Академический Документы
Профессиональный Документы
Культура Документы
Cerebrovascular Accident
Загружено:
plethoraldork100%(10)100% нашли этот документ полезным (10 голосов)
15K просмотров8 страницCerebrovascular Accident, Stroke
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
DOC, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документCerebrovascular Accident, Stroke
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
100%(10)100% нашли этот документ полезным (10 голосов)
15K просмотров8 страницCerebrovascular Accident
Загружено:
plethoraldorkCerebrovascular Accident, Stroke
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 8
Clients with Cerebrovascular Disease
Cerebrovascular Accident (CVA)
Commonly known as stroke or brain attack
A condition in which neurologic deficits result from decreased blood
flow to localized area of the brain
Neurologic deficits determined by the area of brain involved, size of
affected area, length of time blood flow is decreased or stopped
Major loss of blood supply to brain can cause severe disability or death; if
short or small area involved client may not be aware
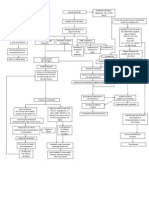
Pathophysiology
Characterized by gradual, rapid onset of neurologic deficits due to
compromised cerebral blood flow
Blood flow and oxygenation of cerebral neurons decreased or
interrupted; changes occur in 4 – 5 minutes
Cells swell and cerebral blood vessels swell decreasing blood flow;
vasospasm and increased blood viscosity further impede blood flow
Penumbra is a central core of dead or dying cells surrounded by
band of minimally perfused cells
Cells of the penumbra receives marginal blood flow and their
metabolic activities are impaired
These cells may survive if adequate circulation is re-
established
Neurologic deficits occur on opposite side where stroke occurred in
brain: contralateral deficit
Causes
Ischemia
Occurs when the blood supply to a part of the brain is
interrupted or totally occluded
Commonly due to thrombosis or embolism
• Thrombotic (large vessel) stroke
o The most common cause of ischemic stroke
o Atherosclerosis is the primary cause
o Fatty materials deposit on large vessel walls
(especially at arterial bifurcations) and
eventually these plaques causes stenosis of the
artery
o Blood swirls around the irregular surface of the
plaques causing platelets to adhere and the
vessel becomes obstructed
o These causes infarcts usually affecting the
cortex
o Most common type of stroke in people with
diabetes
• Lacunar (small vessel) stroke
o Endothelium of smaller vessel is primarily
affected due to hypertension
o Leading to arteriosclerosis and stenosis
o Infarcts are usually located in the deeper,
noncortical parts of the brain or in the brainstem
• Embolic stroke
o Occlusion of a cerebral artery by an embolus or
blood clot
o Embolus forms outside the brain, detaches and
travels through the cerebral circulation where it
lodges and causes an obstruction
o Chronic atrial fibrillation is associated with a
high incidence
o Other sources of emboli include tumor, fat,
bacteria and air
o Usually has a sudden onset with immediate
maximum deficit
Hemorrhage
Results from rupture of a cerebral vessel causing bleeding
into the brain tissues
Bleeding results with edema, compression of the brain
contents or spasm of the adjacent blood vessels
Often secondary to hypertension and most common after age
50
Other factors includes ruptured intracranial aneurysms,
trauma, erosion of blood vessels by tumors, arteriovenous
malformations, anticoagulant therapy, blood disorders
Usually produce extensive residual functional loss and
slowest recovery
Risk factors
Hypertension
Diabetes mellitus
