Академический Документы
Профессиональный Документы
Культура Документы
1011 SUR Annual EARS Net 2009
Загружено:
mais_bАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
1011 SUR Annual EARS Net 2009
Загружено:
mais_bАвторское право:
Доступные форматы
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe
2009
www.ecdc.europa.eu
Antimicrobial resistance surveillance in Europe
Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net)
2009
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Suggested citation for full report: European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2009. Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Stockholm: ECDC; 2010. Cover picture istockphoto ISBN 978-92-9193-227-6 doi 10.2900/35994 European Centre for Disease Prevention and Control, 2010. Reproduction is authorised, provided the source is acknowledged.
ii
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Contents
Abbreviations and acronyms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .vii Countries participating in EARS-Net 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .ix National institutions/organisations participating in EARS-Net . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . xi Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .1 1 Introduction. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3 2 Escherichia coli and Staphylococcus aureus: bad news and good news. Analysis of data from laboratories reporting continuously from 2002 to 2009
5
........................... .
2.1 Methods of analysis. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8 2.2 Limitations of the analysis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8 2.3 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8
3 External Quality Assessment Exercise (EQA) 2009. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9
3.1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9 3.2. Results . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9 3.3 Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
4 EARS-Net laboratory/hospital denominator data 2009
................................................................. .
15
4.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 4.2 Methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 4.3 Participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 4.4 Population coverage . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 4.5 Hospital denominator information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 4.6 Hospital characteristics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 4.7 Laboratory denominator information. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 4.8 Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
5 Antimicrobial resistance in Europe . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .19
5.1 Streptococcus pneumoniae . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19 5.2 Staphylococcus aureus. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 5.3 Enterococci . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 31 5.4 Escherichia coli . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 36 5.5 Klebsiella pneumoniae . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47 5.6 Pseudomonas aeruginosa . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57 5.7 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70
Annex 1: Technical notes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 71 Annex 2: Country summary sheets . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 75
iii
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
List of tables
2.1: Average numbers of Escherichia coli and Staphylococcus aureus isolates per country reported yearly from 2002 to 2009 by laboratories participating continuously in EARSS/EARS-Net during this time interval . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6 3.1: Escherichia coli (9448): Minimum inhibitory concentration (MIC) and intended results reported by reference laboratories and the overall concordance of the participating laboratories . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 3.2: Klebsiella pneumoniae (9449): Minimal inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 3.3: Streptococcus pneumoniae (9450): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 3.4: Pseudomonas aeruginosa (9451): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13 3.5: Pseudomonas aeruginosa (9452): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13 3.6: Staphylococcus aureus (9453): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
17 17 4.3: Laboratory denominator information for 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
4.1: Hospital denominator data for 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2: Hospital characteristics for 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.1: Number of invasive S. pneumoniae isolates and proportion of penicillin-non-susceptible (PNSP), penicillin-resistant (PRSP), macrolide non-susceptible (MNSP), single penicillin (PEN), single macrolides (MACR) and dual non-susceptible (DUAL) isolates, including 95% confidence intervals (95% CI), reported per country in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26 5.2: Distribution of single penicillin, single macrolides and dual penicillin-macrolides non-susceptibility, among the most common serogroups reported per country in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26 5.3: Number of invasive S. aureus isolates and proportion resistant to meticillin (MRSA) and rifampin (RIF), including 95% confidence intervals (95% CI), reported per country in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29 5.4: Number of invasive E. faecalis and E. faecium isolates and proportion of high-level aminoglycoside-resistant E. faecalis and vancomycin-resistant E. faecium (%R), including 95% confidence intervals (95% CI), reported per country in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34 5.5: Number of invasive E. coli isolates and proportion aminopenicillins, third-generation cephalosporins, fluoroquinolones, aminoglycosides and multiresistance (%R), including 95% confidence intervals (95% CI), reported per country in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 5.6: Number of invasive E. coli isolates resistant to third-generation cephalosporins (CREC) and proportion of ESBL positive among these isolates, as ascertained by the participating laboratories in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 5.7: Overall resistance and resistance combinations among invasive Escherichia coli isolates tested against aminopenicillins, fluoroquinolones, third-generation cephalosporins and aminoglycosides (n= 42 898) in Europe, 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40 5.8: Number of invasive K. pneumoniae isolates and proportion of fluoroquinolones, third-generation cephalosporins, aminoglycosides and multiresistance (%R), including 95% confidence intervals (95% CI), reported per country in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55 5.9: Number of invasive K. pneumoniae isolates resistant to third-generation cephalosporins (CRKP) and proportion of ESBL positive among these isolates, as ascertained by the participating laboratories in 2009. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55 5.10: Overall resistance and resistance combinations among invasive Klebsiella pneumoniae isolates tested against fluoroquinolones, third-generation cephalosporins and aminoglycosides (n= 10 952) in Europe, 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56 5.11: Number of invasive P. aeruginosa isolates and proportion of piperacillintazobactam, fluoroquinolones, ceftazidime, aminoglycosides, carbapenems and multiresistance (%R), including 95% confidence intervals (95% CI), reported per country in 2009. . . . . . . . . .68 5.12: Overall resistance and resistance combinations among invasive Pseudomonas aeruginosa isolates tested against at least three antibiotic classes among piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems (n= 8 376) in Europe, 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 69
List of figures
2.1: Yearly number of bloodstream infections caused by Escherichia coli and Staphylococcus aureus. EARSS/EARS-Net 20022009 (22 countries/198 laboratories) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7 2.2: Proportion of third-generation cephalosporin-resistant Escherichia coli (CREC) and meticillin-resistant Staphylococcus aureus (MRSA). EARSS/EARS-Net 20022009 (22 countries/198 laboratories) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7 2.3: Combined resistance (R) of Escherichia coli to aminopenicillins, third-generation cephalosporins, fluoroquinolones and aminoglycosides. EARSS/EARS-Net 20022009 (22 countries/198 laboratories) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7 3.1: Proportion of participating laboratories returning reports per country, 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 3.2: Adherence to guidelines: number of laboratories per country . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 4.1: Number of laboratories and hospitals reporting AMR and/or denominator data in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
iv
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
4.2: Proportion of small, medium and large hospitals per country, based on the number of beds, for all hospital reporting both antimicrobial resistance data and denominator data in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 5.1: Streptococcus pneumoniae: proportion of invasive isolates non-susceptible to penicillin (PNSP) in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 5.2: Streptococcus pneumoniae: proportion of invasive isolates non-susceptible to macrolides in 2009
..............................................
22
5.3: Streptococcus pneumoniae: proportion of invasive isolates with dual non-susceptibility to penicillin and macrolides in 2009 . . . . . . . . . . . . . . . . 22
23 5.5: Streptococcus pneumoniae: trend of macrolides non-susceptibility by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24 5.6: Streptococcus pneumoniae: trend of dual non-susceptibility (penicillin and macrolides) by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25 5.7: Distribution of serogroups and the resistance profile of S. pneumoniae isolates per serogroup in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27 5.8: Staphylococcus aureus: proportion of invasive isolates resistant to meticillin (MRSA) in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29 5.9: Staphylococcus aureus: trend of meticillin-resistance (MRSA) by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30 5.10: Enterococcus faecalis: proportion of invasive isolates with high-level resistance to aminoglycosides in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32 5.11: Enterococcus faecalis: trends of high-level aminoglycoside resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33 5.12: Enterococcus faecium: proportion of invasive isolates resistant to vancomycin in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34 5.13: Enterococcus faecium: trends of vancomycin resistance by country 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35 5.14: Escherichia coli: proportion of third-generation cephalosporin resistance in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40 5.15: Escherichia coli: proportion of invasive isolates with resistance to fluoroquinolones in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41 5.16: Escherichia coli: proportion of invasive isolates with resistance to aminoglycosides in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41 5.17: Escherichia coli: trends of aminopenicillin resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42 5.18: Escherichia coli: trends of third-generation cephalosporin resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43 5.19: Escherichia coli: trends of fluoroquinolone resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44 5.20: Escherichia coli: trends of aminoglycoside resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45
5.4: Streptococcus pneumoniae: trend of penicillin non-susceptibility by country, 20062009
.........................................................
5.21: Escherichia coli: trends of combined resistance (resistant to fluoroquinolones, third-generation cephalosporins and aminoglycosides) by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46
49 49 5.24: Klebsiella pneumoniae: proportion of invasive isolates resistant to aminoglycosides in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50 5.25: Klebsiella pneumoniae: proportion of invasive isolates resistant to carbapenems in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50 5.26: Klebsiella pneumoniae: trend of third-generation cephalosporins resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51 5.27: Klebsiella pneumoniae: trend of fluoroquinolones resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52 5.28: Klebsiella pneumoniae: trend of aminoglycosides resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53
5.22: Klebsiella pneumoniae: proportion of invasive isolates resistant to third-generation cephalosporins in 2009 5.23: Klebsiella pneumoniae: proportion of invasive isolates resistant to fluoroquinolones in 2009
..................................... ...................................................
5.29: Klebsiella pneumoniae: trend of multiresistance (third-generation cephalosporins, fluoroquinolones and aminoglycosides) by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54
59 59 5.32: Pseudomonas aeruginosa: proportion of invasive isolates resistant to fluoroquinolones in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .60 5.33: Pseudomonas aeruginosa: proportion of invasive isolates resistant to aminoglycosides in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .60 5.34: Pseudomonas aeruginosa: proportion of invasive isolates resistant to carbapenems in 2009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 61 5.35: Pseudomonas aeruginosa: trend of piperacillintazobactam resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62 5.36: Pseudomonas aeruginosa: trend of ceftazidime resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 63 5.37: Pseudomonas aeruginosa: trend of fluoroquinolones resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 64 5.38: Pseudomonas aeruginosa: trend of aminoglycosides resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 65 5.39: Pseudomonas aeruginosa: trend of carbapenems resistance by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .66
5.30: Pseudomonas aeruginosa: proportion of invasive isolates resistant to piperacillintazobactam in 2009 5.31: Pseudomonas aeruginosa: proportion of invasive isolates resistant to ceftazidime in 2009
....................................... .......................................................
5.40: Pseudomonas aeruginosa: trend of multiresistance (R to three or more antibiotic classes among piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems) by country, 20062009 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Abbreviations and acronyms
AMR AmpC ARMed AST BSAC BSI CC CMY CLSI CREC CRKP CSF DCFP DEFS DG SANCO DIN DNA EARSS EARS-Net ECDC ENSP EU EQA ESAC ESBL ESCMID ESGARS EUCAST FREC GISA GRC ICU IMP Antimicrobial resistance Ampicillinase C Antibiotic resistance surveillance and control in the Mediterranean region Antimicrobial susceptibility testing British Society for Antimicrobial Chemotherapy Bloodstream infections Clonal complex Cephamycinase Clinical and Laboratory Standards Institute Third-generation cephalosporin-resistant E. coli Third-generation cephalosporin-resistant K. pneumoniae Cerebrospinal fluid Data Check and Feedback Programme Data Entry & Feedback Software Directorate-General for Health and Consumer Protection Deutsche Industrie Norm (German) Deoxyribonucleic acid European Antimicrobial Resistance Surveillance System European Antimicrobial Resistance Surveillance Network European Centre for Disease Prevention and Control Erythromycin non-susceptible Streptococcus pneumoniae European Union External quality assessment European Surveillance of Antimicrobial Consumption Extended-spectrum beta-lactamase European Society of Clinical Microbiology and Infectious Diseases ESCMID Study Group for Antimicrobial Resistance Surveillance European Committee on Antimicrobial Susceptibility Testing Fluoroquinolone-resistant E. coli Glycopeptide intermediate-resistant Staphylococcus aureus Commissie Richtlijnen Gevoeligheidsbepalingen (Dutch) Intensive care unit Imipenemase VIM VRE VREF VRSA WHO WHONET UK NEQAS VISA SIR SHV SFM KPC MIC MLS MNSP MRSA NDM-1 NRL NWGA OXA PBP PCV PNSP PRSP RNA SeqNet Klebsiella pneumoniae carbapenemase Minimum inhibitory concentration Macrolide, lincosamide and streptogramin Macrolide non-susceptible S. pneumoniae Meticillin-resistant Staphylococcus aureus New Delhi metallo-beta-lactamase 1 National reference laboratories Norwegian Working Group on Antimicrobials Oxacillinase gene Penicillin-binding protein Pneumococcal conjugate vaccine Penicillin-non-susceptible Streptococcus pneumoniae Penicillin-resistant Streptococcus pneumoniae Ribonucleic acid European Network of Laboratories for Sequence Based Typing of Microbial Pathogens Comit de lAntibiogramme de la Socit Franaise de Microbiologie (French) Sensitive, intermediate, resistant Sulfhydryl-variable extended-spectrum beta-lactamase gene
Spa-typing S. aureus protein A-gene sequence typing SRGA TESSy TEM Swedish Reference Group for Antibiotics The European Surveillance System (at ECDC) Temoneira extended-spectrum betalactamase gene United Kingdom National External Quality Assessment Scheme for Microbiology Vancomycin-intermediate Staphylococcus aureus Verona integron-encoded metallo-beta-lactamase Vancomycin-resistant enterococci Vancomycin-resistant Enterococcus faecalis Vancomycin-resistant Staphylococcus aureus World Health Organization WHO microbiology laboratory database software
vii
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Countries participating in EARS-Net 2010
Participating countries Non participating countries
IS
FI NO SE EE LV DK IE UK NL BE LU DE CZ PL LT
FR
AT SI
HU RO
PT ES IT BG
EL
MT
CY
AT BE BG CY CZ DE DK EE EL ES
Austria Belgium Bulgaria Cyprus Czech Republic Germany Denmark Estonia Greece Spain
FI FR HU IE IS IT LT LU LV MT
Finland France Hungary Ireland Iceland Italy Lithuania Luxembourg Latvia Malta
NL NO PL PT RO SE SI UK
Netherlands Norway Poland Portugal Romania Sweden Slovenia United Kingdom
As of 1 January 2010, only EU and EEA Member States can report data to EARS-Net. Antimicrobial resistance surveillance data from five countries previously participating in EARSS (Bosnia-Herzegovina, Croatia, Israel, Switzerland and Turkey) are therefore not included in this report.
ix
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
National institutions/organisations participating in EARS-Net
Austria
Federal Ministry of Health Medical University Vienna Elisabethinen Hospital, Linz
www.elisabethinen.or.at
National and Kapodistrian University of Athens, Medical School
www.mednet.gr/whonet
Hungary
National Centre for Epidemiology
www.antsz.hu
Belgium
Scientific Institute of Public Health
www.iph.fgov.be
Ireland
Health Protection Surveillance Centre (HPSC)
www.hpsc.ie
University of Antwerp
Bulgaria
Alexander University Hospital, Sofia National Center of Infectious and Parasitic Diseases
Iceland
National University Hospital of Iceland Centre for Health Security and Infectious Disease Control
Cyprus
Nicosia General Hospital
Italy
National Institute of Public Health
www.simi.iss.it/antibiotico_resistenza.htm
Czech Republic
National Institute of Public Health National Reference Laboratory for Antibiotics
Latvia
Paul Stradins Clinical University Hospital State Agency Infectology Centre of Latvia
Denmark
Statens Serum Institut, Danish Study Group for Antimicrobial Resistance Surveillance (DANRES)
www.danmap.org
Lithuania
National Public Health Surveillance Laboratory Institute of Hygiene
Estonia
Health Board East-Tallinn Central Hospital Tartu University Hospital
Luxembourg
National Health Laboratory Microbiology Lab, Luxembourgs Hospital Centre
Finland
National Institute for Health and Welfare, Finnish Hospital Infection Program (SIRO)
www.thl.fi/siro
Malta
Hospital of Malta
Netherlands
National Institute for Public Health and the Environment
Finnish Study Group for Antimicrobial Resistance (FiRe)
www.finres.fi
Norway
University Hospital of North Norway Norwegian Institute of Public Health St. Olav University Hospital, Trondheim
France
Piti-Salptrire Hospital National Institute for Public Health Surveillance
www.invs.sante.fr
French National Observatory for the Epidemiology of Bacterial Resistance to Antimicrobials (ONERBA): AzayRsistance, le-de-France and Russir networks
www.onerba.org
Poland
National Medicines Institute
Portugal
National Institute of Health Dr. Ricardo Jorge
www.insarj.pt
National Reference Centre for Pneumococci (CNRP)
Germany
Robert Koch Institute
Ministry of Health Directorate-General of Health
Greece
Hellenic Pasteur Institute National School of Public Health
Romania
National Institute of Research and Development for Microbiology and Immunology Cantacuzino Institute of Public Health
xi
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Slovenia
National Institute of Public Health University of Ljubljana
Spain
Health Institute Carlos lll
www.isciii.es/htdocs/en/index.jsp
National Centre of Epidemiology
Sweden
Swedish Institute for Infectious Disease Control
www.smittskyddsinstitutet.se
United Kingdom
Health Protection Agency
www.hpa.org.uk
Health Protection Scotland Public Health Agency Northern Ireland
xii
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Summary
This is the first Annual Report of the European Antimicrobial Resistance Surveillance Network (EARSNet) after the transition of the European Antimicrobial Resistance Surveillance System (EARSS) to the European Centre of Disease Prevention and Control (ECDC) by 1 January 2010. This report represents the continuation of the series of highly valued EARSS Annual Reports published by the network since 2001. During the last decade, antimicrobial resistance has moved steadily to a more and more prominent position on the public health agenda in Europe. The surveillance of antimicrobial resistance conducted previously by EARSS, and currently by EARS-Net, has played an important role to provide documentation of the occurrence and spread of antimicrobial resistance, and to increase awareness of the problem at the political level, among public health officials and in the scientific community. Based on the antimicrobial resistance data reported to EARS-Net by 28 countries in 2009, and on the results of trend analyses including EARSS data from previous years, the resistance situation in Europe displays large variation depending on pathogen type, antimicrobial substance and geographic region. In 2009, the most concerning resistance results come from the rapidly decreasing susceptibility of invasive Escherichia coli to basically all antimicrobial agents included in the EARS-Net surveillance except carbapenems, and from the high prevalence of resistance in Klebsiella pneumoniae to third-generation cephalosporins, fluoroquinolone and aminoglycosides. In half of the reporting countries, the proportion of multiresistant K. pneumoniae isolates (combined resistance to third-generation cephalosporins, fluoroquinolones and aminoglycosides) is above 10%, and a few countries are now also reporting high proportions of resistance to carbapenems. These antibiotics have been widely used in many countries due to the increasing rate of extended-spectrum beta-lactamase (ESBL) producing Enterobacteriaceae with a consequent impact on the emergence of carbapenemase production (VIM, KPC and NDM-1), especially in K. pneumoniae. The highest resistance proportions in E. coli were reported for aminopenicillins ranging up to 66%. Irrespective of the high level of resistance, proportions continue to increase even in countries already presenting resistance levels well above 50%. Resistance to third-generation cephalosporins in E. coli has also increased significantly during the last four years in more than half of the reporting countries. This resistance is directly linked to the high proportions (85100%) of ESBL positives among the resistant isolates in countries reporting on ESBL in 2009. Other trends in the occurrence of resistance reported to EARS-Net bring hope that national efforts on infection control and efforts targeted at containment of resistance may in some cases bring the development of resistance to a halt, or even reverse undesirable resistance trends, as exemplified by the development for meticillin-resistant Staphylococcus aureus (MRSA). Even though the proportion of MRSA among Staphylococcus aureus is still above 25% in 10 out of 28 countries, the occurrence of MRSA is stabilising or decreasing in some countries and a sustained decrease was observed in Austria, France, Ireland, Latvia and UK. Furthermore, the United Kingdom has shown a consistent reduction of resistant proportions in K. pneumoniae for all the antibiotic classes under surveillance, and in a few countries (Greece, Germany, Italy and France) the efforts to control glycopeptide resistance in Enterococcus faecium seem to be successful and resulting in a continuous decrease of proportions of resistant isolates. Meanwhile, high-level aminoglycoside resistance in Enterococcus faecalis seems to stabilise at a relatively high level. The majority of countries reported proportions of resistant isolates between 30% and 50%. For Streptococcus pneumoniae, non-susceptibility to penicillin is generally stable in Europe and non-susceptibility to macrolides has declined in six countries while no country reported increasing trends. For Pseudomonas aeruginosa, high proportions of resistance to fluoroquinolones, carbapenems and combined resistance have been reported by many countries, especially in southern and eastern Europe. For several antimicrobial and pathogen combinations, e.g. fluoroquinolone resistance in E. coli, K. pneumoniae, P. aeruginosa and for MRSA, a north to south gradient is evident in Europe. In general, lower resistance proportions are reported in the north and higher proportions in the south of Europe likely reflecting differences in infection control practices, presence or absence of legislation regarding prescription of antimicrobials and other factors known to influence the occurrence of resistance. However, for K. pneumoniae, increasing trends of resistance to specific antibiotic classes and of multiresistance have been observed also in northern European countries, like Denmark and Norway, with a traditionally prudent approach to the antibiotic use. In addition to the regular trend analysis and situation overview, this 2009 EARS-Net report features a new focus chapter providing in-depth analysis for E. coli and MRSA. These analyses are based exclusively on data from laboratories reporting consistently over several years. The in-depth analysis confirms a consistent rise in multidrug resistance and reveals a steady and significant decline of antimicrobial susceptibility in E. coli
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
over several years. For MRSA, the observed decline likely reflects the efficacy of infection control measures at hospital level, and may even leave some hope for the success of containment strategies in other areas. In conclusion, the data reported to EARS-Net for 2009 by the participating countries provide a knowledge baseline on the occurrence of antimicrobial resistance in Europe and document the unfortunate and steadily diminishing antimicrobial treatment options for major bacterial pathogens.
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
1 Introduction
The European Antimicrobial Resistance Surveillance Network (EARS-Net) is a European-wide network of national surveillance systems, providing European reference data on antimicrobial resistance for public health purposes. The network is coordinated and funded by the European Centre for Disease Prevention and Control (ECDC). The surveillance of antimicrobial resistance within the EU is carried out in agreement with Decision No 2119/98/ EC of the European Parliament and of the Council of 24 September 1998 and Regulation (EC) No 851/2004 of the European Parliament and of the Council of 21 April 2004 establishing a European Centre for Disease Prevention and Control. The coordination of EARS-Net (former EARSS) was transferred from the Dutch National Institute for Public Health and the Environment (RIVM) to ECDC in January 2010. At the same time, EU Member States were requested to nominate disease-specific contact points for antimicrobial resistance. Five non-EU Member States previously participating in EARSS (Bosnia-Herzegovina, Croatia, Israel, Switzerland and Turkey) had to be detached from the network. At ECDC, the management and coordination of EARS-Net is carried out by the Section for Antimicrobial Resistance and Healthcare-associated Infections. Scientific guidance and support to the coordination of the network is provided by the EARS-Net Coordination Group (previous EARSS Advisory Board), composed of experts selected among the nominated disease-specific contact points and experts selected from other organisations involved in surveillance of antimicrobial resistance. EARS-Net consists of national antimicrobial resistance surveillance networks in Europe and conducts surveillance of antimicrobial susceptibility in seven major invasive pathogens of public health importance: Streptococcus pneumoniae, Staphylococcus aureus, Escherichia coli, Enterococcus faecalis, Enterococcus faecium, Klebsiella pneumoniae and Pseudomonas aeruginosa. The national networks systematically collect data from clinical laboratories in their own countries. At present, EARS-Net includes over 900 public health laboratories serving over 1 400 hospitals in Europe. The national networks upload data to a central database at ECDC (The European Surveillance System TESSy). EARS-Net maintains an interactive database at the ECDC website (www.ecdc.europa.eu) and publishes annual reports on the occurrence of antimicrobial resistance in Europe. This constitutes an important source of information on antimicrobial resistance for policymakers, scientists, doctors and the public.
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
2 Escherichia coli and Staphylococcus aureus: bad news and good news. Analysis of data from laboratories reporting continuously from 2002 to 2009
The results presented in this focus chapter are based on data from laboratories (n=198) that participated to EARS-Net and previously EARSS from 2002 to 2009, and reported continuously during the period on susceptibility of Escherichia coli and Staphylococcus aureus to selected antimicrobial agents. The long-standing contribution of these laboratories to the surveillance of antimicrobial resistance allow for accurate comparison of proportions of resistant isolates and number of reported infections over time. Thus, results presented in this focus chapter may be slightly different from results obtained from the full group of laboratories reporting to EARS-Net and previously to EARSS. and combined resistance of invasive and non-invasive isolates is reported in several national European surveillance reports [26]. At the same time, the proportion of MRSA has showed a significant decrease in many European countries. The numbers of BSI caused by MRSA, as reported by the mandatory surveillance system in England, decreased by 56% between 2004 and 2008 [7], and in France a significant decrease in the occurrence of MRSA was reported in 2008 [8] A similar reduction of the rate of healthcare-associated invasive MRSA infections has been observed at population level in the United States [9]. A total of 198 laboratories in 22 countries reported continuously from 2002 to 2009. The number of laboratories per country ranged between 1 (Iceland and Malta) and 33 (Czech Republic) (Table 2.1). Considering the whole group of selected laboratories, the reported number of E. coli BSI, increased by 71% from 10 688 in 2002 to 18 240 in 2009. In the same period, S. aureus BSI showed a 34% increase from 7 855 to 10 503 (Figure 2.1); this increase was observed in most but not all countries (Table 2.1). During this interval, the proportion of third-generation cephalosporin-resistant E. coli increased significantly from 1.7% to 8% (p < 0.001) and the proportion of MRSA decreased from 21.5% to 19.7% (p < 0.001) (Figure 2.2). The trends of resistance proportions at country level were consistent with those of the whole group of 198 laboratories in 18 countries out of 22 for E. coli and in seven countries out of 22 for S. aureus. Combined resistance in E. coli (defined as resistance to two, three and four antibiotic classes reported to EARS-Net) showed a significant increase (Figure 2.3) (p < 0.001) and became a frequent phenotype in most countries, whereby single resistance diminished from 37.1% in 2002 and 35.8% in 2009 (p < 0.001). The proportion of isolates susceptible to all four antibiotic classes decreased from 51.4% in 2002 to 41.7% in 2009 (p < 0.001). The decline of antimicrobial activity in E. coli was evident both through the observed increase of combined resistance and through the reduction of full susceptibility to the antimicrobials included in the analysis. In the same time period and considering the same data source, a significant decrease of meticillin resistance was observed for S. aureus. For this species, the number of BSI increased less (+34%) than for E. coli BSI (+71%).
Key points
A significant decline of antimicrobial susceptibility was observed for E. coli between 2002 and 2009, with a concomitant increase of reported bloodstream infections of 71%. S. aureus showed a different tendency, with a significant decrease of the proportion of meticillin resistance (MRSA) and an increase of 34% in the number of reported bloodstream infections. The trends observed for E. coli could suggest an incremental burden of disease caused by this microorganism, and the simultaneous decline of antimicrobial susceptibility is a serious public health concern. The reduction of the MRSA proportion and the relative containment of the number of S. aureus infections could result from efficacy of infection control measures at hospital level in some countries. However, efforts to reduce MRSA occurrence should remain a priority, irrespective of decreasing trends.
Escherichia coli and Staphylococcus aureus are the most frequent causes of bloodstream infections (BSI). The temporal trends of resistance and the trends in the incidence of BSI caused by these microorganisms, observed through the EARSS/EARS-Net data, are described for the period 20022009. The antimicrobial susceptibility of E. coli BSI isolates shows an alarming Europe-wide decline as previously reported by EARSS [1]. Increasing resistance in E. coli
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Importantly, most of the rise (38% of 71%) in E. coli BSI appeared to be due to isolates resistant to two or more antibiotics. Furthermore, the increase in the number of BSI was similar for meticillin-susceptible S. aureus (MSSA, 37%) and for fully susceptible E. coli (39%). Despite the possible limitations of the presented results (see section 2.2), the trends of third-generation cephalosporins and combined resistance are relevant findings that deserve further consideration. According to the results, it appears that, during the study period, the emergence and spread of combined resistance is the main factor that influences the decline of antimicrobial activity against E. coli. In the period 20022009, only an increase of combined resistance with a concurrent relative reduction of the proportion of single resistance was observed. The resistant subpopulation with the largest relative growth in the period 20022009 was the resistance to all the four antibiotic classes under surveillance: this pattern increased more than fivefold from 0.6% to 3.4%. This trend suggests that inside the subpopulation of resistant isolates there was a continuous relative growth of combined resistance possibly caused by the addition of resistance traits to strains that were already resistant to at least one among the considered antibiotic classes. This trend may be explained by the spread of multidrug-resistant plasmids, which also contain genes for extended-spectrum beta-lactamase (ESBL) production [10]. The growing number of E. coli BSI indicates an increasing burden of disease caused by this microorganism. A similar trend in the number of reported cases of E. coli BSI has been observed in England, Wales and Northern Ireland by the national voluntary surveillance scheme, in the period 20042008. The increase (38%) observed by
the British surveillance system is greater than the 16% increase in all BSI reported in the country during the same time period [11]. In conclusion, the reported data show a significant increase of antimicrobial resistance in E. coli invasive isolates and an overall increase in BSI caused by this microorganism. This is a serious public health concern since, if the increasing trend of antimicrobial resistance and the spread of ESBL are not contained, the use of carbapenems will increase favouring the emergence of carbapenemase-producing enterobacteria. This has been already observed for Klebsiella pneumoniae in Greece, Israel and Cyprus [1]. At the same time, S. aureus showed a relatively smaller increase in the number of reported BSI, but a significant decrease in the proportion of MRSA overall in EARSS/ EARS-Net. This could be the result of the public health efforts targeted at containment of MRSA in several European countries and in the US. Even though an overall decreasing trend for MRSA is evident in Europe, not all countries contribute to this result. Efforts to reduce MRSA occurrence should remain a priority irrespective of decreasing trends. In this perspective, coordinated international surveillance is particularly important in order to obtain accurate knowledge of the occurrence and spread of antimicrobial resistance and to enable planning of public health interventions aimed at prevention and control of the problem.
2.1 Methods of analysis
Data for E. coli and S. aureus BSIs were extracted from the EARSS/EARS-Net database for laboratories
Table 2.1: Average numbers of Escherichia coli and Staphylococcus aureus isolates per country reported yearly from 2002 to 2009 by laboratories participating continuously in EARSS/EARS-Net during this time interval
Country Austria Belgium Bulgaria Czech Republic Estonia Finland France Germany Greece Hungary Iceland Ireland Italy Luxemburg Malta Netherlands Norway Portugal Slovenia Spain Sweden United Kingdom Number of laboratories 10 9 7 33 5 5 12 2 22 14 1 15 3 4 1 4 7 8 9 19 3 5 Number of E. coli isolates average per year (20022009) 802 646 96 1 837 142 849 1 583 156 829 446 97 1 086 237 176 104 291 975 559 572 1 973 578 641 Number of S. aureus isolates average per year (20022009) 630 343 82 1 290 125 381 1 018 121 472 526 56 961 166 80 96 238 467 574 321 835 331 373
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 2.1: Yearly number of bloodstream infections caused by Escherichia coli and Staphylococcus aureus. EARSS/ EARS-Net 20022009 (22 countries/198 laboratories)
20000 No. bloodstream infections E. coli S. aureus 15000
10000
5000 2002 2003 2004 2005 2006 2007 2008 2009
Only laboratories reporting susceptibility results for specific antimicrobials continuously during the period 20022009 are included in the analysis.
Figure 2.2: Proportion of third-generation cephalosporin-resistant Escherichia coli (CREC) and meticillin-resistant Staphylococcus aureus (MRSA). EARSS/EARS-Net 20022009 (22 countries/198 laboratories)
25 MRSA Third-generation cephalosporin-resistant E. coli
Percent resistant isolates among species
20
15
10
0 2002 2003 2004 2005 2006 2007 2008 2009
Only laboratories reporting susceptibility results for specific antimicrobials continuously during the period 20022009 are included in the analysis.
Figure 2.3: Combined resistance (R) of Escherichia coli to aminopenicillins, third-generation cephalosporins, fluoroquinolones and aminoglycosides. EARSS/EARS-Net 20022009 (22 countries/198 laboratories)
12 10 Percent isolates 8 6 4 2 0 2002 2003 2004 2005 2006 2007 2008 2009 R to two antimicrobial classes R to three antimicrobial classes R to four antimicrobial classes
Only laboratories reporting susceptibility results for specific antimicrobials continuously during the period 20022009 are included in the analysis.
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
reporting susceptibility results continuously during the period 20022009 for aminopenicillin, fluoroquinolones, third-generation cephalosporin and aminoglycosides in E. coli and for oxacillin in S. aureus. Countries with no laboratory participating for the entire period or with small amount of data (less than 20 isolates per microorganism and per year) were not included in the analysis. Only the first isolate per patient, microorganism and year was included. The number of BSI caused by E. coli and S. aureus and the proportions of third-generation cephalosporin resistant E. coli and of MRSA were calculated for each year of the period 20022009. Three additional antibiotic classes (aminopenicillins, aminoglycosides and fluoroquinolones) were also considered for E. coli to assess the patterns of combined resistance of this pathogen. The significance of the temporal trends for resistance proportions was evaluated by the Cochran-Armitage test for trend.
8.
Anonymous. Recent trends in antimicrobial resistance among Streptococcus pneumoniae and Staphylococcus aureus isolates: the French experience. Euro Surveill. 13 Nov 2008;13(46). Kallen AJ, Mu Y, Bulens S et al. Health care-associated invasive MRSA infections, 20052008. JAMA 2010;304(6):641-648.
9.
10. Coque TM, Baquero F, Canton R. Increasing prevalence of ESBLproducing Enterobacteriaceae in Europe. Euro Surveill 20 Nov 2008;13(47). 11. HPA. Escherichia coli bacteraemia in England, Wales, and Northern Ireland, 2004 to 2008. London: Health Protection Agency, 2009.
2.2 Limitations of the analysis
Even considering a stable group of laboratories, it is still possible that a change in the population coverage of these laboratories has occurred over time. The different trends observed for E. coli and S. aureus could also be explained by ascertainment bias leading to higher reporting of E. coli infections and caused by an increase of empirical treatment failures triggering delayed diagnostic procedures (blood culture). The indicator used to monitor the resistance trend was the SIR (sensitive, intermediate, resistant) interpretation, since the actual MIC (minimum inhibitory concentration) values are not systematically made available by participating laboratories. Reporting MIC instead of the SIR interpretation defined by clinical breakpoints would improve the monitoring of dynamic and subtle changes of antimicrobial susceptibility.
2.3 References
1. 2. RIVM. EARSS annual report 2008. Bilthoven: Rksinstituut voor Volksgezondheid en Milieu; 2009. DANMAP 2008. Jensen VJ, Hammerum A (eds). Consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, food and humans in Denmark. Copenhagen: National Food Institute, Technical University of Denmark; 2009. Health Protection Agency. Antimicrobial Resistance and Prescribing in England, Wales and Northern Ireland, 2008. London: Health Protection Agency; 2008. NORM/NORM-VET 2009. Norstrm M, Simonsen GS (eds). Usage of Antimicrobial Agents and Occurrence of Antimicrobial Resistance in Norway. Troms/Oslo; 2010. RIVM, SWAB. NethMap 2009. Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands. SWEDRES 2009. Dohnhammar U, Olsson-Liljequist B (eds). A Report on Swedish Antimicrobial Utilisation and Resistance in Human Medicine. Swedish Strategic Programme against Antibiotic Resistance (STRAMA). Stockholm: Swedish Institute for Infectious Disease Control; 2010. Pearson A, Chronias A, Murray M. Voluntary and mandatory surveillance for methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus (MSSA) bacteraemia in England. J Antimicrob Chemother. 2009;64(Suppl 1):i11-7.
3.
4.
5.
6.
7.
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
3 External Quality Assessment Exercise (EQA) 2009
3.1. Introduction
Since 2000, EARSS has been organising external quality assessment (EQA) exercises of antimicrobial susceptibility testing in collaboration with UK NEQAS (United Kingdom National External Quality Assessment Service). UK NEQAS is based at the Health Protection Agency, in London, and is a non-profit organisation with more than 35 years experience with external quality assessment in different countries (www.ukneqasmicro.org.uk). The rationale of these EQA exercises is: to assess the ability of participating laboratories to identify antimicrobial resistance of clinical and public health importance; to determine the accuracy of susceptibility test results reported by individual laboratories; and to decide on the overall comparability of routinely collected test results between laboratories and countries and thus provide the means for justifying the pooling and comparison of antimicrobial susceptibility test (AST) data across Europe. The external quality assessment exercise, held in the second half of 2009, was open to all countries participating in EARSS in 2009, including Bosnia-Herzegovina, Croatia, Israel and Turkey. A panel of six strains was included in the exercise. The strains were characterised and tested in two reference laboratories (Addenbrookes Hospital, Cambridge, and City Hospital, Birmingham). Both reference laboratories confirmed MICs and interpreted the results according to frequently used breakpoint criteria such as CLSI and EUCAST, as indicated in each of the species chapters. or combined methods (23%). For species identification, 60% used automated and 40% used conventional methods. The majority of laboratories applied CLSI guidelines (68%), and some countries used national guidelines, e.g. France (SFM), UK (BSAC), and Sweden (SRGA). The use of EUCAST guidelines was mainly reported by laboratories that utilise automated diagnostic test systems already calibrated for EUCAST breakpoints. However, the UK, Sweden, the Netherlands, Germany, France and Norway have been implementing EUCAST breakpoints in their national MIC breakpoint recommendations as harmonised breakpoints have been agreed, and in addition have adjusted the interpretation of their disk diffusion methods accordingly. Harmonisation efforts between the different national guideline committees have accomplished a satisfactory degree of agreement and, therefore, previous discrepancies between different guidelines have become less significant. Figure 3.2 shows the adherence to (inter)national guidelines by number of laboratories per country.
3.2.1. Specimen 9448 Escherichia coli
This specimen consisted of an Escherichia coli with CTX-M-14 ESBL production. Unlike most TEM- and SHVderived ESBLs, CTX-M enzymes are more active against cefotaxime than ceftazidime. This organism should clearly be interpreted as resistant to cefotaxime (MIC 128 mg/L) using EUCAST (S 1, R > 2 mg/L), and CLSI (S 8, R 64 mg/L) guidelines. With ceftazidime (MIC 2 mg/L) the isolate appears intermediate by EUCAST guidelines (S 1, I 28, R > 8 mg/L) and susceptible by standard CLSI guidelines (S 8, I 16, R 32 mg/L). However, current EUCAST expert rules recommend that ESBL-producing isolates are reported resistant if they appear intermediate in routine tests and intermediate if they appear susceptible. Resistance should be reported if CLSI ESBL screening methods are used as recommended. Detection of reduced susceptibility to cefotaxime and ceftriaxone was not a problem and < 1% participants reported the organism susceptible to these agents. With ceftazidime, reports of intermediate (15%) and susceptible (6%) were more common. A large majority (98%) of participants testing for ESBLs correctly reported the organism ESBL-positive. This organism was susceptible to piperacillin+tazobactam in MIC tests (MIC 24 mg/L). Despite some reports of clinical efficacy, there has been considerable debate about whether ESBL-producing strains from serious infections should be reported susceptible to beta-lactamase inhibitor combinations when they appear susceptible in routine tests. While the majority
3.2. Results
Strain panels were distributed to 886 participating laboratories, who were asked to report the clinical susceptibility categorisation susceptible, intermediate and resistant (S, I, R) according to the guideline used. The laboratories returned 775 (87%) reports, which is equivalent to the return rate of previous years. Turkey was not able to perform the tests, due to difficulties related to the shipment of strains. Figure 3.1 shows the proportion of participating laboratories returning reports per country. All results were collected via the UK NEQAS internet website. Results were analysed and considered concordant if the reported categorisation agreed with the interpretation of the reference laboratories. For the determination of AST results, laboratories used automated methods (35%), disc diffusion tests (33%),
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 3.1: Proportion of participating laboratories returning reports per country, 2009
AT BA BE BG CY CZ DE DK EE EL ES FI FR HR HU IE IL IS IT LT LU LV MT NL NO PL PT RO SE SI TR UK 0 20 40 60 80 100 Results No results
Country code
Number of laboratories
The external quality assessment exercise was open to all countries participating in EARSS in 2009. BA = Bosnia-Herzegovina; HR = Croatia; IL = Israel; TR = Turkey.
