Академический Документы
Профессиональный Документы
Культура Документы
CyBorD Stellar Response Rates in AL AMY
Загружено:
Daniel DrimerАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
CyBorD Stellar Response Rates in AL AMY
Загружено:
Daniel DrimerАвторское право:
Доступные форматы
From bloodjournal.hematologylibrary.org by guest on May 16, 2012. For personal use only.
2012 119: 4343-4345 doi:10.1182/blood-2012-03-413112
CyBorD: stellar response rates in AL amyloidosis
Giampaolo Merlini
Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/content/119/19/4343.full.html Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
From bloodjournal.hematologylibrary.org by guest on May 16, 2012. For personal use only.
inside blood
10 MAY 2012 I VOLUME 119, NUMBER 19 CLINICAL TRIALS
Comment on Mikhael et al, page 4391, and on Venner et al, page 4387
CyBorD: stellar response rates in AL amyloidosis ---------------------------------------------------------------------------------------------------------------Giampaolo Merlini
PAVIA UNIVERSITY HOSPITAL SAN MATTEO
In two independent retrospective studies, Mikhael et al and Venner et al report unprecedentedly high hematologic response rates, 94% and 81%, including complete response (CR) in 71% and 42%, respectively, to the combination of cyclophosphamide-bortezomib-dexamethasone in patients with either naive or relapsed light chain (AL) amyloidosis.1,2
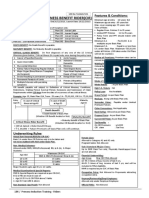
ight chain amyloidosis is caused by a small or modest, relatively indolent, plasma cell clone synthesizing misfolded light chains. These abnormal light chains behave like sick molecules, a term coined by Jan Waldenstrom, because they display a patho logic conformation prone to aggregation and become toxic for cells and tissues, producing devastating systemic damage (see gure). light chains are more prone to misfold than are light chains, and certain subgroups have been reported to be preferentially associated with specic organ targeting (eg, IGVL1-44
AL amyloidosis is caused by a small or modest, relatively indolent, plasma cell clone secreting light chains (ratio of to light chains, 4:1) with abnormal folding (misfolded) caused by mutations (symbolized by red dot) that affect critical structural sites. These light chains are prone to aggregation, form amyloid brils, and become toxic for cells and tissues, producing failure of vital organs. Heart involvement is the most clinically relevant because it is the cause of death in virtually all patients. Inset: Survival of 1131 patients with AL amyloidosis according to the year of diagnosis followed at the Pavia Amyloid Research and Treatment Center. Although survival continues to improve, the slope of the rst part of the curves has not changed during almost 30 years, mostly because of early death of patients with severe cardiac involvement. ANS indicates autonomous nervous system; CHF, congestive heart failure dened as New York Heart Association class III or IV; GI, gastrointestinal tract; and PNS, peripheral nervous system. Professional illustration by Kenneth X. Probst.
blood 1 0 M A Y 2 0 1 2 I V O L U M E 1 1 9 , N U M B E R 1 9
4343
From bloodjournal.hematologylibrary.org by guest on May 16, 2012. For personal use only.
with heart involvement).3 The misfolded monoclonal light chain can be directly cytotoxic to cardiomyocytes,4 and the extent of cardiac damage is a major prognostic determinant because heart failure and fatal arrhythmias are the cause of death in a substantial number of patients. Cardiac biomarkers, troponins, and particularly the natriuretic peptide type B (NT-proBNP), are very sensitive and reliable sensors of light chain cardiotoxicity and allow early assessment of cardiac response to therapy. They are also powerful prognostic determinants used to stratify the risk according to the Mayo cardiac staging system.5 The light chaininduced cardiac damage is progressive, but potentially reversible, unless the myocardial lesions are advanced. Improvement of cardiac function after therapy, assessed by NT-proBNP, translates into improved survival.6,7 Thus, the strategy for improving survival in AL amyloidosis should be based on early detection of amyloid cardiac involvement while the damage is still reversible, and on the rapid and profound reduction of the amyloid light chain concentration to arrest the progression of the cardiac damage and rescue the hearts function. The most sensitive, although not specic, marker of early cardiac involvement is NT-proBNP, which can anticipate the onset of symptoms related to heart failure by several months.8 Because patients with monoclonal gammopathy of undetermined signicance (MGUS) are at risk, albeit low, of developing AL amyloidosis it would be advisable that periodic checkups of individuals with this condition include measurement of NTproBNP, to detect and treat amyloid cardiomyopathy promptly. The goal of chemotherapy is rapid, profound, and persistent reduction of amyloid light chain concentration to rescue organ function and improve survival. Although signicant progress has been made toward this goal (see gure inset) standard therapy based on melphalan and dexamethasone9,10 is not effective in patients with severe cardiac involvement (Mayo cardiac stage III). The dismal outcome is mainly due to the high early death rate (23%-33%), from advanced cardiac amyloidosis, in the rst 2 to 3 months after starting therapy.9,10 These patients do not have enough time to respond to this therapy. Since the very rst investigations, it was evident that bortezomib might represent a breakthrough in the care of AL amyloidosis,