Atherosclerosis
Substance abuse including alcohol, nicotine, heroin, amphetamines,
cocaine
Obesity, sedentary life-style, hyperlipidemia, atrial fibrillation, cardiac
disease, cigarette smoking, previous transient ischemic attacks
Women: oral contraceptive use, pregnancy, menopause
Clinical manifestations
Stroke manifestations can be correlated with the cause and with the
area of the brain in which perfusion is affected
Manifestations of thrombotic stroke develop over minutes to
hours to days (slow onset is related to increasing size of the
thrombus)
Embolic strokes occur suddenly and without warning
Hemorrhagic stroke occurs rapidly with manifestations
developing over minutes to hours
General findings unrelated to specific vessel sites includes
headache, vomiting, seizures and changes in mental status
Early warnings of impending ischemic stroke includes
Transient hemiparesis
Loss of speech
Hemisensory loss
Specific deficits after stroke
Motor deficits
Affects connections involving motor areas of cerebral cortex,
basal ganglia, cerebellum, peripheral nerves
Produce effects in contralateral side ranging from mild
weakness to severe limitation
Hemiplegia (paralysis of half of body)
Hemiparesis (weakness of half of body)
Apraxia (inability to perform a previously learned skilled task
in the absence of paralysis)
• Able to conceptualize the content of the message to
send to muscles but motor patterns necessary to
convey the impulse cannot be reconstructed
• Instructions do not reach the limb from the brain and
desired action cannot happen
• E.g. dressing and bathing
Flaccidity (absence of muscle tone or hypotonia)
Spasticity (increased muscle tone usually with some degree
of weakness)
Affected arm and leg are initially flaccid and become spastic
in 6 – 8 weeks, causes characteristic body positioning
• When voluntary muscle control is lost, strong flexor
muscles overbalance the extensors
• Imbalance can cause serious contractures
o Adduction of shoulder
o Pronation of forearm
o Flexion of fingers
o Extension of hip and knee
o Foot drop, outward rotation of leg, with
dependent edema
Muscles of the thorax and abdomen are usually not affected
because they are innervated from both cerebral hemispheres
Communication disorders
Usually result of stroke affecting dominant hemisphere (left
hemisphere dominant in 95% right-handed persons; 70% left-
handed persons)
Aphasia (deficit in the ability to communicate or inability to
use or understand language)
• Involve any or all aspects of communication including
speaking, reading, writing and understanding spoken
language
• Wernicke’s aphasia
o Receptive, sensory or fluent aphasia
o Sensory speech problem in which one cannot
understand spoken or written word
o Speech may be fluent but with inappropriate
content
o Result of infarction in the temporal lobe
• Broca’s aphasia
o Expressive, motor or nonfluent aphasia
o Motor speech problem in which client
understands what is said but can only respond
verbally in short phases or inability to combine
sounds into appropriate words and syllables
o Ability to write, make signs or speak is lost
o Result of infarction in the frontal lobe
• Mixed or global aphasia
o Affects both speech comprehension and
speech production
o Can be so extensive that neither expressive nor
receptive language abilities are retained
Dysarthria (imperfect articulation that causes difficulty in
speaking)
• Client understands language but has difficulty
pronouncing words
• No disturbance is evident in grammar and sentence
construction unlike in aphasia
• Caused by cranial nerve dysfunction resulting with
weakness or paralysis of the muscles of the lips,
tongue and larynx