Figure 3.2: Adherence to guidelines*: number of laboratories per country
AT BA BE BU CY CZ DE DK EE EL ES FI FR HR HU IE IL IS IT LT LU LV MT NL NO PL PT RO SE SI UK 0 10 20 30 40 50 60 70 80 BSAC COMB CRG DIN EUCAST FIRE NCCLS NWGA SFM SRGA Other
Country code
Number of laboratories
BSAC, British Society for Antimicrobial Chemotherapy; CRG, (Dutch) Commissie Richtlijnen Gevoeligheidsbepalingen; DIN, Deutsche Industrie Norm; EUCAST, European Committee on Antimicrobial Susceptibility Testing; NCCLS/CLSI, (American) Clinical and Laboratory Standards Institute; NWGA, Norwegian Working Group on Antimicrobials; SFM, Comit de lAntibiogramme de la Socit Franaise de Microbiologie; SRGA, Swedish Reference Group for Antibiotics. BSAC, CRG, DIN, NWGA, SFM and SRGA have implemented EUCAST breakpoints for MIC determinations and have adjusted the interpretation of their disk diffusions accordingly. The external quality assessment exercise was open to all countries participating in EARSS in 2009. BA = Bosnia-Herzegovina; HR = Croatia; IL = Israel.
10
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
of participants (71%) reported the organism susceptible to piperacillin+tazobactam, significant proportions reported intermediate (9%) or resistant (20%). In reference tests, this organism was resistant to gentamicin, highly variable in susceptibility to tobramycin (reference MICs 4 to > 128 mg/L) and susceptible to amikacin. It is likely that this reflects production of an ANT (2) enzyme, expression of which can be variable. EUCAST expert rules suggest that such isolates should be reported resistant to tobramycin if they appear intermediate. While 99% participants reported the organism gentamicin resistant and 98% amikacin susceptible, for tobramycin, 30%, 28% and 42% were reporting resistant, intermediate and susceptible, respectively (Table3.1).
3.2.2. Specimen 9449 Klebsiella pneumoniae
This organism is a Klebsiella pneumoniae with a highlevel beta-lactamase production; not only penicillin resistant, but also reduced susceptibility to beta-lactamase inhibitor combinations. Piperacillin+tazobactam MICs of 64 to 128 mg/L for this organism indicate resistance by EUCAST breakpoints and intermediate/resistant by CLSI breakpoints. Among participants, 70% reported the organism resistant, 25% intermediate and 5% susceptible. ESBL production was incorrectly reported by 9% participants and this was frequently associated with incorrect reporting of resistance to cefotaxime, ceftriaxone and ceftazidime by these participants (Table 3.2).
oxacillin discs, those that screened with oxacillin and confirmed with a penicillin MIC, and those that tested with other methods. Overall, 76% reported the isolate as being of intermediate susceptibility to penicillin, with a further 8% reporting the isolate resistant. Susceptibility reported to clinicians for this organism if isolated from cases of meningitis or pneumonia indicates that many participants do interpret test results to suit the clinical situation. Eighty-five per cent reported the isolate as resistant when the isolate was from a case of meningitis and 70% as susceptible when the isolate was from a case of pneumonia, but significant numbers of participants interpreted the organism as intermediate in susceptibility to penicillin irrespective of whether the isolate was from meningitis (11% reported intermediate) or from pneumonia (26% reported intermediate). However, it is recognised that some local reporting guidelines may recommend categorisation of pneumonia isolates with intermediate penicillin susceptibility as intermediate, with the note that the isolate is susceptible if the patient is treated with a high dose. With EUCAST, breakpoints for ciprofloxacin wild type organisms such as this (MIC 1 mg/L) are reported intermediate in susceptibility to ciprofloxacin, reflecting the uncertain outcome of therapy. CLSI do not give ciprofloxacin breakpoints for S. pneumoniae. This uncertainty was reflected in the high discrepancy rate in reporting for this agent (69% susceptible, 27% intermediate and 4% resistant) (Table 3.3).
3.2.3. Specimen 9450 Streptococcus pneumoniae
This organism is a Streptococcus pneumoniae with reduced susceptibility to penicillin (MIC 0.25 mg/L). For S. pneumoniae with no mechanism of resistance to penicillin, MICs are 0.06 mg/L. EUCAST guidelines divide reduced susceptibility to penicillin into intermediate (penicillin MIC 0.122 mg/L) and resistant (MIC >2mg/L) categories. However, the interpretation of susceptibility to penicillin depends on whether the isolate is from a patient with meningitis or other infections (most commonly pneumonia). Strains with intermediate susceptibility are treatable with the high doses of penicillin, ampicillin or amoxicillin routinely used to treat pneumonia. Hence such strains may be reported susceptible in this situation. Patients with meningitis caused by strains with intermediate susceptibility to penicillin are unlikely to respond to therapy, and hence such strains should be reported as resistant in this situation. Overall, 92% participants reported resistance in the oxacillin screening test for penicillin resistance. A further 3% reported the isolate intermediate to oxacillin, although the oxacillin screening test does not distinguish penicillin intermediate and resistant isolates and published guidelines do not include an intermediate category. The participants results for penicillin will include those that only screened for reduced susceptibility with
3.2.4. Specimen 9451 Pseudomonas aeruginosa
This organism is a Pseudomonas aeruginosa with borderline resistance to piperacillin+tazobactam (MIC 3264 mg/L) but susceptible to ceftazidime, a susceptibility profile seen with some beta-lactamaseproducing strains. This organism produces the PSE-4 (CARB-1) beta-lactamase. The borderline resistance to piperacillin+tazobactam was reflected in the variation in susceptibility reported by participants, with 49% reporting susceptible, 12% intermediate and 39% resistant. The different categorisation largely relates to the breakpoint differences between EUCAST (susceptible 16 mg/L, resistant > 16 mg/L) and CLSI (susceptible 64mg/L, resistant 128 mg/L) (Table 3.4).
3.2.5. Specimen 9452 Pseudomonas aeruginosa
This organism is a Pseudomonas aeruginosa resistant to gentamicin and susceptible to other reference agents tested. Some laboratories experienced problems with piperacillin+tazobactam testing in that overall 14% participants reported the isolate intermediate and 2% resistant. The reason for the problems is not obvious as the isolate was clearly susceptible in reference tests (Table 3.5).
3.2.6. Specimen 9453 Staphylococcus aureus
This organism is a meticillin-resistant Staphylococcus aureus (EMRSA-6) and most participants correctly reported resistance. There was no significant difference
11
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
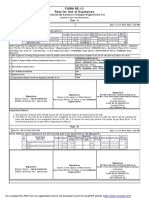
Table 3.1: Escherichia coli (9448): Minimum inhibitory concentration (MIC) and intended results reported by reference laboratories and the overall concordance of the participating laboratories
Antibiotic agent Amikacin Amoxicillin Ampicillin Cefotaxime Ceftazidime Ceftriaxone Ciprofloxacin ESBL Gentamicin Imipenem Meropenem Piperacillin Piperacillin+tazobactam Tobramycin MIC range ref. lab. from 1 NT* > 128 128 2 > 128 64 32 0.12 0.03 128 2 4 to 1 > 128 > 128 2 > 128 128 64 0.12 0.03 128 4 > 128 Intended interpretation EUCAST/CLSI Overall concordance (%) S 98 R 93 R 100 R 97 R (expert rule) 80 R 99 R 100 positive 98 R 99 S 100 S 99 R 99 S 71 I-R/S-I-R
* Not tested, result inferred from ampicillin.
Table 3.2: Klebsiella pneumoniae (9449): Minimal inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories
Antibiotic agent Amikacin Ampicillin/amoxicillin Cefotaxime Ceftazidime Ceftriaxone Ciprofloxacin ESBL Gentamicin Imipenem Meropenem Piperacillin Piperacillin+tazobactam Tobramycin MIC range ref. lab. from 64 128 0.12 0.12 0.5 0.015 64 0.12 0.03 64 64 16 to 64 128 0.5 0.25 0.5 0.03 128 0.12 0.03 128 128 128 EUCAST/CLSI R R S S S S negative R S S I/R I/R R Intended interpretation Overall concordance (%) 97 100 92 93 93 100 91 99 99 99 99 95 99
Table 3.3: Streptococcus pneumoniae (9450): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories
Antibiotic agent Cefotaxime Meningitis Pneumonia Ceftriaxone Meningitis Pneumonia Ciprofloxacin Clindamycin Erythromycin Oxacillin Penicillin Meningitis Pneumonia MIC range ref. lab. from 0.06 0.06 1 0.12 0.12 0.25 to 0.12 0.12 1 0.12 0.25 0.25 EUCAST/CLSI S S S S S S I/S S R I R S Intended interpretation Overall concordance (%) 98 96 99 98 95 98 27 99 99 92 76 85 70
12
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Table 3.4: Pseudomonas aeruginosa (9451): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories
Antibiotic agent Amikacin Ceftazidime Ciprofloxacin Gentamicin Imipenem Meropenem Piperacillin+tazobactam Tobramycin MIC range ref. lab. from 1 1 0.12 1 1 0.5 32 0.5 to 8 2 0.5 4 2 2 64 1 EUCAST/CLSI S S S S S S R/S S Intended interpretation Overall concordance (%) 100 98 100 97 99 99 39 99
Table 3.5: Pseudomonas aeruginosa (9452): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories
Antibiotic agent Amikacin Ceftazidime Ciprofloxacin Gentamicin Imipenem Meropenem Piperacillin+tazobactam Tobramycin MIC range ref. lab. from 1 1 0.12 16 1 0.5 4 0.5 to 4 2 0.25 64 2 2 8 1 EUCAST/CLSI S S S R S S S S Intended interpretation Overall concordance (%) 99 99 100 99 99 99 84 99
Table 3.6: Staphylococcus aureus (9453): Minimum inhibitory concentration (MIC) and intended results reported by the reference laboratories and the overall concordance of the participating laboratories
Antibiotic agent Cefoxitin Ciprofloxacin Erythromycin Fucidic acid Gentamicin Methicillin Oxacillin Penicillin Rifampicin Teicoplanin Tetracycline Vancomycin MIC range ref. lab. from 8 0.5 4 0.06 0.25 NT* 8 1 0.004 1 64 1 to 16 0.5 128 0.12 0.50 32 4 0.008 1 64 2 EUCAST/CLSI R S I/R S S R R R S S R S Intended interpretation Overall concordance (%) 95 95 93 100 99 97 94 99 99 99 97 99
* Not tested, result inferred from oxacillin and cefoxitin.
13
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
in reliability of detection of meticillin resistance in tests with oxacillin (94% participants reported resistance) and cefoxitin (95% participants reported resistance). About a third of participants reported a result for meticillin (97% resistant) but it may be that oxacillin or cefoxitin were actually tested. Erythromycin reference MICs were very variable (4 to > 128 mg/L), probably because resistant colonies of this organism grew slowly. MICs in this range indicate resistance by EUCAST breakpoints and intermediate/resistant by CLSI breakpoints; 93% participants reported the organism resistant and only 6% intermediate (Table 3.6).
3.3 Conclusions
In this eighth EARSS EQA exercise, participation of laboratories was high. The results show that routinely reported results, as collected by EARSS in most instances, have sufficient accuracy to provide good estimates of overall resistance prevalence and trends. The overall concordance was high, except in case of borderline susceptibility, when various guidelines reveal remaining discrepancies in routine susceptibility testing, and when a breakpoint was recently changed. The latter was found for penicillin susceptibility of Streptococcus pneumoniae in relation to the source of the isolate, where the isolate was regularly reported non-susceptible for pneumonia. Furthermore, differences in interpretation of results were found for piperacillin+tazobactam (as frequently noted previously). EARSS Management Team would like to thank UK NEQAS for Microbiology, the reference laboratories, the members of the Advisory Board, the country coordinators for the swift distribution of the strains, and all the participating laboratories for their excellent response rate.
14
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
4 EARS-Net laboratory/hospital denominator data 2009
4.1 Introduction
For correct interpretation of the EARS-Net data on antimicrobial resistance, accurate background information is important. Therefore, laboratory and hospital and denominator data are collected and presented in this chapter. laboratories and hospitals cluster in big cities and, for this reason, some of the catchment areas overlap. This could lead to double counts, which could artificially increase the estimated coverage. The coverage at European level possibly increased in 2009 compared to the previous year since the number of reporting laboratories increased from 825 in 2008 to 916 in 2009. A high coverage at country level is very important to properly describe the country profile and it also allows a more accurate calculation of the culture rate and the MRSA incidence rate. Calculation of the MRSA incidence rate (not included in the 2009 report) would be based on the assumption that each hospital is served by one laboratory. Therefore, in cases where the laboratory denominator data is referring to a specific hospital (with patient days available), calculation of the culture rate for that hospital is possible. Similarly, having AMR data referring to a specific hospital (with patient days available) would enable calculation the MRSA rate for that hospital. However, looking into the available data, this assumption seems not always correct. Some hospitals are served by more than one laboratory; it occurs mainly in UK (where the hospital code often refers to a trust instead of a single hospital), but there are examples also in Ireland and Hungary. The implication of the relation one hospital to more than one laboratory is that, if one hospital is reported in the AMR and denominator data while only one of the laboratories serving this hospital is reported, then the culture rate and the MRSA incidence rate will be underestimated.
4.2 Methods
Questionnaires, in Microsoft Excel files, were sent to the EARS-Net contact points at the beginning of June 2010. The contact points distributed the questionnaires to the participating laboratories and hospitals in their country. Information was collected on the total number of blood culture sets processed in the laboratories, and the number of hospital beds for each participating hospital, the type of hospital, the bed occupancy and the number of admissions. The national data managers received the completed questionnaires, compiled them and produced the final format suitable for uploading in the European Surveillance System (TESSy). Laboratories have been defined as reporting denominator data if they have provided the number of blood culture sets performed for one or for more than one hospital; hospitals have been defined as reporting denominator data if they have provided the number of beds.
4.3 Participation
Fifteen out of 28 countries reporting antimicrobial resistance results returned hospital denominator data while 14 countries returned laboratory denominator data. Considering the responding countries, 219 of the 307 laboratories (71.3%) and 606 of the 871 hospitals (69.6%) reporting antimicrobial susceptibility results for the 15 countries in 2009, also provided denominator data (Figures 4.14.2, Tables 4.14.3). Some denominator data of laboratories and hospitals not participating to antimicrobial resistance surveillance, or reporting zero cases, have been included in Figure 4.1, but were not included in the analysis.
4.5 Hospital denominator information
The total number of hospital beds for the hospitals reporting AMR results and providing denominator data in different countries ranged from 1 274 in Malta to 143 433 in France, reflecting the size of the country as well as the rate of participation to EARS-Net and the rate of response to the questionnaires. The proportion of ICU beds over total hospital beds shows wide variation according with the country, ranging from 1% in UK to 9% in Cyprus. The median length of stay was 6.6 days with a minimum in UK (3.4 days) and a maximum in Malta (12.7 days). The annual occupancy rate was 75% or higher in 10 out of 15 countries (Table 4.1).
4.4 Population coverage
The population coverage of antimicrobial resistance data at country level is not reported for 2009 because of the low number of countries submitting denominator data and because of possible limitations in the use of the data on population coverage: laboratories/hospitals reporting antimicrobial susceptibility data do not always provide denominator data and this could give a biased figure of the country population coverage since it can be calculated only for laboratories/hospitals with denominator data; and
4.6 Hospital characteristics
Both the size of a hospital and the level of specialisation can influence the proportion of resistance. As can be seen from Table 4.2 and Figure 4.2, the distribution of size and specialisation level of hospitals varied
15
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 4.1: Number of laboratories and hospitals reporting AMR and/or denominator data in 2009 A)
BG CY DE EE FR HU Country code IE IT LT LV MT PL PT SI UK 0 50 100 150 200 250 300 350 400 AMR and denominator information AMR information only Denominator information only
Number of hospitals
B)
BG CY DE EE FR HU Country code IE IT LT LV MT PL PT SI UK 0 50 100 150 200 250 AMR and denominator information AMR information only Denominator information only
Number of laboratories
16
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Table 4.1: Hospital denominator data for 2009
Country Bulgaria Cyprus Estonia France Germany Hungary Ireland Italy Latvia Lithuania Malta Poland Portugal Slovenia United Kingdom Hospitals reporting (denominator/AMR data) (20/22) (5/5) (13/14) (231*/242) (47/173) (62/65) (52/71) (25/25) (11/12) (22/30) (3/3) (30/30) (23/25) (12/12) (50/142) Total number of beds 9 326 1 313 4 989 143 433 18 897 40 749 12 175 15 358 5 251 9 792 1 274 15 045 10 885 6 559 60 775 Proportion of ICU beds (%) 8 9 6 5 6 2 3 5 2 4 5 2 5 5 1 Annual occupancy rate (%) 77 72 75 83 73 76 87 84 68 75 85 70 79 79 74 Median length of stay (days) 6.3 5.5 6.4 7.7 7.1 7.8 5.8 6.8 7.0 12.7 5.5 7.3 5.4 3.4 IQR length of stay (days) 5.46.9 5.45.7 5.17.0 6.49.2 6.79.1 6.59.6 4.67.1 5.67.4 6.38.1 5.438.6 4.46.2 5.58.6 4.86.2 2.76.1
* 178 hospitals in France reported data for a six-month period.
Table 4.2: Hospital characteristics for 2009
Country Bulgaria Cyprus Estonia France Germany Hungary Ireland Italy Latvia Lithuania Malta Poland Portugal Slovenia United Kingdom Hospitals reporting (denominator/AMR data) (20/22) (5/5) (13/14) (231/242) (47/173) (62/65) (52/71) (25/25) (11/12) (22/30) (3/3) (30/30) (23/25) (12/12) (50/142) Proportion of hospitals by level of care (%) Secondary level Primary level 35 5 20 40 38 23 78 0 32 30 29 15 52 12 28 4 55 0 55 5 33 0 77 10 26 4 50 17 20 6
Tertiary level 50 20 31 22 23 50 17 68 36 41 33 13 57 17 6
Other 10 20 0 0 15 6 17 0 0 0 33 0 13 17 18
Unknown 0 0 8 0 0 0 2 0 9 0 0 0 0 0 50
Primary level or district hospital = has few specialties, limited laboratory services; bed capacity ranges from 30 to 200 beds. Secondary level, or provincial hospital = highly differentiated by function with five to 10 clinical specialties; bed capacity ranging from 200 to 800 beds. Tertiary level or central/regional hospital = highly specialised staff and technical equipment; clinical services are highly differentiated by function; may have teaching activities; bed capacity ranges from 300 to 1500 beds. Other = hospitals for a specific patient population, like a military hospital, or hospitals with any single specialty, like a burns unit. Unknown = not available.
Table 4.3: Laboratory denominator information for 2009
Country Bulgaria Cyprus Estonia Germany Hungary Ireland Italy Latvia Lithuania Malta Poland Portugal Slovenia United Kingdom Laboratories reporting (denominator/AMR data) (18/20) (5/5) (9/11) (6/17) (26/27) (37/43) (25/25) (10/12) (12/13) (1/1) (30/30) (21/22) (9/9) (10/72) Number of hospitals* 20 5 11 28 60 51 25 10 20 3 30 23 12 10 Total number of blood culture sets 19 855 12 991 11 691 38 466 83 624 184 985 125 577 7 859 15 618 4 879 82 521 158 902 46 040 95 017 Number of blood culture sets per 1000 patient days 7.5 37.6 10.7 14.7 7.8 47.8 26.8 6.2 6.1 12.4 21.6 50.7 24.2 45.2
* Number of hospitals served by laboratories reporting denominator data.
17
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
considerably between the reporting countries. This does not necessarily reflect different distributions of the origin of EARS-Net blood cultures per country, because not all hospitals contribute evenly to the EARS-Net database. On the other hand, this diversity can indicate differences in case-mix, which may confound comparison of AMR results between countries. The type of hospital and the size of hospital are not always linked and it is not rare, especially in small countries, that university hospitals have less than 500 beds.
data could have implications on inter-country comparison of both the incidence rate of infections, which could be underestimated in some countries, and of the proportion of resistance. In particular, the proportion of resistance could be overestimated if there is a frequent use of empiric therapy also for invasive infections, and if the cultures are more likely to be performed in patients not responding to the empiric treatment.
4.8 Conclusions
In summary, the situation as assessed from denominator data reported in 2009 is similar to 2008, with only few changes. For future improvement of the denominator data collection and analysis, it is important to address the following issues: increase the number of countries reporting denominator data; increase the number of hospital and laboratories participating within countries; improve the data quality for the variable HospitalId (unique identifier for the hospital within each laboratory); and improve the estimation of the coverage of the EARSNet surveillance, e.g. by using estimations done at the national level based on knowledge of the countryspecific situation.
4.7 Laboratory denominator information
In 2009, the number of blood culture sets processed in the EARS-Net laboratories responding to the questionnaire was 888 025. The median culturing frequency was 18.2 blood culture sets per 1 000 patient days in 2009. The highest rate was reported by Portugal (50.7) and the lowest by Lithuania (6.1). For the majority of the reporting countries, only minor changes in the number of blood culture sets taken per 1 000 patient days (Table 4.3) was observed when comparing 2008 data to 2009. The most significant change was observed for the UK and may originate from the increasing number of reporting hospitals (10 in 2008 and 20 in 2009). The BSIs ascertainment is strongly linked to the blood culture rate. Therefore, the very wide range of culture rate observed in the countries providing denominator
Figure 4.2: Proportion of small, medium and large hospitals per country, based on the number of beds, for all hospital reporting both antimicrobial resistance data and denominator data in 2009
Large hospitals (> 500 beds) Medium hospitals (201500 beds) Small hospitals ( 200 beds)
BG (20/22) CY (5/5) Country codes (responding/all hospitals providing AMR data) DE (47/173) EE (13/14) FR (231/242) HU (62/65) IE (52/71) IT (25/25) LT (22/30) LV (11/12) MT (3/3) PL (30/30) PT (23/25) SI (12/12) UK (50/142) 0 20 40 60 80 100
Proportion of hospitals
18
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
5 Antimicrobial resistance in Europe
5.1 Streptococcus pneumoniae
5.1.1 Clinical and epidemiological importance
Streptococcus pneumoniae is a common cause of disease, especially among young children, elderly people and patients with compromised immune functions. The clinical spectrum ranges from upper airway infections, such as sinusitis, and otitis media to pneumonia and invasive bloodstream infections and meningitis. Since S. pneumoniae is the most common cause of pneumonia worldwide, morbidity and mortality are high and annually approximately 3 million people are estimated to die of pneumococcal infections. Pneumococci carry a variety of virulence factors that facilitate adherence and transcytosis of epithelial cells. The cell wall of pneumococci is coated with a viscous polysaccharide slime layer termed the capsule. This is the most important virulence factor because it protects the bacteria from the adhesion of opsonising antibodies and the destruction by leucocytes. Capsular polysaccharides are highly diverse and play an important role in immune evasion. Around 80 different serotypes have been described. The serotype distribution varies with age, disease and geographical region. Interestingly, serotypes most frequently involved in pneumococcal disease or colonisation in infants are also most frequently associated with antimicrobial resistance. S. pneumoniae two resistance mechanisms against MLS antibiotics have been reported: The acquisition of an erythromycin ribosomal methylation gene (erm) results in a post-transcriptional modification of the 23S subunit of ribosomal RNA, which blocks the binding of the macrolide to the ribosome. Once expression of the gene is induced, this often results in high-level resistance (MICs > 128 mg/L) to macrolide, lincosamines and streptogramin B, termed MLSB resistance. The acquisition of a macrolide efflux system gene (mefE) results in the excretion of the antimicrobial, and effectively reduces intracellular erythromycin, azithromycin and clarithromycin to subinhibitory concentrations. In contrast to beta-lactam resistance, macrolide resistance via these mechanisms (particularly for MLSB ) provides very high MICs, and cannot be overcome by increasing the dosages of antibiotics. Since S. pneumoniae is the most frequent cause of community-acquired pneumonia and cannot clinically be easily distinguished from lower airway infections caused by other pathogens, empirical treatment of community-acquired lower respiratory infections needs to be active against pneumococci and should take the local prevalence of antimicrobial resistance into account. Habitual prescription of non-beta-lactam compounds is therefore typical in countries where penicillin resistance has been frequently reported. Such reactive prescribing increases the selection pressure for alternative antibiotics such as macrolides and novel fluoroquinolones. It is therefore no surprise to see a dynamic antimicrobial resistance picture emerge in different European countries. At the same time, the existence of frequent dual beta-lactam/macrolides resistance, particularly among childrens serotypes, assures that in practice the use of drugs of any of these families will increase resistance for the members of the other one, and so the extended use of macrolides has been considered as a major driver for the increase in beta-lactam resistance. Even though a certain small decrease in penicillin resistance was detected in some countries before the introduction of the PCV7 vaccine, the widespread use of this vaccine is probably an important factor that may have influenced the decrease in antibiotic resistance levels, eliminating the infections (and more importantly, the childrens carriage) of frequent classic resistant serotypes, 14, 6B, 19F and 23F, all of them covered by PCV7. The distribution of serotypes detected in this 2009 report (almost identical to that of 2008) includes serotypes 1 (15%), 19A (12%), 7F (11%), 3 (8%), 12F (7%), 6A (6%), 14 (5%). Even though a limited number of countries have provided serotyping data, ad hoc studies in other EU countries, like France, Spain, Greece, Norway
5.1.2 Resistance mechanisms
Beta-lactam antibiotics bind to cell wall synthesising enzymes, so called penicillin-binding proteins (PBPs) and interfere with the biosynthesis and remodelling of the bacterial cell wall during cell growth and division. The mechanism of penicillin resistance in S. pneumoniae consists of alterations in PBPs, which results in reduced affinity to this class of antibiotics. Alterations in PBPs occur in a stepwise fashion that causes different degrees of resistance proceeding from reduced susceptibility through low-level clinical resistance conventionally termed intermediate1 (I) to full clinical resistance (R). Although intermediately resistant strains are clearly less susceptible than sensitive strains, in absence of meningitis, infections with these strains are often successfully treated with high doses of penicillin or other beta-lactam compounds. Macrolide, lincosamine and streptogramin (MLS) antibiotics are chemically distinct, but all bind to a ribosomal subunit inhibiting the initiation of mRNA binding and thus act as protein synthesis inhibitors. In
1 Microorganisms are defined as intermediate by a level of antimicrobial activity with uncertain clinical effect. Occasionally, this can be overcome if antibiotics can be administered at a higher dose and/or are concentrated at the infected body site.
19
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
and Portugal, confirm the current generality of this pattern. This shift indicates the effect of the PCV7 vaccine, selecting the non-vaccine serotypes, and more importantly the serotype 19A. In fact the classic diversity pattern of well-adapted types of S. pneumoniae clones in children has been maintained, being these clones disguised under the PCV7-non-covered 19A capsule type. At least 10 non-19A serotypes had a 19A capsular switch. Eventually, the introduction of PCV13 vaccine (covering 19A) will produce a new reduction in antibiotic resistance in S. pneumoniae.
Trends in the 20062009 period have been calculated for 22 countries. No country reported a significant increasing trend (Figure 5.5). Significant decreasing trends have been observed for six countries. In four of these countries the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.5). In 2009, these six countries reported the following proportion of resistance to macrolides: 15% in one case (United Kingdom), 510% in two cases (Netherlands and Norway), 1025% in two cases (Belgium and Italy) and 2550% in one case (France). Dual non-susceptibility (penicillin and macrolides) Twenty-seven countries reported 10 577 isolates tested for penicillin and macrolides. In 2009, 5% of isolates had dual non-susceptibility to these two antibiotic classes. One country (Malta) reported less than 10 isolates (therefore not included in Figure 5.3). Proportion of dual non-susceptibility was: below 1% in seven countries, 15% in seven countries, 510% in three countries, 1025% in seven countries and 2550% in two countries (Figure 5.3, Table 5.1). Trends for 20062009 were calculated for 22 countries. A significant increase was observed for Ireland reporting 12% dual non-susceptibility in 2009. A significant decreasing trend has been observed for Belgium (proportion of dual non-susceptibility in 2009 was < 1%) (Figure 5.6). Serogroups Six countries reported 2 959 S. pneumoniae isolates with identification of the serotype/serogroup (Table5.2). In 2009 data, the serogroup 1 was the most prevalent (16% of total), followed by serogroups 19 and 7 (both 11% of total), serogroup 3 (8%), serogroup 12 (7%) and serogroups 6, 14, 9 and 22 (all at 5%) (Figure 5.7, Table5.2). Dual non-susceptibility has been mainly retrieved in serogroups 14, 19, 6, 9 and 23. Single non-susceptibility to penicillin in serogroups 14, 9, 19 and 6. Single non-susceptibility to macrolides in serogroups 1, 19, 14, 6, 33, 15, 9, 23, 11, 3 and 12 (Figure 5.7, Table 5.2).
5.1.3 Results
Penicillin Twenty-seven countries reported 11 055 isolates of which 828 were non-susceptible to penicillin; 344 of the 828 non-susceptible isolates were identified as resistant. One country did not report (Greece) and one country reported less than 10 isolates (Malta), therefore, no data displayed on the maps. Proportion of non-susceptibility was: below 1% in three countries, 15% in nine countries, 510% in two countries, 1025% in seven countries and 2550% in five countries (Figure 5.1, Table 5.1). Trends in the 20062009 period have been calculated for 22 countries. Three countries (Bulgaria, Ireland and Luxembourg) reported a significant increasing trend with proportions of non-susceptibility to penicillin, which, in 2009, were 37%, 20% and 19%, respectively. In one of these countries, the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.4). Significant decreasing trends have been observed for Belgium2, France and Spain with proportions of non-susceptibility to penicillin of < 1%, 27% and 22%, respectively, in 2009. In two of these countries the trend is significant also when considering only data from laboratories consistently reporting all four years (Figure 5.4). Macrolides Twenty-seven countries reported 10 934 isolates of which 1 469 were non-susceptible to macrolides. One country (Malta) reported less than 10 isolates (no data displayed in maps). Proportion of non-susceptibility was: 15% in seven countries, 510% in four countries, 1025% in 10 countries and 2550% in five countries (Figure 5.2, Table 5.1).
5.1.4 Conclusions
In 2009, the proportion of non-susceptibility to penicillin remained generally stable in Europe with three countries reporting significant increasing trends and other three reporting significant decreasing trends. Fourteen of 26 countries reported proportions of non-susceptibility below 10%. The proportion of non-susceptibility to macrolides declined significantly in six countries while no country reported increasing trends. Nevertheless, 14 countries out of 25 reported proportion of non-susceptibility above 10%.
2 The proportion of Streptococcus pneumoniae non-susceptible to penicillin reported by Belgium dropped from 8% in 2008 to < 1% in 2009. This is largely due to the fact that the clinical breakpoints (CLSI) used to determine SIR have changed. The laboratory that performs all the susceptibility tests started using the new CLSI clinical breakpoints in the beginning of 2009. During the entire EARS-Net surveillance, the same method of susceptibility testing has been used, only clinical breakpoints have changed.
20
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
The dual non-susceptibility to penicillin and macrolides was above 10% in eight countries out of 25 countries reporting more than 10 isolates. The highest proportions of non-susceptibility of S. pneumoniae to penicillin and/or macrolides were reported by countries of southern and eastern Europe, with Finland as the only northern exception. So far, the serogroup data reported to EARS-Net should not be regarded as representative for Europe in general; only six countries reported more than 30 isolates with serogroup information and more than 60% of results were provided by Belgium. The serogroup distribution reported in 2009 is similar to the previous year. Most non-susceptible isolates belong to few serogroups, especially serogroups 1, 19, 14, 6 and 9. The serogroup 14, which is particularly important in relation to penicillin resistance, was the most frequent serogroup only in Ireland (12%) (Figure 5.7, Table 5.2).
Figure 5.1: Streptococcus pneumoniae: proportion of invasive isolates non-susceptible to penicillin (PNSP) in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
21
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.2: Streptococcus pneumoniae: proportion of invasive isolates non-susceptible to macrolides in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Figure 5.3: Streptococcus pneumoniae: proportion of invasive isolates with dual non-susceptibility to penicillin and macrolides in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
22
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.4: Streptococcus pneumoniae: trend of penicillin non-susceptibility by country, 20062009
IS
BE (<)
2006 2007 2008 2009
EE
NL
NO
DE
UK
SE
DK
CZ
AT Country code
IT
LT
HU
FI
SI
PT
LU (>*)
IE (>*)
ES (<)
FR (<*)
BG (>) 0 5 10 15 20 % penicilllin non-susceptibility
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
25
30
35
40
23
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.5: Streptococcus pneumoniae: trend of macrolides non-susceptibility by country, 20062009
EE
IS
2006 2007 2008 2009
SE
DK
UK (<)
CZ
NL (<*)
NO (<)
LT
DE
AT Country code
LU
IE
SI
HU
ES
IT (<*)
PT
BE (<)
BG
FR (<)
FI 0 5 10 15 20 25 30 35 40
% macrolides non-susceptibility
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
24
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.6: Streptococcus pneumoniae: trend of dual non-susceptibility (penicillin and macrolides) by country, 20062009
EE*
IS
2006 2007 2008 2009
BE (<)
SE
NL
DE
DK
CZ
NO
UK
AT Country code
LT
IT
LU
HU
SI
FI
ES
PT
IE (>)
BG
FR 0 5 10 15 % Dual non-susceptibility
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. * 0% resistance for all four years.
20
25
30
25
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Table 5.1: Number of invasive S. pneumoniae isolates and proportion of penicillin-non-susceptible (PNSP), penicillinresistant (PRSP), macrolide non-susceptible (MNSP), single penicillin (PEN), single macrolides (MACR) and dual non-susceptible (DUAL) isolates, including 95% confidence intervals (95% CI), reported per country in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic Denmark Estonia Finland France Germany Hungary Iceland Ireland Italy Latvia Lithuania Luxembourg Malta Netherlands Norway Poland Portugal Romania Slovenia Spain Sweden United Kingdom Number of isolates tested for (PEN/ MACR/both) 352/319/294 1 885/1 885/1 885 27/26/26 11/11/11 297/297/297 996/996/996 82/63/63 652/679/643 826/826/826 328/339/323 143/134/134 35/35/35 356/336/336 202/191/178 30/30/30 46/44/44 64/61/59 7/8/7 572/679/505 554/545/545 68/62/62 237/237/237 17/16/16 213/213/213 708/697/697 1 058/1 008/1 005 1 300/1 252/1 166 %PNSP (95%CI) 4.5 (37) 0.3 (01) 37.0 (1958) 36.4 (1169) 4.4 (27) 3.5 (25) 1.2 (07) 12.9 (1016) 26.8 (2430) 2.4 (15) 11.9 (718) 0.0 (010) 19.9 (1624) 5.9 (310) 0.0 (012) 8.7 (221) 18.8 (1030) 14.3 (058) 1.4 (13) 2.2 (14) 29.8 (1843) 18.1 (1324) 29.4 (1056) 17.4 (1323) 22.0 (1925) 3.3 (25) 2.8 (24) %PRSP (95%CI) 2.6 (15) 0.2 (01) 22.2 (942) 18.2 (252) 0.7 (02) 0.7 (01) 0.0 (04) 1.7 (13) 5.9 (48) 0.6 (02) 2.8 (17) 0.0 (010) 6.2 (49) 3.0 (16) 0.0 (012) 6.5 (118) 10.9 (521) 0.0 (041) 0.2 (01) 0.4 (01) 29.8 (1843) 18.1 (1324) 11.8 (136) 1.4 (04) 8.3 (611) 2.5 (24) 1.0 (12) %MNSP (95%CI) 13.8 (1018) 23.1 (2125) 26.9 (1248) 36.4 (1169) 4.7 (38) 4.2 (36) 1.6 (09) 27.7 (2431) 27.0 (2430) 8.3 (612) 19.4 (1327) 2.9 (015) 17.3 (1322) 21.5 (1628) 3.3 (017) 6.8 (119) 16.4 (828) 12.5 (053) 5.0 (37) 5.7 (48) 16.1 (827) 22.4 (1728) 25.0 (752) 17.8 (1324) 19.4 (1623) 4.1 (35) 4.2 (35) %single PEN (95%CI) 2.7 (15) 0.1 (00) 23.1 (944) 9.1 (041) 3.0 (16) 2.9 (24) 1.6 (09) 2.8 (24) 3.5 (25) 1.5 (14) 5.2 (210) 0.0 (010) 7.7 (511) 1.7 (05) 0.0 (012) 6.8 (119) 6.8 (216) 0.0 (041) 0.6 (02) 0.9 (02) 8.8 (318) 7.2 (411) 6.3 (030) 10.8 (716) 11.8 (914) 2.8 (24) 1.5 (12) %single MACR (95%CI) 12.9 (917) 23.0 (2125) 11.5 (230) 9.1 (041) 3.4 (26) 3.2 (25) 1.6 (09) 17.9 (1521) 3.8 (35) 7.4 (511) 14.2 (921) 2.9 (015) 5.4 (38) 16.3 (1123) 3.3 (017) 4.5 (115) 11.9 (523) 0.0 (041) 4.8 (37) 4.4 (36) 1.5 (08) 11.4 (816) 0.0 (021) 11.3 (716) 9.2 (712) 3.5 (25) 2.7 (24) %DUAL (95%CI)* 1.7 (14) 0.2 (00) 15.4 (435) 27.3 (661) 1.3 (03) 1.0 (02) 0.0 (06) 10.0 (813) 23.2 (2026) 0.9 (03) 5.2 (210) 0.0 (010) 11.9 (916) 3.9 (28) 0.0 (012) 2.3 (012) 5.1 (114) 14.3 (058) 0.6 (02) 1.3 (13) 14.7 (725) 11.0 (716) 25.0 (752) 6.6 (411) 10.2 (813) 0.6 (01) 1.4 (12)
* Dual non-susceptibility defined as being non-susceptible to penicillin and macrolides.
Table 5.2: Distribution of single penicillin, single macrolides and dual penicillin-macrolides non-susceptibility, among the most common serogroups reported per country in 2009
Belgium % single MACR % single PEN Serogroups Czech Republic % single MACR % single PEN Iceland % single MACR % single PEN Ireland % single MACR % single PEN Slovenia % single MACR % single PEN United Kingdom % single MACR 0 0 0 0 6 0 0 9 0 8 0 64 0 0 7 0 0 0 11 0 5 % single PEN
% DUAL
% DUAL
% DUAL
% DUAL
% DUAL
1 3 4 5 6 7 8 9 10 11 12 14 15 18 19 20 22 23 33 other Total/ average
368 125 42 115 71 202 42 49 40 24 193 37 38 16 201 5 88 49 36 139 1 880
0 0 0 0 0 0 0 0 0 0 0 0 0 0 1 0 0 0 0 0 0
48 1 0 1 30 0 2 22 3 17 2 65 39 0 64 0 0 20 64 9 23
0 0 0 0 1 0 0 0 0 0 0 3 0 0 0 0 0 0 0 0 0
28 24 20 0 18 24 14 28 11 2 0 26 3 6 16 3 7 23 1 12 266
0 0 0 0 0 0 0 25 0 0 0 4 0 0 6 0 0 0 0 0 3
0 4 5 0 6 0 0 4 0 0 0 8 0 0 25 0 0 0 0 0 4
0 0 0 0 0 0 0 0 0 0 0 12 0 0 0 0 0 4 0 0 2
1 1 0 0 3 4 0 9 0 1 0 6 0 0 4 1 0 2 1 0 33
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0
0 0 0 0 0 0 0 0 0 0 0 17 0 0 0 0 0 0 0 0 3
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0
13 18 11 1 22 32 9 20 1 5 4 33 11 16 32 3 15 20 7 10 283
0 0 0 0 5 0 0 15 0 0 0 27 0 13 6 0 0 0 0 20 7
0 6 0 0 5 3 0 0 0 20 0 36 9 0 3 0 0 0 0 0 6
0 0 0 0 45 0 0 20 0 0 0 24 0 0 28 0 0 5 0 10 12
25 33 9 1 16 9 1 21 2 3 1 28 3 5 21 0 2 11 6 9 206
4 0 0 0 13 0 0 29 0 0 0 21 0 0 29 0 0 0 0 0 10
0 0 0 0 13 0 0 5 0 0 0 61 0 0 5 0 0 9 17 11 12
0 0 0 0 13 0 0 0 0 0 0 18 0 0 24 0 0 9 0 11 7
28 23 6 0 18 41 26 11 2 13 7 11 7 1 41 0 25 8 9 14 291
0 4 0 0 0 0 4 0 0 0 0 0 0 0 2 0 4 13 0 7 2
Only countries reporting more that 30 isolates were presented.