4344
producing prompt and profound responses even in pretreated patients. The molecular basis of the high sensitivity of amyloidogenic plasma cells to proteasome inhibition is still under intense investigation. A prospective phase 1/2 study on bortezomib as a single agent in relapsed patients using either a weekly or a twice-weekly schedule resulted in hematologic response rates of 68.8% and 66.7%, respectively, including 37.5% and 24.2% CR. Bortezomib showed limited cardiac toxicity. Importantly, the median time to rst response for the twice-weekly schedule was just 1 cycle. The addition of bortezomib to an alkylating agent, melphalan, and dexamethasone further improved outcome. A phase 2 prospective study including 26 patients with AL amyloidosis showed that this regimen produced a hematologic response in 94% of patients, with 56% achieving a CR.11 After impressive response rates observed in multiple myeloma, the combination of bortezomib, cyclophosphamide, and dexamethasone (CyBorD, or CVD) has been explored in AL amyloidosis. Here, Mikhael et al report the retrospective analysis of 17 patients with AL amyloidosis, 10 of whom were treatmentnaive, who were treated with a median of 3 cycles (range, 2-6) of weekly administration of CyBorD before autologous stem cell transplantation (ASCT), as an alternative to highdose therapy for those deemed ineligible, and as salvage for relapsing patients.1 The reported 94% of hematologic responses is excellent and the 71% CR rate unprecedented in AL amyloidosis. The estimated median duration of CR was 22 months (range, 5-30 months). Organ response was observed in 50% of patients with renal involvement. Notably, 3 patients originally not eligible for ASCT became eligible after treatment with CyBorD. Treatment was well tolerated, with only 2 patients experiencing grade 1 or 2 peripheral neuropathy, possibly thanks to the weekly schedule of bortezomib. In the London National Amyloidosis Center study by Venner et al, 43 patients (20 treatment-naive) were treated with biweekly bortezomib and dexamethasone.2 Because 46% of patients had Mayo cardiac stage III disease, both bortezomib and dexamethasone dosages were attenuated. The hematologic response rate was 81.4% with a CR rate of 39.5%. As expected, neuropathy was more frequent in this study using biweekly bortezomib, occurring in 30% of patients and resulting in discontinuation of therapy in
14%. The remarkable nding of this study was that in the 20 patients with Mayo cardiac stage III disease, the estimated overall survival at 2 years was 94.4%, thus strikingly better than the median survival with melphalan and dexamethasone, which is 10 months from diagnosis.9 This is the rst hint that the profound and rapid hematologic response induced by bortezomib may modify the course of severe amyloid cardiomyopathy. Although the results of these 2 studies should be interpreted with caution given their retrospective design with possible selection bias, limited number, variable entry criteria, and, above all, short follow-up (median 21 months1 and 14 months,2 respectively), they clearly show that CyBorD/CVD has a profound and rapid effect on the amyloidogenic clone. Because there is strong evidence linking the quality of response to survival in AL amyloidosis,12 CyBorD/CVD has great potential to change the natural history of the disease. The availability of this powerful regimen opens new perspectives in the care of AL amyloidosis and raises several challenging questions that should be addressed through controlled, prospective trials. First, given the sparing of stem cells with this regimen, it is uncertain whether patients who achieve CR should proceed with ASCT, in light of the risk of the procedure in these fragile individuals. Second, the rapid responses produced by CyBorD/CVD open up the possibility of thwarting the high rate of early mortality in patients with advanced cardiac amyloidosis. A European phase 2 trial using attenuated doses is being developed for patients with Mayo cardiac stage III disease. Third, the overall impact of adding bortezomib to alkylating agents front-line on the natural history of the disease should also be assessed in prospective randomized trials. Because time is life in this frequently rapidly progressive disease, we need to answer these important questions quickly. AL amyloidosis is a rare disease and international collaboration is needed to accrue patients in clinical trials. Through an unprecedented international effort, a randomized trial comparing the present standard of care, melphalan-dexamethasone, versus bortezomib-melphalan-dexamethasone is now under way in Europe, Australia, and in the United States. This recently established network of referral centers dedicated to AL amyloidosis is a precious resource for conducting future trials. Furthermore, investigators
10 MAY 2012 I VOLUME 119, NUMBER 19
blood
From bloodjournal.hematologylibrary.org by guest on May 16, 2012. For personal use only.