• Often manifested with difficulty chewing and
swallowing (dysphagia) because of poor muscle
control
Sensory-perceptual deficits
Visual changes
• Parietal and temporal lobe strokes may cause visual
acuity impairment
• Depth perception and visual perception of horizontal
and vertical plane may also be impaired
• Diplopia (double vision) and ptosis (drooping of
eyelids) are also common
Homonymous hemianopia
• Visual loss in the same half of the visual field of each
eye
• Client may see clearly on one side of the midline but
see nothing on the other side
Agnosia (inability to recognize one or more subjects that
were previously familiar through the senses)
• May be visual, tactile or auditory
• Client with visual agnosia sees objects but is unable to
recognize or attach meaning to them
• Disorientation is common due to inability to recognize
environmental cues, familiar faces or symbols
Hemisensory loss (loss of sensation on one side of the body)
• Paresthesia is common
• Proprioception (ability to perceive the relationship of
body parts to the external environment) is impaired
Unilateral neglect (inability to respond to stimulus on the
contralateral side of the cerebral infarct)
• Attention disorder in which client ignores affected part
of body
• Client cannot integrate or use perceptions from
affected side of body or from environment on affected
side
Elimination disorders
Partial loss of sensation that triggers bladder and bowel
elimination
• Urinary frequency, urgency and incontinence are
common
Bowel elimination changes result from LOC changes,
immobility, dehydration
May also relate to cognitive deficits
Cognitive and behavioral changes
Ranges from mild confusion to coma
May result from actual tissue damage from stroke, cerebral
edema, or increased intracranial pressure
May exhibit
• Emotional lability: laughing or crying inappropriately
• Loss of self-control (i.e. swearing, refusing to
cooperate)
• Decreased tolerance for stress (anger, depression)
• Intellectual changes: memory loss, decreased
attention span, poor judgment, inability to think
abstractly
Diagnostic tests
CT scan without contrast: determine hemorrhage, tumors,
aneurysms, ischemia, edema, tissue necrosis, shifting in intracranial
contents
Arteriography of cerebral vessels: reveals abnormal vessel
structures, vasospasm, stenosis of arteries
MRI: detect shifting of brain tissues resulting from hemorrhage or
edema
Positron emission tomography (PET), single-photon emission
computed tomography (SPECT): examine cerebral blood flow
distribution and metabolic activity of brain
Management and Nursing care
Medical management is directed at early diagnosis and early
identification
Maintain cerebral oxygenation and cerebral blood flow
Maintain patent airway and turn patient to side if unconscious
Elevate head and neck should not be flexed
Hypertension may be reduced with vasodilators and calcium
channel blockers
Thrombolytic agents are given to dissolve the clot
• Intracerebral hemorrhage should be ruled out first
• Must be given within 3 hours of onset of
manifestations
• E.g. streptokinase, urokinase and tissue plasminogen
activator (alteplase)
Antiplatelet and anticoagulants are given to prevent clot
formation
• Heparin and warfarin
• Aspirin, clopidogrel (Plavix), ticlodipine (Ticlid) or
dipyridamole (Persantine)
Corticosteroids to treat cerebral edema, diuretics to reduce
increased intracranial pressure and anticonvulsants to
prevent seizures
Hyperthermia is treated immediately
• Temperature elevations lead to increased cerebral
metabolic needs which in turn cause cerebral edema
which can lead to further ischemia
• Antipyretics are used
• Causing the client to shiver should be avoided