26
% DUAL 0 0 0 0 0 0 4 0 0 0 0 9 14 0 0 0 0 0 0 0 1
Number
Number
Number
Number
Number
Number
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.7: Distribution of serogroups and the resistance profile of S. pneumoniae isolates per serogroup in 2009
1 19 7 3 12 6 14 9 Serogroups 22 5 23 8 4 15 33 10 11 18 20 Other 0 2 4 6 8 Proportion 10 12 14 16
Fully susceptible* Single macrolides non-susceptible Dual non-susceptible** Single penicillin non-susceptible
Only countries that reported serogroup information for more than 30 isolates were included in the figure. * Susceptible to at least penicillin and macrolides. ** Non-susceptible to penicillin and macrolides.
27
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
5.2 Staphylococcus aureus
5.2.1 Clinical and epidemiological importance
Staphylococcus aureus is a gram-positive bacterium that colonises the skin of about 30% of healthy humans. Although mainly a harmless coloniser, S. aureus can cause severe infection. Its oxacillin-resistant form (meticillin-resistant S. aureus, MRSA) is the most important cause of antibiotic-resistant healthcare-associated infections worldwide. Since healthcare-associated MRSA infections add to the number of infections caused by meticillin-susceptible S. aureus, a high incidence of MRSA adds to the overall burden of infections caused by this species in hospitals. Moreover, infections with MRSA may result in prolonged hospital stay and in higher mortality rates, owing mainly to the increased toxicity and limited effectiveness of alternative treatment regimens. MRSA is currently the most commonly identified antibiotic-resistant pathogen in hospitals in many parts of the world, including Europe, the Americas, North Africa and the Middle- and Far East.
One country (Czech Republic) reported a significant increasing trend of MRSA proportion (Figure 5.9) which, in 2009, was 15%. Rifampin Twenty-five countries reported 21 190 isolates of which 203 were identified as resistant to rifampin. Seventeen countries reported at least one resistant isolate. Most resistant isolates (159) were also MRSA. The proportion of rifampin resistance was 3.7% among the MRSA isolates and 0.3% among the MSSA isolates. Proportion of resistance was: below 1% in 17 countries, 15% in six countries, 510% in one country, 1025% in one country (Table 5.3).
5.2.4 Conclusions
The proportion of MRSA is stabilising or decreasing in most European countries. Eight countries reported decreasing trends while only one reported an increasing trend. The countries showing a more evident and sustained decrease of MRSA proportion are: Austria, France, Ireland, Latvia and UK. Although these signals provide reasons for optimism, MRSA should remain a public health priority, since the proportion of MRSA is still above 25% in 10 out of 28 countries, mainly in southern Europe and on the British Isles. The occurrence of resistance to rifampin, which is recommended in combination with other antimicrobials to treat various staphylococcal infections, is still very low in most European countries.
5.2.2 Resistance mechanisms
S. aureus acquires resistance to meticillin and all other beta-lactam antibiotics through expression of the exogenous mecA gene, that codes for a variant penicillin binding protein PBP2 (PBP2a) with low affinity to betalactams, thus preventing the drug induced inhibition of cell wall synthesis. The level of meticillin resistance, defined by its MIC, depends on the amount of PBP2 production, which is influenced by various genetic factors. Resistance levels of mecA-positive strains can thus range from phenotypically susceptible to highly resistant. Upon challenge with meticillin, a population of a heterogeneously resistant MRSA strain may quickly be outgrown by a subpopulation of highly resistant variants.
5.2.3 Results
Beta-lactams Twenty-eight countries reported 30 680 isolates of which 5 965 were identified as meticillin-resistant Staphylococcus aureus (MRSA). Proportion of MRSA was: below 1% in two countries, 15% in five countries, 510% in two countries, 1025% in nine countries, 2550% in nine countries and above 50% in one country (Figure 5.8, Table 5.3). Trends in the 20062009 period have been calculated for 28 countries. Significant decreasing trends have been observed for eight countries. In six of these countries the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.9). In 2009, these eight countries reported the following proportion of MRSA: 510% in two cases (Austria and Latvia), 1025% in two cases (Bulgaria and France) and 2550% in four cases (Greece, Ireland, Romania and UK).
28
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.8: Staphylococcus aureus: proportion of invasive isolates resistant to meticillin (MRSA) in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Table 5.3: Number of invasive S. aureus isolates and proportion resistant to meticillin (MRSA) and rifampin (RIF), including 95% confidence intervals (95% CI), reported per country in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic Denmark Estonia Finland France Germany Greece Hungary Iceland Ireland Italy Latvia Lithuania Luxembourg Malta Netherlands Norway Poland Portugal Romania Slovenia Spain Sweden United Kingdom Meticillin N 1 739 949 221 89 1 695 1 395 213 978 4 720 1 885 996 1 068 59 1 261 978 186 254 113 86 1 035 907 506 1 824 45 424 1 715 2 456 2 883 Rifampin N 1 677 0 137 89 716 1 395 63 934 4 519 1 152 0 287 0 1 051 908 159 164 72 86 861 262 259 828 45 395 1 614 1 608 1 909
% MRSA (95%CI) 6.3 (58) 21.1 (1924) 15.8 (1121) 32.6 (2343) 14.6 (1316) 2.1 (13) 3.3 (17) 1.9 (13) 22.8 (2224) 18.5 (1720) 40.4 (3743) 29.0 (2632) 0.0 (06) 26.8 (2429) 37.4 (3441) 9.1 (514) 11.0 (716) 13.3 (821) 58.1 (4769) 1.0 (02) 0.3 (01) 20.2 (1724) 49.1 (4751) 35.6 (2251) 10.1 (713) 25.9 (2428) 1.0 (11) 27.8 (2629)
% RIF (95%CI) 0.2 (01) 2.9 (17) 0.0 (04) 1.3 (12) 0.1 (01) 0.0 (06) 0.0 (00) 1.2 (12) 0.5 (01) 2.4 (15) 0.4 (01) 5.5 (47) 0.6 (03) 0.0 (02) 0.0 (05) 0.0 (04) 0.0 (00) 0.0 (01) 1.2 (03) 3.5 (25) 15.6 (629) 0.5 (02) 0.5 (01) 0.1 (00) 0.6 (01)
29
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.9: Staphylococcus aureus: trend of meticillin-resistance (MRSA) by country, 20062009
IS NO SE NL FI DK EE AT (<) LV (<) SI LT LU CZ (>) BG (<*) DE PL BE FR (<) ES IE (<) UK (<) HU CY RO (<*) IT EL (<) PT MT 0 10 20 30 40 % MRSA 50 60 70
2006 2007 2008 2009
Country code
80
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
30
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
5.3 Enterococci
5.3.1 Clinical and epidemiological importance
Enterococci belong to the normal bacterial flora of the gastrointestinal tract of humans, other mammals, birds and reptiles. Enterococci are regarded harmless commensals, and are even believed to have positive effects on a number of gastrointestinal and systemic conditions. However, when the commensal relationship with the host is disrupted, enterococci can cause invasive diseases. Recently, the recognition of high risk clones as those of the polyclonal subcluster CC17 in Enterococcus faecium, suggests that some particular strains can act as true pathogens, and not only as opportunistic commensals. Enterococci can cause a variety of clinical syndromes, including endocarditis, bacteraemia, meningitis, wound and urinary tract infections and are associated with peritonitis and intra-abdominal abscesses. In the United States, three to four nosocomial bloodstream infections per 10 000 hospital discharges are caused by enterococci, and contribute to patient mortality as well as additional hospital stay. The vast majority (around 80%) of clinical enterococcal infections in humans are caused by Enterococcus faecalis, whereas E. faecium accounts for the majority of the remaining 20%. Epidemiological data collected over the last two decades have documented the emergence of enterococci, and in particular E. faecium, as important nosocomial pathogens, which is seen as the expansion of a major hospital adapted polyclonal subcluster CC17, but also in E. faecalis CC2 and CC9, which are also isolated from farm animals. The emergence of particular clones and clonal complexes of E. faecalis and E. faecium was paralleled by increases in glycopeptide and high-level aminoglycoside resistance. These two antimicrobial groups represent the few remaining therapeutic options for treatment of human infections caused by E. faecium when resistance has emerged against penicillins. Besides the fact that infections caused by resistant enterococci are difficult to treat, they are highly tenacious and thus easily disseminate in the hospital setting.
the first choice for treatment of infections caused by this microorganism is still an aminopenicillin such as ampicillin. In E. faecium, ampicillin-resistance has increased significantly during the last years due to the wide dissemination of ampicillin-resistant strains belonging to the polyclonal subcluster CC17. Aminoglycosides In addition to the intrinsic mechanism of low-level resistance, which causes a low uptake of the drug, enterococci have acquired genes conferring high-level resistance to aminoglycosides. High-level resistance to streptomycin can be mediated by single mutations within a protein of the 30S ribosomal subunit, the target of aminoglycoside activity. In addition, different aminoglycoside-modifying enzymes have been identified, targeting eight different aminoglycosides. Glycopeptides Vancomycin resistance in enterococci was first encountered in France and England but showed the most dramatic increase in the United States and was attributed to the widespread use of vancomycin in US hospitals. Whereas vancomycin consumption was less pronounced in Europe, a closely related glycopeptide, avoparcin, was widely used as growth promoter in animal husbandry from the late-1970s until it was banned in the EU by 1998. Glycopeptide resistance is due to the synthesis of modified cell wall precursors that show a decreased affinity for glycopeptides. Five phenotypes have been identified of which two have clinical relevance: VanA, with high-level resistance to both vancomycin and teicoplanin; and VanB, with a variable level of resistance to only vancomycin. The VanA and VanB phenotypes, mostly found among E. faecalis and E. faecium, may be transferred by plasmids and conjugative transposition.
5.3.3 Results E. faecalis
High-level aminoglycosides Twenty-six countries reported 6 950 isolates of which 2 484 were high-level resistant to aminoglycosides. Three countries reported resistance proportions above 50% (Cyprus, Greece and Hungary), and the majority of countries (18 of 26) reported resistant proportions between 50% and 30%. Among five countries reporting proportions below 30%, the lowest proportions were reported by Sweden (18.6%), France (18.0%) and Iceland (15.4%) (Figure 5.10 and Table 5.4). Nineteen of 26 countries reported more than 20 isolates per year since 2006 and were included in the trend analysis for the period 20062009. During the past four years, a significant increase was observed for three of 19 countries. Only for Cyprus, the increasing trend was significant, when considering data from laboratories reporting consistently for all four years (Figure 5.11). Two countries (Germany and Ireland) reported significant decreasing trends of high-level aminoglycosides resistance. The decreasing trend was significant only for Ireland when considering data from laboratories reporting consistently for all four years (Figure 5.11).
5.3.2 Resistance mechanisms
Enterococci are intrinsically resistant to a broad range of antibiotics including cephalosporins, sulphonamides and low concentrations of aminoglycosides. Patient safety in hospitals is challenged by the ability of enterococci to acquire additional resistance through the transfer of plasmids and transposons and recombination or mutation. Beta-lactam antibiotics By nature, enterococci have low susceptibility to many beta-lactam antibiotics a consequence of their low-affinity PBPs. Two possible mechanisms of resistance of enterococci to beta-lactams have been reported: the production of beta-lactamase, which is an extremely rare finding; and the overproduction and modification of penicillin-binding proteins (PBPs, particularly PBP5) that causes high-level penicillin resistance in E. faecium. Complete penicillin resistance in E. faecalis is currently absent; therefore,
31
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
5.3.4 Results E. faecium
Vancomycin Twenty-eight countries reported 4 945 isolates of which 451 were resistant to vancomycin. Only two countries (Malta and Romania) reported less than 10 isolates (thus not shown in Figure 5.12). Three countries reported resistance proportions above 25% (Ireland, Luxembourg and Greece) and five countries reported resistant proportions between 10% and 25%, while the majority of countries (18 of 26) reported resistant proportions below 10%. Several countries reported even below 1% (Bulgaria, Estonia, Finland, France, Norway, Romania and Sweden) (Figure5.12 and Table 5.4). Nineteen of 28 countries reported more than 20 isolates per year since 2006 and were included in the trend analysis for the period 20062009. During the past four years, a significant increase was observed only for Austria; however, the increasing trend was not significant when considering data from laboratories reporting consistently for all four years (Figure5.13). Four countries (Greece, Germany, Italy and France) reported significant decreasing trends of vancomycin resistance. Considering data from laboratories reporting consistently for all four years, the decreasing trend was significant for Greece and Italy (Figure 5.13).
5.3.5 Conclusions
High-level aminoglycoside resistance in E. faecalis seems stable in Europe but at a relatively high level. The majority of countries reported proportions of resistant isolates between 30% and 50%, however, a consistent decrease was reported by Germany and Ireland. The occurrence of vancomycin resistance in E. faecium seems also to stabilise in Europe, although fluctuations may arise from hospitals outbreaks, e.g. related to the continuing dissemination of strains belonging to the polyclonal subcluster CC17. This may, however, not reflect the overall trend or the situation in hospitals, which have remained unaffected. In some countries (Greece, Germany, Italy and France) the efforts to control glycopeptide-resistant enterococci seem to be successful and resulting in a continuous decrease of proportions of resistant isolates, and several countries reported resistant proportions below 1%.
Figure 5.10: Enterococcus faecalis: proportion of invasive isolates with high-level resistance to aminoglycosides in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
32
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.11: Enterococcus faecalis: trends of high-level aminoglycoside resistance by country, 20062009
FR
SE
2006 2007 2008 2009
BE
NL
AT
IE (<)
PT
NO
BG
Country code
UK
DE (<*)
ES (>*)
EE
SI
CZ
IT (>*)
HU
EL
CY (>) 0 10 20 40 50 60 70 80
30
% aminoglycoside high-level resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
33
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.12: Enterococcus faecium: proportion of invasive isolates resistant to vancomycin in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Table 5.4: Number of invasive E. faecalis and E. faecium isolates and proportion of highlevel aminoglycoside resistant E. faecalis and vancomycinresistant E. faecium (%R), including 95% confidence intervals (95% CI), reported per country in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic Denmark Estonia Finland France Germany Greece Hungary Iceland Ireland Italy Latvia Lithuania Luxembourg Malta Netherlands Norway Poland Portugal Romania Slovenia Spain Sweden United Kingdom High-level aminoglycoside resistant E. faecalis N % R (95% CI) 252 31.0 (2537) 150 23.3 (1731) 53 35.8 (2350) 65 66.2 (5377) 626 46.8 (4351) 52 32.7 (2047) 23 43.5 (2366) 0 1 298 18.0 (1620) 450 39.6 (3544) 547 61.2 (5765) 368 50.5 (4556) 26 15.4 (435) 260 34.2 (2840) 136 49.3 (4158) 26 38.5 (2059) 31 48.4 (3067) 32 28.1 (1447) 0 190 30.5 (2438) 252 35.7 (3042) 163 38.7 (3147) 420 34.3 (3039) 17 35.3 (1462) 115 44.3 (3554) 735 42.9 (3947) 597 18.6 (1622) 66 37.9 (2651) Vancomycin-resistant E. faecium N % R (95% CI) 310 4.2 (27) 67 4.5 (113) 26 0.0 (013) 15 13.3 (240) 209 5.7 (310) 348 1.7 (14) 40 0.0 (09) 243 0.0 (02) 591 0.8 (02) 408 6.1 (49) 435 26.9 (2331) 76 1.3 (07) 25 8.0 (126) 386 37.8 (3343) 188 4.3 (28) 22 18.2 (540) 19 10.5 (133) 14 35.7 (1365) 6 0.0 (046) 207 1.0 (03) 101 0.0 (04) 85 1.2 (06) 217 22.6 (1729) 9 0.0 (034) 69 4.3 (112) 342 2.6 (15) 221 0.5 (02) 266 12.8 (917)
34
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.13: Enterococcus faecium: trends of vancomycin resistance by country 20062009
EE
NO**
2006 2007 2008 2009
FI
SE
FR (<*)
NL
HU
DK
ES
Country code
AT (>*)
SI
IT (<)
BE
CZ
DE (<*)
UK
PT
EL (<)
IE 0 10 20 30 40 50
% vancomycin resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years. ** 0% resistance for all four years.
35
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
5.4 Escherichia coli
5.4.1 Clinical and epidemiological importance
Escherichia coli is the most frequent gram-negative rod isolated from blood cultures in clinical settings. It is the most frequent cause of bacteremia, community and hospital-acquired urinary tract infections, is associated with spontaneous and surgical peritonitis and with skin and soft tissue infections due to multiple microorganisms, causes neonatal meningitis and is one of the most important foodborne pathogens worldwide.
5.4.2 Resistance mechanisms
Beta-lactamases hydrolyse the beta-lactam ring of betalactam antibiotics, which is crucial for inhibition of PBPs in bacteria. In E. coli, resistance to broad-spectrum penicillins such as ampicillin or amoxicillin is usually conferred by plasmid coded beta-lactamases mainly of the TEM type and to a lesser extend of the SHV type, whereby TEM-1 accounts for up to 60% of aminopenicillin resistance. In 1982 the first ESBL was identified during a hospital outbreak of Klebsiella pneumoniae in Germany. It was soon understood that single or multiple amino acid substitutions in the basic structure of SHV or TEM enzymes can alter their spectrum of activity and enhance their hydrolysing ability to include thirdgeneration cephalosporins (in this report referring to: cefotaxime, ceftriaxone, ceftazidime) and monobactams. Most ESBLs can be inhibited by beta-lactamase inhibitors such as clavulanic acid, sulbactam or tazobactam. More than 200 ESBL variants are known to date. Most of them belong to four enzyme families TEM, SHV, CTX-M and OXA (an overview of identified ESBL types is given on http://www.lahey.org/studies/). Until 2000, over 90% of ESBL resistance was mediated through TEM or VHS variants. In the late 1980s, new ESBLs of the CTX-M family emerged first in South America and, during early 2000s, attained global importance. In contrast to conventional TEM, and SHV ESBLs, most CTX-Ms display a higher hydrolysing ability against cefotaxime than ceftazidime (hence their name). An important part of this global success is due to the wide dissemination of particular plasmids or bacterial clones producing ESBL (e.g. CTX-M15). Other enzymes affecting the susceptibility to third-generation cephalosporins include plasmid encoded variants from the chromosomal AmpC betalactamases. CMY-2 is the most widespread enzyme belonging to this group, which is still less common in E. coli in Europe but frequent in the United States. An important threat that will require close surveillance in the future is the development of carbapenem-resistance in E coli, mediated by metallo-beta-lactamases (as VIM or IMP enzymes, or the emerging NDM enzyme) and serin-beta-lactamases (as KPC enzymes), providing resistance to virtually all available beta-lactam agents. Fluoroquinolones interact with DNA gyrase and topoisomerase IV, which are enzymes that regulate conformational changes in the bacterial chromosome
during replication and transcription. This interaction leads to irreversible inhibition of the enzyme activity followed by DNA fragmentation and eventually to cell death. Resistance to fluoroquinolones arises through stepwise mutations in the coding regions of the gyrase subunits (gyrA and gyrB) and DNA topoisomerase IV (parC). Accumulation of mutations in several of these genes increases the MIC in a stepwise manner. Low-level resistance to fluoroquinolones may also arise through changes in outer membrane porins or from upregulation of efflux pumps, resulting in lower outer membrane permeability and higher efflux, respectively. In recent years, several plasmid-mediated quinolone resistance mechanisms have also been identified, including the Qnr proteins, which protect DNA topoisomerases from quinolone binding, the AAC6-Ib-cr enzyme, which inactivates some fluoroquinolones by acetylation, and the QepA efflux pump, which effluxes hydrophilic quinolones. These mechansims are of concern because of transferability and their frequent association with CTX-M and CMY-type enzymes inactivating third-generation cephalosporins. Aminoglycosides block protein synthesis by binding to the ribosomes, which are involved in the translation of RNA into proteins, and are also able to damage the outer membrane of gram-negative rods. Resistance to aminoglycosides can be due to targeted modification (methylation) of the large ribosomal subunit, which excludes aminoglycoside molecules, or by aminoglycoside modifying enzymes that acetylate, adenylate or phosphorylate their target molecules and thereby neutralise the biologic effect of aminoglycosides.
5.4.3 Results
Aminopenicillins Twenty-eight countries reported 47 318 isolates of which 25 254 were resistant to aminopenicillins. The majority of countries (19 of 28) reported resistance proportions from 50% to 66.5%. Among nine countries reporting proportions below 50%, the lowest proportions were reported by Sweden (33.2 %), Finland (36.4%) and Norway (37.2 %) (Table 5.5). Trends for the period 20062009 were calculated for 28 countries. During the past four years, a significant increase was observed in 10 of 28 countries. In seven of these countries, the trends were significant also when considering only data from laboratories reporting consistently for all four years (Figure 5.17). Among the 10 countries with increasing trends, four countries reported proportion of resistance to aminopenicillin higher than 60% even though these countries were already at relatively high levels, five countries reported between 60% and 50%, and one country reported below 50%. Two countries (Austria and Estonia) reported significant decreasing trends of resistance to aminopenicillin, although both countries were already at relatively low levels (Figure 5.17).
36
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Third-generation cephalosporins Twenty-eight countries reported 49 720 isolates of which 3 657 were resistant to third-generation cephalosporins. Nine of 28 countries reported third-generation cephalosporins resistance higher than 10% and the proportions ranged up to 19.2%. Among the 19 countries reporting less than 10% resistance, the lowest proportions were reported by Iceland (1.8%), Estonia (2.2%) and Norway (2.3%) (Table 5.5 and Figure 5.14). Trends for the period the 20062009 were calculated for 28 countries. During the past four years, a significant increase was observed in more than half (16 of 28) of the countries. In 15 of these, the trends were significant also when considering only data from laboratories reporting consistently for all four years (Figure 5.18). Among the 16 countries with increasing trends for 20062009, five countries reported proportions of resistance to third-generation cephalosporins above 10%, nine countries reported between 10% and 5%, and two countries reported below 5%. Only one country reported a decreasing trend in resistance to third-generation cephalosporins, however the trend was not significant when considering only data from laboratories reporting consistently for all four years. Extended-spectrum beta-lactamase (ESBL) Among E. coli isolates resistant to third-generation cephalosporins, a large proportion has been ascertained as ESBL positive by the participating laboratories in 2009. Twelve of 13 countries reported proportions of ESBL production between 85% and 100% among isolates resistant to third-generation cephalosporins (Table 5.6). Fluoroquinolones Twenty-eight countries reported 48 054 isolates of which 9 488 were resistant to fluoroquinolones. The majority of countries (16 of 28) reported resistant proportions higher than 20%, ranging up to 43.4%. Seven countries reported between 20% and 10%. Among five countries reporting below 10%, the lowest proportions of resistant isolated were reported by Iceland (7.1%), Sweden (8.2 %) and Estonia (8.3%) (Table 5.5 and Figure 5.15). Trends in the period 20062009 were calculated for 28 countries. A significant increase was observed for seven countries. In six of these countries the trends were significant also when considering only data from laboratories reporting consistently all four years (Figure 5.19). Among the seven countries with increasing trends for 20062009, two reported proportions of resistance to fluoroquinolones above 30%, two reported between 30% and 20%, and three countries reported below 20%.
Only two countries (Austria and Germany) reported significant decreasing trends in resistance to fluoroquinolones (Figure 5.19). Aminoglycosides Twenty-eight countries reported 50 699 isolates of which 3 983 were resistant to aminoglycosides. Eleven of 28 countries reported proportions of resistance higher than 10%, ranging up to 21.4%. Eleven countries reported between 10% and 5%. Among six countries reporting below 5%, the lowest proportions of resistant isolated were reported by Norway (3.3%), Finland (2.8%) and Sweden (2.5%) (Table 5.5 and Figure 5.16). Trends in the period 20062009 were calculated for 28 countries. A significant increase in the proportion of isolates resistant to aminoglycosides was observed for 10 countries. Among these, five countries reported proportions higher than 10%, one country reported between 10% and 5%, and four countries reported below 5%. For two countries (Austria and Romania) the proportions of resistance to aminoglycosides significantly decreased over the last four years. For Austria, the trend was significant also when considering only data from laboratories consistently reporting for all four years (Figure 5.20). Combined resistance (aminopenicillins, third-generation cephalosporins, fluoroquinolones and aminoglycosides) In 2009, 28 countries reported 42 898 isolates tested for aminopenicillins, third-generation cephalosporins, fluoroquinolones and aminoglycosides. Fifty-seven per cent of these isolates were resistant to one or more of the four considered antibiotic classes. In nine countries, the proportion of multiresistant isolates (resistance to third-generation cephalosporins, fluoroquinolones and aminoglycosides) was higher than 5%, between 5% and 1% in 14 countries, and below 1% in four countries (Table 5.7 and Figure 5.21). Trends in the period 20062009 were calculated for 28 countries. A significant increase in proportions of multiresistant isolates was observed for 12 countries. In 10 of these countries the trends were significant also when considering only data from laboratories reporting consistently for all four years (Figure 5.21). Among the 12 countries with significantly increasing proportions of multiresistant isolates, four countries reported above 5%, eight countries reported between 5% and 1%, whereas no country reported below 1%. No country had a significantly decreasing trend of proportions of multiresistance in E. coli in 20062009. The most frequent resistance phenotypes in E. coli were single aminopenicillin resistance (33.3%), followed by dual resistance to aminopenicillins and fluoroquinolones (8.7%). Combined resistance to all four antimicrobials was reported for 3.3% of the isolates and combined resistance to aminopenicillins,
37
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
fluoroquinolones and aminoglycosides was 3.2% (Table 5.7).
5.4.4 Conclusions
The remarkable and constant Europe-wide decline of antimicrobial susceptibility in E. coli observed during recent years continued in 2009. Resistance in E. coli shows increasing trends in several countries and for both multiresistance and for single antimicrobials under surveillance. The highest proportions of resistance in E. coli were reported for aminopenicillins ranging up to 66.5%. Irrespective of the high level of resistance, proportions continue to increase in several countries, including those already presenting resistance well above 50%. The proportion of third-generation cephalosporins resistance reported for E. coli has increased significantly during the last four years in more than half of the reporting countries. Among isolates resistant to thirdgeneration cephalosporins, a high proportion (85100%) was identified as ESBL positive. These data indicate that ESBL production is highly prevalent in third-generation cephalosporin-resistant E. coli in European hospitals. Fluoroquinolone resistance in E. coli continues the increase as in previous years. Although the number of countries showing an increasing trend over the last four years was reduced compared to 2008, the situation becomes progressively dire and more than half of the countries are reporting resistance proportions higher than 20%. Ten countries had significant increases in the proportion of isolates resistant to aminoglycosides and five of these countries reported proportions higher than 10%. This indicates that aminoglycosides resistance is increasing even among the countries already reporting higher levels of resistance. The most frequent resistance phenotypes in E. coli were single aminopenicillin resistance (33.3%), followed by dual resistance to aminopenicillins and fluoroquinolones (8.7%). Combined resistance to all four antimicrobials was reported for 3.3% of the isolates and combined resistance to aminopenicillins, fluoroquinolones and aminoglycosides was 3.2%. Resistance to third-generation cephalosporins was associated with resistance to aminoglycosides in almost half of the cases and to fluoroquinolones in approximate 75% of the cases. These results indicate that the loss of antimicrobial susceptibility in E. coli requires close surveillance.
38
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Table 5.5: Number of invasive E. coli isolates and proportion aminopenicillins, third-generation cephalosporins, fluoroquinolones, aminoglycosides and multiresistance (%R), including 95% confidence intervals (95% CI), reported per country in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic Denmark Estonia Finland France Germany Greece Hungary Iceland Ireland Italy Latvia Lithuania Luxembourg Malta Netherlands Norway Poland Portugal Romania Slovenia Spain Sweden United Kingdom Aminopenicillins N %R (95%CI) 2 605 48.6 (4751) 1 607 55.9 (5358) 181 66.3 (5973) 136 66.2 (5874) 2 759 60.6 (5962) 3 531 42.9 (4145) 319 38.2 (3344) 1 906 36.4 (3439) 8 436 55.5 (5457) 2 158 56.1 (5458) 1 694 50.9 (4853) 1 047 59.8 (5763) 109 49.5 (4059) 1 987 66.5 (6469) 764 63.4 (6067) 86 43.0 (3254) 291 58.4 (5364) 298 57.0 (5163) 159 54.7 (4763) 2 359 45.1 (4347) 1 845 37.2 (3539) 487 64.7 (6069) 1 919 58.3 (5661) 12 83.3 (5298) 783 53.8 (5057) 3 821 64.7 (6366) 2 195 33.2 (3135) 3 824 61.6 (6063) Fluoroquinolones N %R (95%CI) 2 616 20.5 (1922) 1 504 19.9 (1822) 193 28.0 (2235) 136 43.4 (3552) 2 758 23.2 (2225) 3 406 13.2 (1214) 302 8.3 (512) 2 223 9.2 (810) 8 353 18.6 (1819) 2 786 23.4 (2225) 1 806 23.4 (2125) 1 046 30.5 (2833) 99 7.1 (314) 2 005 21.7 (2024) 863 36.2 (3339) 85 23.5 (1534) 295 14.6 (1119) 300 25.7 (2131) 159 30.8 (2439) 2 377 11.0 (1012) 1 830 8.7 (710) 567 23.1 (2027) 1 973 27.7 (2630) 53 22.6 (1236) 783 18.9 (1622) 3 810 31.5 (3033) 1 596 8.2 (710) 4 130 18.0 (1719) Third-gen. cephalosporins N %R (95%CI) 2 597 7.5 (79) 1 596 6.5 (58) 193 19.2 (1425) 136 14.0 (921) 2 759 9.8 (911) 2 705 6.2 (57) 319 2.2 (14) 2 176 2.8 (24) 8 449 6.7 (67) 2 759 8.2 (79) 1 815 10.1 (912) 1 052 12.9 (1115) 110 1.8 (06) 1 986 6.5 (58) 687 17.0 (1420) 86 11.6 (620) 293 7.8 (512) 300 8.3 (512) 159 15.1 (1022) 2 368 4.3 (35) 1 846 2.3 (23) 584 9.1 (712) 1 912 9.2 (811) 53 17.0 (830) 783 6.6 (59) 3 821 11.3 (1012) 4 233 2.8 (23) 3 943 9.4 (810) Aminoglycosides N %R (95%CI) 2 619 6.1 (57) 1 195 7.3 (69) 194 18.0 (1324) 136 9.6 (516) 2 742 9.0 (810) 3 530 4.4 (45) 320 3.8 (26) 2 033 2.8 (24) 8 448 8.2 (89) 2 796 8.4 (79) 1 828 14.5 (1316) 1 056 15.9 (1418) 110 7.3 (314) 2 009 8.8 (810) 863 12.5 (1015) 86 12.8 (722) 297 15.2 (1120) 300 9.3 (613) 159 21.4 (1529) 2 389 4.4 (45) 1 841 3.3 (34) 595 7.1 (59) 2 038 10.8 (912) 80 12.5 (622) 783 10.5 (813) 3 820 13.0 (1214) 4 121 2.5 (23) 4 311 7.4 (78) Multiresistance* N %R (95%CI) 2 588 2.2 (23) 1 175 1.6 (13) 192 7.3 (412) 136 5.1 (210) 2 741 3.0 (24) 2 634 1.4 (12) 301 0.7 (02) 1 984 1.5 (12) 8 350 3.0 (33) 2 745 3.2 (34) 1 806 6.4 (58) 1 042 9.8 (812) 99 0.0 (04) 1 976 2.4 (23) 687 5.5 (48) 85 5.9 (213) 291 3.8 (27) 300 4.3 (27) 159 12.6 (819) 2 339 1.4 (12) 1 827 0.7 (01) 546 1.8 (13) 1 885 5.5 (47) 53 15.1 (728) 783 4.6 (36) 3 809 4.5 (45) 1 529 0.7 (01) 3 616 4.0 (35)
* Multiresistance defined as being resistant to third-generation cephalosporins, fluoroquinolones and aminoglycosides.
Table 5.6: Number of invasive E. coli isolates resistant to third-generation cephalosporins (CREC) and proportion of ESBL positive among these isolates, as ascertained by the participating laboratories in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic France Ireland Lithuania Netherlands Poland Portugal Sloveni Spain Number of laboratories 24 4 12 5 42 38 25 8 6 16 15 7 33 Number of CREC 86 14 37 19 270 316 117 23 40 53 122 52 432 %ESBL 94.2 92.9 94.6 100 85.6 64.9 85.5 100 90 89 91.8 92.3 90.7
Only data from laboratories consistently reporting the ESBL test results for all isolates identified as resistant to third-generation cephalosporins and from countries with at least 10 of such isolates were selected for the analysis.
39
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Table 5.7: Overall resistance and resistance combinations among invasive Escherichia coli isolates tested against aminopenicillins, fluoroquinolones, third-generation cephalosporins and aminoglycosides (n= 42 898) in Europe, 2009
Resistance pattern Fully susceptible Single resistance (to indicated drug classes) Aminopenicillins Fluoroquinolones Aminoglycosides Resistance to two classes of antimicrobial drugs Aminopenicillins + fluoroquinolones Aminopenicillins + third-generation cephalosporins Aminopenicillins + aminoglycosides Fluoroquinolones + aminoglycosides Resistance to three classes of antimicrobial drugs Aminopenicillins + fluoroquinolones + aminoglycosides Aminopenicillins + third-generation cephalosporins + fluoroquinolones Aminopenicillins + third-generation cephalosporins + aminoglycosides Resistance to four classes of antimicrobial drugs Aminopenicillins + third-generation cephalosporins + fluoroquinolones + aminoglycosides Number 18 622 14 292 908 86 3 718 640 555 40 1 387 1 123 132 1 395 % of total 43.4 33.3 2.1 0.2 8.7 1.5 1.3 0.1 3.2 2.6 0.3 3.3
Figure 5.14: Escherichia coli: proportion of third-generation cephalosporin resistance in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
40
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.15: Escherichia coli: proportion of invasive isolates with resistance to fluoroquinolones in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Figure 5.16: Escherichia coli: proportion of invasive isolates with resistance to aminoglycosides in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
41
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.17: Escherichia coli: trends of aminopenicillin resistance by country, 20062009
SE (>) FI NO EE (<) DK LV NL AT (<) IS EL (>) SI (>) MT FR (>) Country code BE DE LU (>) PT LT HU (>) CZ (>) UK (>*) IT (>*) ES PL (>*) CY BG IE 0 10 20 30 40 % aminopenicillin resistance 50 60 70
2006 2007 2008 2009
80
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
42
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.18: Escherichia coli: trends of third-generation cephalosporin resistance by country, 20062009
IS EE NO SE (>) FI (>) NL DK (>) IE (>) BE (>) SI (>) FR (>) AT LT DE (>*) LU (>) PL (>) PT UK CZ (>) EL (>) ES (>) LV HU (>) CY MT (>) IT (>) RO (<*) BG 0 10 20 30 40
2006 2007 2008 2009
Country code
50
% third-generation cephalosporins resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
43
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.19: Escherichia coli: trends of fluoroquinolone resistance by country, 20062009
IS SE EE NO (>) FI NL DK (>) LT UK FR (>) SI BE AT (<) IE RO PL (>*) CZ EL (>) DE (<) LV LU PT BG HU MT ES (>) IT (>) CY 0 10 20 30 40
2006 2007 2008 2009
Country code
50
% uoroquinolones resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
44
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.20: Escherichia coli: trends of aminoglycoside resistance by country, 20062009
SE (>) FI NO (>) EE NL (>) DK (>) AT (<) PL BE IS UK FR (>) DE IE CZ LU CY SI (>) PT IT (>) RO (<*) LV ES (>) EL (>) LT HU (>) BG MT 0 10 20 30 40
2006 2007 2008 2009
Country code
50
% aminoglycosides resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
45
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.21: Escherichia coli: trends of combined resistance (resistant to fluoroquinolones, third-generation cephalosporins and aminoglycosides) by country, 20062009
IS EE NO SE DK (>) NL FI BE PL AT IE (>) FR (>) CZ (>) DE (>*) LT UK (>*) LU ES (>) SI (>) CY IT (>) PT LV EL (>) BG HU (>) MT (>) RO 0 5 10 15 % Multiresistance 20 25
2006 2007 2008 2009
Country code
30
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
46
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
5.5 Klebsiella pneumoniae
5.5.1 Clinical and epidemiological importance
Bacteria of the genus Klebsiella are frequent colonisers of the gastrointestinal tract in humans but may also be found on skin, in the oropharynx and upper airways in hospitalised individuals. Klebsiella pneumoniae is associated with opportunistic infections in individuals with impaired immune defences, such as diabetics, alcoholics and hospitalised patients with indwelling devices. The most common sites of infection are the urinary and the respiratory tract. Organisms can spread rapidly, from the gastrointestinal tract of patients and via the hands of hospital personnel to other patients, leading to nosocomial outbreaks. K. pneumoniae is the second most frequent cause of gram-negative bloodstream infections after Escherichia coli. The mortality rates of pneumonia caused by K. pneumoniae can be high even when appropriate antibiotic treatment is given, however, also depends on the severity of the underlying condition.
been observed for nine countries. In eight of these, the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.26). In 2009, the nine countries with increasing trends reported the following proportion of resistance to third-generation cephalosporins: 1025% in three cases (Denmark, Estonia and France), 2550% in three cases (Hungary, Luxembourg and Portugal) and above 50% in three cases (Czech Republic, Greece and Latvia). Two countries (Malta and the United Kingdom) reported significant decreasing trends of proportions of resistance to third-generation cephalosporins (Figure 5.26) which, in 2009, were 0% and 7%, respectively. Extended-spectrum beta-lactamase (ESBL) Sixteen countries have been included in the analysis of ESBL proportion for K. pneumoniae. Only data from laboratories consistently reporting ESBL test results for all isolates identified as resistant to third-generation cephalosporins and from countries with at least 10 of such isolates were selected for the analysis. The proportion of K. pneumoniae isolates resistant to third-generation cephalosporins and ESBL producers, as ascertained by the participating laboratories, ranged between 73% and 100%. Proportion of ESBL producers was: 7080% in three countries, 8090% in four countries and above 90% in nine countries (Table 5.9). Fluoroquinolones Twenty-eight countries reported 11 344 isolates of which 3 203 were resistant to fluoroquinolones. Proportion of resistance was: below 1% in one country, 15% in four countries, 510% in three countries, 1025% in 10 countries, 2550% in eight countries and above 50% in two countries (Figure 5.23, Table5.8). Trends in the 20062009 period have been calculated for 23 countries. A significant increase has been observed for 11 countries. In 10 of these countries the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.27). In 2009, the 11 countries with increasing trends reported the following proportion of resistance to fluoroquinolones: 1025% in four cases (Denmark, Estonia, France and Spain), 2550% in five cases (Bulgaria, Cyprus, Hungary, Lithuania and Portugal) and above 50% in two cases (Czech Republic and Greece). Two countries (Ireland and the United Kingdom) reported significant decreasing trends of proportions of resistance to fluoroquinolones (Figure 5.27) which, in 2009, were 11% and 6%, respectively. Aminoglycosides Twenty-eight countries reported 11 922 isolates of which 2 787 were resistant to aminoglycosides.
5.5.2 Resistance mechanisms
Similar to E. coli, K. pneumoniae can be resistant to multiple antibiotics, and resistance traits are frequently acquired through plasmids. However, in contrast to E. coli, K. pneumoniae has a chromosomally encoded SHV beta-lactamase and is thus intrinsically resistant against aminopenicillins. Moreover, this organism readily acquires plasmid-mediated resistance determinants. Many novel ESBL variants were initially identified in K. pneumoniae and were only subsequently found in E. coli. Since the resistance mechanisms do not significantly differ from those described for E. coli, readers should refer to the E. coli chapter for further details. Carbapenems have been widely used in many countries due to the increasing rate of ESBL-producing Enterobacteriaceae with a consequent impact on the emergence of resistance to these antibiotics, especially in K. pneumoniae. KPC carbapenemase-producing clones of K. pneumoniae have been observed in the United States, Greece and Israel, while plasmids encoding the VIM metallo-carbapenemase are frequent in K. pneumoniae in Greece. Recently, a new type of plasmidic carbapenemase, the New Delhi metallo-beta-lactamase 1 (NDM-1), has been observed in patients returning from the Indian subcontinent.