working in the eld of AL amyloidosis have recently dened a framework for clinical research including dening clinically relevant end points, study populations, and other criteria for collaborative clinical research that should encourage rapid testing of therapies and expedite new drug development. This framework will be formally presented in May 2012 at the XIII International Symposium on Amyloidosis at the University Medical Center Groningen before being published. Conict-of-interest disclosure: The author declares no competing nancial interests.
REFERENCES
1. Mikhael JR, Schuster SR, Jimenez-Zepeda VH, et al. Cyclophosphamide-bortezomib-dexamethasone (CyBorD) produces rapid and complete hematologic response in patients with AL amyloidosis. Blood. 2012;119(19):43914394. 2. Venner CP, Lane T, Foard D, et al. Cyclophosphamide, bortezomib, and dexamethasone therapy in AL amyloidosis is associated with high clonal response rates and prolonged progression-free survival. Blood. 2012; 119(19):4387-4390. 3. Perfetti V, Palladini G, Casarini S, et al. The repertoire of lambda light chains causing predominant amyloid heart involvement and identication of a preferentially involved germline gene, IGLV1-44. Blood. 2012;119(1):144-150. 4. Shi J, Guan J, Jiang B, et al. Amyloidogenic light chains induce cardiomyocyte contractile dysfunction and apoptosis via a non-canonical p38alpha MAPK pathway. Proc Natl Acad Sci U S A. 2010;107(9):4188-4193.
5. Dispenzieri A, Gertz MA, Kyle RA, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22(18):3751-3757. 6. Palladini G, Barassi A, Klersy C, et al. The combination of high-sensitivity cardiac troponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide type B (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood. 2010;116(18):3426-3430. 7. Madan S, Kumar SK, Dispenzieri A, et al. High-dose melphalan and peripheral blood stem cell transplantation for light-chain amyloidosis with cardiac involvement. Blood. 2012;119(5):1117-1122. 8. Palladini G, Campana C, Klersy C, et al. Serum Nterminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation. 2003;107(19):2440-2445. 9. Lebovic D, Hoffman J, Levine BM, et al. Predictors of survival in patients with systemic light-chain amyloidosis and cardiac involvement initially ineligible for stem cell transplantation and treated with oral melphalan and dexamethasone. Br J Haematol. 2008;143(3):369-373. 10. Dietrich S, Schonland SO, Benner A, et al. Treatment with intravenous melphalan and dexamethasone is not able to overcome the poor prognosis of patients with newly diagnosed systemic light chain amyloidosis and severe cardiac involvement. Blood. 2010;116(4):522-528. 11. Gasparetto C, Sanchorawala V, Snyder RM, et al. Use of melphalan (M)/dexamethasone (D)/bortezomib in AL amyloidosis [abstract]. J Clin Oncol (Meeting Abstracts). 2010;28(15 suppl):8024. 12. Palladini G, Dispenzieri A, Gertz MAA, et al. Validation of the criteria of response to treatment In AL amyloidosis [lsqb[abstract]. Blood (ASH Annual Meeting Abstracts). 2010;116(21):1364.