Aspiration precaution is done
• Oral food and fluids are generally withheld for 24-48
hours
• Tube feeding is done
Prevent valsalva maneuver
• Maneuver increases ICP
• Straining stool, excessive coughing, vomiting, lifting
and use of the arms to change position should be
avoided
• Mild laxatives and stool softeners are often prescribed
Compensate for perceptual difficulties
For clients with visual deficits
• Approach the client from the unaffected side
• Place articles on the unaffected side
• Teach client to turn the head from side to side to see
entire visual field
• Eye patch over one eye in clients with diplopia is
helpful
Assist and support client
• Prevent injury and falls
• Promote self-care and prevent skin breakdown
Prevent complications
Physical therapy to prevent contractures and to improve
muscle strength and coordination
• Encourage bed exercise
• Facilitate ROM and isometric exercises
o Do not force extremities beyond the point of
initiating pain and spasm
o Always support the joint and move the extremity
smoothly
• Allow client to work on balance and proprioception
skills
Occupational therapy
• Help client relearn ADLs and to use assistive devices
that promote independence
• Teach client how to use the wheelchair and promote
walking with assitance
Speech therapy for clients with impaired verbal
communication
• Most aphasic clients regain some speech through
spontaneous recovery or speech therapy
• Speech therapy should be started early
• For aphasic clients
o Speak at a slower rate
o Give client time to respond
o Do not shout and always put client at ease
o Repeat simple directions until they are
understood
o Give client practice in repeating words after you
o The family should not do all the talking for the
client
Provide emotional support and health education to the client and
family
Вам также может понравиться
- Cerebrovascular AccidentДокумент31 страницаCerebrovascular AccidentKoRnflakes83% (6)
- Congestive Heart FailureДокумент4 страницыCongestive Heart FailureAnnie Grace PoliranОценок пока нет
- Intracranial HemorrhageДокумент41 страницаIntracranial Hemorrhagedoctormussieaberra100% (1)
- Group 4 - Hemorrhagic StrokeДокумент60 страницGroup 4 - Hemorrhagic StrokeKitz T AnasarioОценок пока нет
- Hemorrhagic Cerebro Vascular DiseaseДокумент37 страницHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- Pathophysiology CAP and HTNДокумент5 страницPathophysiology CAP and HTNLeonaPunzalanОценок пока нет
- Hemorrhagic StrokeДокумент12 страницHemorrhagic StrokeManggara Surya DharmaОценок пока нет
- Hemorrhagic StrokeДокумент30 страницHemorrhagic StrokeAstrina SupandyОценок пока нет
- Hemothorax HandoutsДокумент2 страницыHemothorax HandoutsJunathan L. DelgadoОценок пока нет
- Pa Tho Physiology of Hemorrhagic StrokeДокумент2 страницыPa Tho Physiology of Hemorrhagic StrokeMerlash MerlaОценок пока нет
- Cva-Hypertension-Case-Analysis-Group-I FinalДокумент59 страницCva-Hypertension-Case-Analysis-Group-I FinalVhince Norben PiscoОценок пока нет
- Obstructive Uropathy Secondary To Benign Prostatic HyperplasiaДокумент74 страницыObstructive Uropathy Secondary To Benign Prostatic HyperplasiaGregory Litang100% (1)
- Pathophysiology of DMДокумент4 страницыPathophysiology of DMNicole Louise N. VillanuevaОценок пока нет
- Diarrhea Care PlanДокумент2 страницыDiarrhea Care Planzepoli_zepoly6232100% (1)
- Path o PhysiologyДокумент9 страницPath o PhysiologyKyle Ü D. CunanersОценок пока нет
- Myocardial InfarctionДокумент15 страницMyocardial InfarctionameerОценок пока нет
- Pathophysiology of NephrosclerosisДокумент2 страницыPathophysiology of NephrosclerosisJessica Damasen Caballero0% (1)