5.5.3 Results
Third-generation cephalosporins Twenty-eight countries reported 11 665 isolates of which 3 214 were resistant to third-generation cephalosporins. Proportion of resistance was: below 1% in two countries, 15% in three countries, 510% in three countries, 1025% in seven countries, 2550% in seven countries and above 50% in six countries (Figure 5.22, Table 5.8). Trends in the 20062009 period have been calculated for 24 countries. A significant increase has
47
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Proportion of resistance was: below 1% in three countries, 15% in four countries, 510% in five countries, 1025% in seven countries, 2550% in six countries and above 50% in three countries (Figure 5.24, Table 5.8). Trends in the 20062009 period have been calculated for 24 countries. A significant increase has been observed for 11 countries. In 10 of these countries the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.28). In 2009, the 11 countries with increasing trends reported the following proportion of resistance to aminoglycosides: 15% in one case (Norway), 510% in one case (Denmark), 1025% in four cases (Estonia, France, Luxembourg and Portugal), 2550% in three cases (Czech Republic, Hungary and Latvia) and above 50% in two cases (Greece and Lithuania). Two countries (Malta and the United Kingdom) reported significant decreasing trends of proportions of resistance to aminoglycosides (Figure 5.28) which, in 2009, were 0% and 5%, respectively. Combined resistance (third-generation cephalosporins, fluoroquinolones and aminoglycosides) Twenty-eight countries reported 10 952 isolates tested for third-generation cephalosporins, fluoroquinolones and aminoglycosides. In 2009, 35% of isolates were resistant to one or more of the three considered antibiotic classes. The most frequent pattern of resistance was the multiresistance (R to all three antibiotic classes) (19%). More than 90% of the isolates resistant to third-generation cephalosporins were also resistant to either fluoroquinolones or aminoglycosides and two thirds were resistant to both these classes (Table5.10). Proportion of multiresistance was: below 1% in four countries, 15% in six countries, 510% in four countries, 1025% in nine countries, 2550% in four countries and above 50% in one country (Table 5.8). Trends in the 20062009 period have been calculated for 23 countries. A significant increase of multiresistance has been observed for 13 countries. In 10 of these countries the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.29). In 2009, the 13 countries with increasing trends reported the following proportion of multiresistance: below 1% in one case (Sweden), 15% in two cases (Norway and Spain), 510% in two cases (Denmark and Estonia), 1025% in three cases (Latvia, France and Portugal), 2550% in four cases (Bulgaria, Czech Republic, Hungary and Lithuania) and above 50% in one case (Greece). One country (the United Kingdom) reported a significant decreasing trend of proportions of multiresistance (Figure 5.29), which, in 2009, was 3%. Carbapenems Twenty-seven countries reported 10 573 isolates of which 738 were resistant to carbapenems. Most of
the resistant isolates (708) were identified in Greece; other 12 countries reported at least one resistant isolate. Proportion of resistance was: 43.5% in Greece, 17.0% in Cyprus, 1.3% in Italy, 1.2% in Belgium and below 1% in the other 23 reporting countries (Figure 5.25).
5.5.4 Conclusions
The antimicrobial resistance of K. pneumoniae is a worrisome problem in Europe. In 2009, many countries reported high proportions and increasing trends of resistance to third-generation cephalosporins, fluoroquinolones and aminoglycosides. Greece and Cyprus have also reported high proportions of resistance to carbapenems; proportions of resistance to these agents above 1% have been observed so far in Belgium and Italy. Two thirds of the countries reported proportions of resistance to third-generation cephalosporins and fluoroquinolones higher than 10%. Proportions of multiresistance (R to third-generation cephalosporins, fluoroquinolones and aminoglycosides) above 10% have been reported by half of the countries. The majority of isolates resistant to third-generation cephalosporins were resistant also to fluoroquinolones and aminoglycosides. Increasing trends of resistance to specific antibiotic classes and of multiresistance have been observed also in northern European countries, like Denmark and Norway, with a traditionally prudent approach to the antibiotic use. Only the United Kingdom has shown a consistent reduction of resistance proportion of K. pneumoniae for all the antibiotic classes under surveillance. Decreasing trends for specific antibiotic classes were also observed for Ireland and Malta.
48
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.22: Klebsiella pneumoniae: proportion of invasive isolates resistant to third-generation cephalosporins in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Figure 5.23: Klebsiella pneumoniae: proportion of invasive isolates resistant to fluoroquinolones in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
49
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.24: Klebsiella pneumoniae: proportion of invasive isolates resistant to aminoglycosides in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Figure 5.25: Klebsiella pneumoniae: proportion of invasive isolates resistant to carbapenems in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
50
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.26: Klebsiella pneumoniae: trend of third-generation cephalosporins resistance by country, 20062009
MT (<)
FI
2006 2007 2008 2009
SE
NO
NL
UK (<)
AT
ES
IE
DK (>)
DE
Country code
EE (>)
FR (>)
LU (>)
PT (>*)
SI
IT
HU (>)
CY
CZ (>)
LV
LT (>)
EL (>)
BG 0 10 20 30 40 50 60 70 80
% third-generation cephalosporins resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
51
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.27: Klebsiella pneumoniae: trend of fluoroquinolones resistance by country, 20062009
SE
MT
2006 2007 2008 2009
FI
NL
NO
UK (<)
AT
IE (<)
DE
ES (>)
DK (>) Country code
EE (>)
IT
FR (>)
PT (>*)
SI
HU (>)
LV
LT (>)
CY (>)
BG (>)
CZ (>)
EL (>) 0 10 20 30 40 % uoroquinolones resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
50
60
70
80
52
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.28: Klebsiella pneumoniae: trend of aminoglycosides resistance by country, 20062009
MT (<)
SE
2006 2007 2008 2009
FI
NO (>)
NL
AT
UK (<)
DK (>)
ES
DE
IE
Country code
EE (>)
LU (>*)
CY
IT
FR (>)
PT (>)
SI
HU (>)
LV (>)
CZ (>)
LT (>)
EL (>)
BG 0 10 20 30 40 % aminoglycosides resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
50
60
70
80
53
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.29: Klebsiella pneumoniae: trend of multiresistance (third-generation cephalosporins, fluoroquinolones and aminoglycosides) by country, 20062009
MT
FI
2006 2007 2008 2009
SE (>*)
NL
NO (>)
AT
UK (<)
ES (>)
IE
DK (>)
DE Country code
EE (>)
IT
PT (>*)
FR (>)
CY
LV (>)
SI
HU (>)
LT (>)
CZ (>)
BG (>*)
EL (>) 0 10 20 30 % Multiresistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
40
50
60
54
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Table 5.8: Number of invasive K. pneumoniae isolates and proportion of fluoroquinolones, third-generation cephalosporins, aminoglycosides and multiresistance (%R), including 95% confidence intervals (95% CI), reported per country in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic Denmark Estonia Finland France Germany Greece Hungary Iceland Ireland Italy Latvia Lithuania Luxembourg Malta Netherlands Norway Poland Portugal Romania Slovenia Spain Sweden United Kingdom Fluoroquinolones N %R (95%CI) 604 8.4 (611) 142 13.4 (820) 95 48.4 (3859) 53 43.4 (3058) 1 415 54.3 (5257) 791 16.2 (1419) 58 19.0 (1031) 375 3.2 (26) 1 352 24.0 (2226) 479 14.8 (1218) 1 626 65.6 (6368) 355 33.2 (2838) 26 0.0 (013) 315 10.8 (815) 299 20.4 (1625) 44 34.1 (2050) 67 37.3 (2650) 28 21.4 (841) 38 2.6 (014) 393 4.1 (27) 392 5.6 (48) 139 32.4 (2541) 537 27.6 (2432) 18 11.1 (135) 168 28.6 (2236) 627 15.8 (1319) 248 1.6 (04) 660 5.8 (48) Third-gen. cephalosporins N %R (95%CI) 615 7.6 (610) 142 14.8 (922) 95 69.5 (5979) 53 41.5 (2856) 1 415 52.1 (4955) 623 11.2 (914) 58 17.2 (929) 367 1.4 (03) 1 378 18.7 (1721) 471 13.2 (1017) 1 634 68.7 (6671) 359 38.4 (3344) 27 0.0 (013) 314 11.1 (815) 272 37.1 (3143) 44 54.5 (3970) 67 56.7 (4469) 28 25.0 (1145) 38 0.0 (09) 400 5.5 (38) 396 2.8 (15) 143 49.0 (4157) 556 27.5 (2431) 18 55.6 (3178) 168 33.9 (2742) 628 11.1 (914) 701 1.7 (13) 655 7.2 (59) Aminoglycosides N %R (95%CI) 618 3.6 (25) 142 9.9 (516) 95 65.3 (5575) 53 18.9 (932) 1 394 47.2 (4550) 822 7.2 (69) 60 15.0 (727) 349 1.1 (03) 1 378 19.6 (1822) 478 9.6 (713) 1 644 60.3 (5863) 361 40.4 (3546) 27 0.0 (013) 316 11.1 (815) 309 19.4 (1524) 44 43.2 (2859) 68 55.9 (4368) 28 17.9 (637) 38 0.0 (09) 397 3.3 (26) 394 3.0 (25) 150 29.3 (2237) 564 20.4 (1724) 26 30.8 (1452) 168 28.0 (2135) 628 9.2 (712) 676 0.4 (01) 695 5.5 (47) Multiresistance* N %R (95%CI) 599 2.5 (14) 142 2.8 (17) 95 38.9 (2949) 53 17.0 (830) 1 394 35.3 (3338) 600 6.8 (59) 56 8.9 (320) 341 0.6 (02) 1 352 15.5 (1417) 470 7.2 (510) 1 625 54.0 (5256) 354 28.8 (2434) 26 0.0 (013) 313 5.1 (38) 254 12.6 (917) 44 22.7 (1138) 66 34.8 (2448) 28 14.3 (433) 38 0.0 (09) 380 1.1 (03) 391 1.5 (13) 133 15.0 (922) 532 14.5 (1218) 18 11.1 (135) 168 23.2 (1730) 627 4.8 (37) 235 0.9 (03) 618 3.1 (25)
* Multiresistance defined as being resistant to third-generation cephalosporins, fluoroquinolone and aminoglycosides.
Table 5.9: Number of invasive K. pneumoniae isolates resistant to third-generation cephalosporins (CRKP) and proportion of ESBL positive among these isolates, as ascertained by the participating laboratories in 2009
Country Austria Bulgaria Cyprus Czech Republic Estonia Spain France Ireland Italy Lithuania Latvia Netherlands Poland Portugal Romania Slovenia Number of laboratories 16 10 4 44 4 20 27 12 7 9 5 4 12 11 3 7 Number of CRKP 40 66 22 737 10 70 89 32 47 38 17 11 70 92 10 57 %ESBL 87.5 98.5 86.4 79.9 100 85.7 80.9 78.1 91.5 97.4 94.1 72.7 92.9 90.2 100 96.5
Only data from laboratories consistently reporting ESBL test results for all isolates identified as resistant to third-generation cephalosporins and from countries with at least 10 of such isolates were selected for the analysis.
55
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Table 5.10: Overall resistance and resistance combinations among invasive Klebsiella pneumoniae isolates tested against fluoroquinolones, third-generation cephalosporins and aminoglycosides (n= 10 952) in Europe, 2009
Resistance pattern Fully susceptible Single resistance (to indicated drug classes) Fluoroquinolones Third-generation cephalosporins Aminoglycosides Resistance to two classes of antimicrobial drugs Third-generation cephalosporins + fluoroquinolones Third-generation cephalosporins + aminoglycosides Fluoroquinolones + aminoglycosides Resistance to three classes of antimicrobial drugs third-generation cephalosporins + fluoroquinolones + aminoglycosides Number 7 108 409 241 135 477 320 150 2 112 % of total 64.9 3.7 2.2 1.2 4.4 2.9 1.4 19.3
56
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
5.6 Pseudomonas aeruginosa
5.6.1 Clinical and epidemiological importance
Pseudomonas aeruginosa is a non-fermenting gram-negative bacterium that is ubiquitously present in aquatic environments in nature. It is an opportunistic pathogen for plants, animals and humans, and is a major and dreaded cause of infection among hospitalised patients with localised or systemic impairment of immune defences, being a common cause of hospital-acquired pneumonia (including ventilator-associated pneumonia), bloodstream and urinary tract infections. Because of its ubiquitous presence, its enormous versatility and intrinsic tolerance to many detergents, disinfectants and antimicrobial compounds, it is difficult to control P. aeruginosa in hospitals and institutional environments. Moreover, P. aeruginosa is a frequent cause of skin infections such as folliculitis and otitis externa in recreational and competitive swimmers. In patients with cystic fibrosis, P. aeruginosa causes the most important bacterial complication leading to chronic colonisation and intermittent exacerbations ranging from bronchiolitis to acute respiratory distress syndrome. Finally, P. aeruginosa is a common pathogen found in burns units, and in these locations it is almost impossible to eradicate colonising strains by classical infection control procedures.
Proportion of resistance was: 15% in six countries, 510% in four countries, 1025% in 12 countries and 2550% in six countries (Figure 5.30, Table 5.11). Trends in the 20062009 period have been calculated for 21 countries. A significant increase has been observed for France and Hungary that, in 2009, reported a proportion of resistance to piperacillintazobactam of 21% and 19%, respectively. A significant decreasing trend has been observed for Greece (proportion of resistance in 2009 was 33%) (Figure 5.35). Ceftazidime Twenty-eight countries reported 7 937 isolates of which 1 171 were resistant to ceftazidime; one country (Romania) reported less than 10 isolates and, therefore, it was not included in the map. Proportion of resistance was: 15% in four countries, 510% in eight countries, 1025% in 12 countries and 2550% in three countries (Figure 5.31, Table 5.11). Trends in the 20062009 period have been calculated for 21 countries. A significant increase has been observed for France and Hungary, which, in 2009, reported a proportion of resistance to ceftazidime of 17% and 12%, respectively. A significant decreasing trend has been observed for Portugal (proportion of resistance in 2009 was 13%) but the trend significance disappears when considering only data from laboratories consistently reporting all four years (Figure 5.36). Fluoroquinolones Twenty-eight countries reported 8 253 isolates of which 1 884 were resistant to fluoroquinolones. Proportion of resistance was: 15% in one country, 510% in five countries, 1025% in 13 countries and 2550% in nine countries (Figure 5.32, Table 5.11). Trends in the 20062009 period have been calculated for 20 countries. A significant increase has been observed for Hungary (proportion of resistance in 2009 was 27%). A significant decreasing trend has been observed for Germany, Ireland and Norway, which, in 2009, reported a proportion of resistance to fluoroquinolones of 17%, 9% and 3%, respectively. In two of these countries (Ireland and Norway) the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.37). Aminoglycosides
5.6.2 Resistance mechanism
P. aeruginosa is intrinsically resistant to the majority of antimicrobial compounds due to its selective ability to exclude various molecules from penetrating its outer membrane. The antibiotic classes that remain active include the fluoroquinolones, the aminoglycosides, some beta-lactams (piperacillin, ceftazidime, carbapenems) and colistin. Acquired resistance in P. aeruginosa is caused by one or more of several mechanisms: mutational modification of antibiotic targets, such as gyrase, topoisomerase or ribosomal proteins, which confer resistance to fluoroquinolones or aminoglycosides, respectively; mutational derepression of the chromosomally coded AmpC beta-lactamase; mutational loss of outer membrane proteins preventing the uptake of antimicrobial substances such as carbapenems; mutational upregulation of efflux systems, that can confer resistance to beta-lactams, fluoroquinolones and aminoglycosides; and acquisition of plasmid-mediated resistance genes coding for various beta-lactamases and aminoglycoside modifying enzymes that can confer resistance to various beta-lactams including carbapenems (e. g. metallo-beta-lactamases) and aminoglycosides.
Twenty-eight countries reported 8 223 isolates of which 1 437 were resistant to aminoglycosides. Proportion of resistance was: below 1% in four countries, 15% in four countries, 510% in six countries, 1025% in seven countries and 2550% in seven countries (Figure 5.33, Table 5.11). Trends in the 20062009 period have been calculated for 21 countries. Three countries (Hungary, Malta and Spain) reported a significant increasing trend (Fig
5.6.3 Results
Piperacillintazobactam Twenty-eight countries reported 8 028 isolates of which 1 306 were resistant to piperacillintazobactam.
57
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
5.38) with proportions of resistance to aminoglycosides of 29%, 21% and 19%, respectively, in 2009. Significant decreasing trends have been observed for five countries. In three of these the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.38). In 2009, these five countries reported the following proportion of resistance to aminoglycosides: 15% in one case (the United Kingdom), 510% in one case (Germany), 1025% in one case (Portugal) and 2550% in two cases (Greece and Poland). Carbapenems Twenty-eight countries reported 8 129 isolates of which 1 541 were resistant to carbapenems. Proportion of resistance was: below 1% in one country, 15% in two countries, 510% in nine countries, 1025% in 10 countries, 2550% in five countries and above 50% in one country (Figure 5.34, Table 5.11). Trends in the 20062009 period have been calculated for 20 countries. Three countries (France, Hungary and Italy) reported a significant increasing trend with proportions of resistance to carbapenems, which, in 2009, were 17%, 27% and 31%, respectively. In two of these countries (Hungary and Italy) the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure5.39). Significant decreasing trends have been observed for Austria, Czech Republic and Germany, with proportions of resistance to carbapenems of 9%, 29% and 11%, respectively, in 2009. In one of these countries (Austria) the trend is significant also when considering only data from laboratories consistently reporting all four years (Figure 5.39). Combined resistance (piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems) Twenty-eight countries reported 8 376 isolates tested for at least three antibiotic classes among piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems. In 2009, 33% of isolates were resistant to one or more of the five considered antibiotic classes while 16% were resistant to three or more. The most frequent pattern was the resistance to all five antibiotic classes (5%) (Table 5.12). Proportion of multiresistance (R to at least three of the five considered antibiotic classes) was: below 1% in one country, 15% in seven countries, 510% in four countries, 1025% in 11 countries and 2550% in five countries (Table 5.11). Trends in the 20062009 period have been calculated for 21 countries. Significant increasing trends of multiresistance have been observed for four countries. In three of these countries the trends are significant also when considering only data from laboratories
consistently reporting all four years (Figure 5.40). In 2009, these four countries (France, Hungary, Malta and Spain) reported proportion of multiresistance between 10% and 25%. Significant decreasing trends of multiresistance have been observed for four countries. In two of these the trends are significant also when considering only data from laboratories consistently reporting all four years (Figure 5.40). In 2009, these four countries reported the following proportion of multiresistance: 15% in one case (Ireland), 510% in one case (Germany), 1025% in one case (Portugal) and 2550% in one case (Greece).
5.6.4 Conclusions
High proportions of resistance of P. aeruginosa to antimicrobials have been reported by many countries especially in southern and eastern Europe. The combined resistance is also frequent with 16% of isolates resistant to at least three antibiotic classes (multiresistance) and with 5% of isolates resistant to all five antibiotic classes under surveillance. Despite the high proportions of resistance, the situation appears to be generally stable in Europe with few countries reporting significant increasing or decreasing trends of resistance. The countries with increasing trends of resistance to specific antibiotic classes or of multiresistance are: France, Hungary, Italy, Malta and Spain. In 2009, Greece reported the highest proportion of multiresistance (40%) although a significant decreasing trend was observed from 2006 to 2009.
58
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.30: Pseudomonas aeruginosa: proportion of invasive isolates resistant to piperacillintazobactam in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Figure 5.31: Pseudomonas aeruginosa: proportion of invasive isolates resistant to ceftazidime in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
59
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.32: Pseudomonas aeruginosa: proportion of invasive isolates resistant to fluoroquinolones in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
Figure 5.33: Pseudomonas aeruginosa: proportion of invasive isolates resistant to aminoglycosides in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
60
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.34: Pseudomonas aeruginosa: proportion of invasive isolates resistant to carbapenems in 2009
< 1% 1% to < 5% 5% to < 10% 10% to < 25% 25% to < 50% 50% No data reported or less than 10 isolates Not included
Non-visible countries Luxembourg Malta
61
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.35: Pseudomonas aeruginosa: trend of piperacillintazobactam resistance by country, 20062009
SE
NL
2006 2007 2008 2009
UK
NO
IE
AT
FI
ES
EE
DE Country code
LU
PT
CY
SI
HU (>)
FR (>)
IT
CZ
PL
EL (<)
MT 0 10 20 30 40 50
% Piperacillintazobactam resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
62
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.36: Pseudomonas aeruginosa: trend of ceftazidime resistance by country, 20062009
NL
FI
2006 2007 2008 2009
NO
UK
IE
AT
SE
EE
ES
SI Country code
DE
HU (>)
PT (<*)
LU
IT
FR (>)
CY
PL
CZ
MT
EL 0 10 20 30 40 50
% ceftazidime resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
63
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.37: Pseudomonas aeruginosa: trend of fluoroquinolones resistance by country, 20062009
NO (<)
SE
2006 2007 2008 2009
NL
UK
IE (<)
FI
LU
CY
AT
SI Country code
DE (<*)
EE
PT
MT
FR
ES
HU (>)
CZ
IT
EL 0 10 20 30 40 50
% uoroquinolones resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
64
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.38: Pseudomonas aeruginosa: trend of aminoglycosides resistance by country, 20062009
NO
SE
2006 2007 2008 2009
NL
UK (<)
FI
CY
IE
DE (<*)
AT
LU Country code
EE
PT (<*)
SI
FR
ES (>)
MT (>)
PL (<)
HU (>)
CZ
IT
EL (<) 0 10 20 30 40 50
% aminoglycosides resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
65
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Figure 5.39: Pseudomonas aeruginosa: trend of carbapenems resistance by country, 20062009
NL
NO
2006 2007 2008 2009
SE
FI
UK
CY
IE
AT (<)
DE (<*)
ES Country code
PT
EE
SI
FR (>*)
MT
PL
HU (>)
CZ (<*)
IT (>)
EL 0 10 20 30 40 50
% carbapenems resistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
66
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 5.40: Pseudomonas aeruginosa: trend of multiresistance (R to three or more antibiotic classes among piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems) by country, 20062009
SE
NO
2006 2007 2008 2009
UK
NL
IE (<*)
FI
AT
EE
DE (<)
CY Country code
SI
PT
ES (>)
LU
FR (>*)
MT (>)
HU (>)
PL (<*)
IT
CZ
EL (<) 0 10 20 % multiresistance
Only countries that reported 20 isolates or more per year were included. The symbols > and < indicate significant increasing and decreasing trend, respectively. The asterisks indicate significant trends in the overall data that were not supported by data from laboratories consistently reporting for all four years.
30
40
50
67
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Table 5.11: Number of invasive P. aeruginosa isolates and proportion of piperacillintazobactam, fluoroquinolones, ceftazidime, aminoglycosides, carbapenems and multiresistance (%R), including 95% confidence intervals (95% CI), reported per country in 2009
Country Austria Belgium Bulgaria Cyprus Czech Republic Denmark Estonia Finland France Germany Greece Hungary Iceland Ireland Italy Latvia Lithuania Luxembourg Malta Netherlands Norway Poland Portugal Romania Slovenia Spain Sweden United Kingdom Piperacillin tazobactam N %R (95%CI) 512 6.4 (49) 104 6.7 (313) 36 33.3 (1951) 62 17.7 (930) 574 27.9 (2432) 373 1.9 (14) 40 12.5 (427) 229 6.6 (411) 1 156 21.0 (1923) 284 13.0 (918) 1 084 32.7 (3036) 505 18.8 (1522) 16 12.5 (238) 235 4.3 (28) 185 24.3 (1831) 18 16.7 (441) 20 20.0 (644) 35 14.3 (530) 58 36.2 (2450) 233 3.0 (16) 161 3.7 (18) 151 29.8 (2338) 535 17.0 (1420) 11 36.4 (1169) 93 18.3 (1128) 539 8.2 (611) 224 2.2 (15) 555 3.1 (25) Fluoroquinolones N 512 134 36 62 575 411 43 233 1 204 285 1 080 513 16 236 193 17 21 35 58 230 162 149 517 11 93 544 259 624 %R (95%CI) 12.9 (1016) 15.7 (1023) 33.3 (1951) 12.9 (624) 41.4 (3746) 5.4 (38) 18.6 (833) 10.7 (715) 24.8 (2227) 17.2 (1322) 45.4 (4248) 26.5 (2331) 12.5 (238) 9.3 (614) 42.0 (3549) 11.8 (136) 33.3 (1557) 11.4 (327) 22.4 (1335) 7.0 (411) 2.5 (16) 25.5 (1933) 20.5 (1724) 36.4 (1169) 15.1 (824) 25.0 (2129) 6.6 (410) 7.1 (59) Ceftazidime N %R (95%CI) 483 6.0 (49) 134 6.0 (311) 35 22.9 (1040) 62 17.7 (930) 575 29.0 (2533) 311 3.5 (26) 43 7.0 (119) 233 4.7 (28) 1 085 16.8 (1519) 284 10.9 (815) 1 074 33.7 (3137) 516 11.6 (915) 16 6.3 (030) 232 6.0 (310) 164 16.5 (1123) 18 16.7 (441) 21 14.3 (336) 35 14.3 (530) 58 29.3 (1843) 228 4.4 (28) 164 4.9 (29) 121 21.5 (1530) 536 12.5 (1016) 8 37.5 (976) 93 10.8 (519) 544 7.7 (610) 317 6.9 (410) 547 5.5 (48) Aminoglycosides N %R (95%CI) 509 7.9 (611) 105 9.5 (517) 33 33.3 (1852) 62 4.8 (113) 575 32.2 (2836) 428 0.7 (02) 42 9.5 (323) 224 4.5 (28) 1 159 19.0 (1721) 284 7.4 (511) 1 090 41.3 (3844) 516 29.1 (2533) 16 0.0 (021) 235 6.4 (410) 151 36.4 (2945) 18 22.2 (648) 21 19.0 (542) 35 8.6 (223) 58 20.7 (1133) 230 1.3 (04) 165 0.0 (02) 143 27.3 (2035) 536 11.9 (915) 11 45.5 (1777) 91 14.3 (823) 543 19.2 (1623) 321 0.3 (02) 622 1.3 (13) Carbapenems N 513 134 34 61 575 347 29 229 1 219 283 1 095 516 16 224 188 14 21 33 58 234 166 142 520 11 93 540 326 508 %R (95%CI) 8.8 (612) 9.0 (515) 23.5 (1141) 8.2 (318) 28.9 (2533) 2.9 (15) 17.2 (636) 7.9 (512) 17.4 (1520) 10.6 (715) 44.0 (4147) 26.6 (2331) 0.0 (021) 8.5 (513) 30.9 (2438) 7.1 (034) 19.0 (542) 15.2 (532) 20.7 (1133) 3.0 (16) 5.4 (310) 25.4 (1833) 16.3 (1320) 54.5 (2383) 17.2 (1026) 16.1 (1319) 7.7 (511) 8.1 (611) Multiresistance* N %R (95%CI) 516 6.0 (48) 134 5.2 (210) 36 27.8 (1445) 62 11.3 (522) 575 30.8 (2735) 415 1.7 (13) 43 7.0 (119) 233 3.9 (27) 1 220 16.8 (1519) 285 7.4 (511) 1 077 40.2 (3743) 516 20.7 (1724) 16 0.0 (021) 236 3.8 (27) 195 27.7 (2235) 18 11.1 (135) 21 19.0 (542) 35 14.3 (530) 58 19.0 (1031) 234 2.1 (15) 165 1.8 (05) 152 22.4 (1630) 536 13.8 (1117) 11 36.4 (1169) 93 12.9 (721) 544 14.0 (1117) 330 1.2 (03) 620 1.9 (13)
* Multiresistance defined as being resistant to three or more antibiotic classes among piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems.
68
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Table 5.12: Overall resistance and resistance combinations among invasive Pseudomonas aeruginosa isolates tested against at least three antibiotic classes among piperacillintazobactam, ceftazidime, fluoroquinolones, aminoglycosides and carbapenems (n= 8 376) in Europe, 2009
Resistance pattern Fully susceptible (to the tested drugs) Resistance to one class of antimicrobial drugs Fluoroquinolones Carbapenems Aminoglycosides Ceftazidime Piperacillin(tazobactam) Resistance to two classes of antimicrobial drugs Fluoroquinolones + aminoglycosides Piperacillin(tazobactam) + ceftazidime Fluoroquinolones + carbapenems Piperacillin(tazobactam) + fluoroquinolones Piperacillin(tazobactam) + carbapenems Piperacillin(tazobactam) + aminoglycosides Aminoglycosides + carbapenems Ceftazidime + carbapenems Fluoroquinolones + ceftazidime Ceftazidime + aminoglycosides Resistance to three classes of antimicrobial drugs Fluoroquinolones + aminoglycosides + carbapenems Piperacillin(tazobactam) + fluoroquinolones + aminoglycosides Piperacillin(tazobactam) + ceftazidime + carbapenems Piperacillin(tazobactam) + fluoroquinolones + ceftazidime Fluoroquinolones + ceftazidime + aminoglycosides Piperacillin(tazobactam) + fluoroquinolones + carbapenems Fluoroquinolones + ceftazidime + carbapenems Piperacillin(tazobactam) + aminoglycosides + carbapenems Piperacillin(tazobactam) + ceftazidime + aminoglycosides Ceftazidime + aminoglycosides + carbapenems Resistance to four classes of antimicrobial drugs Piperacillin(tazobactam) + fluoroquinolones + aminoglycosides + carbapenems Fluoroquinolones + ceftazidime + aminoglycosides + carbapenems Piperacillin(tazobactam) + fluoroquinolones + ceftazidime + aminoglycosides Piperacillin(tazobactam) + fluoroquinolones + ceftazidime + carbapenems Piperacillin(tazobactam) + ceftazidime + aminoglycosides + carbapenems Resistance to five classes of antimicrobial drugs Piperacillin(tazobactam) + fluoroquinolones + ceftazidime + aminoglycosides + carbapenems Number 5 588 350 309 101 83 72 185 147 93 27 26 21 16 16 11 5 165 83 62 39 36 19 16 12 9 9 139 100 96 94 18 429 % of total 66.7 4.2 3.7 1.2 1 0.9 2.2 1.8 1.1 0.3 0.3 0.3 0.2 0.2 0.1 0.1 2 1 0.7 0.5 0.4 0.2 0.2 0.1 0.1 0.1 1.7 1.2 1.1 1.1 0.2 5.1
69
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
5.7 References
Prevention of pneumococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 1997;46:1-24. Arthur M, Molinas C, Depardieu F, Courvalin P. Characterization of Tn1546, a Tn3-related transposon conferring glycopeptide resistance by synthesis of depsipeptide peptidoglycan precursors in Enterococcus faecium BM4147. J Bacteriol 1993;175:117-27. Banerjee SN, Emori TG, Culver DH, Gaynes RP, Jarvis WR, Horan T et al. Secular trends in nosocomial primary bloodstream infections in the United States, 19801989. National Nosocomial Infections Surveillance System. Am J Med 1991;91:86S-9S. Benyacoub J, Czarnecki-Maulden GL, Cavadini C, Sauthier T, Anderson RE, Schi rin EJ et al. Supplementation of food with Enterococcus faecium (SF68) stimulates immune functions in young dogs. J Nutr 2003;133:1158-62. Berger-Bachi B, Rohrer S. Factors inuencing methicillin resistance in staphylococci. Arch Microbiol 2002;178:165-71. Chow JW. Aminoglycoside resistance in enterococci. Clin Infect Dis 2000;31:586-9. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillinresistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53-9. DiazGranados CA, Jernigan JA. Impact of vancomycin resistance on mortality among patients with neutropenia and enterococcal bloodstream infection. J Infect Dis 2005;191:588-95. Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN et al. Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacic region for the SENTRY Antimicrobial Surveillance Program, 19971999. Clin Infect Dis 2001;32 Suppl 2:S114-32. Evans AS BP. Bacterial infections of humans, epidemiology and control. New York: Plenum Medical Book Company; 1991. p. 525-46. Fluit AC, Jones ME, Schmitz FJ, Acar J, Gupta R, Verhoef J. Antimicrobial susceptibility and frequency of occurrence of clinical blood isolates in Europe from the SENTRY antimicrobial surveillance program, 1997 and 1998. Clin Infect Dis 2000;30:454-60. Fontana R, Ligozzi M, Pittaluga F, Satta G. Intrinsic penicillin resistance in enterococci. Microb Drug Resist 1996;2:209-13. Franz CM, Holzapfel WH, Stiles ME. Enterococci at the crossroads of food safety? Int J Food Microbiol 1999;47:1-24. Garau J. Role of beta-lactam agents in the treatment of communityacquired pneumonia. Eur J Clin Microbiol Infect Dis 2005;24:83-99. Gold HS, Moellering RC Jr. Antimicrobial-drug resistance. N Engl J Med 1996;335:1445-53. Hausdor WP, Bryant J, Kloek C, Paradiso PR, Siber GR. The contribution of specic pneumococcal serogroups to di erent disease manifestations: implications for conjugate vaccine formulation and use, part II. Clin Infect Dis 2000;30:122-40. Hausdor WP, Bryant J, Paradiso PR, Siber GR. Which pneumococcal serogroups cause the most invasive disease: implications for conjugate vaccine formulation and use, part I. Clin Infect Dis 2000;30:100-21. Hausdor WP, Siber G, Paradiso PR. Geographical di erences in invasive pneumococcal disease rates and serotype frequency in young children. Lancet 2001;357:950-2. Hawkey PM. Mechanisms of quinolone action and microbial response. J Antimicrob Chemother 2003;51 Suppl 1:29-35. Herwaldt LA. Control of methicillin-resistant Staphylococcus aureus in the hospital setting. Am J Med 1999;106:11S-8S; discussion 48S-52S. Hiramatsu K, Cui L, Kuroda M, Ito T. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol 2001;9:486-93. Huycke MM, Sahm DF, Gilmore MS. Multiple-drug resistant enterococci: the nature of the problem and an agenda for the future. Emerg Infect Dis 1998;4:239-49. Jacobs MR. In vivo veritas: in vitro macrolide resistance in systemic Streptococcus pneumoniae infections does result in clinical failure. Clin Infect Dis 2002;35:565-9. Jacobs MR. Worldwide trends in antimicrobial resistance among common respiratory tract pathogens in children. Pediatr Infect Dis J 2003;22(8 Suppl):S109-19. Jett BD, Huycke MM, Gilmore MS. Virulence of enterococci. Clin Microbiol Rev 1994;7:462-78. Karchmer AW. Nosocomial bloodstream infections: organisms, risk factors, and implications. Clin Infect Dis 2000;31 Suppl 4:S139-43. Kumarasamy KK, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis 2010;10:597-602.
Landry SL, Kaiser DL, Wenzel RP. Hospital stay and mortality attributed to nosocomial enterococcal bacteremia: a controlled study. Am J Infect Control 1989;17:323-9. Leclercq R, Courvalin P. Resistance to glycopeptides in enterococci. Clin Infect Dis 1997;24:545-54; quiz 555-6. Marchaim D, Navon-Venezia S, Schwaber MJ, and Carmeli Y. Isolation of imipenem-resistant Enterobacter species: Emergence of KPC-2 carbapenemase, molecular characterization, epidemiology, and outcomes. Antimicrob Agents Chemother 2008;52(4): 141318. Published online 2008 January 28. doi: 10.1128/AAC.01103-07. McCormick AW, Whitney CG, Farley MM, Lyneld R, Harrison LH, Bennett NM et al. Geographic diversity and temporal trends of antimicrobial resistance in Streptococcus pneumoniae in the United States. Nat Med 2003;9:424-30. McGowan JE. Resistance in nonfermenting gram-negative bacteria: multidrug resistance to the maximum. Am J Infect Control 2006;34(5 Suppl 1). Mitra AK, Rabbani GH. A double-blind, controlled trial of bioorin (Streptococcus faecium SF68) in adults with acute diarrhea due to Vibrio cholerae and enterotoxigenic Escherichia coli. Gastroenterology 1990;99:1149-52. Mundy LM, Sahm DF, Gilmore M. Relationships between enterococcal virulence and antimicrobial resistance. Clin Microbiol Rev 2000;13:513-22. Murray BE. Beta-lactamase-producing enterococci. Antimicrob Agents Chemother 1992;36:2355-9. Paterson DL. Resistance in gram-negative bacteria: Enterobacteriaceae. Am J Infect Control 2006;34(5 Suppl 1). Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H et al. International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum betalactamase production in nosocomial Infections. Ann Intern Med 2004;140:26-32. Perichon B, Reynolds P, Courvalin P. VanD-type glycopeptide-resistant Enterococcus faecium BM4339. Antimicrob Agents Chemother 1997;41:2016-8. Peterson LR. Squeezing the antibiotic balloon: the impact of antimicrobial classes on emerging resistance. Clin Microbiol Infect 2005;11 Suppl 5. Reacher MH, Shah A, Livermore DM, Wale MC, Graham C, Johnson AP, et al. Bacteraemia and antibiotic resistance of its pathogens reported in England and Wales between 1990 and 1998: trend analysis. BMJ 2000;320:213-6. Rodriguez-Martinez JM, Poirel L, Pascual A, Nordmann P. Plasmidmediated quinolone resistance in Australia. Microb Drug Resist 2006;12:99-102. Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A. Plasmid-mediated quinolone resistance: a multifaceted threat. Clin Microbiol Rev. 2009;22:664-89. Schmitt HJ. Pneumococcal conjugate vaccines in Europe, Berlin, Germany, 23-25 August 2000. Report of a European advisory board meeting. Vaccine 2001;19:3347-54. Shepard BD, Gilmore MS. Antibiotic-resistant enterococci: the mechanisms and dynamics of drug introduction and resistance. Microbes Infect 2002;4:215-24. Sturenburg E, Mack D. Extended-spectrum beta-lactamases: implications for the clinical microbiology laboratory, therapy, and infection control. J Infect 2003;47:273-95. Vatopoulos A. High rates of metallo-beta-lactamase-producing Klebsiella pneumoniae in Greece a review of the current evidence. Euro Surveill 2008; 13(4) pii 8023. Watson DA, Musher DM. A brief history of the pneumococcus in biomedical research. Semin Respir Infect 1999;14:198-208. Weisblum B. Insights into erythromycin action from studies of its activity as inducer of resistance. Antimicrob Agents Chemother 1995;39:797-805. Willems RJ, Top J, van Santen M, Robinson DA, Coque TM, Baquero F et al. Global spread of vancomycin-resistant Enterococcus faecium from distinct nosocomial genetic complex. Emerg Infect Dis 2005;11:821-8. Wuorimaa T, Kayhty H. Current state of pneumococcal vaccines. Scand J Immunol 2002;56:111-29. Zhong P, Cao Z, Hammond R, Chen Y, Beyer J, Shortridge VD et al. Induction of ribosome methylation in MLS-resistant Streptococcus pneumoniae by macrolides and ketolides. Microb Drug Resist 1999;5:183-8.
70
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Annex 1: Technical notes
71
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Technical notes for chapter 4
Number of blood culture sets
The total number of blood culture sets was defined as the number of blood samples, not the number of patients sampled.
Technical notes for chapter 5
Resistance trend analysis
Resistance trends were calculated for the last four years. To determine significant trends over time, the Cochrane-Armitage test was used, excluding countries reporting less than 20 isolates per year. To exclude possible biases in the trend analyses, a sensitivity analysis was done, per country, to determine the sensitivity of the trend analysis for using the complete dataset, versus a subset from laboratories reporting all four years. In the graphs, trends were indicated in the following way: using <* if decreasing or >* if increasing when significant trends were only identified in the complete dataset; and using < if decreasing or > if increasing when a significant trend was detected in both the subset and the complete dataset.
Patient days
If patient days were not available at hospital level, these were calculated by: Number of beds * (annual occupancy / 100) * 365
Type of hospitals
Since hospital categorisation was always intricate, more specific definitions from WHO have been implemented to make the categorisation of hospitals easier. Primary level, often referred to as a district hospital or first-level referral: A hospital with few specialities, mainly internal medicine, obstetrics-gynecology, paediatrics, and general surgery, or only general practice; limited laboratory services are available for general, but not for specialised pathological analysis; the bed capacity ranges from 30 to 200 beds. Secondary level, often referred to as provincial hospital: A hospital highly differentiated by function with five to 10 clinical specialities; bed capacity ranging from 200 to 800 beds. Tertiary level, often referred to as central, regional or tertiary-level hospital: A hospital with highly specialised staff and technical equipment, e.g., cardiology, ICU and specialised imaging units; clinical services are highly differentiated by function; the hospital may have teaching activities; bed capacity ranges from 300 to 1 500 beds. A fourth category was for hospitals with a single specialty.