IMMUNOBIOLOGY
Comment on Guimont-Desrochers et al, page 4349
IKDCs or B220 NK cells are pre-mNK cells ---------------------------------------------------------------------------------------------------------------Laurence Zitvogel and Franck Housseau
CANCER CENTER INSTITUT GUSTAVE ROUSSY; SIDNEY KIMMEL COMPREHENSIVE
The cell lineage origin of interferon-producing killer dendritic cells (IKDCs) has been challenged since 2006 when the unique capacity of these cells to accumulate in tumors and mediate remarkable antitumor effects was rst described.1-4 In this issue of Blood, Guimont-Desrochers et al redene B220 NK cells as a novel intermediate in NK-cell differentiation preceding the acquisition of CD27.5
KDCs were originally dened as CD11cintB220 CD49b MHC class II cells, endowed with an unexpected functional plasticity compared with classical NK cells. After in vivo exposure to imatinib mesylate and IL-2 or TLR9L, conditions of transpresentation of IL-15R /IL-15, IKDCs lost MHC class II molecules and harbored potent TRAIL-dependent lytic activity
leading to immunogenic cell death of their targets.6 In contrast, when licensed by tumor cells, IKDCs up-regulated MHC class II and CD86 molecules and acquired the capacity to cross-present exogenous antigens to naive CD8 and CD4 T cells in an MHC class I and class II dependent fashion, respectively.4,7 On TLR-9 activation in vitro, IKDCs down-regulated NKG2D/
DAP10/DAP12 molecules as well as their killing potential and started producing IL12p40.2 In vivo, MCMV infection triggered their migration to lymph nodes and their maturation into professional APCs able to cross-prime MCMV-specic CD8 T cells.2 After lung viral infection with inuenza virus, IKDCs were recruited to lungs and were endowed with antigenpresenting capacities.8 Most of these studies demonstrated the intrinsic APC functions of IKDCs using adoptive transfer of IKDCs in vivo (puried from resting spleens or cultured from bone marrow in the presence of growth factors) into hosts presenting genetic defects in the MHC class I4,7 or class II pathway7 or depleted from CD11chigh classical dendritic cells (DCs). In these reports, IKDCs drastically differed from B220 or MHC class II NK cells that failed to present antigens to naive T cells.2,7 However, several arguments indicated that IKDCs may truly belong to the NK-cell lineage (as opposed to a bona de DC origin), challenging the acronym IKDC. First, IKDCs were dependent on IL-15, IL-2R chain, and Id2 but independent of Flt3L for their in vivo differentiation.6,9,10 Secondly, gene- and NK receptor expression proling suggested that IKDCs resemble mature NK cells.5 Finally, many IKDC-related markers (CD11c, B220, and MHC class II) can be shared by mature NK cells, at least on in vitro activation.9 Therefore, a consensual view emerged as to reconsidering IKDCs as B220 NK cells endowed with unique tumoricidal and/or APC potential. In this issue of Blood, GuimontDesrochers et al report that B220 NK cells are a novel intermediate in NK-cell differentiation preceding the acquisition of CD27.5 After adoptive transfer of CD45.1 B220 NK cells (CD11cintCD122 ) into C57BL/6 or B6.Rag1 / CD45.2 hosts, B220 NK cells highly proliferated and progressively adopted a mature NK phenotype (B220 CD43 CD11bhigh). In contrast, B220 or CD27 NK cells failed to acquire the so-called B220 activation marker even on in vivo stimulation with Poly I:C or antiCD40 agonistic antibodies (see gure). The high incorporation rate of BrdU as well as a transcriptional prole highlighting genes associated with cell-cycle and microtubule organization, a large size, and high levels of
4345
blood 1 0 M A Y 2 0 1 2 I V O L U M E 1 1 9 , N U M B E R 1 9
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Immunoglobulin Light Chain Amyloidosis 2011 Update On Diagnosis - GertzДокумент7 страницImmunoglobulin Light Chain Amyloidosis 2011 Update On Diagnosis - GertzDaniel DrimerОценок пока нет
- Pomalidomide Activity Blood 2012 Dispenzieri Blood 2012-02-413161Документ32 страницыPomalidomide Activity Blood 2012 Dispenzieri Blood 2012-02-413161Daniel DrimerОценок пока нет
- Flc's and Cardiac Bio Markers - JCO 2011 38 5724 FullДокумент7 страницFlc's and Cardiac Bio Markers - JCO 2011 38 5724 FullDaniel DrimerОценок пока нет