- Angina Pectoris PathophysiologyДокумент2 страницыAngina Pectoris PathophysiologyALIANA KIMBERLY MALQUESTOОценок пока нет
- Cerebral Aneurysms: Aneurysms Posterior Circulation Basilar Artery Vertebral Arteries Posterior Communicating ArteryДокумент10 страницCerebral Aneurysms: Aneurysms Posterior Circulation Basilar Artery Vertebral Arteries Posterior Communicating ArteryRani SujithОценок пока нет
- NCP Impaired Physical MobilityДокумент9 страницNCP Impaired Physical MobilityChristian Apelo SerquillosОценок пока нет
- Case-Study Hemorrhagic-Stroke FinalДокумент102 страницыCase-Study Hemorrhagic-Stroke FinalAngela QuiñonesОценок пока нет
- Stevens-Johnson Syndrome CASEДокумент38 страницStevens-Johnson Syndrome CASEChristy Rose AgrisОценок пока нет
- Fractures, PathophysiologyДокумент1 страницаFractures, Pathophysiology4kscribdОценок пока нет
- Metabolism Case StudiesДокумент3 страницыMetabolism Case StudiesEpoy Bantawig0% (1)
- HCVD KoДокумент10 страницHCVD KoMarianne BaquilalaОценок пока нет
- Pathophysiology of Angina PectorisДокумент1 страницаPathophysiology of Angina PectorisCheryl100% (1)
- CvaДокумент42 страницыCvad_94Оценок пока нет
- Cardiogenic ShockДокумент21 страницаCardiogenic ShockIslamOteshОценок пока нет
- 418-M3-Cu14 Nursing Care of Clients in Emergency Situations 1 - AbcsДокумент9 страниц418-M3-Cu14 Nursing Care of Clients in Emergency Situations 1 - AbcsDanica FrancoОценок пока нет
- Intracerebral HemorrageДокумент13 страницIntracerebral HemorrageChristian JuarezОценок пока нет
- NCP CvaДокумент7 страницNCP CvaEmerson SilverioОценок пока нет
- Pathophysiology of Acute PancreatitisДокумент1 страницаPathophysiology of Acute PancreatitisHarvin FrancoОценок пока нет
- Pathophysiology Hemorrhagic StrokeДокумент1 страницаPathophysiology Hemorrhagic StrokeJeffrey Dela CruzОценок пока нет
- Bsn3-2c UC-BCF CVA Case StudyДокумент49 страницBsn3-2c UC-BCF CVA Case StudyclarheenaОценок пока нет
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: STO: Within 4 Hour of DX: DX: Sto: Goal MetДокумент5 страницAssessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: STO: Within 4 Hour of DX: DX: Sto: Goal MetRussel SantosОценок пока нет
- Name of Drug Mechanism: MemantineДокумент4 страницыName of Drug Mechanism: MemantineCarlmeister Ambray JudillaОценок пока нет
- Tetanus PathoДокумент3 страницыTetanus PathoElisha Gine AndalesОценок пока нет
- Schistosomiasis (From Anatomy To Pathophysiology)Документ10 страницSchistosomiasis (From Anatomy To Pathophysiology)Tiger Knee100% (1)
- Final patho-HCVDДокумент2 страницыFinal patho-HCVDAlvin RamirezОценок пока нет
- NCP CvaДокумент4 страницыNCP CvaMariquita BuenafeОценок пока нет
- DB13 - Pathophysiology of AtherosclerosisДокумент2 страницыDB13 - Pathophysiology of Atherosclerosisi_vhie03Оценок пока нет
- Pathophysiology of StrokeДокумент3 страницыPathophysiology of StrokeAqeel Al-Mahdaly0% (1)
- Casestudy Pott's DiseaseДокумент36 страницCasestudy Pott's DiseaseyasiraОценок пока нет
- CHOLElithiasisДокумент93 страницыCHOLElithiasisfranciscomaricris13Оценок пока нет
- Pathophysiology and Schematic Diagram of Typhoid FeverДокумент3 страницыPathophysiology and Schematic Diagram of Typhoid FeverCyrus De AsisОценок пока нет
- Patho of MIДокумент2 страницыPatho of MIInchan Montesines0% (1)
- CABGДокумент3 страницыCABGblessed23Оценок пока нет
- Spinal Cord InjuryДокумент9 страницSpinal Cord InjurytasneemОценок пока нет
- Pathophysiology of StrokeДокумент11 страницPathophysiology of StrokeAgronaSlaughterОценок пока нет
- PathophysiologyДокумент1 страницаPathophysiologyHazel PalomaresОценок пока нет
- Bladder CancerДокумент1 страницаBladder CancerCarmina AguilarОценок пока нет