European maps showing resistance levels
To be included in the maps of Europe displaying the resistance proportions per country, for all drug-bug combinations under surveillance by EARS-Net, a country had to report results for at least 10 isolates.
Averaged variables
Annual occupancy rate and length of stay were averaged per country. In these totals only laboratory/hospital questionnaires that provided information on all variables needed for the specific formula were included.
73
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Annex 2: Country summary sheets
75
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Explanation to the country summary sheets
General information about EARS-Net participating laboratories and hospitals
Table 1 gives the number of laboratories and isolates reported by year and by pathogen under EARS-Net surveillance for the period 20022009.
PNSP at laboratory level/MRSA, FREC and CRKP at hospital level
Figures 1, 2, 3 and 4 show the local variation in the proportions of PNSP by laboratory and of MRSA, FREC and CRKP by hospital. These figures are based on data from 2008 and 2009, only including the laboratories and hospitals that reported at least five isolates in these two years. The total number of laboratories or hospitals, the minimum, maximum, median, first and third quartile of the proportion of resistance is displayed in a box in the figures.
Antibiotic resistance 20022009
Table 2 provides information on the proportion of invasive bacterial isolates non-susceptible (I+R) or resistant (R) to the antibiotics or antibiotic classes mentioned in the EARSS protocols. When interpreting the results in Table 2, always check the number of isolates provided in Table 1.
Demographic characteristics
Table 3 gives the proportional distribution of the isolates reported by source, gender, age, and hospital department, and the proportion of resistance within the different groups, for the period 20082009. The abbreviations used in this table stand for: PNSP = penicillin-non-susceptible S. pneumoniae; MRSA = meticillin-resistant S. aureus; FREC = fluoroquinolone-resistant E. coli; VRE = vancomycin-resistant E. faecalis or E. faecium; CRKP = third-generation cephalosporin resistant K. pneumoniae; and CRPA = carbapenem-resistant P. aeruginosa. If the number of isolates in a certain category accounts for less than 0.5% of the total number of isolates, the % total is set at 0 and the % resistance is not shown.
77
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Austria
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 10 80 20 163 28 257 31 298 32 293 35 322 38 380 38 379 S. aureus Labs Isolates 11 456 20 871 30 1 453 32 1 481 33 1 640 34 1 577 38 1 899 38 1 794 E. coli Labs Isolates 10 479 21 985 31 1 862 33 2 058 33 2 483 34 2 545 38 2 985 38 2 625 Enterecocci Labs Isolates 10 181 19 327 28 604 30 568 33 699 33 688 38 864 36 825 K. pneumoniae Labs Isolates 7 89 30 434 33 445 38 583 37 622 P. aeruginosa Labs Isolates 8 77 31 405 33 411 38 510 36 525
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 1 10 12 33 4 10 1 3 29 <1 84 21 7 2003 1 9 13 15 41 5 14 2 1 33 <1 85 22 <1 2004 1 5 13 14 46 6 17 3 <1 23 <1 85 22 <1 2005 <1 5 15 14 49 6 19 4 1 29 <1 85 30 1 3 11 6 13 7 10 6 14 2006 <1 5 13 9 53 8 22 7 2 29 <1 89 21 <1 5 8 6 8 9 15 9 15 2007 2 5 13 11 53 8 26 9 2 30 <1 82 28 2 5 13 8 6 5 12 9 15 2008 <1 5 12 8 50 7 23 7 2 21 <1 91 19 2 6 12 8 8 6 11 8 12 2009 3 5 14 6 49 6 20 8 1 31 <1 88 31 4 4 8 8 6 6 9 8 13
78
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=719 % total % PNSP 97 3 57 42 1 8 4 41 47 <1 15 50 2 30 2 4 15 6 3 0 7 4 5 4 0 7 4 7 5 2 S. aureus n=3 633 % total % MRSA 100 58 41 1 2 2 37 58 <1 12 48 11 28 2 7 8 6 16 5 3 10 12 25 18 9 17 8 7 E. coli n=5 591 % total % FREC 100 <1 41 58 1 2 1 28 70 <1 7 54 8 28 2 22 25 25 19 13 6 19 21 21 29 24 19 18 24 21 E. faecalis n=1 020 % total % VRE 100 62 37 1 4 1 36 59 0 18 39 13 28 3 0 1 0 0 0 0 0 0 0 1 0 0 0 0 E. faecium n=644 % total % VRE 100 58 41 1 1 1 42 56 <1 27 33 13 24 3 3 4 2 0 0 0 2 2 0 2 2 1 2 5 K. pneumoniae n=1 194 % total % CRKP 100 0 56 44 1 2 <1 34 63 12 41 12 31 3 8 0 10 5 17 8 0 10 6 12 6 7 8 0 P. aeruginosa n=1 020 % total % CRPA 100 <1 58 40 1 1 1 35 63 17 33 10 37 3 10 0 11 9 7 7 5 16 9 18 9 6 12 3
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
79
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Austria
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
AT011 (0/6) AT032 (0/10) AT007 (0/28) AT035 (0/5) AT036 (0/6) AT027 (0/29) AT030 (0/18) AT018 (0/12) AT033 (0/15) AT034 (0/12) AT014 (0/5) AT042 (0/7) AT015 (0/11) AT026 (0/26) AT003 (0/19) AT022 (0/11)
N laboratories Minimum First quartile Median Third quartile Maximum
36 0 0 0 5.8 25
AT017 (0/11) AT041 (0/10) AT002 (1/47) AT010 (1/36) AT006 (1/35) AT005 (2/61) AT024 (1/26) AT001 (2/48) AT016 (1/23) AT019 (1/22) AT008 (1/14) AT025 (4/47) AT009 (2/17) AT012 (2/17) AT021 (2/15) AT031 (2/14) AT023 (1/5) AT020 (1/5) AT028 (8/32)
25
50
75
100
Hospital codes
AT037 (0/8)
AT015W (0/6) AT032D (0/7) AT015M (0/7) AT029O (0/9) AT022R (0/5) AT005U (0/8) AT030W (0/23) AT030G (0/28) AT030F (0/26) AT009W (0/8) AT022L (0/23) AT036H (0/8) AT012Z (0/13) AT032E (0/5) AT007F (0/15) AT026Z (0/12) AT008B (0/12) AT010R (0/6) AT030L (0/5) AT036B (0/7) AT015S (0/18) AT009R (0/18) AT023F (0/6) AT022S (0/7) AT022B (0/24) AT30UE (0/12) AT023E (0/9) AT042T (0/20) AT005K (0/25) AT022K (0/19) AT012D (0/19) AT030H (0/14) AT032R (0/9) AT030V (0/6) AT007V (0/8) AT014R (1/66) AT037P (1/47) AT015A (1/45) AT005L (1/44) AT024V (2/79) AT012W (1/38) AT005Z (1/38) AT011W (1/37) AT026S (1/37) AT001S (2/71) AT042B (1/33) AT023K (1/31) AT016W (3/92) AT010B (1/22) AT010H (1/21) AT021V (3/60) AT028R (5/100) AT006N (1/19) AT008S (1/19) AT005I (8/146) AT016G (1/18) AT017K (2/35) AT041E (1/17) AT007W (1/17) AT035H (4/67) AT010F (4/58) AT001E (5/71) AT003G (2/28) AT007K (9/124) AT040A (3/40) AT012H (1/13) AT005R (1/12) AT009S (1/12) AT034E (6/69) AT019P (9/103) AT025K (13/143) AT005S (1/11) AT018M (7/75) AT002A (23/232) AT009K (1/10) AT033D (10/98) AT032J (1/9) AT011P (2/18) AT006S (11/99) AT024G (4/34) AT001B (4/34) AT024B (4/32) AT023S (7/56) AT022M (1/8) AT017T (2/16) AT033F (4/31) AT021S (2/14) AT027L (24/168) AT031W (17/113) AT020W (10/66) AT005H (1/6) AT005J (1/5) AT032B (7/29) AT032V (2/8) AT020N (2/7) AT032G (6/19)
N hospitals Minimum First quartile Median Third quartile Maximum
96 0 0 3.9 9.2 31.6
Laboratory codes
25
50
75
100
80
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
AT017T (0/5) AT010F (0/11) AT012D (0/5) AT042T (0/9) AT026S (0/11) AT021V (0/14) AT023K (0/18) AT020N (0/12) AT032B (0/11) AT010B (0/12) AT009K (0/6) AT041E (0/14) AT012W (0/5) AT042B (0/23) AT007V (0/8) AT037P (0/7) AT023S (0/19) AT029O (0/7) AT008S (0/5) AT024B (0/5) AT001S (0/26) AT032G (0/6) AT017K (0/16) AT036B (0/5) AT022L (0/10) AT001B (0/7) AT014R (0/10) AT005H (0/5) AT028R (1/51) AT031W (1/30) AT025K (3/69) AT027L (3/64) AT034E (1/20) AT006S (3/46) AT005L (1/14) AT035H (2/28) AT016W (2/27) AT002A (4/53) AT011W (1/13) AT030F (1/12) AT024V (2/22) AT015A (1/10) AT001E (3/29) AT005Z (1/9) AT003G (1/9) AT007K (3/26) AT024G (1/8) AT033D (5/36) AT005K (2/14) AT020W (5/33) AT005I (12/75) AT019P (3/17) AT033F (2/11) AT030V (1/5) AT018M (5/22) AT040A (3/11) AT030G (2/6) AT005S (2/5) AT005C (7/7) N hospitals Minimum First quartile Median Third quartile Maximum 59 0 0 3.3 11.1 100
AT023G (0/5) AT030V (0/23) AT023F (0/6) AT009K (0/10) AT024U (0/9) AT022S (0/9) AT009R (1/22) AT012Z (1/14) AT009S (1/13) AT032V (2/24) AT032B (3/36) AT024B (4/46) AT023K (5/55) AT024G (4/42) AT022R (1/10) AT032D (1/10) AT006N (1/10) AT024V (12/112) AT036H (2/18) AT015S (2/18) AT010H (4/35) AT005L (8/69) AT010F (8/67) AT036B (3/25) AT001B (6/44) AT016W (21/154) AT032R (2/14) AT005K (5/33) AT010B (9/59) AT009W (2/13) AT003G (5/32) AT034E (12/76) AT007V (6/38) AT016G (4/25) AT008S (5/31) AT040A (11/66) AT019L (2/12) AT008A (2/12) AT026S (14/83) AT033F (9/53) AT030H (6/35) AT023S (17/98) AT015W (5/28) AT042T (5/27) AT028R (43/232) AT021V (10/53) AT007F (4/21) AT014R (15/78) AT030W (8/41) AT012W (8/41) AT015A (18/92) AT011G (2/10) AT015M (3/15) AT008M (1/5) AT041E (22/109) AT006S (23/110) AT025K (69/326) AT011P (7/33) AT030F (19/89) AT001S (28/131) AT005R (3/14) AT007W (6/28) AT021S (3/14) AT031W (33/152) AT020W (20/92) AT022L (14/64) AT001E (34/153) AT019P (22/98) AT020N (7/31) AT032G (7/31) AT022K (5/22) AT30UE (3/13) AT002A (47/200) AT007K (40/169) AT029O (6/25) AT026Z (4/16) AT012H (2/8) AT018M (27/107) AT017T (4/15) AT005Z (14/52) AT033D (38/137) AT042B (10/36) AT027L (82/289) AT023E (4/14) AT030G (11/38) AT017K (18/61) AT035H (32/107) AT012D (7/23) AT022B (5/16) AT036M (2/6) AT011W (15/45) AT005J (5/14) AT037P (19/53) AT032P (4/11) AT010R (6/16) AT005U (3/8) AT005S (8/19) AT012T (3/7) AT005I (102/231) AT003M (4/9) AT006O (6/13) AT005H (10/21) AT005C (3/6) AT005N (5/10) AT022A (3/6)
N hospitals Minimum First quartile Median Third quartile Maximum
105 0 14.3 20 26.7 50
Hospital codes
25
50
75
100
Hospital codes
25
50
75
100
81
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Belgium
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 98 1 210 107 1 488 95 1 443 97 1 539 98 1 427 105 1 511 101 1 647 101 1 885 S. aureus Labs Isolates 48 1 092 47 1 133 49 1 227 41 1 048 33 858 34 855 38 906 34 949 E. coli Labs Isolates 27 1 184 24 1 326 25 1 601 25 1 592 21 1 632 17 1 460 16 1 430 18 1 610 Enterecocci Labs Isolates 23 205 16 146 18 228 19 223 22 267 20 245 19 236 14 227 K. pneumoniae Labs Isolates 8 142 P. aeruginosa Labs Isolates 8 136
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 14 34 28 47 6 13 3 <1 20 <1 56 5 <1 2003 <1 12 34 30 50 5 12 3 1 17 1 78 <1 <1 2004 <1 9 33 33 50 5 15 3 2 22 <1 63 11 5 2005 3 12 31 31 53 4 17 4 <1 26 <1 61 22 14 2006 4 10 31 22 54 6 19 3 <1 30 <1 67 19 4 2007 3 9 25 23 57 5 19 4 <1 26 1 68 23 <1 2008 <1 8 24 21 55 4 17 4 3 30 <1 76 17 5 2009 <1 <1 23 21 56 7 20 6 1 23 1 90 32 4 10 13 15 7 6 9 10 16
82
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=3 532 % total % PNSP 96 4 53 46 1 19 5 34 41 14 34 2 30 21 4 7 4 5 0 11 3 6 11 9 9 10 9 8 S. aureus n=1 855 % total % MRSA 100 61 38 1 4 2 34 58 1 15 34 10 26 16 21 22 19 13 8 9 21 32 20 34 24 30 26 23 E. coli n=2 828 % total % FREC 100 <1 46 53 1 2 1 29 68 <1 3 10 2 14 71 19 0 20 17 6 5 13 16 18 50 17 16 18 15 17 E. faecalis n=335 % total % VRE 100 63 34 2 4 1 29 66 0 23 34 9 24 11 1 1 0 0 0 0 0 1 0 0 1 0 0 1 E. faecium n=126 % total % VRE 100 55 41 4 3 37 59 1 22 31 6 26 15 5 7 2 0 0 2 6 0 4 3 0 5 10 K. pneumoniae n=142 % total % CRKP 99 1 58 41 1 6 31 63 100 15 0 16 14 0 22 18 12 15 P. aeruginosa n=134 % total % CRPA 100 66 34 3 1 25 72 100 9 6 15 0 0 12 8 9
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
83
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Belgium
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
BE153 (0/6) BE083 (0/25) BE018 (0/9) BE064 (0/23) BE164 (0/29) BE100 (0/20) BE101 (0/35) BE102 (0/29) BE159 (0/13) BE081 (0/11) BE033 (0/23) BE044 (0/5) BE160 (0/14) BE087 (0/5) BE146 (0/28) BE010 (0/15) BE157 (0/16) BE048 (0/33) BE171 (0/7) BE107 (0/17) BE103 (0/27) BE073 (0/9) BE024 (0/61) BE110 (0/28) BE054 (0/47) BE037 (0/28) BE031 (0/22) BE051 (0/29) BE125 (0/9) BE139 (0/51) BE049 (0/37) BE017 (0/16) BE021 (0/56) BE007 (0/20) BE072 (0/19) BE105 (0/38) BE111 (1/102) BE115 (1/68) BE030 (1/67) BE075 (1/58) BE008 (1/54) BE032 (1/48) BE063 (1/42) BE113 (1/40) BE108 (4/154) BE061 (2/76) BE090 (1/36) BE077 (1/36) BE114 (1/34) BE004 (1/34) BE093 (1/32) BE003 (1/31) BE005 (1/27) BE035 (1/25) BE043 (4/98) BE011 (1/24) BE060 (1/24) BE074 (2/48) BE001 (3/69) BE092 (5/115) BE104 (2/44) BE116 (1/22) BE091 (4/88) BE022 (2/41) BE009 (1/20) BE046 (3/58) BE154 (1/19) BE056 (4/75) BE166 (1/18) BE118 (2/36) BE070 (5/90) BE014 (2/32) BE026 (1/16) BE137 (1/15) BE057 (1/15) BE019 (2/29) BE161 (3/43) BE045 (7/99) BE109 (1/13) BE016 (5/63) BE023 (3/37) BE112 (6/74) BE097 (5/60) BE012 (2/23) BE006 (4/44) BE152 (1/11) BE098 (4/43) BE071 (2/21) BE076 (1/10) BE084 (3/28) BE069 (2/17) BE129 (1/8) BE158 (1/6) BE029 (2/11) BE095 (7/35) BE143 (7/31) BE127 (2/8) BE065 (2/6)
N laboratories Minimum First quartile Median Third quartile Maximum
98 0 0 2.9 6.7 33.3
BE041A (0/15) BE048A (0/10) BE030A (1/31) BE077A (6/93) BE054A (3/45) BE111A (3/27) BE060A (4/31) BE022A (5/38) BE164A (2/14) BE005A (3/20) BE063A (16/105) BE045A (9/52) BE008A (23/121) BE016A (26/132) BE074A (16/80)
N hospitals Minimum First quartile Median Third quartile Maximum
33 0 14.3 20.2 26.5 43.6
Laboratory codes
Hospital codes 0 25 50 75 100
BE139A (10/50) BE112A (24/119) BE002A (12/58) BE115A (18/87) BE061A (25/113) BE097A (17/74) BE007A (5/21) BE012A (6/25) BE006A (16/62) BE024A (18/68) BE070A (35/125) BE029A (5/17) BE032A (25/84) BE019A (7/23) BE056A (6/19) BE152A (7/19) BE125A (3/8) BE143A (24/55)
25
50
75
100
84
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 8 0 0 8 21.7 26.9
BE164A (1/29)
BE032A (22/227)
N hospitals Minimum First quartile Median Third quartile Maximum
16 3.4 14.8 17.8 24.6 31.6
BE003A (0/11)
BE006A (18/166) BE006A (0/10) BE022A (18/124)
BE097A (52/345) BE016A (0/14) BE007A (13/86)
BE016A (43/266) BE042A (1/13)
Hospital codes
BE008A (55/316)
BE112A (48/265)
Hospital codes
BE077A (1/12) BE092A (7/34) BE008A (5/22) BE115A (7/26)
BE061A (47/212)
BE139A (32/133)
BE070A (34/140)
BE012A (19/76)
BE063A (60/239)
BE005A (18/64)
BE077A (43/136)
25
50
75
100
25
50
75
100
85
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Bulgaria
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 11 25 13 22 13 32 16 43 11 29 10 32 13 29 10 27 S. aureus Labs Isolates 21 116 20 157 22 170 26 160 23 159 14 121 21 160 20 221 E. coli Labs Isolates 20 135 20 158 20 167 23 203 20 196 15 127 22 147 17 194 Enterecocci Labs Isolates 16 42 16 49 16 75 21 95 19 98 13 65 18 70 16 92 K. pneumoniae Labs Isolates 15 34 15 55 9 29 11 49 12 95 P. aeruginosa Labs Isolates 9 34 13 31 6 14 10 23 11 36
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 8 8 9 33 52 17 14 13 26 63 <1 71 83 <1 2003 9 14 11 31 54 22 19 18 7 36 <1 60 60 <1 2004 22 22 17 23 64 20 24 22 15 33 2 59 62 <1 2005 30 33 8 29 69 24 29 28 8 24 <1 96 56 <1 53 26 50 50 45 38 53 47 2006 7 7 15 28 64 28 26 29 31 53 2 97 79 <1 60 24 60 33 13 14 42 17 2007 9 16 17 13 70 20 35 23 13 29 <1 100 75 <1 59 41 55 14 21 7 29 14 2008 21 21 4 25 65 31 32 29 8 44 <1 93 84 <1 59 52 73 48 55 17 48 36 2009 22 37 27 16 66 18 28 19 16 36 <1 96 65 <1 65 48 69 33 23 24 33 33
86
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=56 % total % PNSP 63 38 63 38 13 9 58 18 1 15 31 2 51 34 19 26 33 41 10 14 30 33 16 20 0 23 S. aureus n=381 % total % MRSA 100 61 39 0 10 5 57 28 <1 15 35 12 38 20 21 18 100 34 14 24 23 20 40 15 38 23 E. coli n=339 % total % FREC 99 1 48 52 7 4 48 41 1 11 47 12 29 <1 30 0 36 23 12 20 27 26 50 31 20 35 29 50 E. faecalis n=101 % total % VRE 100 67 33 11 1 50 37 <1 20 34 11 35 0 0 0 0 0 1 0 0 0 1 0 0 E. faecium n=54 % total % VRE 100 48 52 16 1 49 31 4 35 18 13 35 0 0 0 0 0 0 0 0 0 0 0 0 K. pneumoniae n=144 % total % CRKP 100 65 35 13 4 47 36 20 24 19 37 71 71 71 67 82 68 56 73 47 70 67 P. aeruginosa n=57 % total % CRPA 100 74 26 8 2 60 30 32 16 16 36 21 17 33 18 0 18 33 31 5 19 23 -
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
87
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Bulgaria
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum BG023 (0/5)
5 0 12.5 20 50 60
BG023A (1/21)
BG011A (1/13)
N hospitals Minimum First quartile Median Third quartile Maximum
16 4.8 10.9 15.1 32.5 44.4
BG013A (1/12)
BG017A (7/70)
BG002A (2/17) BG005 (1/8)
BG021A (3/25)
BG029A (1/7)
Laboratory codes
Hospital codes 0 25 50 75 100
BG007A (6/42)
BG017 (2/10)
BG003A (4/25)
BG027A (3/10)
BG009A (3/10)
BG029 (3/6) BG006A (6/20)
BG001A (7/20)
BG018A (14/38)
BG003 (3/5)
BG005A (8/21)
BG022A (4/9)
25
50
75
100
88
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 8 56.3 64.1 68.3 84.5 88.2
BG013A (2/25)
N hospitals Minimum First quartile Median Third quartile Maximum
15 8 16.7 26.7 43.8 71.4
BG007A (9/16)
BG009A (1/10)
BG014A (1/6) BG001A (8/13)
BG011A (3/18)
BG003A (4/22) BG018A (14/21)
BG005A (6/24)
BG023A (7/27)
BG017A (18/27)
Hospital codes
BG018A (12/45)
Hospital codes
BG011A (7/10) BG021A (15/18) BG002A (6/7) BG006A (15/17)
BG001A (8/26)
BG021A (4/10)
BG017A (19/44)
BG007A (14/32)
BG027A (3/6)
BG006A (9/17)
BG002A (5/7)
25
50
75
100
25
50
75
100
89
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Cyprus
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 1 3 1 7 4 16 5 13 4 15 4 14 4 11 S. aureus Labs Isolates 1 28 3 39 5 54 5 62 4 85 5 92 5 89 E. coli Labs Isolates 1 19 4 46 5 75 5 90 5 109 4 119 5 136 Enterecocci Labs Isolates 1 28 3 38 3 40 4 48 3 63 5 85 5 80 K. pneumoniae Labs Isolates 4 9 4 26 4 39 5 62 5 53 P. aeruginosa Labs Isolates 4 8 4 37 3 52 5 43 5 62
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2003 <1 <1 33 64 63 11 32 11 <1 43 <1 100 <1 2004 <1 14 <1 49 61 11 22 9 3 77 3 100 33 33 2005 <1 19 13 56 72 13 29 16 3 71 <1 80 <1 40 11 22 33 13 38 13 13 13 2006 31 38 31 34 62 10 35 16 5 44 <1 43 14 14 12 12 27 27 24 11 11 27 2007 7 33 27 48 72 11 39 18 2 61 <1 92 33 25 13 23 31 31 15 19 25 23 2008 21 43 29 46 58 10 45 19 16 65 1 60 10 20 21 23 35 23 9 19 21 38 2009 18 36 36 33 66 10 43 14 32 66 <1 80 13 13 19 43 42 18 18 8 5 13
90
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=25 % total % PNSP 96 4 64 36 10 6 15 9 59 6 65 29 42 0 38 44 13 20 33 57 30 40 31 26 S. aureus n=181 % total % MRSA 100 67 32 1 2 2 18 21 56 19 35 13 33 <1 39 40 36 50 10 27 36 53 46 42 46 58 38 100 E. coli n=255 % total % FREC 100 55 45 <1 3 2 13 27 57 9 54 6 30 1 44 45 43 100 0 44 39 50 34 35 38 42 37 50 E. faecalis n=140 % total % VRE 100 68 31 1 1 0 17 28 54 30 29 19 22 1 0 2 0 0 0 0 1 1 0 0 0 3 E. faecium n=25 % total % VRE 100 64 36 4 2 11 39 45 38 25 21 16 16 19 11 0 0 33 9 28 19 14 25 22 K. pneumoniae n=115 % total % CRKP 100 57 37 6 4 2 23 28 43 31 27 11 31 38 34 40 71 57 0 45 33 30 49 20 35 34 P. aeruginosa n=104 % total % CRPA 100 59 34 8 5 1 24 25 46 41 20 14 26 1 13 16 9 0 0 0 10 12 19 18 10 26 4 0
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
91
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Cyprus
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum
1 50 50 50 50 50 CY003A (3/19)
N hospitals Minimum First quartile Median Third quartile Maximum
4 15.8 24.6 35.7 46.8 55.6
CY004A (3/9)
Laboratory codes
CY001 (7/14)
Hospital codes
CY001A (40/105) CY002A (25/45)
25
50
75
100
25
50
75
100
92
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum CY003A (2/15) 5 13.3 39.1 40 47.6 50
N hospitals Minimum First quartile Median Third quartile Maximum CY005A (2/6)
5 33.3 38.9 40.5 48.6 51.5
CY004A (7/18)
CY001A (25/64)
Hospital codes
CY001A (51/126)
Hospital codes 0 25 50 75 100
CY004A (2/5)
CY003A (18/37)
CY002A (10/21)
CY002A (35/68)
CY005A (5/10)
25
50
75
100
93
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Czech Republic
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 34 144 32 204 37 162 39 195 39 172 41 205 40 244 41 297 S. aureus Labs Isolates 41 1 168 45 1 387 45 1 444 47 1 553 47 1 527 47 1 653 47 1 715 46 1 695 E. coli Labs Isolates 40 1 587 43 1 766 44 1 966 47 2 234 47 2 176 48 2 407 46 2 738 45 2 759 Enterecocci Labs Isolates 39 587 44 630 41 660 45 758 45 697 47 816 44 883 44 835 K. pneumoniae Labs Isolates 37 478 45 1 130 48 1 230 45 1 493 45 1 415 P. aeruginosa Labs Isolates 36 257 43 490 41 517 42 568 45 575
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 8 4 6 45 6 10 1 2 39 <1 73 35 9 2003 <1 2 2 6 45 5 13 1 4 44 <1 80 48 3 2004 2 6 4 9 47 5 16 2 <1 43 <1 81 43 3 2005 <1 4 2 13 50 6 20 2 <1 45 <1 92 69 14 36 38 32 21 40 31 28 45 2006 <1 2 3 12 56 8 23 5 2 43 <1 90 74 4 38 47 35 29 30 33 30 47 2007 <1 4 5 13 56 7 24 7 3 49 1 91 79 6 43 48 46 30 33 36 34 43 2008 <1 3 3 14 60 9 26 10 2 49 <1 94 75 8 42 52 48 27 44 29 45 46 2009 <1 4 5 15 61 9 23 10 <1 47 <1 98 65 6 47 54 52 28 29 29 32 41
94
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=540 % total % PNSP 85 15 56 44 11 6 51 32 <1 23 38 2 35 2 3 6 3 6 7 3 4 4 0 4 4 7 5 6 S. aureus n=3 410 % total % MRSA 100 61 39 4 3 44 49 <1 22 47 11 20 1 14 14 15 3 3 11 13 0 16 10 13 8 16 E. coli n=5 494 % total % FREC 100 <1 43 57 0 3 1 33 63 <1 17 51 8 24 <1 25 6 28 22 100 6 12 19 22 0 23 20 20 21 22 E. faecalis n=1 275 % total % VRE 100 64 36 4 1 45 50 41 30 10 20 <1 0 0 0 1 0 1 0 0 0 1 0 0 E. faecium n=443 % total % VRE 100 59 41 1 1 50 47 43 23 6 28 <1 7 8 5 0 0 10 4 3 5 1 16 100 K. pneumoniae n=2 908 % total % CRKP 100 <1 60 40 3 1 42 54 <1 38 34 10 17 <1 50 27 53 45 26 32 49 43 20 52 37 46 43 48 P. aeruginosa n=1 139 % total % CRPA 99 1 63 37 3 2 44 51 <1 41 28 7 23 1 29 50 30 27 13 26 37 28 0 38 26 27 28 31
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
95
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Czech Republic
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
CZ037 (0/9) CZ029 (0/11) CZ026 (0/9) CZ017 (0/19) CZ004 (0/16) CZ019 (0/6) CZ049 (0/12) CZ002 (0/9) CZ031 (0/15) CZ008 (0/11) CZ041 (0/5) CZ009 (0/17) CZ036 (0/6) CZ003 (0/10)
N laboratories Minimum First quartile Median Third quartile Maximum
31 0 0 0 11.1 40
CZ037C (0/6) CZ047A (0/8) CZ036A (0/29) CZ017B (0/30) CZ046A (0/15) CZ009B (0/20) CZ007D (0/11) CZ021A (3/90) CZ014A (2/46) CZ031F (1/21) CZ030A (4/84) CZ028A (2/41) CZ022A (2/41) CZ040A (1/17) CZ038A (1/16) CZ039A (1/15) CZ019A (3/45) CZ037A (2/30) CZ039B (1/14) CZ029A (3/40) CZ027A (10/131) CZ032A (3/38) CZ017A (8/99) CZ011A (3/37) CZ016A (9/109) CZ015B (1/12) CZ002A (6/71) CZ020A (10/113) CZ004A (7/76) CZ006A (20/204) CZ031C (1/10) CZ044A (5/47) CZ035A (7/58) CZ018A (27/223) CZ034B (1/8) CZ031J (2/16) CZ043C (1/8) CZ031V (1/8) CZ013A (9/68) CZ015A (16/118) CZ009A (18/130) CZ026A (10/64) CZ031P (3/19) CZ031A (11/67) CZ007A (16/96) CZ037D (3/17) CZ048A (8/45) CZ042A (8/45) CZ025A (8/44) CZ008A (8/43) CZ024A (27/143) CZ031K (2/10) CZ041A (9/43) CZ003A (19/88) CZ051A (2/9) CZ034C (4/17) CZ033A (16/65) CZ043B (3/12) CZ049A (7/26) CZ034A (14/52) CZ012B (2/7) CZ044C (4/14) CZ007B (5/15) CZ005A (40/113) CZ012A (14/36) CZ023A (27/56) CZ049B (3/6) CZ050A (17/28) CZ012C (7/7)
N hospitals Minimum First quartile Median Third quartile Maximum
69 0 6.7 12.5 20 100
Laboratory codes
CZ007 (0/20) CZ024 (0/26) CZ016 (1/60) CZ044 (1/31) CZ006 (2/55) CZ015 (1/22) CZ033 (1/19) CZ042 (1/17) CZ014 (1/14) CZ023 (2/18) CZ013 (1/9) CZ027 (3/26) CZ047 (1/8) CZ030 (1/8) CZ025 (1/8) CZ040 (1/8) CZ018 (2/5)
25
50
75
100
Hospital codes
25
50
75
100
96
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
CZ047B (0/5) CZ034B (0/8) CZ039A (0/10) CZ031P (2/15) CZ014A (8/49) CZ015A (8/45) CZ032A (5/24) CZ029A (6/24) CZ026A (14/56) CZ030A (7/27) CZ017A (18/67) CZ044A (5/17) CZ020A (25/84) CZ008A (12/40) CZ039B (4/11) CZ031A (20/54) CZ048B (8/21) CZ049B (6/15) CZ016A (24/59) CZ033A (23/56) CZ012B (3/7) CZ034A (19/44) CZ013A (14/32) CZ009B (14/31) CZ022A (13/28) CZ031F (7/15) CZ017B (16/34) CZ003A (42/88) CZ024A (41/85) CZ041A (14/29)
CZ047B (0/15) CZ015B (0/9) CZ034B (0/5) CZ029A (4/70) CZ047A (4/45) CZ031V (1/11) CZ020A (9/88) CZ032A (14/114) CZ014A (13/105) CZ040A (1/8) CZ030A (20/148) CZ037A (7/50) CZ003A (13/90) CZ013A (18/122) CZ012A (6/40) CZ015A (30/199) CZ007D (3/19) CZ016A (28/173) CZ037D (6/35) CZ019A (19/110) CZ012B (4/22) CZ024A (32/163) CZ009B (1/5) CZ048A (9/45) CZ008A (19/92) CZ007A (24/115) CZ022A (23/105) CZ031A (20/91) CZ042A (32/144) CZ006A (90/396) CZ004A (30/131) CZ018A (56/238) CZ031J (8/33) CZ044C (11/43) CZ039A (8/31) CZ017A (29/111) CZ046A (24/91) CZ005A (38/144) CZ026A (31/113) CZ048B (14/51) CZ044A (20/72) CZ021A (38/136) CZ031P (7/25) CZ031Y (2/7) CZ050A (5/17) CZ037C (5/17) CZ023A (33/112) CZ011A (14/47) CZ031F (9/29) CZ049A (23/74) CZ027A (57/183) CZ031K (5/16) CZ038A (17/54) CZ035A (26/82) CZ034A (15/47) CZ009A (57/174) CZ041A (20/61) CZ043B (2/6) CZ051A (6/18) CZ025A (24/70) CZ033A (26/71) CZ028A (35/89) CZ017B (26/65) CZ002A (77/185) CZ031C (5/12) CZ049B (11/26) CZ007E (3/7) CZ039B (16/37) CZ034C (4/9) CZ012C (8/17) CZ036A (30/60) CZ007B (19/36) CZ017C (4/5)
N hospitals Minimum First quartile Median Third quartile Maximum
73 0 17.1 26.4 31.9 80
N hospitals Minimum First quartile Median Third quartile Maximum
66 0 38.1 50 60.7 88.2
Hospital codes
Hospital codes
CZ018A (107/220) CZ005A (68/138) CZ002A (6/12) CZ012A (12/24) CZ031C (5/10) CZ049A (22/43) CZ004A (31/60) CZ036A (14/27) CZ019A (31/58) CZ006A (119/221) CZ037A (12/22) CZ038A (16/29) CZ037D (5/9) CZ027A (68/120) CZ035A (48/83) CZ023A (22/38) CZ007E (3/5) CZ031V (3/5) CZ046A (23/38) CZ048A (17/28) CZ028A (20/32) CZ007A (24/38) CZ021A (40/63) CZ034C (7/11) CZ042A (34/52) CZ009A (147/219) CZ047A (13/18) CZ011A (25/34) CZ007B (21/28) CZ025A (30/40) CZ044C (13/17) CZ050A (10/13) CZ031J (12/15) CZ043B (10/12) CZ012C (5/6) CZ031K (15/17)
25
50
75
100
25
50
75
100
97
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Denmark
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 5 366 5 606 15 1 188 14 1 081 15 872 15 1 030 15 934 15 996 S. aureus Labs Isolates 5 752 5 671 15 1 436 15 1 350 15 1 279 14 1 315 15 1 295 15 1 395 E. coli Labs Isolates 5 1 283 11 2 723 12 3 021 14 3 283 14 3 532 Enterecocci Labs Isolates 11 711 13 927 14 1 005 14 1 100 K. pneumoniae Labs Isolates 11 607 13 784 14 793 14 822 P. aeruginosa Labs Isolates 13 417 14 420 14 429
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 4 5 <1 2003 <1 3 5 <1 2004 <1 3 5 1 2005 <1 4 6 2 40 2 5 1 2006 <1 4 6 2 42 3 7 2 <1 <1 87 <1 2 6 4 2007 <1 3 6 <1 43 4 9 3 2 <1 88 <1 6 13 10 3 2 2 1 6 2008 <1 3 7 2 43 4 10 4 2 37 <1 88 61 <1 7 16 9 2 3 1 1 3 2009 <1 4 4 2 43 4 13 6 1 33 <1 88 52 2 7 16 11 2 4 3 <1 5
98
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=1 930 % total % PNSP 3 3 3 3 4 4 1 3 4 4 S. aureus n=2 690 % total % MRSA 100 62 38 3 3 40 54 <1 2 19 7 6 65 2 2 1 1 1 1 1 0 2 1 2 1 1 E. coli n=6 424 % total % FREC 100 <1 49 51 <1 1 1 29 69 <1 3 44 17 21 15 12 0 14 9 100 6 3 11 9 0 15 9 8 11 12 E. faecalis n=926 % total % VRE 100 71 29 <1 2 1 33 64 12 42 19 22 5 0 0 0 0 0 0 0 0 0 0 0 1 0 E. faecium n=692 % total % VRE 100 58 41 <1 1 2 45 52 32 24 18 18 7 1 0 2 0 0 5 0 1 1 0 1 1 2 K. pneumoniae n=1 243 % total % CRKP 100 <1 59 41 1 1 35 63 5 44 22 24 5 10 0 12 7 3 5 10 8 8 9 8 9 11 P. aeruginosa n=687 % total % CRPA 99 1 61 39 2 2 31 65 8 29 13 30 20 2 0 2 2 0 9 4 1 12 0 3 1 2
Isolate source Blood 93 CSF 7 Gender Male 24 Female 24 Unknown 52 Age (years) 04 8 519 2 2064 38 65 and over 52 Unknown Hospital department ICU Internal med. Surgery Other Unknown 100
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
99
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Denmark
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
DK011 (1/73)
N laboratories Minimum First quartile Median Third quartile Maximum
15 1.4 2.1 3.6 4 5
DK010A (0/44) DK004X (0/7) DK013B (0/42) DK012E (0/16) DK014A (0/34) DK014C (0/36) DK015X (0/14) DK016D (0/15) DK014E (0/5) DK010D (0/18) DK012F (0/11) DK015B (0/5) DK016F (0/9) DK013D (0/5) DK011A (0/76) DK005X (0/6)
N hospitals Minimum First quartile Median Third quartile Maximum
54 0 0 0 2.6 28.6
DK010 (1/60)
DK006 (2/102)
DK003 (4/191)
DK014 (5/209)
DK015C (0/16) DK016B (0/41) DK014N (0/92) DK016G (0/6) DK004C (0/24) DK004A (0/106) DK008A (0/19)
DK004 (4/128)
DK013 (3/85)
DK006A (0/85)
Laboratory codes
Hospital codes 0 25 50 75 100
DK015G (0/6) DK006C (0/10) DK010B (0/6) DK016C (0/15) DK016A (1/151) DK009B (2/253) DK003C (2/169) DK002A (1/84) DK014Y (1/65) DK007B (1/64)
DK016 (7/196)
DK009 (4/163)
DK007 (3/81)
DK003B (1/62) DK003A (1/60) DK005A (1/59) DK014D (1/59) DK001A (5/212) DK002F (1/40) DK009A (1/39)
DK005 (4/103)
DK015 (4/101)
DK015A (2/69) DK013A (2/68) DK006B (2/57) DK014B (2/49) DK007A (3/63) DK002B (6/119) DK012D (1/18) DK004B (1/17) DK005B (2/30) DK002E (3/41) DK002X (2/25)
DK001 (2/46)
DK012 (6/134)
DK002 (12/258)
DK007D (1/5) DK012B (2/7)
25
50
75
100
100
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 34 0 0 6.6 12.5 42.1
DK009H (0/5) DK009G (0/10) DK007D (0/11) DK014A (1/67) DK011D (1/27) DK016G (1/26) DK007A (3/77) DK016F (2/42) DK007B (3/59) DK012E (6/117) DK002E (9/145) DK004C (11/167) DK016B (11/158) DK009A (15/213) DK016D (4/55) DK014D (13/174) DK005B (13/159) DK016C (7/81) DK003B (19/211) DK004A (19/209) DK012D (11/116) DK013D (2/21)
N hospitals Minimum First quartile Median Third quartile Maximum
49 0 7 10.7 13.4 26.2
