-CMTri Muhammad HaniОценок пока нет
- Gram08 28Документ21 страницаGram08 28Hendra Wana Nur'aminОценок пока нет
- Copy Pedia DrugsДокумент3 страницыCopy Pedia DrugsMonica LeeОценок пока нет
- NSTP ProjДокумент11 страницNSTP ProjLeeroi Christian Q Rubio100% (2)
- Nurs 205 Concept MapДокумент1 страницаNurs 205 Concept MapJami SpearsОценок пока нет
- OLFU Intesive Post Test 50 ItemsДокумент5 страницOLFU Intesive Post Test 50 ItemsmonmonОценок пока нет
- Dramatizing Dementia: Madness in The Plays of Tennessee WilliamsДокумент8 страницDramatizing Dementia: Madness in The Plays of Tennessee WilliamsMarcusFelsmanОценок пока нет
- Rheomac 730Документ2 страницыRheomac 730Mosstafa100% (1)
- Wound AssessmentДокумент19 страницWound Assessmentdrsonuchawla100% (1)
- Potential Long-Term Side Effects of Exposure To ChemoДокумент21 страницаPotential Long-Term Side Effects of Exposure To ChemoMichael BubleОценок пока нет
- Flopamfo 4490Документ15 страницFlopamfo 4490sabapahty chettiyarОценок пока нет
- Psychotherapy Assessment FormatДокумент10 страницPsychotherapy Assessment Formatshivani singh100% (1)
- Philippines Tuberculosis ProfileДокумент4 страницыPhilippines Tuberculosis ProfileElica Bolhano NarcisoОценок пока нет
- Brand Name Generic Name Disease Group Consumer Medicine Information More InfoДокумент9 страницBrand Name Generic Name Disease Group Consumer Medicine Information More InfoBairavi RathakrishnanОценок пока нет
- 1000 Days Ni Baby PDFДокумент31 страница1000 Days Ni Baby PDFppantollanaОценок пока нет
- Non-Modifiable Risk Factors: Modifiable Risk FactorsДокумент9 страницNon-Modifiable Risk Factors: Modifiable Risk FactorsKimberly Bomediano100% (1)
- A Case Study For Electrical StimulationДокумент3 страницыA Case Study For Electrical StimulationFaisal QureshiОценок пока нет
- Exam Procedures: Steps for Completing a Biochemistry ExamДокумент19 страницExam Procedures: Steps for Completing a Biochemistry Exampmp123456Оценок пока нет
- Biosecurity in Poultry Farms: Top PriorityДокумент3 страницыBiosecurity in Poultry Farms: Top PriorityPhénix Atakoun'sОценок пока нет
- Grade9 STE Con.-Chem. Q4 Module-5 Wk6 ADMДокумент20 страницGrade9 STE Con.-Chem. Q4 Module-5 Wk6 ADMChelzy CatabasОценок пока нет
- Nucleus DropДокумент1 страницаNucleus DropYovinus DenyОценок пока нет
- History of Psychology Milestones (387 BC to PresentДокумент4 страницыHistory of Psychology Milestones (387 BC to PresentKrea Quizo100% (1)