- Nursing Care Plan For Pulmonary Edema PDFДокумент2 страницыNursing Care Plan For Pulmonary Edema PDFAsmaa100% (1)
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaДокумент5 страницDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいОценок пока нет
- Case StudyДокумент6 страницCase StudyApoorv Jain100% (1)
- Jennelyn LumbreДокумент5 страницJennelyn LumbrejoyaksОценок пока нет
- Cerebrovascular Accident (CVA) : The BrainДокумент6 страницCerebrovascular Accident (CVA) : The BrainBrenn Marie RamosОценок пока нет
- Cerebrovascular Accident (Cva)Документ19 страницCerebrovascular Accident (Cva)Darl DacdacОценок пока нет
- Focus On StrokeДокумент92 страницыFocus On StrokeDIAH RETNO WULAN100% (2)
- NonmodifiableДокумент4 страницыNonmodifiableAmoroso, Marian Corneth D.Оценок пока нет
- Neurologic EmergenciesДокумент13 страницNeurologic EmergenciesRENEROSE TORRESОценок пока нет
- Summit College NCLEX LECTURE NOTES VIDEO 1-11Документ98 страницSummit College NCLEX LECTURE NOTES VIDEO 1-11plethoraldork90% (20)
- Behaviour Change Behaviour Change OverviewДокумент12 страницBehaviour Change Behaviour Change OverviewplethoraldorkОценок пока нет
- 9 NCLEX-style Questions & Rationales From NCBSN 2019 NCLEX-RN Test PlanДокумент9 страниц9 NCLEX-style Questions & Rationales From NCBSN 2019 NCLEX-RN Test PlanNikkaLim100% (2)
- PLANNING and EVALUATION 220117Документ13 страницPLANNING and EVALUATION 220117plethoraldorkОценок пока нет
- Normal Lab ValuesДокумент3 страницыNormal Lab ValuesHОценок пока нет
- Final OSCE Script 220117Документ18 страницFinal OSCE Script 220117plethoraldorkОценок пока нет
- Acute Renal FailureДокумент48 страницAcute Renal FailureNalin AbeysingheОценок пока нет
- Normal Lab ValuesДокумент3 страницыNormal Lab ValuesHОценок пока нет
- SATAДокумент4 страницыSATAplethoraldorkОценок пока нет
- Management of The EVDДокумент7 страницManagement of The EVDplethoraldork100% (1)
- Nursing ProcessДокумент62 страницыNursing ProcessplethoraldorkОценок пока нет
- New IELTS Writing Answer SheetДокумент4 страницыNew IELTS Writing Answer Sheetraaj2240% (5)
- Med ListДокумент4 страницыMed ListCrystal MalicatОценок пока нет
- TB Guidelines PDFДокумент185 страницTB Guidelines PDFplethoraldorkОценок пока нет
- Guidelines For HemodyalysiДокумент132 страницыGuidelines For HemodyalysipranshamОценок пока нет
- Confession GuideДокумент1 страницаConfession GuideSimon Chee100% (1)
- Confession GuideДокумент1 страницаConfession GuideSimon Chee100% (1)
- Av FistulaДокумент1 страницаAv FistulaplethoraldorkОценок пока нет
- CBT Study GuideДокумент10 страницCBT Study Guideplethoraldork100% (5)
- Acne Clinical Recommendations PamphletДокумент6 страницAcne Clinical Recommendations PamphletplethoraldorkОценок пока нет
- Hemodialysis PDFДокумент244 страницыHemodialysis PDFMorrison Njage100% (1)
- Vascular Access HemodialysisДокумент19 страницVascular Access Hemodialysisplethoraldork100% (1)
- New IELTS Writing Answer SheetДокумент4 страницыNew IELTS Writing Answer Sheetraaj2240% (5)
- Management of The EVDДокумент7 страницManagement of The EVDplethoraldork100% (1)
- Accreditation Requirements HemodialysisДокумент12 страницAccreditation Requirements HemodialysisplethoraldorkОценок пока нет
- New IELTS Writing Answer SheetДокумент4 страницыNew IELTS Writing Answer Sheetraaj2240% (5)
- New IELTS Writing Answer SheetДокумент4 страницыNew IELTS Writing Answer Sheetraaj2240% (5)
- Stroke Guidelines: Cva Critical Pathway Department of NeurologyДокумент5 страницStroke Guidelines: Cva Critical Pathway Department of NeurologyplethoraldorkОценок пока нет
- Hemodialysis Accreditation RequirementsДокумент13 страницHemodialysis Accreditation RequirementsplethoraldorkОценок пока нет