DK011A (0/38) DK012B (0/9) DK016C (0/11) DK015G (0/11) DK011D (0/5) DK012F (0/36) DK013B (0/20) DK012E (0/17) DK014A (0/14) DK014A (0/14) DK016D (0/9) DK013A (0/12) DK014C (0/18) DK015A (1/35) DK009A (2/46) DK004C (2/38)
Hospital codes
Hospital codes 0 25 50 75 100
DK003A (17/164) DK014Y (17/159) DK002B (28/261) DK012B (7/65) DK012F (16/145) DK006B (15/135) DK009B (48/428) DK008A (8/70) DK006C (2/17) DK013B (15/126) DK015G (9/72) DK011A (26/196) DK016A (49/369) DK006A (8/60) DK013A (13/97) DK014B (10/69) DK006X (16/110) DK014C (10/68) DK003C (68/460) DK005A (30/198) DK004B (20/129) DK015A (31/192) DK002A (37/227) DK014N (17/98) DK015B (2/9) DK002F (36/149) DK001A (50/191)
DK012D (1/17) DK016A (7/111) DK005A (3/43) DK014B (2/28) DK014D (4/52) DK014N (3/38) DK002E (2/23) DK009B (13/148) DK014Y (4/36) DK004A (5/42) DK002B (8/64) DK016F (1/8) DK016B (3/23) DK005B (4/30) DK008A (1/7) DK001A (28/137) DK002A (12/58) DK002F (12/29) DK004B (8/19)
25
50
75
100
101
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Estonia
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 5 21 8 26 6 40 7 53 8 52 8 64 10 66 8 82 S. aureus Labs Isolates 8 82 9 98 9 104 8 141 9 154 10 206 11 185 11 213 E. coli Labs Isolates 6 67 9 98 10 167 10 156 9 215 11 219 11 267 11 320 Enterecocci Labs Isolates 3 13 6 27 5 63 7 66 8 85 8 66 11 86 8 72 K. pneumoniae Labs Isolates 7 38 6 47 9 63 10 72 7 60 P. aeruginosa Labs Isolates 5 38 6 43 8 48 8 41 6 43
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 <1 <1 <1 42 10 5 2 10 50 <1 33 67 <1 2003 <1 <1 10 4 42 3 5 1 4 22 <1 75 50 <1 2004 <1 <1 6 5 55 2 6 4 14 32 <1 79 79 <1 2005 <1 2 <1 2 45 4 5 1 14 50 <1 83 74 <1 8 <1 8 27 18 38 28 14 2006 <1 2 3 3 52 2 7 <1 9 35 <1 84 78 <1 9 5 9 12 7 29 8 10 2007 <1 <1 2 9 50 6 7 1 <1 23 <1 94 89 <1 2 2 3 9 7 18 7 9 2008 <1 5 4 4 47 5 7 5 9 27 <1 85 75 3 15 7 12 18 13 30 17 18 2009 <1 1 2 3 38 4 8 2 9 43 <1 90 79 <1 15 19 17 13 7 17 10 19
102
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=147 % total % PNSP 85 15 60 40 6 3 55 27 8 37 25 2 36 <1 3 0 2 3 4 0 1 1 3 1 2 0 1 0 S. aureus n=398 % total % MRSA 100 59 39 2 10 4 48 29 8 23 33 11 33 <1 4 3 4 17 5 6 4 5 1 6 2 2 6 0 E. coli n=554 % total % FREC 99 1 39 60 1 3 3 40 48 6 17 41 6 35 <1 8 0 9 7 0 2 5 7 7 5 7 5 14 7 0 E. faecalis n=79 % total % VRE 100 59 41 17 <1 31 45 6 29 25 8 37 <1 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=79 % total % VRE 100 46 53 1 10 2 41 45 2 39 16 8 38 1 0 2 0 0 0 1 0 0 0 0 0 1 K. pneumoniae n=127 % total % CRKP 100 57 43 16 1 38 43 2 30 28 6 36 14 16 11 5 0 9 14 0 11 14 6 6 P. aeruginosa n=69 % total % CRPA 100 57 43 4 5 46 45 1 55 12 6 27 25 26 23 25 33 33 20 0 31 17 9 25 -
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
103
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Estonia
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
EE001 (0/35)
N laboratories Minimum First quartile Median Third quartile Maximum
7 0 0 0 4 13.3
EE009K (0/31)
N hospitals Minimum First quartile Median Third quartile Maximum
11 0 0 2 3.7 50
EE008V (0/16)
EE011 (0/6) EE002L (0/44)
EE010N (0/13)
EE009 (0/10)
EE011L (0/11)
Laboratory codes
EE005 (0/14)
Hospital codes 0 25 50 75 100
EE004P (1/51)
EE005P (1/34)
EE002 (1/36)
EE002M (2/66)
EE006K (1/27) EE004 (1/25)
EE001A (5/89)
EE006 (2/15) EE003R (5/10)
25
50
75
100
104
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 7 0 9.5 14.3 21.4 29.4
EE012P (0/7)
N hospitals Minimum First quartile Median Third quartile Maximum
12 0 2.5 7 11.3 23.5
EE002L (0/13)
EE010N (0/8)
EE005P (1/52)
EE002M (2/21)
EE009K (1/32)
EE001A (4/33) EE001A (7/141)
Hospital codes
Hospital codes 0 25 50 75 100
EE002M (7/102)
EE005P (1/7)
EE003R (1/14)
EE004P (8/73) EE004P (3/16)
EE008V (2/18)
EE006K (9/78)
EE006K (3/14)
EE002L (1/6)
EE009K (5/17) EE011L (4/17)
25
50
75
100
105
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Finland
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 15 454 16 517 17 548 17 543 15 501 16 547 15 643 20 688 S. aureus Labs Isolates 15 721 16 727 17 883 17 790 15 894 16 814 15 923 20 978 E. coli Labs Isolates 15 1 330 15 1 450 17 1 749 17 1 924 15 1 875 16 1 949 15 2 111 20 2 224 Enterecocci Labs Isolates 14 278 15 266 17 336 17 340 15 348 16 400 15 381 20 506 K. pneumoniae Labs Isolates 14 175 14 228 15 273 12 288 20 375 P. aeruginosa Labs Isolates 13 108 14 162 14 183 12 175 18 233
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2 6 14 <1 30 <1 6 <1 2 13 <1 80 <1 1 2003 2 10 20 1 33 1 5 1 <1 39 <1 79 4 <1 2004 <1 8 20 3 33 2 7 2 <1 39 <1 69 12 <1 2005 <1 7 20 3 35 2 7 2 <1 27 <1 78 1 <1 3 3 2 8 5 15 11 16 2006 2 12 24 3 36 2 8 2 <1 25 <1 80 16 <1 1 4 <1 8 3 8 8 17 2007 1 13 25 2 34 3 8 2 2 22 <1 87 19 <1 <1 <1 1 7 5 9 8 11 2008 <1 11 24 3 35 4 9 2 <1 13 <1 87 15 <1 1 2 2 8 5 6 6 15 2009 2 13 28 2 36 3 9 3 <1 <1 87 <1 1 3 1 7 5 8 4 11
106
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=1 294 % total % PNSP 96 4 56 44 1 15 4 49 33 <1 1 8 2 29 61 12 9 11 13 0 15 9 9 10 0 8 9 4 10 11 S. aureus n=1 901 % total % MRSA 100 62 38 1 4 5 44 48 <1 2 12 5 20 61 2 3 2 16 2 2 2 2 100 5 2 3 2 2 E. coli n=4 332 % total % FREC 100 <1 36 64 1 2 1 31 66 <1 1 8 4 22 65 9 13 11 8 13 2 7 7 8 0 8 6 8 7 8 E. faecalis n=475 % total % VRE 100 71 29 1 5 1 30 63 <1 3 10 8 18 60 0 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=398 % total % VRE 100 60 40 1 2 1 38 58 4 11 10 16 60 0 0 0 0 0 0 0 0 0 0 0 0 1 K. pneumoniae n=655 % total % CRKP 100 <1 56 44 1 2 1 31 67 2 9 5 21 63 2 0 1 2 17 14 0 2 1 0 2 1 2 1 P. aeruginosa n=404 % total % CRPA 97 3 64 36 1 <1 1 29 69 4 8 6 18 65 7 8 7 8 7 25 8 12 7 19 6 7 10 8
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
107
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Finland
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
FI019 (0/8)
FI015 (1/37)
N laboratories Minimum First quartile Median Third quartile Maximum
20 0 8.7 10.8 15.2 18.3
FI00HX (0/147)
FI00CX (0/53)
N hospitals Minimum First quartile Median Third quartile Maximum
24 0 0 1.8 3.1 12.8
FI009X (0/81) FI00C (2/26) FI018X (0/23) FI00E (8/99) FI003A (0/41) FI012 (4/47)
FI008X (0/28)
FI010 (6/68)
FI014X (0/28)
FI019X (0/23) FI00H (10/113) FI00AX (0/20) FI018 (1/11) FI003X (0/45) FI020 (7/72) FI00EX (1/155)
Laboratory codes
FI005 (8/76)
Hospital codes 0 25 50 75 100
FI015X (1/57)
FI009 (4/36)
FI021X (1/54)
FI002X (13/542) FI00L (2/17) FI011A (1/41) FI017 (5/41) FI017X (2/77) FI002 (55/391) FI014A (1/34) FI011 (9/61)
FI00LX (1/33)
FI00A (5/32)
FI011X (1/32)
FI010X (3/92) FI021 (4/25) FI00AA (1/25) FI014 (8/46) FI005X (5/124) FI008 (5/28) FI012X (3/60) FI003 (11/60)
FI020X (11/86)
25
50
75
100
108
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
24 2.5 5.8 8.8 9.4 17.4 N hospitals Minimum First quartile Median Third quartile Maximum 21 0 0 0 0 6
FI011A (2/79)
FI014A (2/66)
N hospitals Minimum First quartile Median Third quartile Maximum
FI010X (0/14)
FI011A (0/16)
FI008X (4/105) FI014X (0/15) FI009X (7/139) FI00LX (0/13) FI012X (6/117) FI021X (0/18) FI00AX (2/36) FI012X (0/20)
FI003A (7/117)
FI010X (14/226)
FI020X (0/27)
FI015X (9/127)
FI011X (0/14)
FI00HX (29/376)
FI00CX (0/35)
FI005X (21/267) FI003A (0/14)
Hospital codes
FI021X (10/115)
Hospital codes 0 25 50 75 100
FI005X (0/33)
FI003X (11/123)
FI00AX (0/10)
FI017X (18/201) FI015X (0/15)
FI00LX (9/99)
FI00CX (12/130)
FI009X (0/32)
FI020X (9/97)
FI003X (0/13)
FI00AA (4/43)
FI019X (0/6)
FI00EX (27/287) FI008X (0/8) FI002X (154/1348) FI00HX (1/57) FI011X (9/74) FI002X (5/215) FI019X (5/41) FI017X (1/30)
FI014X (9/73)
FI018X (8/46)
FI00EX (3/50)
25
50
75
100
109
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
France
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 195 632 97 371 168 663 127 557 225 826 S. aureus Labs Isolates 21 1 664 21 1 710 50 3 355 50 3 484 50 3 824 57 4 265 56 4 380 54 4 727 E. coli Labs Isolates 21 2 495 21 2 266 50 5 678 50 6 056 50 6 718 57 8 093 56 7 993 54 8 451 Enterecocci Labs Isolates 21 467 20 468 46 871 47 1 023 50 1 152 56 1 545 54 1 555 54 1 969 K. pneumoniae Labs Isolates 49 838 50 963 56 1 187 54 1 138 52 1 378 P. aeruginosa Labs Isolates 48 993 47 1 006 56 1 305 54 1 225 32 1 221
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 33 52 4 8 <1 5 15 <1 34 10 2 2003 29 50 5 9 <1 3 16 <1 30 23 <1 2004 29 47 4 8 <1 1 17 <1 56 21 5 2005 5 36 41 27 50 5 11 1 <1 15 <1 64 24 3 5 7 4 15 9 14 22 27 2006 4 32 36 27 53 6 14 2 1 16 <1 69 30 3 7 9 6 11 6 12 16 23 2007 4 34 37 26 54 6 15 2 1 15 <1 67 30 1 11 14 10 11 7 14 18 24 2008 7 30 31 24 54 7 16 4 <1 18 <1 68 30 <1 17 21 15 14 8 14 15 22 2009 6 27 27 23 55 8 19 7 1 18 <1 63 38 <1 20 24 19 21 17 17 19 25
110
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=1 383 % total % PNSP 69 31 55 44 <1 25 11 32 32 <1 73 27 29 26 26 31 20 35 16 26 39 25 33 27 S. aureus n=9 096 % total % MRSA 100 61 38 2 4 3 41 52 <1 17 34 15 32 2 24 23 24 22 12 9 19 34 40 28 28 26 24 23 E. coli n=15 838 % total % FREC 100 47 51 2 2 1 35 61 <1 9 29 12 49 2 17 20 15 17 4 8 13 14 9 15 14 15 13 16 E. faecalis n=2 431 % total % VRE 100 64 35 2 3 1 39 56 <1 24 28 17 29 2 0 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=944 % total % VRE 100 60 38 2 3 1 44 51 <1 24 26 17 32 1 1 1 0 0 0 0 2 1 11 2 1 2 2 0 K. pneumoniae n=2 516 % total % CRKP 100 58 40 2 2 1 45 51 <1 15 30 16 36 3 17 20 14 5 14 18 14 9 56 24 9 15 6 14 P. aeruginosa n=2 442 % total % CRPA 100 60 39 1 2 2 48 48 <1 29 24 12 32 2 16 16 15 26 5 14 19 11 17 23 11 14 10 10
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
111
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
France
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
FR009 (0/8) FR306 (0/6) FR025 (0/6) FR172 (0/6) FR162 (0/5) FR112 (0/5) FR120 (0/8) FR519 (0/6) FR473 (1/11) FR022 (1/10) FR043 (1/9) FR250 (1/8) FR251 (1/8) FR150 (1/7) FR088 (1/7) FR037 (1/7) FR100 (1/7) FR137 (4/26) FR490 (1/6) FR505 (1/6) FR148 (1/6) FR265 (2/12) FR279 (2/12) FR167 (3/17) FR036 (4/22) FR032 (1/5) FR466 (1/5) FR492 (1/5) FR241 (1/5) FR077 (2/10) FR470 (2/10) FR228 (1/5) FR108 (4/19) FR186 (4/18) FR232 (2/9) FR476 (4/18) FR213 (4/17) FR164 (6/25) FR047 (2/8) FR499 (5/20) FR008 (2/8) FR010 (11/43) FR249 (3/11) FR094 (11/40) FR071 (4/14) FR006 (10/34) FR076 (6/20) FR514 (3/10) FR269 (12/37) FR109 (13/40) FR270 (2/6) FR246 (13/39) FR260 (3/9) FR079 (2/6) FR020 (3/9) FR219 (2/6) FR277 (2/6) FR467 (11/31) FR263 (14/39) FR999 (4/11) FR116 (3/8) FR130 (6/16) FR125 (4/10) FR274 (2/5) FR230 (2/5) FR131 (4/10) FR235 (2/5) FR035 (2/5) FR194 (4/10) FR224 (3/7) FR244 (3/7) FR226 (3/7) FR493 (3/7) FR271 (6/14) FR041 (3/7) FR214 (14/32) FR028 (3/6) FR142 (3/6) FR403 (3/6) FR479 (16/31) FR104 (3/5) FR198 (3/5) FR064 (6/7)
N laboratories Minimum First quartile Median Third quartile Maximum
83 0 16.7 25.6 40 85.7
FR202A (3/25) FR084A (6/46) FR401A (7/50) FR164A (40/251) FR095A (6/37) FR040A (48/290) FR226A (85/504) FR010A (54/320) FR105A (22/124) FR165A (32/174) FR211A (8/43) FR362A (22/115) FR072A (17/88) FR248A (46/237) FR145A (10/50) FR238A (75/359) FR135A (14/66) FR134A (23/107) FR263A (134/603) FR094A (63/283) FR213A (26/115) FR126A (20/88) FR237A (20/88) FR138A (75/329) FR403A (13/57) FR008A (8/35) FR109A (60/262) FR249A (42/183) FR276A (23/100) FR400A (9/39) FR121A (47/203) FR250A (46/195) FR076A (73/306) FR434A (22/91) FR214A (16/66) FR006A (125/510) FR246A (39/154) FR052A (73/285) FR224A (26/101) FR194A (31/120) FR055A (14/54) FR037A (10/37) FR015A (14/51) FR064A (57/204) FR009A (32/114) FR193A (13/45) FR120A (19/64) FR067A (48/160) FR130A (120/387) FR259A (48/152) FR479A (119/365) FR098A (18/52) FR046A (16/45) FR260A (55/150) FR208A (15/34) FR179A (38/80)
N hospitals Minimum First quartile Median Third quartile Maximum
56 12 19.7 23 27.2 47.5
Laboratory codes
25
50
75
100
Hospital codes
25
50
75
100
112
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
FR098A (0/10) FR194A (0/15) FR067A (0/30) FR008A (0/9) FR145A (0/8) FR260A (0/29) FR400A (0/11) FR109A (0/80) FR072A (0/8) FR130A (0/43) FR276A (0/20) FR135A (0/14) FR237A (0/13) FR211A (0/17) FR208A (0/8) FR202A (0/11) FR040A (1/46) FR362A (1/31) FR052A (1/29) FR250A (2/50) FR094A (4/79) FR434A (1/19) FR249A (2/28) FR076A (6/84) FR010A (4/49) FR126A (3/31) FR238A (5/47) FR105A (8/73) FR006A (17/154) FR037A (1/9) FR224A (2/18) FR401A (5/42) FR009A (3/25) FR263A (22/178) FR248A (11/84) FR479A (12/88) FR084A (2/14) FR164A (1/7) FR134A (4/27) FR120A (3/20) FR214A (4/25) FR055A (4/25) FR165A (13/79) FR064A (8/47) FR259A (12/67) FR015A (3/16) FR403A (7/34) FR121A (13/59) FR179A (10/43) FR213A (11/47) FR246A (12/46) FR193A (5/19) FR095A (4/13) FR046A (5/16) FR226A (96/225) FR138A (102/197) N hospitals Minimum First quartile Median Third quartile Maximum 56 0 0 11 16.2 51.8
FR145A (4/56) FR008A (10/122) FR135A (10/120) FR194A (19/196) FR250A (45/434) FR226A (73/695) FR238A (56/519) FR067A (36/321) FR130A (64/564) FR211A (14/122) FR400A (15/127) FR202A (16/131) FR072A (18/147) FR134A (34/268) FR276A (28/220) FR434A (32/248) FR260A (36/275) FR208A (10/76) FR120A (20/151) FR121A (41/305) FR193A (13/92) FR403A (18/127) FR249A (46/317) FR009A (36/240) FR214A (19/120) FR224A (34/214) FR040A (64/398) FR263A (82/501) FR010A (80/488) FR126A (42/250) FR037A (16/95) FR401A (20/118) FR094A (78/445) FR164A (63/358) FR084A (15/81) FR109A (116/622) FR362A (51/270) FR213A (56/293) FR052A (92/480) FR098A (36/177) FR237A (43/208) FR076A (113/546) FR246A (67/314) FR105A (69/320) FR248A (71/323) FR095A (11/50) FR006A (202/909) FR055A (22/96) FR479A (127/548) FR165A (77/330) FR138A (141/599) FR015A (28/115) FR064A (103/405) FR259A (74/248) FR046A (13/34) FR179A (6/10)
N hospitals Minimum First quartile Median Third quartile Maximum
56 7.1 12.7 16.4 21 60
Hospital codes
25
50
75
100
Hospital codes
25
50
75
100
113
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Germany
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 17 248 17 175 16 145 15 119 15 85 11 75 11 209 16 346 S. aureus Labs Isolates 18 1 067 20 920 22 1 107 17 827 18 799 12 853 14 1 090 17 1 894 E. coli Labs Isolates 16 1 068 19 997 22 1 217 17 961 18 850 12 977 14 1 615 17 2 803 Enterecocci Labs Isolates 14 290 17 347 22 606 17 569 16 529 12 648 13 451 17 952 K. pneumoniae Labs Isolates . . . . . . 12 105 14 148 10 173 11 235 15 479 P. aeruginosa Labs Isolates . . . . 12 12 11 11 16 117 162 197 167 287
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 1 14 18 50 5 15 <1 10 42 <1 80 68 4 2003 <1 1 11 18 47 5 14 <1 7 47 <1 78 47 3 2004 <1 1 13 20 55 4 24 2 7 42 <1 93 61 11 2005 <1 4 17 21 54 6 23 2 3 34 <1 96 52 10 10 6 7 18 11 25 12 23 2006 1 5 12 20 60 10 29 4 3 29 <1 94 38 8 12 12 14 17 12 17 18 28 2007 <1 3 8 16 55 6 30 8 7 67 <1 95 73 15 6 9 6 17 17 22 9 28 2008 <1 5 10 19 55 7 23 5 <1 39 <1 95 35 6 10 15 11 9 8 11 10 22 2009 <1 2 8 18 56 8 23 8 3 40 <1 94 45 6 10 15 13 13 11 11 7 17
114
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=527 % total % PNSP 93 7 36 29 35 11 3 38 48 <1 21 46 2 27 4 3 5 3 5 3 6 4 2 2 0 3 2 0 3 0 S. aureus n=2 974 % total % MRSA 100 43 24 33 2 2 35 60 <1 20 42 12 22 4 19 19 18 20 5 9 17 21 7 25 17 21 17 21 E. coli n=4 396 % total % FREC 100 <1 30 37 32 2 1 29 69 <1 14 49 8 25 4 24 0 28 21 22 3 22 26 22 16 23 20 26 29 18 E. faecalis n=816 % total % VRE 100 49 21 31 3 1 38 57 <1 26 35 12 25 3 0 1 0 0 0 0 0 0 0 1 0 0 0 0 E. faecium n=583 % total % VRE 100 48 28 24 3 1 46 50 <1 37 24 13 25 1 6 6 5 8 2 24 10 8 0 7 9 5 15 4 K. pneumoniae n=706 % total % CRKP 100 <1 43 28 28 3 1 33 63 0 20 38 12 28 2 13 0 13 9 15 9 25 16 9 0 10 8 7 18 8 P. aeruginosa n=450 % total % CRPA 99 1 46 24 30 3 2 37 58 <1 21 31 12 33 2 10 33 10 13 10 10 19 22 12 100 23 11 13 18 9
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
115
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Germany
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
DE1302 (0/6)
N laboratories Minimum First quartile Median Third quartile Maximum
15 0 0 2.6 5.7 15.4
DE0402 (0/8)
DE0907 (0/82)
DE0908 (0/26)
DE0401 (0/18)
DE1303 (0/5)
DE0202 (0/5)
DE0301 (1/39)
DE0107 (1/29)
DE0911 (3/76)
DE0110 (7/162)
DE0102 (2/35)
DE1203 (1/11)
DE0111 (1/9)
DE0909 (2/13)
DE091112 (0/5) DE010702 (0/7) DE011087 (0/7) DE030107 (0/6) DE091110 (0/5) DE011041 (0/6) DE091114 (0/5) DE090807 (0/10) DE091116 (0/7) DE090819 (0/12) DE40202 (0/5) DE091106 (0/14) DE0401D (0/7) DE011039 (0/14) DE011086 (0/12) DE011044 (0/12) DE2020 (3/52) DE091117 (2/33) DE091120 (1/15) DE090802 (1/15) DE0102B (1/15) DE091131 (1/14) DE091105 (1/14) DE011083 (3/40) DE011001 (1/13) DE090718 (1/13) DE011028 (1/12) DE011018 (1/12) DE040201 (1/12) DE0401A (11/127) DE011007 (2/23) DE011017 (2/22) DE040204 (1/11) DE070102 (1/11) DE010701 (4/43) DE0102A (17/169) DE011061 (1/9) DE011029 (1/9) DE011006 (1/9) DE011101 (9/79) DE011010 (3/26) DE090804 (1/8) DE011026 (2/15) DE011062 (2/14) DE070101 (17/113) DE091135 (2/13) DE091143 (2/13) DE130201 (7/45) DE011003 (3/19) DE090701 (10/61) DE090708 (6/36) DE090704 (5/30) DE090906 (2/12) DE091107 (1/6) DE040202 (1/6) DE091129 (2/12) DE090812 (1/6) DE011012 (3/17) DE011038 (7/39) DE090705 (17/91) DE011021 (6/32) DE090901 (3/16) DE030103 (4/21) DE011024 (7/36) DE090801 (10/51) DE091101 (4/20) DE091102 (3/15) DE070103 (3/15) DE130320 (1/5) DE090709 (9/44) DE120301 (28/135) DE090715 (4/19) DE011034 (4/18) DE011004 (4/18) DE011022 (4/18) DE091133 (5/22) DE011025 (6/26) DE030101 (8/34) DE090716 (17/72) DE091132 (8/33) DE011014 (6/24) DE011031 (4/16) DE011016 (5/20) DE011058 (3/12) DE090707 (8/32) DE090706 (10/39) DE030110 (11/42) DE090903 (5/19) DE011085 (4/15) DE090710 (4/15) DE091126 (7/26) DE091134 (3/11) DE090808 (3/11) DE0401B (3/11) DE011042 (3/11) DE011045 (5/18) DE091122 (7/25) DE011066 (4/14) DE090803 (4/14) DE090905 (13/44) DE090713 (3/10) DE011020 (11/36) DE030109 (11/36) DE030108 (13/41) DE011005 (3/9) DE090714 (5/15) DE091127 (4/11) DE090806 (13/34) DE091108 (2/5) DE091125 (7/17) DE011015 (3/7) DE130307 (7/16) DE011063 (4/9) DE030102 (5/11) DE091119 (5/11) DE011068 (4/7) DE090814 (4/7) DE011037 (11/19) DE090902 (3/5) DE011067 (3/5)
N hospitals Minimum First quartile Median Third quartile Maximum
120 0 8.7 18.7 26.8 60
Laboratory codes
25
50
75
100
Hospital codes
25
50
75
100
116
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
DE090706 (0/5) DE0401D (0/7) DE030101 (0/13) DE011021 (0/11) DE030110 (0/10) DE130201 (0/10) DE011007 (0/5) DE011022 (0/7) DE011031 (0/10) DE040201 (0/6) DE030103 (0/9) DE0401A (0/20) DE011001 (0/6) DE090802 (0/7) DE090708 (0/5) DE091105 (0/6) DE090710 (0/5) DE030109 (0/8) DE090705 (1/14) DE011101 (3/40) DE070101 (2/24) N hospitals Minimum First quartile Median Third quartile Maximum 47 0 0 10.5 16.7 60
DE090804 (0/7) DE011041 (0/9) DE090808 (0/7) DE011028 (0/14) DE011009 (0/5) DE090807 (1/17) DE090802 (2/31) DE011029 (2/23) DE010702 (2/22) DE011038 (4/39) DE010701 (9/83) DE040201 (3/27) DE091129 (2/18) DE011044 (1/9) DE091131 (3/27) DE091117 (3/25) DE090715 (6/49) DE091107 (2/16) DE091134 (1/8) DE011061 (4/31) DE091104 (2/15) DE040202 (3/22) DE011086 (3/21) DE030103 (5/34) DE090901 (7/47) DE090905 (12/80) DE090803 (3/20) DE011042 (6/39) DE011015 (2/13) DE040204 (3/19) DE030110 (13/78) DE011039 (3/18) DE011031 (6/36) DE010703 (2/12) DE011087 (1/6) DE090904 (1/6) DE011012 (7/41) DE011018 (4/23) DE091122 (9/51) DE011068 (4/22) DE091125 (5/27) DE091126 (8/41) DE011010 (9/46) DE011088 (1/5) DE091121 (2/10) DE091108 (3/15) DE091143 (4/20) DE090706 (9/44) DE2020 (8/39) DE090806 (5/24) DE090801 (16/76) DE0401A (23/109) DE011025 (10/47) DE090708 (11/51) DE011024 (13/60) DE090902 (2/9) DE091132 (9/40) DE011062 (7/31) DE030102 (5/22) DE090705 (13/57) DE0102A (58/254) DE090906 (8/35) DE011022 (12/52) DE091127 (3/13) DE011063 (3/13) DE090716 (34/146) DE011034 (8/34) DE090903 (6/25) DE091102 (7/29) DE130201 (13/53) DE0401B (3/12) DE090718 (3/12) DE091120 (7/28) DE130307 (3/12) DE011019 (4/16) DE011067 (2/8) DE011027 (2/8) DE030109 (16/63) DE090701 (22/86) DE011026 (10/39) DE011037 (8/31) DE090819 (6/23) DE011003 (6/23) DE030101 (19/72) DE011004 (4/15) DE090714 (4/15) DE090704 (7/26) DE011014 (13/48) DE091133 (6/22) DE011085 (5/18) DE070101 (42/151) DE090710 (7/25) DE091106 (4/14) DE130320 (4/14) DE011083 (14/49) DE011020 (20/70) DE011045 (10/34) DE011017 (9/30) DE091101 (10/33) DE011021 (17/56) DE091105 (8/26) DE011001 (8/26) DE120301 (49/152) DE011016 (10/31) DE011066 (14/43) DE090709 (28/86) DE090719 (3/9) DE091135 (13/38) DE090713 (10/28) DE090707 (6/16) DE011007 (12/32) DE070103 (7/18) DE030108 (13/33) DE011101 (54/131) DE011032 (3/7) DE011002 (3/7) DE030106 (3/7) DE011005 (6/13) DE030107 (8/17) DE091119 (4/8) DE011006 (6/11)
N hospitals Minimum First quartile Median Third quartile Maximum
121 0 16.7 22.8 27.8 54.5
Hospital codes
Hospital codes 0 25 50 75 100
DE011020 (1/10) DE011083 (1/10) DE090716 (2/19) DE090801 (1/9) DE120301 (5/41) DE090707 (1/8) DE0102A (5/36) DE090906 (1/7) DE090715 (1/7) DE011025 (1/7) DE090905 (3/20) DE090806 (2/12) DE091131 (1/6) DE011012 (1/6) DE090701 (2/12) DE090803 (1/6) DE030108 (1/6) DE011015 (1/6) DE090709 (3/16) DE2020 (2/10) DE090901 (2/9) DE011038 (2/8) DE011024 (3/7) DE011034 (3/6) DE090713 (3/5) DE011079 (3/5)
25
50
75
100
117
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Greece
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates S. aureus Labs Isolates 33 368 34 682 35 610 35 682 42 828 41 819 46 907 48 1 025 E. coli Labs Isolates 35 588 35 1 076 39 1 131 35 1 140 41 1 253 43 1 234 44 1 462 49 1 831 Enterecocci Labs Isolates 28 292 32 621 34 565 34 737 39 949 39 999 42 992 47 1 190 K. pneumoniae Labs Isolates 33 774 38 841 38 972 41 1 093 47 1 649 P. aeruginosa Labs Isolates 33 699 38 818 37 802 42 920 47 1 123
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 44 45 7 13 6 4 60 13 75 52 19 2003 45 44 6 12 6 4 52 7 89 40 18 2004 44 46 6 12 6 4 59 4 84 52 20 2005 42 46 7 12 7 3 54 4 85 34 37 60 54 61 30 27 39 40 39 2006 43 46 7 14 6 5 57 5 88 35 42 54 50 58 39 34 48 47 45 2007 48 48 9 19 8 4 65 7 91 44 37 54 55 62 38 40 47 49 50 2008 41 50 15 22 10 3 52 7 85 52 28 55 64 66 34 37 49 48 48 2009 40 51 14 23 10 4 61 6 86 63 27 60 66 69 33 34 44 41 45
118
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=. % total % PNSP S. aureus n=1 855 % total % MRSA 100 8 4 88 3 <1 2 2 93 14 67 12 3 5 41 38 36 41 41 0 33 54 43 65 37 58 33 43 E. coli n=3 252 % total % FREC 99 1 6 8 86 3 <1 2 2 92 4 77 11 3 5 23 0 23 19 23 17 0 14 23 17 24 16 24 5 15 E. faecalis n=1 341 % total % VRE 100 6 4 90 4 <1 1 3 92 35 46 14 1 3 6 4 2 7 9 0 6 5 6 10 4 4 2 10 E. faecium n=803 % total % VRE 100 9 7 84 5 3 3 90 32 48 14 2 4 27 28 25 28 38 46 33 30 34 31 24 32 26 K. pneumoniae n=2 714 % total % CRKP 98 2 6 4 90 6 <1 2 2 91 46 36 13 3 2 67 77 59 63 68 74 0 52 56 64 87 39 62 32 40 P. aeruginosa n=2 011 % total % CRPA 95 5 6 3 91 4 <1 2 2 92 44 38 14 1 2 45 72 38 48 47 50 0 40 24 46 58 33 44 20 27
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
119
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Greece
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
No data reported
GR048X (0/13) GR018X (3/19) GR066X (7/35) GR044X (2/10) GR035X (16/75) GR027X (11/49) GR028X (14/58) GR055X (3/12) GR047X (32/118) GR009X (2/7) GR013X (18/57) GR075X (25/73) GR031X (25/72) GR010X (15/42) GR015X (17/46) GR008X (8/21) GR049X (8/21) GR052X (2/5) GR070X (13/32) GR032X (7/17) GR051X (8/19)
N hospitals Minimum First quartile Median Third quartile Maximum
47 0 34.2 43.9 52.4 100
Hospital codes
GR033X (19/45) GR043X (29/67) GR068X (18/41) GR007X (26/59) GR040X (90/202) GR042X (17/37) GR030X (43/93) GR050X (13/28) GR022X (7/15) GR037X (35/75) GR059X (27/57) GR024X (18/37) GR026X (7/14) GR071X (3/6) GR005X (11/21) GR038X (7/13) GR001X (28/50) GR060X (4/7) GR014X (26/45) GR011X (7/12) GR004X (9/15) GR012X (15/25) GR039X (37/58) GR072X (8/12) GR062X (7/10) GR057X (7/7)
25
50
75
100
120
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 44 16.7 48.4 62.5 76.8 86.3
GR057X (0/5) GR011X (1/26) GR026X (2/25) GR052X (4/46) GR048X (2/22) GR071X (2/22) GR062X (2/18) GR010X (5/44)
N hospitals Minimum First quartile Median Third quartile Maximum
47 0 14.3 23.2 28 51.9
GR062X (1/6) GR066X (2/10) GR004X (2/10) GR044X (2/8) GR008X (2/8) GR028X (28/81) GR027X (33/91) GR051X (4/11)
GR031X (14/112) GR050X (10/76) GR051X (3/22) GR066X (6/42) GR027X (18/117) GR009X (2/13) GR068X (7/43) GR008X (6/36) GR060X (2/12) GR022X (3/16) GR043X (14/74) GR028X (49/254) GR035X (28/138) GR055X (11/29) GR018X (5/12) GR047X (66/141) GR032X (4/8) GR038X (4/8) GR070X (23/45) GR042X (8/14) GR049X (8/14) GR075X (45/78) GR048X (10/17) GR071X (3/5) GR059X (36/59)
Hospital codes
Hospital codes 0 25 50 75 100
GR001X (25/119) GR042X (15/65) GR047X (64/276) GR038X (13/55) GR014X (22/93) GR005X (14/58) GR024X (20/82) GR004X (5/20) GR015X (27/108) GR030X (37/147) GR075X (31/120) GR044X (12/46) GR033X (19/72) GR070X (12/43) GR040X (76/271) GR012X (11/39) GR039X (15/51) GR059X (24/78)
GR035X (78/127) GR011X (10/16) GR072X (10/16) GR013X (11/17) GR030X (112/164) GR010X (41/59) GR039X (139/197) GR037X (83/117) GR043X (65/90) GR001X (74/102) GR022X (8/11) GR050X (35/48) GR014X (62/81) GR031X (104/135) GR040X (253/324) GR033X (47/60) GR024X (44/56)
GR032X (9/27) GR007X (16/48) GR018X (14/41) GR055X (24/70) GR037X (22/63) GR013X (21/56) GR072X (5/12) GR049X (14/27) GR012X (52/66) GR057X (4/5) GR026X (12/15) GR068X (84/104) GR007X (52/63) GR005X (51/61) GR015X (101/117)
25
50
75
100
121
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Hungary
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 17 61 20 134 26 143 23 133 23 151 22 146 22 166 22 143 S. aureus Labs Isolates 24 416 27 858 30 1 020 28 1 083 27 1 127 26 1 199 26 1 181 26 1 068 E. coli Labs Isolates 24 354 27 842 28 967 27 1 046 26 1 135 25 1 179 25 1 057 25 1 057 Enterecocci Labs Isolates 23 169 25 279 26 366 27 476 25 453 26 400 21 428 27 444 K. pneumoniae Labs Isolates 21 314 24 302 23 322 23 369 24 361 P. aeruginosa Labs Isolates 24 507 25 546 24 518 25 513 25 518
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 3 23 21 9 45 6 10 2 2 100 <1 89 100 <1 2003 3 24 25 15 49 8 15 <1 <1 87 <1 91 96 <1 2004 <1 16 25 17 55 10 19 3 2 57 <1 95 80 <1 2005 4 21 32 20 51 9 22 4 1 43 <1 91 64 <1 26 21 28 10 10 18 32 28 2006 1 18 19 25 53 12 27 5 3 47 <1 88 67 <1 20 13 20 9 8 16 23 21 2007 5 23 36 23 54 11 26 5 2 48 <1 88 53 <1 29 22 25 11 9 19 26 24 2008 8 27 32 23 59 13 26 9 3 53 <1 96 62 3 36 33 35 13 11 26 26 26 2009 3 12 19 29 60 16 30 13 2 51 <1 97 70 1 40 33 38 19 12 27 29 27
122
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=309 % total % PNSP 71 29 82 18 1 12 5 55 29 26 19 2 44 9 22 14 21 16 0 36 22 18 18 20 16 24 22 21 S. aureus n=2 249 % total % MRSA 100 89 11 1 2 2 48 49 <1 18 28 12 30 12 26 26 23 16 8 8 21 23 0 30 18 28 17 18 E. coli n=2 091 % total % FREC 100 84 16 1 2 1 41 56 <1 12 29 7 41 11 28 30 22 13 7 23 23 25 0 23 20 26 25 25 E. faecalis n=716 % total % VRE 100 93 7 1 4 2 46 48 31 20 11 28 11 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=147 % total % VRE 100 93 7 1 5 1 49 44 36 14 12 28 9 2 1 10 0 0 0 1 0 0 0 0 2 0 K. pneumoniae n=728 % total % CRKP 99 1 91 9 1 9 2 44 45 27 19 11 33 10 37 40 38 26 17 35 32 33 26 38 22 28 27 34 P. aeruginosa n=1 010 % total % CRPA 98 2 90 10 1 4 2 50 44 39 12 12 27 10 26 25 26 31 7 13 28 24 18 24 13 19 22 19
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
123
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Hungary
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
HU023 (0/7)
HU033 (0/8)
N laboratories Minimum First quartile Median Third quartile Maximum
17 0 9.1 21.7 33.3 50
HU001R (0/5) HU022A (0/8) HU034C (0/6) HU006W (0/5) HU005J (2/19) HU024A (5/44)
N hospitals Minimum First quartile Median Third quartile Maximum
42 0 15.4 20 30.5 61.8
HU020 (1/16)
HU020L (4/32) HU002G (4/32)
HU026 (1/13)
HU032A (15/119) HU019A (17/111) HU006B (6/39)
HU002 (1/11)
HU027A (7/45) HU026A (16/97)
HU034 (1/10)
HU019H (1/6) HU016G (1/6) HU002M (1/6)
HU022 (10/70) HU025A (14/82) HU022P (7/40) HU009 (5/31) HU028A (32/181)
Laboratory codes
Hospital codes 0 25 50 75 100
HU034A (13/69) HU031A (1/5) HU001Q (1/5) HU022I (26/129) HU019G (14/63) HU023A (7/29) HU035A (12/46)
HU019 (5/23)
HU028 (2/8)
HU032 (5/19) HU004G (5/19) HU007C (4/15) HU029 (9/30) HU009B (14/52) HU023D (26/86) HU024 (2/6) HU007B (10/33) HU023I (18/59) HU029V (65/206) HU027 (4/11) HU006A (11/30) HU020C (3/8) HU025 (7/18) HU009A (59/152) HU012G (11/27) HU020A (18/42) HU005 (2/5) HU033A (55/128) HU008F (4/8) HU006 (3/6) HU005A (37/66) HU022S (21/34)
25
50
75
100
124
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 28 0 16.3 28.9 48.1 75
HU001R (0/5) HU005J (0/6) HU004G (1/16) HU035A (2/28) HU016D (1/12) HU022P (2/20) HU012G (2/19)