- Changes in Serum FLC's To Measure Response - 21948 - FTPДокумент5 страницChanges in Serum FLC's To Measure Response - 21948 - FTPDaniel DrimerОценок пока нет
- How To Manage Primary Amyloidosis Ma GertzДокумент8 страницHow To Manage Primary Amyloidosis Ma GertzDaniel DrimerОценок пока нет
- Troponin Past and PresentДокумент20 страницTroponin Past and PresentDaniel DrimerОценок пока нет
- Doxycycline Reduces Fibril Formation in A Transgenic Mouse Model of AL AmyloidosisДокумент40 страницDoxycycline Reduces Fibril Formation in A Transgenic Mouse Model of AL AmyloidosisDaniel DrimerОценок пока нет
- Amyloidosis - Pathogenesis and New Therapeutic OptionsДокумент10 страницAmyloidosis - Pathogenesis and New Therapeutic OptionsDaniel DrimerОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Vocal Health PedagogyДокумент33 страницыVocal Health PedagogySushiQ0% (1)
- Critical Illness Rider LICДокумент1 страницаCritical Illness Rider LICSwadeep Kumar ShuklaОценок пока нет
- Next To Normal - Abridged ScriptДокумент13 страницNext To Normal - Abridged Scriptterrify007Оценок пока нет
- Jet Lag PDFДокумент8 страницJet Lag PDFIan FitzpatrickОценок пока нет
- CHPP 0913 ClarkДокумент7 страницCHPP 0913 ClarkFarzana AfrinОценок пока нет
- 2020 Drug PricesДокумент25 страниц2020 Drug PricesChris-Goldie LorezoОценок пока нет
- 2021 American College of Rheumatology Guideline For The Treatment of Rheumatoid ArthritisДокумент30 страниц2021 American College of Rheumatology Guideline For The Treatment of Rheumatoid Arthritisjose pablo quero reyesОценок пока нет
- Brochure Biology & Medicine 03 2022 - CompressedДокумент40 страницBrochure Biology & Medicine 03 2022 - CompressedMerida Bertrand Alex PodgaОценок пока нет
- Ecg Notes RetdemДокумент2 страницыEcg Notes RetdemJerica Mae VenoyaОценок пока нет
- 51 Diseases of Ruminants - Dr. SulaДокумент92 страницы51 Diseases of Ruminants - Dr. SulaCholid MawardiОценок пока нет
- New International Society of Hypertension (Ish) Guidelines 2020 - January 17TH 2021Документ35 страницNew International Society of Hypertension (Ish) Guidelines 2020 - January 17TH 2021Rhama Patria100% (1)
- Insurance Implications of DSM-5: Frequently Asked QuestionsДокумент4 страницыInsurance Implications of DSM-5: Frequently Asked QuestionszaneaxtenОценок пока нет
- Cases For Medical MalpracticeДокумент136 страницCases For Medical MalpracticeJose Van TanОценок пока нет
- Chandana Final Report 20-09-2020Документ67 страницChandana Final Report 20-09-2020Anup JiОценок пока нет
- Dettol Liquid Antiseptic Disinfected ProposalДокумент7 страницDettol Liquid Antiseptic Disinfected ProposalabdullahОценок пока нет
- PTIДокумент19 страницPTIDick Jerzy Salazar FranciaОценок пока нет
- Infectous DiseaseДокумент9 страницInfectous DiseasejamikawasОценок пока нет
- Intracranial NeoplasmaДокумент21 страницаIntracranial NeoplasmaLuvi PujiОценок пока нет
- Avena SativaДокумент46 страницAvena SativaJuliana VarelaОценок пока нет
- NCP Self HarmДокумент1 страницаNCP Self HarmJoshua ArevaloОценок пока нет
- Efficacy of Stuttering Therapies - PDF /KUNNAMPALLIL GEJOДокумент24 страницыEfficacy of Stuttering Therapies - PDF /KUNNAMPALLIL GEJOKUNNAMPALLIL GEJO JOHNОценок пока нет
- Mindray BS-120 / BS-200 / BS-300 / BS-380 / BS-400: MTD Diagnostics, SRLДокумент40 страницMindray BS-120 / BS-200 / BS-300 / BS-380 / BS-400: MTD Diagnostics, SRLCarlos SoutoОценок пока нет
- Shock Study Guide NursingДокумент4 страницыShock Study Guide NursingKory Christina100% (2)
- Menastil Complete Clinical Trials - Pain Relief That Works.Документ43 страницыMenastil Complete Clinical Trials - Pain Relief That Works.emoryholstОценок пока нет
- Azucar y Caries DentalДокумент8 страницAzucar y Caries Dentalgeraldine romaniОценок пока нет
- Resusitasi Jantung ParuДокумент31 страницаResusitasi Jantung ParuJohan100% (1)
- Soil Transmitted Helminth Infections: The Nature, Causes and Burden of The ConditionДокумент79 страницSoil Transmitted Helminth Infections: The Nature, Causes and Burden of The ConditionYokaiCO100% (1)
- Antacid Booklet Final Sept 2015Документ49 страницAntacid Booklet Final Sept 2015MarianelaMolocheОценок пока нет
- Antifertility DrugsДокумент12 страницAntifertility DrugsforplancessОценок пока нет
- Cramp Pages 1Документ10 страницCramp Pages 1masi10Оценок пока нет