- Ao2012-0001 New Rules & Regulations Governing The Licensing & Regulation of Dialysis Facilities in The Phils PDFДокумент41 страницаAo2012-0001 New Rules & Regulations Governing The Licensing & Regulation of Dialysis Facilities in The Phils PDFplethoraldorkОценок пока нет
- 1.15 ANATOMY - The LarynxДокумент2 страницы1.15 ANATOMY - The LarynxPaolo NaguitОценок пока нет
- Heart FailureДокумент21 страницаHeart FailureJazzy Kathlene Dumable0% (1)
- Treatment of Portal HypertensionДокумент10 страницTreatment of Portal HypertensionLourianne NcОценок пока нет
- Unit 13 Endocrine GlandДокумент73 страницыUnit 13 Endocrine GlandChandan ShahОценок пока нет
- Episcleritis - EyeWikiДокумент3 страницыEpiscleritis - EyeWikiJorge Leonardo BedoyaОценок пока нет
- Cor PulmonaleДокумент22 страницыCor Pulmonalenatijahtun istiqomahОценок пока нет
- DR Lila - Patient Preparation For Emergencies Surgeries - New 11012017Документ37 страницDR Lila - Patient Preparation For Emergencies Surgeries - New 11012017bloadyroar100% (1)
- Surgical TermsДокумент10 страницSurgical TermsCLaui SagibalОценок пока нет
- Emergency Medicine EbookДокумент642 страницыEmergency Medicine Ebookgulsoomro100% (1)
- Hypertension True/false QuestionsДокумент10 страницHypertension True/false QuestionsAfiya Mohammed100% (2)
- Early Detection of Hepato-Biliary DisorderДокумент68 страницEarly Detection of Hepato-Biliary DisorderIbsa GetachoОценок пока нет
- Status EpilepticusДокумент17 страницStatus EpilepticusXavier AbrilОценок пока нет
- Mousab Kibreet Notes of Internal Medicine 2ed EditionДокумент253 страницыMousab Kibreet Notes of Internal Medicine 2ed EditionAbdulltif AliОценок пока нет
- Anesthetic Consideration For Down Syndrom: Pediatric S Assignme NT Group 7Документ23 страницыAnesthetic Consideration For Down Syndrom: Pediatric S Assignme NT Group 7mihret tedlaОценок пока нет
- Anti ArrhythmicsДокумент46 страницAnti Arrhythmicsnk999999Оценок пока нет
- Pathognomonic SignsДокумент12 страницPathognomonic Signsclarice_jimenezОценок пока нет
- Heart FailureДокумент1 страницаHeart FailureCecil-An DalanonОценок пока нет
- Winninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualДокумент66 страницWinninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualTiglao, Camile Ann C.0% (1)
- Quarter: 4 / Semester: 2 / WEEK: 4: Online Resource/sДокумент17 страницQuarter: 4 / Semester: 2 / WEEK: 4: Online Resource/sTristan Paul PagalananОценок пока нет
- Soal Sepsis 0807 Blok7Документ2 страницыSoal Sepsis 0807 Blok7Suryadi VOoОценок пока нет
- LidocaineДокумент2 страницыLidocaineLeigh Marie LastimosaОценок пока нет
- Byzantine Surgery and Unnecessary Modern SurgeryДокумент14 страницByzantine Surgery and Unnecessary Modern SurgerynicofreshwaterОценок пока нет
- Heart Rhythm Interpretation ECG Strips 2019Документ21 страницаHeart Rhythm Interpretation ECG Strips 2019daniel situngkirОценок пока нет
- 32 - Thelma Vda. de Canilang V CAДокумент5 страниц32 - Thelma Vda. de Canilang V CAPatrice ThiamОценок пока нет
- Balloon-Assisted Cannulation For Difficult Anterior Cerebral Artery AccessДокумент5 страницBalloon-Assisted Cannulation For Difficult Anterior Cerebral Artery AccessaldyОценок пока нет
- Health Effects of Cigarette Smoking Vanessa BenningДокумент4 страницыHealth Effects of Cigarette Smoking Vanessa Benningapi-489132887Оценок пока нет
- Asthma - FactsДокумент24 страницыAsthma - Factsvsvp100Оценок пока нет
- Rheumatic Fever Is AnДокумент7 страницRheumatic Fever Is AnHamza SaeedОценок пока нет
- HyperkalemiaДокумент9 страницHyperkalemiaFabdul RaufОценок пока нет
- Managing For Client With Diabetic MellitusДокумент23 страницыManaging For Client With Diabetic MellitusNur HikmaОценок пока нет