N hospitals Minimum First quartile Median Third quartile Maximum
36 0 16 25 30.7 52.2
HU020L (0/5) HU024A (0/5) HU035A (0/9) HU005J (0/8) HU009B (1/10) HU019G (1/10)
HU020L (4/35) HU007B (4/25) HU006A (4/25) HU023I (6/37) HU026A (4/22) HU002G (6/33) HU019A (17/92) HU024A (8/42) HU023A (5/24) HU026A (11/51) HU023A (3/12) HU004G (1/5) HU019A (4/19) HU025A (9/37) HU022I (4/25) HU023I (2/12)
Hospital codes
Hospital codes 0 25 50 75 100
HU027A (15/63) HU034C (2/8) HU031A (2/8) HU006B (6/24) HU023D (11/41) HU022I (70/260) HU033A (27/100) HU020A (12/44) HU009B (13/47)
HU027A (3/11) HU005A (7/23) HU028A (31/96) HU034A (11/29) HU033A (13/34) HU023D (5/12) HU029V (43/101)
HU034A (21/74) HU029V (58/197) HU025A (33/103) HU019G (20/61) HU022S (7/13) HU032A (38/115) HU002B (2/6) HU020C (4/11) HU028A (68/184) HU005A (13/31) HU009A (22/35) HU022S (21/46) HU009A (72/138) HU031A (6/8) HU020A (7/13) HU012G (5/9) HU007B (9/16) HU002G (9/19) HU032A (45/92)
25
50
75
100
125
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Iceland
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 2 43 2 35 2 54 2 37 2 52 2 42 2 46 2 35 S. aureus Labs Isolates 2 60 2 64 2 55 2 78 2 57 2 65 2 63 2 59 E. coli Labs Isolates 2 83 2 100 2 119 2 130 2 130 2 105 2 123 2 111 Enterecocci Labs Isolates 2 25 2 22 1 27 2 31 2 40 1 29 2 17 2 51 K. pneumoniae Labs Isolates 2 22 2 13 2 27 1 24 2 27 P. aeruginosa Labs Isolates 1 13 1 9 1 11 2 7 2 16
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2 5 5 <1 19 1 3 <1 <1 6 <1 29 <1 <1 2003 <1 9 20 <1 42 2 6 1 <1 <1 <1 57 <1 <1 2004 2 17 8 <1 43 <1 2 <1 <1 5 <1 63 13 <1 2005 <1 8 17 <1 38 <1 3 <1 <1 <1 <1 80 <1 <1 <1 <1 <1 8 8 8 <1 <1 2006 <1 6 10 <1 45 7 12 <1 7 3 <1 56 14 <1 <1 <1 <1 <1 <1 <1 <1 <1 2007 2 7 17 <1 46 6 17 2 <1 13 <1 57 14 <1 <1 <1 <1 <1 <1 <1 <1 <1 2008 <1 9 22 2 44 7 6 <1 <1 30 <1 43 43 <1 4 8 4 <1 <1 <1 <1 <1 2009 <1 <1 3 <1 50 7 7 2 <1 15 <1 68 36 8 <1 <1 <1 6 <1 <1 13
126
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=81 % total % PNSP 96 4 51 49 1 22 3 38 38 3 8 <1 64 25 5 0 2 8 0 9 0 9 7 0 4 0 9 7 S. aureus n=122 % total % MRSA 100 61 39 1 5 9 40 46 <1 4 16 6 49 25 1 1 0 16 0 0 1 0 0 0 0 0 0 0 E. coli n=214 % total % FREC 100 <1 44 56 1 4 1 31 64 2 9 4 61 25 7 0 9 4 13 3 0 9 6 0 6 12 8 3 E. faecalis n=36 % total % VRE 100 78 22 1 4 29 67 12 16 8 41 23 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=32 % total % VRE 100 50 50 1 1 1 26 71 12 10 10 48 21 6 13 0 0 0 0 5 2 0 0 0 5 0 K. pneumoniae n=51 % total % CRKP 100 53 47 1 37 63 3 16 8 71 3 2 0 4 17 2 0 0 0 0 1 0 P. aeruginosa n=23 % total % CRPA 100 74 26 1 2 27 71 7 16 2 71 4 0 0 0 7 0 0 3 0 0 0 3 0
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
127
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Iceland
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum
2 0 0 2.8 5.6 5.6
N hospitals Minimum First quartile Median Third quartile Maximum
2 0 0 0.5 1 1
IS003 (0/10)
IS003A (0/16)
Laboratory codes
IS001 (4/71)
Hospital codes
IS001A (1/100)
25
50
75
100
25
50
75
100
128
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
4 0 0 0 3.8 7.7 N hospitals Minimum First quartile Median Third quartile Maximum 1 2.1 2.1 2.1 2.1 2.1
N hospitals Minimum First quartile Median Third quartile Maximum IS001B (0/8)
IS001C (0/10)
Hospital codes
Hospital codes
IS001G (0/6) IS001A (14/183)
IS001A (1/48)
25
50
75
100
25
50
75
100
129
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Ireland
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 20 277 24 363 28 399 31 397 32 406 33 435 35 442 34 356 S. aureus Labs Isolates 22 998 26 1 108 38 1 286 38 1 360 38 1 347 41 1 332 38 1 242 41 1 261 E. coli Labs Isolates 20 736 26 978 37 1 235 39 1 424 39 1 638 42 1 750 41 1 875 41 2 012 Enterecocci Labs Isolates 15 250 21 348 29 418 33 502 32 550 37 598 37 685 38 671 K. pneumoniae Labs Isolates 15 42 28 211 31 237 33 307 37 316 P. aeruginosa Labs Isolates 11 29 23 128 29 172 29 191 30 236
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2 12 13 42 62 3 5 2 8 39 2 89 17 11 2003 3 12 12 42 61 4 10 2 5 32 <1 91 54 19 2004 3 10 14 41 65 5 12 2 <1 42 1 96 56 22 2005 3 11 12 42 67 7 17 4 4 42 3 93 52 31 5 3 7 7 10 11 7 14 2006 3 16 16 42 69 7 21 4 5 43 3 94 44 36 9 16 9 7 6 9 9 17 2007 6 17 17 38 65 10 21 5 2 38 3 93 36 33 10 17 8 6 5 9 10 18 2008 6 23 17 33 67 9 23 6 <1 31 3 95 27 35 9 11 11 5 4 6 6 16 2009 6 20 17 27 66 9 22 6 3 34 <1 93 38 38 11 11 11 4 6 8 6 9
130
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=797 % total % PNSP 96 4 57 43 <1 16 4 37 42 <1 3 17 2 28 50 22 19 21 22 0 19 9 12 18 14 13 16 22 15 15 S. aureus n=2 503 % total % MRSA 100 63 37 <1 6 4 40 50 <1 4 15 7 17 57 30 30 30 50 13 11 31 49 43 53 43 49 28 38 E. coli n=3 861 % total % FREC 100 <1 45 55 <1 3 1 32 62 <1 3 15 7 22 54 22 0 27 18 25 3 5 17 20 16 20 17 19 12 21 E. faecalis n=578 % total % VRE 100 61 39 <1 8 1 37 53 <1 6 14 7 15 58 2 1 3 0 0 4 3 2 0 0 1 3 1 3 E. faecium n=776 % total % VRE 100 57 43 4 2 43 51 <1 10 7 6 9 67 36 38 34 7 28 38 28 33 31 30 18 22 34 K. pneumoniae n=619 % total % CRKP 100 58 42 6 1 41 52 <1 3 9 8 19 61 11 11 11 11 25 11 8 33 9 6 2 6 12 P. aeruginosa n=399 % total % CRPA 99 1 59 41 4 3 37 56 <1 7 11 6 17 60 8 0 9 6 0 28 11 6 0 13 12 10 9 7
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
131
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Ireland
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
IE-60 (2/19) IE-2 (4/32) IE-1 (6/48) IE-50 (9/60) IE-20 (4/26) IE-15 (8/50) IE-32 (4/25) IE-25 (7/42) IE-72 (1/6) IE-49 (3/18) IE-34 (10/55) IE-10 (16/84) IE-47 (4/20) IE-74 (1/5)
N laboratories Minimum First quartile Median Third quartile Maximum
31 10.5 16.7 22.4 33.3 80
IE-65 (0/9) IE-80 (0/5) IE-71 (0/9) IE-57 (0/28) IE-77 (0/22) IE-79 (0/7) IE-63 (1/16) IE-59 (2/23) IE-46 (7/68) IE-76 (1/7) IE-18 (3/19) IE-49 (3/17) IE-60 (7/38) IE-74 (5/26) IE-61 (4/19) IE-12 (8/37) IE-64 (4/18) IE-36 (2/9) IE-44 (9/39) IE-73 (4/17) IE-38 (2/8) IE-21 (5/20) IE-31 (11/44)
N hospitals Minimum First quartile Median Third quartile Maximum
51 0 18.4 27.1 33.8 50
Laboratory codes
IE-18 (2/9) IE-4 (11/49) IE-48 (4/17) IE-63 (2/8) IE-6 (8/29) IE-62 (4/13) IE-44 (4/13) IE-46 (9/29) IE-61 (5/16) IE-70 (5/15) IE-58 (9/27) IE-30 (5/15) IE-31 (9/26) IE-73 (3/8) IE-76 (2/5) IE-43 (5/8) IE-64 (4/5)
Hospital codes
IE-47 (15/58) IE-11 (12/46) IE-6 (13/48) IE-35 (3/11) IE-50 (50/181) IE-32 (15/53) IE-26 (4/14) IE-4 (39/136) IE-13 (9/31) IE-72 (5/17) IE-2 (61/204) IE-15 (50/164) IE-1 (58/185) IE-10 (30/94) IE-43 (5/15) IE-20 (47/139) IE-33 (9/26) IE-51 (7/20) IE-34 (42/113) IE-53 (3/8) IE-75 (2/5) IE-52 (4/10) IE-48 (30/72) IE-29 (74/163) IE-58 (26/56) IE-70 (19/40) IE-62 (10/21) IE-30 (19/38)
25
50
75
100
25
50
75
100
132
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 32 0 0 1.6 12.5 36.4
IE-67 (0/8) IE-37 (0/13) IE-59 (0/26) IE-64 (0/8) IE-77 (0/22) IE-49 (0/16) IE-65 (1/13) IE-18 (4/50) IE-46 (3/35) IE-11 (7/79) IE-13 (9/80) IE-60 (9/71) IE-63 (3/23) IE-50 (28/183) IE-12 (12/78) IE-38 (4/26) IE-48 (22/138) IE-57 (1/6) IE-52 (4/24) IE-36 (8/47) IE-76 (3/17) IE-61 (9/50) IE-33 (7/38) IE-31 (19/98) IE-70 (11/56) IE-2 (59/299) IE-68 (1/5) IE-75 (5/24) IE-74 (11/51) IE-47 (24/108) IE-72 (8/36) IE-4 (36/159) IE-21 (12/52) IE-73 (10/43) IE-10 (27/116) IE-1 (65/279) IE-15 (52/212) IE-34 (44/169) IE-51 (12/45) IE-26 (12/44) IE-44 (25/91) IE-43 (8/29) IE-62 (13/47) IE-20 (61/212) IE-6 (30/101) IE-29 (58/191) IE-71 (4/13) IE-58 (34/108) IE-80 (3/9) IE-30 (20/58) IE-32 (31/84) IE-35 (14/30) IE-53 (3/5)
N hospitals Minimum First quartile Median Third quartile Maximum
53 0 15.3 20 27.3 60
IE-21 (0/21) IE-74 (0/5) IE-49 (0/6) IE-57 (0/5) IE-6 (0/14) IE-36 (0/5) IE-44 (0/8) IE-13 (0/10) IE-12 (0/6) IE-26 (0/5) IE-73 (0/6) IE-47 (0/13) IE-72 (0/5) IE-29 (0/28) IE-46 (0/5)
Hospital codes
Hospital codes
IE-77 (0/5) IE-1 (2/62) IE-48 (1/16) IE-50 (2/32) IE-18 (1/14) IE-11 (1/14) IE-60 (1/10) IE-34 (2/17) IE-58 (1/8) IE-30 (1/8) IE-10 (3/24) IE-31 (1/8) IE-15 (7/56) IE-2 (10/62) IE-20 (8/37) IE-32 (3/10) IE-4 (16/44)
25
50
75
100
25
50
75
100
133
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Italy
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 51 300 44 293 37 271 38 331 34 269 34 298 27 194 21 216 S. aureus Labs Isolates 53 1 343 46 1 480 42 1 225 41 1 479 38 1 164 38 1 167 30 939 23 987 E. coli Labs Isolates 17 618 17 923 14 645 16 1 195 13 910 14 1 052 14 957 9 863 Enterecocci Labs Isolates 49 602 44 634 40 576 40 714 35 650 36 656 31 580 22 509 K. pneumoniae Labs Isolates 38 344 32 321 37 391 27 331 22 313 P. aeruginosa Labs Isolates 12 183 10 185 11 168 10 195
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2 11 32 38 48 6 21 3 6 38 <1 79 37 19 2003 5 13 37 39 52 10 25 6 4 39 2 80 44 24 2004 5 14 29 40 53 9 28 5 4 36 2 78 39 21 2005 5 9 31 37 55 11 28 8 4 38 3 77 36 19 8 11 20 2006 <1 7 33 38 56 8 27 7 4 38 3 86 48 18 26 23 33 23 20 21 30 36 2007 4 15 31 33 58 14 32 11 4 39 2 73 53 11 25 27 35 20 25 27 27 35 2008 3 10 26 34 62 14 38 16 13 47 2 64 49 6 28 28 39 20 24 33 30 36 2009 3 6 21 37 63 13 36 17 20 49 3 60 52 4 19 20 37 24 16 31 36 42
134
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=378 % total % PNSP 90 10 39 23 38 11 3 30 35 21 6 31 2 39 23 7 16 11 8 5 12 10 12 9 13 9 11 13 11 11 S. aureus n=1 908 % total % MRSA 100 43 28 30 2 1 26 46 25 11 34 10 17 28 36 37 40 30 16 22 28 43 40 56 35 42 27 38 E. coli n=1 770 % total % FREC 100 <1 31 34 35 2 <1 17 35 46 4 35 7 14 40 37 0 43 32 37 8 31 31 27 32 28 25 27 34 33 E. faecalis n=618 % total % VRE 100 47 29 24 3 1 23 46 27 18 29 10 15 28 2 3 1 2 0 6 3 2 2 3 2 2 2 2 E. faecium n=403 % total % VRE 100 37 35 28 2 <1 23 43 31 13 29 11 15 32 5 7 5 3 3 0 16 13 16 18 14 15 17 13 K. pneumoniae n=552 % total % CRKP 100 <1 41 25 34 5 1 25 43 26 12 28 10 16 35 38 50 47 36 28 65 50 36 27 31 52 29 34 34 27 P. aeruginosa n=349 % total % CRPA 99 1 33 26 42 1 1 24 39 34 15 14 6 7 58 32 40 34 31 30 30 13 41 24 23 39 17 34 24 27
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
135
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Italy
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
IT031 (0/6)
IT060 (0/17)
N laboratories Minimum First quartile Median Third quartile Maximum
20 0 0 4 17.4 33.3
IT0024 (1/36) IT0069 (2/13) IT0044 (3/19) IT0028 (3/18)
N hospitals Minimum First quartile Median Third quartile Maximum
32 2.8 26.1 33.5 43.7 55.6
IT064 (0/9) IT0077 (5/29) IT067 (0/13) IT0019 (30/162) IT0076 (3/14) IT021 (0/7) IT0070 (10/40) IT0079 (6/22) IT0009 (15/54) IT028 (0/5) IT0059 (35/118) IT0050 (6/20) IT005 (0/9) IT0065 (10/33) IT019 (1/31) IT0001 (19/62) IT0045 (13/41) IT037 (2/55)
IT072 (0/13)
Laboratory codes
Hospital codes 0 25 50 75 100
IT0061 (58/180) IT0031 (40/115) IT0052 (13/37) IT0047 (34/93) IT0075 (15/41)
IT008 (1/23)
IT061 (3/65)
IT009 (1/9) IT0049 (15/39) IT065 (1/7) IT0067 (39/98) IT0008 (18/44) IT077 (1/6) IT0064 (9/21) IT0072 (24/54) IT0005 (25/56) IT059 (4/22) IT0060 (19/42) IT0034 (67/144) IT047 (1/5) IT0042 (19/37) IT024 (3/14) IT0074 (12/23) IT0037 (96/175) IT034 (8/24) IT0035 (15/27)
IT044 (2/11)
25
50
75
100
136
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 27 0 17.2 34.6 77.1 100
IT0079 (0/14)
IT0045 (3/16)
N hospitals Minimum First quartile Median Third quartile Maximum
16 0 29 34.5 39.5 61.7
IT0070 (0/6) IT0044 (0/8) IT0061 (1/46) IT0065 (1/17)
IT0047 (15/72) IT0024 (1/8) IT0037 (4/31) IT0035 (13/45) IT0009 (5/29) IT0035 (1/5) IT0067 (4/20) IT0037 (40/126) IT0059 (6/26) IT0045 (2/8) IT0008 (36/109) IT0001 (7/24)
IT0001 (18/62)
Hospital codes
IT0019 (90/264)
Hospital codes 0 25 50 75 100
IT0050 (3/10) IT0031 (18/52) IT0019 (23/64) IT0005 (8/21)
IT0070 (21/60)
IT0059 (84/238) IT0064 (4/10) IT0042 (8/17) IT0075 (14/29) IT0067 (52/132) IT0076 (7/10) IT0047 (27/35) IT0005 (36/91) IT0049 (17/22) IT0060 (12/14) IT0075 (37/89) IT0052 (8/8) IT0034 (142/303) IT0074 (8/8) IT0077 (9/9) IT0049 (29/47) IT0072 (12/12)
IT0009 (37/102)
25
50
75
100
137
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Latvia
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 4 17 5 36 7 37 6 31 3 18 7 30 S. aureus Labs Isolates 7 87 7 127 11 172 12 169 12 164 12 188 E. coli Labs Isolates 10 62 9 76 10 90 9 86 Enterecocci Labs Isolates 10 56 8 57 9 51 8 48 K. pneumoniae Labs Isolates 6 28 7 27 11 40 10 44 P. aeruginosa Labs Isolates 9 16 6 16 6 11 7 18
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2003 2004 <1 <1 7 26 2005 <1 <1 3 20 2006 <1 <1 3 19 44 5 10 6 9 50 <1 94 73 <1 25 26 36 17 29 13 47 33 2007 <1 <1 <1 8 43 14 17 14 30 <1 77 <1 <1 22 27 44 31 13 6 31 13 2008 6 6 <1 12 48 10 14 11 5 27 <1 90 78 7 52 45 58 30 36 40 44 45 2009 <1 <1 3 9 43 13 24 12 12 38 <1 82 79 18 43 34 55 17 17 7 22 12
138
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=48 % total % PNSP 94 6 56 44 3 4 74 18 1 62 7 2 30 2 0 4 0 20 0 0 0 0 0 0 0 2 S. aureus n=350 % total % MRSA 100 48 51 <1 9 4 54 29 3 23 28 8 39 1 11 12 9 0 4 5 15 17 12 19 11 22 13 0 E. coli n=175 % total % FREC 100 35 65 6 3 50 38 3 23 22 6 49 <1 19 16 20 0 10 17 18 40 31 12 17 12 0 E. faecalis n=46 % total % VRE 100 61 39 12 3 49 33 4 33 20 4 42 2 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=52 % total % VRE 100 46 54 12 43 41 5 54 13 8 24 1 12 8 14 0 2 10 20 11 0 0 0 0 K. pneumoniae n=84 % total % CRKP 100 61 39 19 1 46 31 2 35 11 7 46 1 56 55 58 63 0 45 49 67 59 20 70 47 0 P. aeruginosa n=24 % total % CRPA 100 79 21 18 5 43 32 2 45 11 2 43 21 26 0 0 33 17 17 0 12 0 0 21 -
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
139
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Latvia
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum
2 0 0 0 0 0
LV012A (0/27)
N hospitals Minimum First quartile Median Third quartile Maximum
10 0 0 7.6 11.1 88.9
LV005A (0/21)
LV004 (0/29)
LV009A (0/8)
LV004A (1/63)
Laboratory codes
LV003A (3/48)
Hospital codes
LV001A (10/112) LV002A (2/21) LV003 (0/9) LV006A (1/9) LV007A (4/15) LV013A (16/18)
25
50
75
100
25
50
75
100
140
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 6 0 33.3 46.9 66.7 68.8
LV005A (0/5)
N hospitals Minimum First quartile Median Third quartile Maximum
8 0 5.3 15.5 19.3 43.8
LV012A (0/5)
LV008A (0/5)
LV003A (2/6)
LV003A (5/47)
LV013A (2/5) LV012A (3/21)
Hospital codes
LV002A (2/12) LV004A (7/13)
LV004A (8/43)
Hospital codes
LV001A (16/24) LV006A (1/5) LV002A (11/16) LV001A (14/32)
25
50
75
100
25
50
75
100
141
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Lithuania
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 9 35 10 67 11 48 10 46 S. aureus Labs Isolates 13 167 12 240 12 278 13 258 E. coli Labs Isolates 11 171 13 235 12 304 13 297 Enterecocci Labs Isolates 8 30 10 56 10 67 11 57 K. pneumoniae Labs Isolates 8 35 10 41 11 54 12 68 P. aeruginosa Labs Isolates 7 14 7 21 7 21 8 21
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 2003 2004 2005 2006 <1 16 <1 13 55 15 12 5 5 50 <1 75 75 <1 26 3 23 21 31 21 29 46 2007 1 4 9 9 50 12 9 7 3 41 <1 100 81 <1 37 8 27 5 <1 30 33 38 2008 <1 2 6 11 54 12 14 6 5 33 <1 88 78 <1 41 23 36 14 10 24 38 35 2009 7 9 7 11 58 15 15 8 3 48 <1 95 64 11 56 37 57 20 14 19 19 33
142
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=48 % total % PNSP 94 6 56 44 3 4 74 18 1 62 7 2 30 2 0 4 0 20 0 0 0 0 0 0 0 2 S. aureus n=350 % total % MRSA 100 48 51 <1 9 4 54 29 3 23 28 8 39 1 11 12 9 0 4 5 15 17 12 19 11 22 13 0 E. coli n=175 % total % FREC 100 35 65 6 3 50 38 3 23 22 6 49 <1 19 16 20 0 10 17 18 40 31 12 17 12 0 E. faecalis n=46 % total % VRE 100 61 39 12 3 49 33 4 33 20 4 42 2 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=52 % total % VRE 100 46 54 12 43 41 5 54 13 8 24 1 12 8 14 0 2 10 20 11 0 0 0 0 K. pneumoniae n=84 % total % CRKP 100 61 39 19 1 46 31 2 35 11 7 46 1 56 55 58 63 0 45 49 67 59 20 70 47 0 P. aeruginosa n=24 % total % CRPA 100 79 21 18 5 43 32 2 45 11 2 43 21 26 0 0 33 17 17 0 12 0 0 21 -
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
143
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Lithuania
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum LT011 (0/8)
5 0 0 0 6.3 11.5
LT008A (0/15)
N hospitals Minimum First quartile Median Third quartile Maximum
14 0 0 7 12.5 25
LT013C (0/6)
LT011A (0/16)
LT008C (0/5)
LT004 (0/11) LT013B (0/12)
LT001A (7/109)
Laboratory codes
Hospital codes 0 25 50 75 100
LT007A (6/87)
LT001 (0/17)
LT013A (3/42)
LT003A (3/34)
LT012A (4/37) LT007 (1/16)
LT002A (2/16)
LT010A (1/5)
LT013 (3/26)
LT004A (16/64)
LT005A (15/60)
25
50
75
100
144
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 8 40 47.6 52.8 61.8 70
LT013B (0/10)
N hospitals Minimum First quartile Median Third quartile Maximum
15 0 5.9 9.5 16.7 28.8
LT005A (4/10)
LT013C (0/5)
LT010A (1/19) LT001A (14/31)
LT011A (1/17)
LT008A (1/16) LT003A (3/6)
LT007A (6/90)
LT013D (1/11)
LT013A (3/6)
Hospital codes
LT005A (6/63)
Hospital codes
LT004A (10/18) LT012A (6/10) LT007A (7/11) LT011A (7/10)
LT013A (10/80)
LT004A (10/75)
LT002A (3/20)
LT003A (6/36)
LT012A (3/14)
LT001B (3/12)
LT001A (34/118)
25
50
75
100
25
50
75
100
145
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Luxembourg
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 9 33 7 54 6 36 5 47 5 31 6 48 6 59 6 67 S. aureus Labs Isolates 9 97 8 95 7 96 5 83 5 77 6 117 5 117 6 113 E. coli Labs Isolates 9 193 8 227 7 216 5 188 5 167 6 275 6 303 6 301 Enterecocci Labs Isolates 8 30 7 41 5 28 5 31 4 42 5 37 5 61 5 54 K. pneumoniae Labs Isolates 4 21 6 52 6 52 3 28 P. aeruginosa Labs Isolates 1 1 4 23 5 36 4 33 6 35
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 7 22 25 15 43 4 9 <1 <1 17 <1 60 14 <1 2003 <1 15 28 21 49 4 12 <1 5 32 <1 100 <1 <1 2004 6 11 33 16 49 4 18 <1 <1 18 <1 50 <1 <1 2005 7 12 24 13 49 7 19 3 <1 24 <1 36 23 <1 <1 <1 <1 <1 <1 2006 5 5 26 19 46 6 20 2 <1 32 <1 75 30 <1 <1 6 10 9 10 7 4 10 2007 3 6 24 20 49 5 21 4 <1 44 <1 67 10 <1 4 12 2 15 11 20 22 36 2008 5 11 14 9 56 8 22 6 3 17 3 76 21 5 13 12 19 3 3 25 6 15 2009 11 19 16 13 57 9 26 8 10 28 10 93 29 36 18 21 25 14 14 15 9 11
146
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=120 % total % PNSP 98 3 51 38 11 12 5 40 40 2 12 15 3 26 43 15 33 11 20 15 10 11 8 20 13 8 20 0 9 15 S. aureus n=230 % total % MRSA 100 49 30 22 3 4 40 47 6 11 13 6 22 48 11 8 16 12 11 29 10 19 24 14 22 17 15 15 E. coli n=603 % total % FREC 100 <1 35 47 19 2 <1 28 64 6 7 20 4 20 48 24 50 25 23 25 5 20 16 21 24 14 16 16 22 20 E. faecalis n=78 % total % VRE 100 53 32 15 3 35 59 3 27 14 4 18 37 6 10 4 0 0 1 3 0 0 0 0 0 6 E. faecium n=36 % total % VRE 100 36 33 31 2 31 64 2 22 7 2 29 39 17 23 25 0 0 7 7 0 5 0 0 0 14 K. pneumoniae n=80 % total % CRKP 98 3 39 41 20 1 39 51 9 13 5 3 19 59 22 0 19 27 13 0 19 12 0 15 13 0 24 10 P. aeruginosa n=41 % total % CRPA 100 61 34 5 2 35 62 2 9 9 18 64 17 16 21 0 0 22 12 0 33 17 8 14
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
147
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Luxembourg
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
LU002 (0/7)
N laboratories Minimum First quartile Median Third quartile Maximum
6 0 7.1 10.1 11.8 32.1
LU007A (1/15)
N hospitals Minimum First quartile Median Third quartile Maximum
10 6.7 8.3 9.7 15.6 28.6
LU006A (3/39)
LU006 (1/14)
LU001E (3/36)
LU007Z (2/22)
LU007 (1/11) LU001A (3/32)
Laboratory codes
Hospital codes
LU004T (1/10) LU004 (1/9) LU004A (1/9) LU001 (6/51) LU003S (5/32) LU003A (4/24) LU003 (9/28) LU002A (2/7)
25
50
75
100
25
50
75
100
148
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum LU007Z (0/6) 5 0 15.8 18.2 25 42.1
LU007Z (8/53)
N hospitals Minimum First quartile Median Third quartile Maximum
11 15.1 20.2 26.5 30.8 35.7
LU006A (21/111)
LU001E (18/89)
LU006A (3/19) LU007A (7/31)
LU004T (5/22)
Hospital codes
Hospital codes 0 25 50 75 100
LU003A (18/68)
LU003S (2/11)
LU001A (28/104)
LU004A (6/21) LU001A (4/16)
LU002A (4/13)
LU003S (23/71) LU001E (8/19)
LU002W (5/14)
25
50
75
100
149
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Malta
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 1 12 1 9 1 18 1 13 1 31 1 13 1 17 1 8 S. aureus Labs Isolates 1 87 1 121 1 94 1 77 1 90 1 105 1 108 1 86 E. coli Labs Isolates 1 74 1 91 1 91 1 85 1 94 1 117 1 128 1 159 Enterecocci Labs Isolates 1 33 1 26 1 41 1 38 1 53 1 37 1 32 1 36 K. pneumoniae Labs Isolates 1 18 1 32 1 28 1 36 1 38 P. aeruginosa Labs Isolates 1 45 1 51 1 36 1 31 1 58
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 <1 25 43 43 8 12 3 <1 17 <1 33 <1 <1 2003 <1 <1 38 43 39 18 24 2 5 29 <1 33 50 <1 2004 <1 <1 25 56 48 20 36 4 <1 44 <1 43 <1 <1 2005 8 15 46 56 51 7 31 1 3 32 <1 25 <1 <1 17 11 6 22 11 18 16 44 2006 3 7 45 67 56 15 32 4 2 <1 14 <1 6 6 6 47 30 20 8 24 2007 <1 <1 8 52 54 20 35 13 3 <1 40 <1 <1 11 7 11 3 11 8 11 2008 24 47 35 56 52 22 34 21 <1 <1 60 <1 <1 8 <1 45 33 30 23 19 2009 <1 14 13 58 55 21 31 15 5 <1 75 <1 <1 3 <1 36 29 21 21 22
150
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=24 % total % PNSP 92 8 42 58 18 4 33 42 3 23 39 3 23 12 41 0 30 43 9 20 8 14 0 7 6 50 15 14 S. aureus n=194 % total % MRSA 100 70 30 9 5 40 46 1 17 44 19 11 9 57 60 50 39 38 49 62 25 60 49 60 49 56 E. coli n=287 % total % FREC 100 47 53 3 2 27 68 <1 8 42 22 14 14 32 36 28 0 14 28 33 0 25 31 34 21 32 E. faecalis n=57 % total % VRE 100 67 33 11 3 39 46 0 60 17 13 5 6 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=11 % total % VRE 100 64 36 4 4 43 48 52 28 11 4 4 0 0 0 0 0 0 0 0 0 0 0 0 K. pneumoniae n=74 % total % CRKP 100 62 36 1 9 2 43 46 1 20 43 18 14 5 0 0 0 0 15 0 5 0 0 10 2 0 0 13 P. aeruginosa n=88 % total % CRPA 97 3 65 35 3 5 41 51 52 23 11 9 5 25 0 26 19 0 17 25 17 26 14 20 5 9
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
151
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Malta
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum
1 37.5 37.5 37.5 37.5 37.5
N hospitals Minimum First quartile Median Third quartile Maximum
2 50 50 53.5 57 57
MT001E (5/10)
Laboratory codes
MT001 (9/24)
Hospital codes
MT001A (102/179)
25
50
75
100
25
50
75
100
152
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 1 0 0 0 0 0
N hospitals Minimum First quartile Median Third quartile Maximum
3 29.8 29.8 43.8 44.4 44.4
MT001A (73/245)
Hospital codes
MT001E (14/32)
Hospital codes 0 25 50 75 100
MT001A (0/74)
MT001F (4/9)
25
50
75
100
153
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Netherlands
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 23 892 24 891 22 758 23 815 22 1 006 21 940 17 723 17 746 S. aureus Labs Isolates 23 1 550 23 1 422 22 1 339 23 1 407 23 1 636 21 1 471 16 1 191 16 1 035 E. coli Labs Isolates 22 2 427 23 2 133 21 2 111 23 2 201 22 2 905 21 2 801 16 2 283 16 2 398 Enterecocci Labs Isolates 22 530 23 480 22 444 23 563 23 776 21 827 17 632 16 522 K. pneumoniae Labs Isolates 16 301 18 458 19 497 15 463 15 408 P. aeruginosa Labs Isolates 16 210 19 330 19 338 15 345 15 235
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 1 7 <1 40 2 5 1 3 39 <1 21 4 2 2003 <1 1 5 1 45 3 7 1 4 29 1 30 20 <1 2004 <1 2 8 1 43 3 7 1 3 37 <1 42 20 <1 2005 <1 1 11 <1 48 4 10 2 3 38 <1 61 40 <1 5 6 4 4 5 5 7 9 2006 <1 1 8 <1 47 3 11 3 5 28 <1 73 50 <1 4 4 4 2 5 2 4 9 2007 <1 2 7 2 49 5 13 4 5 38 <1 83 62 <1 5 4 7 2 4 2 3 5 2008 <1 2 7 <1 48 6 14 5 <1 34 <1 86 53 <1 7 7 8 6 6 6 4 8 2009 <1 1 5 <1 45 4 11 4 2 31 <1 89 76 <1 3 4 6 3 4 3 1 7
154
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=1 282 % total % PNSP 94 6 50 47 3 7 3 38 49 3 6 18 3 22 51 2 0 2 1 0 2 1 1 1 2 1 2 1 2 1 S. aureus n=2 111 % total % MRSA 100 57 39 3 9 3 35 50 3 8 17 9 22 44 1 1 1 0 1 1 1 1 0 2 1 2 1 1 E. coli n=4 614 % total % FREC 100 <1 47 49 4 4 1 30 61 4 6 20 7 20 47 13 15 16 9 15 3 18 11 10 11 11 11 9 13 8 E. faecalis n=530 % total % VRE 100 63 32 5 9 1 37 49 4 21 13 9 22 35 0 0 1 0 0 0 0 0 0 0 1 0 0 1 E. faecium n=372 % total % VRE 100 62 38 7 3 42 46 2 26 9 5 21 40 1 1 0 0 0 1 1 0 0 0 2 1 1 K. pneumoniae n=862 % total % CRKP 99 1 57 43 4 1 37 58 <1 10 18 9 21 42 7 13 7 6 7 21 6 5 0 9 3 8 7 4 P. aeruginosa n=579 % total % CRPA 98 2 69 31 3 2 36 60 <1 16 17 10 18 39 5 11 5 5 3 10 4 3 100 8 4 4 3 2
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
155
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Netherlands
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
NL025 (0/31)
NL101 (0/40)
N laboratories Minimum First quartile Median Third quartile Maximum
23 0 0 0 3.6 8.6
NL027A (0/80) NL005B (0/15) NL030H (0/51) NL030E (0/52) NL029A (0/72) NL030J (0/10) NL112B (0/30) NL131C (0/10) NL131B (0/9) NL030G (0/32) NL113A (0/53) NL030C (0/21) NL036B (0/35) NL023D (0/27) NL031A (0/13) NL021C (0/13) NL021B (0/24) NL030B (0/21)
N hospitals Minimum First quartile Median Third quartile Maximum
56 0 0 0 1.1 20
NL132 (0/40)
NL023 (0/69)
NL036 (0/31)
NL030 (0/157)
NL131 (0/49)
NL034 (0/5)
NL007C (0/92) NL113D (0/18) NL030I (0/40) NL014B (0/40) NL023A (0/10)
NL021 (0/37)
NL007 (0/56)
NL026C (0/15) NL030D (0/21) NL031B (0/60) NL014C (0/43) NL030F (0/40) NL101D (0/9) NL031C (0/52) NL0033 (0/13) NL026B (0/79) NL113C (0/23) NL002C (0/63) NL112A (0/8)
Laboratory codes
NL033 (0/52)
NL112 (0/27)
NL003 (0/27)
NL002 (1/159)
Hospital codes 0 25 50 75 100
NL029 (0/36)
NL101B (0/13) NL005A (0/21) NL033B (0/15) NL003A (0/81) NL113B (0/14)
NL031 (1/126)
NL026 (1/36)
NL021A (0/19) NL007A (1/97) NL002B (1/87) NL026A (1/78) NL025A (1/68) NL023B (1/64) NL104B (1/55) NL131A (1/49) NL119A (2/86) NL030A (1/31) NL132A (2/57) NL033A (1/28)
NL027 (1/28)
NL113 (3/83)
NL119 (2/43)
NL014 (4/68)
NL022 (3/42)
NL101A (1/19) NL002A (1/13) NL014A (1/8) NL101C (1/5)
NL005 (3/35)
25
50
75
100
156
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 43 0 0 0 9.5 28.6
NL014A (0/8) NL101B (0/26) NL131A (4/91) NL026A (4/89) NL0033 (1/18) NL030H (7/123) NL030G (6/94) NL030B (4/61) NL023B (8/114) NL026C (1/14) NL113C (3/41) NL104B (7/87) NL031A (3/37) NL101A (5/60) NL002B (17/199) NL113A (11/124) NL005A (5/53) NL030E (15/159) NL002C (17/180) NL030A (8/82) NL014B (8/80) NL131C (3/30) NL021B (3/30) NL025A (9/87) NL031B (20/189) NL030D (10/90) NL036A (1/9) NL031C (17/147) NL113D (6/51) NL023A (4/34) NL131B (2/16) NL021A (3/24) NL112A (4/32) NL119A (19/149) NL023D (8/62) NL030I (16/116) NL030F (22/154) NL030J (5/35) NL005B (7/49) NL112B (9/60) NL021C (5/33) NL029A (26/167) NL022X (32/197) NL007C (18/109) NL036B (12/69) NL132A (27/155) NL014C (15/86) NL113E (3/17) NL113B (7/39) NL033A (12/61) NL030C (12/60) NL003A (28/140) NL007A (31/154) NL033B (12/56) NL002A (9/41) NL026B (20/78) NL101C (2/7) NL101D (7/23) NL027A (4/11)
N hospitals Minimum First quartile Median Third quartile Maximum
59 0 8.5 11.8 17.4 36.4
NL131A (0/10) NL030H (0/14) NL036B (0/14) NL113B (0/11) NL031A (0/5) NL131C (0/8) NL033B (0/5) NL113A (0/15) NL033A (0/9) NL0033 (0/5) NL023A (0/5) NL030A (0/10) NL002A (0/9) NL104B (0/16) NL005B (0/11) NL101A (0/9) NL030E (0/25) NL030F (0/14) NL113D (0/9)
Hospital codes
Hospital codes 0 25 50 75 100
NL030B (0/8) NL030G (0/9) NL031C (0/25) NL031B (1/37) NL014C (1/23) NL025A (1/22) NL119A (2/32) NL030I (1/16) NL101B (1/14) NL022X (6/75) NL002C (3/36) NL026B (2/22) NL002B (5/53) NL014B (2/21) NL007C (4/37) NL112B (1/9) NL027A (4/35) NL003A (4/33) NL023D (1/8) NL132A (3/20) NL026A (3/17) NL007A (6/34) NL023B (4/20) NL026C (2/7)
25
50
75
100
157
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Norway
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 11 453 11 512 11 600 11 606 12 601 13 616 13 576 12 554 S. aureus Labs Isolates 11 502 11 506 11 516 11 553 12 734 13 794 13 837 12 909 E. coli Labs Isolates 11 1 119 11 1 179 11 1 212 11 1 331 12 1 574 13 1 713 13 1 799 12 1 846 Enterecocci Labs Isolates 11 177 11 192 11 235 11 304 12 349 13 416 13 403 12 478 K. pneumoniae Labs Isolates 4 29 4 46 4 51 11 193 12 263 13 320 13 349 12 396 P. aeruginosa Labs Isolates 4 27 4 25 4 27 11 97 12 96 13 105 13 148 12 166
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 <1 6 <1 29 <1 2 <1 4 30 3 49 14 <1 <1 <1 <1 <1 <1 <1 <1 <1 2003 <1 <1 8 <1 34 <1 2 <1 4 38 <1 43 14 <1 <1 <1 <1 <1 <1 <1 <1 4 2004 <1 2 8 <1 32 <1 4 <1 <1 27 <1 80 25 <1 2 <1 <1 13 <1 4 4 5 2005 <1 2 14 <1 34 2 5 <1 3 32 <1 72 44 <1 3 1 2 3 3 3 <1 4 2006 <1 2 12 <1 35 2 5 1 3 33 <1 75 45 <1 <1 7 2 3 5 9 1 9 2007 <1 2 10 <1 38 3 7 2 2 34 <1 81 52 <1 <1 5 2 2 3 9 2 7 2008 <1 2 7 <1 38 3 7 3 2 29 <1 78 54 <1 1 4 2 6 4 7 <1 3 2009 <1 2 6 <1 37 3 9 2 <1 36 <1 76 38 <1 3 6 3 4 5 5 <1 2
158
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=1 128 % total % PNSP 97 3 48 52 <1 7 3 41 49 <1 10 53 4 30 3 2 9 2 2 0 2 0 1 2 0 2 1 3 2 1 S. aureus n=1 743 % total % MRSA 100 63 37 <1 4 3 35 57 <1 7 42 17 31 3 0 0 0 0 1 0 0 0 0 0 0 0 0 1 E. coli n=3 616 % total % FREC 100 45 55 <1 2 1 26 71 <1 5 46 17 30 2 8 10 6 9 4 4 7 5 33 7 5 7 6 4 E. faecalis n=616 % total % VRE 100 74 26 <1 2 1 23 74 <1 9 40 21 28 2 0 0 0 0 3 0 0 0 0 0 0 0 0 0 E. faecium n=211 % total % VRE 100 59 41 1 <1 31 68 15 34 22 28 2 0 0 0 0 0 0 0 0 0 0 0 0 K. pneumoniae n=745 % total % CRKP 100 60 40 0 1 1 27 71 7 41 20 30 2 2 3 1 0 7 6 3 1 4 1 2 2 3 P. aeruginosa n=312 % total % CRPA 100 <1 69 30 1 2 2 27 69 10 41 12 34 2 6 0 6 6 0 27 8 8 5 15 5 6 4 15
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
159
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Norway
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
NO105 (0/16)
N laboratories Minimum First quartile Median Third quartile Maximum
14 0 0 1.4 2.8 8.2
NO502K (0/8) NO204E (0/97) NO102B (0/123) NO205I (0/34) NO502H (0/32) NO402H (0/17)
N hospitals Minimum First quartile Median Third quartile Maximum
34 0 0 0 0 2.3
NO203 (0/90)
NO304 (0/34) NO502D (0/6) NO502L (0/5) NO403 (0/87) NO304K (0/6) NO206Q (0/7) NO103E (0/163) NO205 (0/26) NO203D (0/36) NO106V (0/11) NO206 (1/108) NO502I (0/15) NO203C (0/84)
Laboratory codes
NO106 (2/151)
Hospital codes 0 25 50 75 100
NO206O (0/69) NO101D (0/32) NO106P (0/94) NO106Q (0/29) NO106T (0/21)
NO102 (1/64)
NO104 (2/109)
NO204H (0/7) NO104J (0/144) NO105K (0/26)
NO204 (2/108) NO204I (0/36) NO203X (0/34) NO402 (1/36) NO106U (0/10) NO403E (0/22) NO304J (0/38) NO103 (3/108) NO106S (0/46) NO403D (1/147) NO502 (1/32) NO206P (1/54) NO101C (1/50) NO101 (13/159) NO402B (1/49) NO101A (4/176)
25
50
75
100
160
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 29 0 0 0 3.6 28.6
NO104N (0/6) NO204H (0/6) NO205N (0/7) NO304K (0/21) NO502D (0/11) NO502L (0/15) NO502K (0/19)
N hospitals Minimum First quartile Median Third quartile Maximum
37 0 3.4 7.1 9.3 24.1
NO502L (0/5) NO502I (0/8) NO205I (0/10) NO106V (0/8) NO204I (0/20) NO101A (0/64)
NO205I (1/88) NO304J (1/71) NO106Q (2/59) NO101C (5/122) NO206Q (2/46) NO206Q (0/8) NO203D (4/91) NO304M (1/22) NO403E (4/71) NO203X (3/45) NO101D (0/18) NO204I (5/75) NO203X (0/8) NO304J (0/18) NO106S (0/18) NO106P (0/31) NO502H (0/15)
Hospital codes
Hospital codes 0 25 50 75 100
NO203C (12/170) NO502H (4/56) NO402B (8/108) NO204E (18/243)
NO106Q (0/12) NO204E (0/57) NO403E (0/11) NO402B (0/20)
NO106T (4/52) NO104J (20/255) NO206P (8/102) NO101A (22/255) NO403D (1/49) NO502I (2/22) NO103E (35/378) NO206O (15/161) NO403D (29/296) NO102B (24/232) NO104J (4/81) NO106P (19/179) NO106S (8/73) NO101D (9/78) NO105K (9/77) NO106U (1/8) NO102B (3/40) NO402H (8/51) NO106V (7/29) NO106T (2/7) NO206P (1/19) NO101C (1/18) NO105K (1/15) NO203C (1/42) NO206O (1/28) NO203D (1/22) NO106U (0/5) NO103E (1/64)
25
50
75
100
161
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Poland
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 7 10 11 16 11 16 6 6 4 9 10 22 34 84 20 68 S. aureus Labs Isolates 21 186 24 166 30 262 30 198 24 174 24 185 15 99 30 551 E. coli Labs Isolates 22 135 25 124 29 192 30 176 26 206 27 256 14 84 29 625 Enterecocci Labs Isolates 19 56 16 64 23 52 21 54 21 68 20 71 11 26 28 267 K. pneumoniae Labs Isolates 17 53 15 42 18 32 11 19 25 151 P. aeruginosa Labs Isolates 14 26 16 37 23 67 8 22 27 153
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 30 30 67 23 52 11 11 6 12 41 <1 80 73 <1 2003 19 19 14 19 50 10 7 4 <1 48 <1 91 55 <1 2004 <1 <1 19 19 45 5 9 5 2 33 <1 86 100 <1 2005 17 33 33 24 56 7 20 5 9 48 <1 95 62 5 57 34 66 50 31 27 56 31 2006 <1 <1 11 20 55 11 20 4 2 50 <1 95 85 <1 36 29 38 43 42 30 46 41 2007 10 29 15 56 6 13 2 4 46 2 88 84 <1 31 3 34 36 21 18 40 37 2008 12 13 50 12 54 7 20 2 6 29 <1 78 67 <1 26 32 37 32 27 14 27 13 2009 30 30 16 20 65 7 23 9 <1 39 <1 98 75 1 29 32 49 30 21 25 27 26
162
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=141 % total % PNSP 74 26 56 42 2 16 9 49 26 1 20 39 1 39 1 16 31 22 17 33 32 21 17 14 33 12 15 50 25 67 S. aureus n=605 % total % MRSA 100 57 40 3 9 3 49 38 1 17 38 13 26 7 19 19 19 11 14 16 21 20 6 36 12 31 13 24 E. coli n=651 % total % FREC 99 1 38 59 3 6 1 43 48 2 17 41 10 25 7 23 25 29 19 10 6 5 18 18 23 22 16 18 13 24 E. faecalis n=157 % total % VRE 100 54 42 4 5 1 43 50 2 21 31 19 17 11 0 0 0 0 0 0 1 0 0 0 1 0 0 0 E. faecium n=94 % total % VRE 100 57 36 6 8 1 46 42 3 32 19 16 20 13 1 0 3 0 0 50 1 0 0 2 0 3 0 0 K. pneumoniae n=162 % total % CRKP 99 1 60 35 5 13 1 47 37 2 34 20 14 25 8 48 0 48 46 50 50 33 49 46 57 62 33 60 38 36 P. aeruginosa n=164 % total % CRPA 98 2 57 37 7 5 3 50 38 4 41 15 11 19 14 24 0 27 18 27 13 11 28 20 23 30 20 22 7 32
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
163
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Poland
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
PL036 (0/5)
N laboratories Minimum First quartile Median Third quartile Maximum
9 0 0 7.1 25 71.4
PL0057 (0/6) PL0056 (0/16) PL0006 (0/12) PL0015 (0/9) PL0005 (0/15)
N hospitals Minimum First quartile Median Third quartile Maximum
31 0 0 15.2 28.6 57.6
PL034 (0/7) PL0025 (0/6) PL0009 (0/7) PL0132 (0/9) PL018 (0/10) PL0019 (1/23) PL0048 (1/22) PL0003 (5/58) PL0024 (2/20) PL058 (1/20) PL0041 (4/38) PL0044 (1/9)
Laboratory codes
Hospital codes 0 25 50 75 100
PL0046 (1/7) PL0014 (5/33) PL0124 (4/26) PL0012 (4/24) PL0043 (3/17)
PL024 (1/14)
PL019 (1/5) PL0058 (4/21) PL0052 (3/13) PL0011 (7/28) PL041 (3/12) PL0018 (5/18) PL0131 (6/21) PL0033 (10/33) PL0035 (4/12) PL003 (2/5) PL0031 (4/12) PL0130 (8/22) PL0029 (3/8) PL033 (5/7) PL0023 (9/19) PL0126 (19/33)
25
50
75
100
164
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 11 0 25 66.7 83.3 100
PL0124 (2/24) PL0057 (1/10) PL0015 (1/9) PL0031 (1/8) PL0006 (2/16) PL0058 (6/42)
N hospitals Minimum First quartile Median Third quartile Maximum
26 8.3 14.3 23.1 30 52.9
PL0024 (0/6)
PL0014 (0/7)
PL0130 (3/12) PL0056 (4/28) PL0003 (7/45) PL0024 (7/43) PL0041 (7/39) PL0029 (9/50) PL0044 (2/9) PL0003 (4/14)
PL0035 (5/13)
Hospital codes
PL0023 (3/13) PL0048 (6/26) PL0018 (6/26) PL0014 (10/39) PL0035 (8/31) PL0012 (7/24) PL0043 (8/27) PL0011 (3/10)
Hospital codes 0 25 50 75 100
PL0006 (4/6)
PL0029 (20/27)
PL0011 (10/13)
PL0023 (5/6) PL0132 (2/6) PL0131 (5/15) PL0019 (8/23) PL0130 (9/23) PL0126 (13/33) PL0019 (6/6) PL0005 (9/17) PL0126 (9/10)
25
50
75
100
165
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Portugal
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 14 185 12 95 14 166 13 202 15 183 12 202 14 260 17 237 S. aureus Labs Isolates 16 544 22 1 033 23 1 063 19 1 153 17 1 306 20 1 383 20 1 557 20 1 824 E. coli Labs Isolates 17 444 21 792 19 761 19 1 171 18 1 331 20 1 432 21 1 625 20 2 040 Enterecocci Labs Isolates 13 101 18 398 19 410 17 405 17 464 19 518 20 588 19 675 K. pneumoniae Labs Isolates 1 1 13 315 18 370 21 543 20 564 P. aeruginosa Labs Isolates 11 266 16 340 19 467 18 536
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 20 <1 38 58 9 23 6 2 25 6 79 33 <1 2003 <1 20 45 53 9 26 7 4 34 3 88 55 47 2004 <1 27 20 46 58 13 27 8 5 29 6 83 66 42 2005 <1 17 19 47 58 12 29 12 <1 38 5 92 68 34 <1 <1 2006 <1 17 21 48 59 12 28 10 2 41 5 76 53 26 13 20 21 15 19 21 17 21 2007 <1 16 23 48 59 12 30 10 4 41 4 93 49 29 11 18 17 14 16 15 16 19 2008 <1 18 22 53 58 14 29 10 4 43 4 86 28 24 19 22 26 17 16 18 11 23 2009 18 18 22 49 58 11 28 9 7 34 4 91 49 23 20 28 28 17 13 16 12 21
166
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=497 % total % PNSP 92 8 56 44 <1 9 5 43 37 5 6 15 <1 78 1 18 13 18 18 0 31 17 14 19 30 21 16 14 19 22 S. aureus n=3 380 % total % MRSA 100 62 38 <1 3 2 34 50 11 9 24 8 54 4 51 49 53 100 15 18 38 58 46 58 56 63 40 55 E. coli n=3 550 % total % FREC 100 <1 46 54 1 1 34 56 7 5 22 5 64 3 28 0 33 24 7 15 25 31 21 32 29 30 27 30 E. faecalis n=844 % total % VRE 100 57 43 2 1 30 57 10 15 22 10 50 2 4 4 5 2 4 5 4 5 4 6 2 5 2 E. faecium n=394 % total % VRE 100 53 47 1 1 39 50 8 15 19 13 51 2 23 19 28 20 8 32 28 28 22 32 20 33 38 K. pneumoniae n=1 089 % total % CRKP 100 57 43 <1 2 2 36 48 12 11 18 11 57 3 27 28 25 50 43 18 24 23 22 27 30 18 22 15 P. aeruginosa n=950 % total % CRPA 100 <1 58 42 2 2 41 48 8 17 15 9 56 3 17 100 20 13 7 12 18 17 15 25 15 19 15 21
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
167
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Portugal
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
PT029 (3/42)
N laboratories Minimum First quartile Median Third quartile Maximum
15 7.1 14.4 18.2 23.1 50
PT031A (3/20)
PT009A (5/29)
N hospitals Minimum First quartile Median Third quartile Maximum
25 15 40 46.6 55.8 81
PT015 (1/8)
PT021A (13/56)
PT011A (50/179) PT001 (3/24) PT006A (36/107)
PT031C (5/14) PT019 (14/97) PT027A (6/15)
PT002 (9/55)
PT026A (19/46)
PT001A (57/135) PT018 (8/46) PT023A (72/169)
PT029A (31/72) PT011 (12/67)
Laboratory codes
PT017 (2/11)
Hospital codes 0 25 50 75 100
PT031D (37/82)
PT018A (34/73)
PT003A (164/342)
PT028 (1/5) PT015A (45/90)
PT012A (118/234) PT003 (12/60) PT019A (155/307)
PT008 (5/24)
PT031B (47/86)
PT008A (129/231) PT024 (3/13) PT016A (70/123)
PT002A (110/184) PT016 (3/12) PT028A (29/47)
PT005 (7/18)
PT007A (351/541)
PT005A (115/176) PT026 (4/8) PT022A (17/21)
25
50
75
100
168
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 23 0 18.3 27.3 36.2 70
PT031C (0/11) PT009A (1/11) PT027A (7/38) PT031A (2/10)
N hospitals Minimum First quartile Median Third quartile Maximum
26 0 22.6 25.4 32.3 52
PT027A (0/6)
PT016A (1/29)
PT018A (2/25)
PT023A (4/32) PT023A (38/181) PT006A (10/68) PT026A (13/58) PT019A (15/82) PT011A (68/301) PT031D (24/106) PT015A (24/105) PT021A (15/64) PT012A (34/145) PT019A (65/274) PT003A (30/151)
PT021A (6/28)
PT011A (33/139)
PT029A (5/21)
Hospital codes
PT008A (20/79) PT018A (24/94) PT006A (53/197) PT028A (22/80) PT002A (60/218) PT007A (131/424) PT031B (27/86) PT003A (199/616)
Hospital codes 0 25 50 75 100
PT002A (8/33)
PT008A (6/22)
PT031C (2/7)
PT007A (47/162)
PT005A (12/41)
PT015A (8/27)
PT031D (9/29)
PT012A (17/47) PT029A (40/114) PT026A (6/16) PT001A (49/139) PT031B (15/37) PT016A (34/96) PT009A (3/6) PT005A (30/67) PT025A (5/11) PT022A (13/25) PT001A (27/43)
PT028A (21/30)
25
50
75
100
169
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Romania
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 6 10 5 26 4 9 5 18 8 29 5 27 4 14 3 17 S. aureus Labs Isolates 10 80 9 85 15 95 13 93 11 83 9 42 5 39 5 45 E. coli Labs Isolates 8 28 9 50 12 48 13 84 9 41 9 63 4 58 6 80 Enterecocci Labs Isolates 4 11 5 12 4 9 7 14 9 28 5 14 4 16 5 26 K. pneumoniae Labs Isolates 1 3 5 32 6 30 3 6 3 26 P. aeruginosa Labs Isolates 2 23 2 3 2 4 3 8 3 22
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 10 50 10 36 50 15 20 18 <1 40 <1 100 80 17 2003 21 33 29 46 70 21 14 19 <1 25 <1 86 63 <1 2004 11 11 <1 71 79 33 21 23 29 <1 <1 100 100 <1 2005 22 39 31 60 78 14 9 17 <1 50 <1 100 70 <1 100 33 100 61 52 61 64 64 2006 10 28 25 54 85 41 41 41 <1 15 <1 100 80 <1 91 34 94 33 <1 <1 33 33 2007 22 33 19 26 76 35 27 27 25 50 <1 100 67 <1 80 23 80 25 <1 <1 25 25 2008 54 69 27 33 55 24 27 24 10 22 <1 100 50 <1 60 20 50 25 13 13 38 25 2009 12 29 25 36 83 13 23 17 12 35 <1 100 56 <1 31 11 56 36 38 55 45 36
170
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=30 % total % PNSP 63 37 53 47 22 12 44 20 2 1 5 82 12 63 18 63 29 66 11 34 21 33 50 13 38 29 S. aureus n=84 % total % MRSA 100 35 18 48 24 11 41 12 13 9 8 7 42 34 35 38 33 33 57 23 51 53 47 66 50 61 48 42 E. coli n=105 % total % FREC 100 46 54 20 7 37 33 3 5 20 3 68 3 25 23 26 19 43 20 20 18 20 20 17 23 14 E. faecalis n=27 % total % VRE 100 56 44 27 2 33 34 5 6 20 2 59 13 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=15 % total % VRE 100 53 47 35 8 28 18 11 8 25 3 46 18 0 13 0 0 0 11 0 0 0 0 0 3 8 K. pneumoniae n=22 % total % CRKP 100 59 41 60 7 22 10 8 17 2 71 1 55 62 44 96 50 58 44 71 60 100 85 0 P. aeruginosa n=19 % total % CRPA 95 5 53 37 11 16 4 10 6 63 22 6 51 20 39 0 40 43 0 0 100 80 33 45 82 100 20 40
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
171
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Romania
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
N laboratories Minimum First quartile Median Third quartile Maximum
2 29.4 29.4 56.4 83.3 83.3
RO001I (0/9)
N hospitals Minimum First quartile Median Third quartile Maximum
8 0 18.7 38.1 44.9 57.1
RO01AX (1/7)
RO01A (5/17)
RO001A (3/13)
RO000X (4/12)
Laboratory codes
Hospital codes
RO01BX (3/7) RO001B (4/9) ROROU (5/6) RO01DX (5/11) RO001D (4/7)
25
50
75
100
25
50
75
100
172
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 2 28.6 28.6 57.1 85.7 85.7
RO01CX (0/8)
N hospitals Minimum First quartile Median Third quartile Maximum
7 0 0 10 31.6 43.3
RO01BX (0/7) RO001C (2/7)
RO014A (0/6)
Hospital codes
RO001A (2/20)
RO01AX (1/7)
Hospital codes
RO001B (6/7)
RO001C (6/19)
RO00UX (13/30)
25
50
75
100
25
50
75
100
173
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Slovenia
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 11 101 11 172 10 166 11 208 11 167 10 195 10 209 9 213 S. aureus Labs Isolates 11 276 11 299 11 347 11 349 11 365 10 422 10 418 9 424 E. coli Labs Isolates 11 409 11 401 11 573 11 657 11 717 10 851 10 874 9 783 Enterecocci Labs Isolates 9 45 10 76 9 91 11 119 10 145 9 183 10 196 9 184 K. pneumoniae Labs Isolates 10 78 10 145 10 170 9 157 9 168 P. aeruginosa Labs Isolates 8 38 10 72 9 88 10 95 9 93
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 19 10 14 43 3 12 1 <1 50 <1 69 62 <1 2003 2 15 9 13 41 2 11 <1 <1 49 <1 83 82 <1 2004 2 25 11 12 40 5 12 1 <1 37 <1 76 56 <1 2005 2 11 11 10 42 4 12 2 1 46 <1 93 47 <1 17 14 19 21 11 13 18 29 2006 5 19 13 7 44 7 15 2 1 40 <1 86 54 6 19 21 24 18 8 6 15 21 2007 4 17 17 8 49 7 17 4 <1 50 <1 92 63 5 24 26 28 13 7 19 10 17 2008 3 15 16 7 49 7 17 4 <1 40 <1 96 57 13 23 25 26 21 14 16 13 24 2009 1 17 18 10 54 10 19 7 <1 44 <1 94 58 4 28 29 34 18 11 17 14 15
174
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=422 % total % PNSP 93 7 59 41 21 5 35 39 <1 9 38 1 52 16 21 16 16 30 7 12 15 0 15 13 11 20 S. aureus n=842 % total % MRSA 100 62 38 4 3 38 55 <1 10 46 11 33 0 9 9 8 1 4 9 12 25 15 8 21 7 0 E. coli n=1 657 % total % FREC 100 <1 41 59 3 1 30 67 <1 7 52 6 35 18 0 21 16 2 4 15 16 29 17 14 16 16 E. faecalis n=235 % total % VRE 100 59 41 7 <1 30 63 <1 11 38 15 35 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=145 % total % VRE 100 59 41 1 39 59 <1 21 31 14 33 9 11 7 0 9 3 0 0 1 2 14 K. pneumoniae n=325 % total % CRKP 100 55 45 3 1 31 65 13 42 15 30 30 34 26 15 40 30 26 45 18 32 30 P. aeruginosa n=188 % total % CRPA 99 1 70 30 2 2 38 58 15 35 16 34 16 50 18 12 0 14 23 10 24 9 25 12 -
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
175
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Slovenia
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
SI005 (0/15)
N laboratories Minimum First quartile Median Third quartile Maximum
10 0 13.3 15.4 29.2 43.8
SI003B (0/13)
N hospitals Minimum First quartile Median Third quartile Maximum
14 0 0 3 8.8 17.7
SI004B (0/5)
SI010 (7/57) SI010A (0/20)
SI004 (4/30)
SI011A (0/25)
SI001C (0/17) SI001 (24/174)
SI001B (0/6)
Laboratory codes
SI008 (4/27)
Hospital codes
SI003 (7/44) SI002 (5/23) SI007 (7/24) SI009 (4/12) SI011 (7/16)
SI004A (1/43)
SI002A (2/53)
SI009A (2/50)
SI003A (7/128)
SI007A (3/34)
SI005A (3/31)
SI001A (41/335)
SI008A (14/79)
25
50
75
100
25
50
75
100
176
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 11 0 9.1 19.2 46.2 60
SI003B (1/30)
N hospitals Minimum First quartile Median Third quartile Maximum
14 3.3 10.5 17.7 19.2 35.1
SI002A (0/17)
SI010A (5/57) SI009A (1/16)
SI011A (9/91)
SI005A (1/11) SI004B (2/19)
SI009A (22/142)
SI004A (2/19)
SI002A (16/101) SI001B (1/7)
Hospital codes
SI004A (16/92)
Hospital codes 0 25 50 75 100
SI008A (5/26)
SI001C (7/39)
SI001A (39/113) SI001A (105/549)
SI003A (49/256)
SI003A (29/73)
SI008A (23/120) SI011A (6/13)
SI005A (13/64)
SI001C (6/11) SI007A (15/56)
SI001B (13/37)
SI003B (6/10)
25
50
75
100
177
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Spain
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 35 658 35 656 36 684 34 740 35 625 35 862 31 695 32 708 S. aureus Labs Isolates 36 1 196 36 1 391 36 1 527 34 1 337 35 1 483 35 1 645 32 1 505 33 1 715 E. coli Labs Isolates 29 2 484 29 2 650 36 3 471 34 2 997 35 3 364 35 3 678 32 3 626 33 3 821 Enterecocci Labs Isolates 35 566 36 608 36 710 35 623 34 755 35 885 32 1 002 33 1 093 K. pneumoniae Labs Isolates 14 56 33 564 33 618 30 639 32 628 P. aeruginosa Labs Isolates 13 70 32 405 35 448 32 548 33 544
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 10 33 26 23 60 8 19 2 2 37 <1 59 16 1 2003 7 32 27 24 58 7 21 4 1 36 <1 64 11 3 2004 9 29 27 26 60 7 25 7 2 36 <1 66 17 2 2005 9 25 23 27 62 10 28 8 <1 36 <1 67 16 3 4 11 7 4 6 17 4 14 2006 8 27 22 25 64 9 28 7 2 36 <1 73 21 3 7 8 9 9 7 12 11 19 2007 8 22 18 25 62 10 30 7 1 42 <1 79 40 2 9 17 10 8 10 15 15 25 2008 7 23 22 27 63 11 33 9 3 41 <1 79 35 1 9 15 12 8 11 13 18 23 2009 8 22 19 26 65 13 31 11 3 43 <1 83 38 3 9 16 11 8 8 16 19 25
178
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=1 402 % total % PNSP 97 3 59 38 3 14 4 40 40 2 8 25 1 64 2 22 21 22 23 10 36 13 22 29 22 24 27 24 26 26 S. aureus n=3 220 % total % MRSA 100 65 33 2 4 3 37 55 1 12 35 9 42 2 26 26 28 19 7 9 20 32 19 32 28 32 20 25 E. coli n=7 420 % total % FREC 100 <1 51 47 2 3 1 29 66 1 5 29 7 58 1 32 0 36 28 31 9 13 24 30 18 30 30 26 26 29 E. faecalis n=1 463 % total % VRE 100 61 36 3 8 1 31 57 3 21 26 10 41 1 0 0 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=631 % total % VRE 100 60 38 2 6 1 35 57 1 16 29 14 39 2 2 3 1 0 0 10 4 2 0 3 3 0 2 0 K. pneumoniae n=1 267 % total % CRKP 100 58 39 3 5 1 34 58 3 12 29 9 49 1 12 12 11 16 19 16 10 10 10 15 8 12 11 11 P. aeruginosa n=1 087 % total % CRPA 100 68 30 2 3 1 37 58 2 23 28 7 40 1 15 16 12 4 2 8 19 12 6 26 12 21 8 7
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
179
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Spain
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
ES047 (0/15) ES029 (1/15) ES043 (3/36) ES011 (7/75) ES018 (2/21) ES038 (8/76) ES015 (3/23) ES044 (14/86) ES042 (20/118) ES058 (15/85) ES046 (6/34) ES059 (4/19)
N laboratories Minimum First quartile Median Third quartile Maximum
32 0 16.6 23.5 34.3 60
ES043A (8/78) ES021A (20/173) ES051A (5/40) ES046A (6/47) ES047A (8/54) ES048A (13/82) ES032A (9/54) ES042A (17/96) ES003A (5/27) ES044A (23/122) ES016A (13/61) ES011A (14/65) ES015A (4/18)
N hospitals Minimum First quartile Median Third quartile Maximum
33 10.3 18.5 25 30.9 47.7
ES005 (13/61) ES058A (31/137) ES019 (14/63) ES038A (33/141)
Laboratory codes
ES048 (14/60)
Hospital codes 0 25 50 75 100
ES005A (23/94) ES010A (22/88) ES018A (14/54) ES053A (19/72)
ES057 (7/30) ES010 (13/55) ES004 (9/38) ES049 (3/12)
ES013A (28/106) ES012 (12/48) ES031A (55/204) ES021 (22/86) ES004A (44/160) ES031 (21/73) ES060 (8/26) ES016 (9/28) ES056 (20/55) ES002 (16/43) ES017 (5/13) ES053 (14/36) ES032 (15/38) ES051 (4/10) ES003 (9/19) ES013 (3/5) ES019A (71/242) ES060A (49/166) ES041A (50/162) ES059A (13/39) ES012A (47/138) ES057A (13/36) ES002A (40/110) ES029A (19/52) ES049A (32/80) ES056A (54/134) ES017A (41/86)
25
50
75
100
180
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 31 0 4.8 9.1 13.5 32.1
ES011A (47/232) ES057A (28/136) ES029A (26/113) ES021A (107/404) ES032A (43/160) ES018A (64/236)
N hospitals Minimum First quartile Median Third quartile Maximum
33 20.3 28.7 32.9 35.2 45.9
ES017A (0/12) ES032A (0/21) ES015A (0/9) ES051A (0/17) ES029A (0/8) ES011A (1/39)
ES058A (81/293) ES049A (1/30) ES042A (127/444) ES058A (4/84) ES051A (27/94) ES018A (2/38) ES046A (26/90) ES041A (3/57) ES005A (100/334) ES053A (37/123) ES038A (99/323) ES013A (35/113) ES002A (93/297) ES047A (1/18) ES010A (2/35) ES019A (1/16) ES046A (2/32)
Hospital codes
Hospital codes 0 25 50 75 100
ES044A (97/300) ES010A (92/280) ES049A (36/109) ES019A (183/552) ES012A (82/246) ES041A (75/225) ES060A (87/255) ES048A (60/174)
ES053A (3/33) ES042A (8/88) ES038A (5/54) ES044A (8/77) ES005A (5/48) ES059A (3/26) ES004A (5/42) ES056A (10/77)
ES043A (69/198) ES057A (3/23) ES016A (45/128) ES021A (7/52) ES004A (104/294) ES016A (2/14) ES059A (58/157) ES002A (10/62) ES031A (154/399) ES003A (47/121) ES017A (39/99) ES056A (161/391) ES047A (26/61) ES015A (17/37) ES060A (12/68) ES031A (13/65) ES012A (8/34) ES013A (9/30) ES043A (18/56)
25
50
75
100
181
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Sweden
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 21 830 21 919 21 955 21 1 025 21 996 21 1 032 21 1 219 19 1 061 S. aureus Labs Isolates 21 1 837 21 1 855 21 1 906 21 1 774 21 1 968 21 2 163 21 2 410 19 2 459 E. coli Labs Isolates 21 3 066 21 3 350 21 3 372 21 3 241 20 3 539 20 3 749 20 4 032 18 4 245 Enterecocci Labs Isolates 21 695 21 850 21 856 21 821 21 884 21 932 21 1 059 19 967 K. pneumoniae Labs Isolates 18 282 20 621 20 649 20 826 18 705 P. aeruginosa Labs Isolates 17 149 18 300 20 343 20 315 18 338
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 <1 2 6 <1 25 <1 5 <1 1 <1 75 <1 2003 <1 5 5 <1 29 1 7 <1 <1 17 <1 77 11 2 2004 <1 3 5 <1 23 1 8 <1 <1 16 <1 78 7 1 2005 <1 4 6 1 26 1 6 1 <1 19 <1 74 4 <1 1 5 1 9 5 18 <1 6 2006 <1 2 5 <1 28 2 8 2 <1 20 <1 76 12 <1 <1 5 1 <1 6 5 <1 5 2007 <1 3 5 <1 33 2 10 2 <1 16 <1 79 14 <1 1 6 1 2 4 7 <1 6 2008 <1 2 6 <1 32 2 10 2 <1 20 <1 82 25 2 1 7 2 1 5 4 <1 5 2009 2 3 4 1 33 2 8 3 <1 19 <1 76 24 <1 <1 2 2 2 7 8 <1 7
182
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=2 271 % total % PNSP 98 2 50 50 5 2 41 51 <1 7 44 4 44 <1 3 3 2 3 5 4 2 3 0 2 3 2 3 0 S. aureus n=4 865 % total % MRSA 100 62 38 <1 4 4 33 60 <1 6 41 16 37 <1 1 1 1 0 1 0 1 1 13 1 1 1 1 0 E. coli n=5 176 % total % FREC 100 45 55 1 1 25 73 <1 4 40 20 36 <1 10 12 7 3 6 10 7 0 8 7 8 9 33 E. faecalis n=1 283 % total % VRE 100 70 30 5 1 24 69 6 34 24 36 <1 0 0 0 0 0 0 0 0 0 0 0 0 E. faecium n=554 % total % VRE 100 57 43 3 1 31 65 10 35 27 28 <1 1 1 1 0 0 2 1 2 0 1 1 0 K. pneumoniae n=1 526 % total % CRKP 100 <1 60 40 2 1 24 73 <1 4 38 25 33 <1 2 0 2 2 4 0 3 1 0 2 2 1 2 20 P. aeruginosa n=605 % total % CRPA 100 68 32 2 2 26 70 7 42 14 37 <1 6 6 6 11 12 8 6 13 7 5 5 33
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
183
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
Sweden
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
SE440 (0/135)
SE730 (0/76)
N laboratories Minimum First quartile Median Third quartile Maximum
21 0 1.2 2.2 3 9.3
SE620B (0/32) SE240B (0/30) SE240C (0/53) SE610B (0/37) SE220B (0/64) SE400A (0/140) SE430D (0/48) SE450D (0/39) SE400B (0/112)
N hospitals Minimum First quartile Median Third quartile Maximum
55 0 0 0 1.1 3.7
SE400 (1/123)
SE600 (1/98)
SE610C (0/81) SE730D (0/17) SE110B (0/36) SE440C (0/42) SE620C (0/36)
SE430 (1/94)
SE320 (1/86)
SE200D (0/7) SE300A (0/74) SE610A (0/176) SE400C (0/31) SE730C (0/17) SE730B (0/22) SE100C (0/50) SE450B (0/29)
SE350 (2/113)
SE610 (2/111)
SE300 (1/47)
SE730F (0/86) SE230A (0/83) SE730E (0/26)
Laboratory codes
SE620 (3/136)
Hospital codes 0 25 50 75 100
SE620D (0/14) SE440A (0/136) SE120B (0/23) SE220C (0/11) SE320C (0/20) SE200C (0/32) SE440B (0/52) SE230B (0/30) SE320B (0/44) SE450A (1/160)
SE450 (2/89)
SE200 (6/260)
SE220 (1/42)
SE120 (5/192)
SE430A (1/157) SE100A (2/302) SE250A (1/150) SE240A (1/135) SE350A (1/134) SE350C (1/98) SE220A (1/94) SE310A (3/258)
SE240 (3/105)
SE310 (3/99)
SE230 (2/56)
SE120A (3/233) SE320A (2/153) SE200A (3/228) SE110A (1/76) SE250B (1/66)
SE100 (12/231)
SE540 (2/34)
SE100B (3/187) SE620A (3/166) SE600A (5/250)
SE250 (6/90)
SE600C (1/45) SE350B (1/40) SE200B (4/144) SE540A (2/54)
SE110 (5/54)
25
50
75
100
184
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
SE320B (0/12) SE220D (0/5) SE350B (0/16) SE440A (0/51) SE440B (0/26) SE610B (0/10) SE620A (0/46) SE610C (0/33) SE200C (0/15) SE240A (0/28) SE220A (0/40) SE450B (0/25) SE110A (0/25) SE240C (0/9) SE440C (0/10) SE250A (0/44) SE120B (0/8) SE620C (0/16) SE450D (0/11) SE300A (0/24) SE100C (0/10) SE730F (0/18) N hospitals Minimum First quartile Median Third quartile Maximum 48 0 0 0 3.3 18.2
SE730D (0/20) SE230B (0/20) SE350B (0/64) SE620D (0/24) SE610C (2/60) SE350C (3/82) SE320C (3/79) SE730E (1/26) SE400C (3/68) SE440B (4/89) SE400B (8/146) SE450A (13/237) SE620C (4/71) SE120B (2/34) SE450B (5/85) SE730C (1/17) SE310A (13/209) SE620A (13/194) SE440A (24/340) SE450D (6/79) SE220B (6/75) SE320A (23/280) SE730F (6/71)
N hospitals Minimum First quartile Median Third quartile Maximum
50 0 5.6 9 12.4 27.3
Hospital codes
Hospital codes 0 25 50 75 100
SE300A (12/136) SE430A (26/294) SE730B (1/11) SE400A (21/231) SE540A (4/44) SE220D (1/11) SE120A (33/360) SE610A (12/126) SE430D (8/83) SE440C (6/60) SE240A (12/116) SE620B (6/56) SE350A (10/89) SE110B (4/33) SE110A (13/105) SE320B (11/87) SE220A (18/128) SE230A (9/62) SE240B (3/19) SE250B (10/61) SE240C (7/40) SE250A (19/106) SE100B (38/208) SE610B (6/31) SE100A (52/235) SE100C (8/36) SE220C (6/22)
SE220B (0/19) SE230B (0/8) SE400C (0/9) SE350C (0/26) SE540A (0/21) SE430D (0/11) SE610A (0/58) SE450A (0/48) SE100B (1/61) SE430A (1/59) SE320A (1/55) SE350A (1/46) SE200A (2/78) SE200B (2/61) SE230A (1/30) SE120A (3/82) SE250B (1/27) SE100A (4/108) SE400A (2/54) SE400B (1/26) SE310A (5/87) SE220C (1/11) SE240B (1/10) SE110B (1/9) SE730E (1/6) SE620B (2/11)
25
50
75
100
185
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
United Kingdom
General information about EARS-Net participating laboratories
Table 1: Number of laboratories and number of isolates reported for the period 20022009
Year 2002 2003 2004 2005 2006 2007 2008 2009 S. pneumoniae Labs Isolates 23 617 50 1 334 54 1 059 53 1 375 51 1 514 50 1 785 51 1 223 59 1 396 S. aureus Labs Isolates 21 1 588 51 3 548 54 3 562 58 3 971 55 4 132 55 4 865 55 3 355 69 2 977 E. coli Labs Isolates 20 1 958 19 2 253 20 2 091 23 2 359 26 2 438 20 2 374 15 2 456 28 4 712 Enterecocci Labs Isolates 27 591 22 547 18 435 14 274 26 712 K. pneumoniae Labs Isolates 23 420 22 404 18 382 15 350 27 725 P. aeruginosa Labs Isolates 25 438 24 353 19 370 14 345 26 639
Antibiotic resistance from 2002 to 2009
Table 2: Proportion (%) of antibiotic non-susceptible isolates
Pathogens by antimicrobial classes Streptococcus pneumoniae Penicillin R Penicillin RI Macrolides RI Staphylococcus aureus Oxacillin/Meticillin R Escherichia coli Aminopenicilins R Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Enterococcus faecalis Aminopenicilins RI HL Gentamicin R Vancomycin R Enterococcus faecium Aminopenicilins RI HL Gentamicin R Vancomycin R Klebsiella pneumoniae Aminoglycosides R Fluoroquinolones R Third-gen. cephalosporins R Pseudomonas aeruginosa Piperacillin R Ceftazidime R Carbapenems R Aminoglycosides R Fluoroquinolones R 2002 3 6 13 47 52 3 7 2 2003 1 5 13 44 55 4 11 3 2004 <1 3 13 44 53 6 14 3 2005 2 4 11 44 56 8 17 6 2 47 2 84 53 33 6 12 12 2 3 9 3 8 2006 <1 3 12 42 57 7 20 8 3 52 1 78 18 18 8 13 11 1 3 6 3 8 2007 2 4 10 36 55 7 18 9 4 31 2 82 35 21 9 12 13 5 7 10 5 9 2008 1 5 6 31 61 7 15 7 2 42 4 83 7 28 6 7 7 2 4 6 3 8 2009 1 3 4 28 62 7 18 9 2 38 2 91 38 13 5 6 7 3 5 8 1 7
186
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Demographic characteristics
Table 3: Selected details on invasive isolates from the reporting period 2008 and 2009
Characteristic S. pneumoniae n=2 477 % total % PNSP 99 1 52 47 1 9 4 36 39 12 5 24 1 36 34 4 3 4 4 0 4 4 3 5 3 3 4 3 4 4 S. aureus n=6 233 % total % MRSA 100 61 38 1 4 2 35 49 10 7 26 8 34 25 29 31 27 14 14 13 32 47 42 56 41 50 34 35 E. coli n=6 500 % total % FREC 100 46 53 <1 3 1 26 70 <1 100 17 19 15 35 7 9 16 16 20 16 E. faecalis n=572 % total % VRE 100 62 38 8 1 31 60 <1 100 2 3 1 2 0 3 2 100 2 E. faecium n=354 % total % VRE 100 54 44 3 6 3 39 51 100 17 13 21 22 21 30 29 16 22 K. pneumoniae n=953 % total % CRKP 100 61 38 <1 4 1 31 63 <1 100 7 8 6 0 6 12 10 10 0 9 P. aeruginosa n=759 % total % CRPA 100 64 35 <1 4 3 31 63 100 8 6 11 0 7 18 12 6 8
Isolate source Blood CSF Gender Male Female Unknown Age (years) 04 519 2064 65 and over Unknown Hospital department ICU Internal med. Surgery Other Unknown
PNSP: penicillin-non-susceptible S. pneumoniae; MRSA: meticillin-resistant S. aureus; FREC: fluoroquinolone-resistant E. coli; VRE: vancomycin-resistant Enterococcus; CRKP: third-generation cephalosporin-resistant K. pneumoniae; CRPA: carbapenems-resistant P. aeruginosa.
187
Antimicrobial resistance surveillance in Europe 2009
SURVEILLANCE REPORT
United Kingdom
Figure 1: Proportion (%) of penicillin-non-susceptible S.pneumonia by laboratory (20082009) Figure 2: Proportion (%) of meticillin-resistant S.aureus by hospital (20082009)
UK046 (0/32) UK078 (0/33) UK096 (0/30) UK102 (0/14) UK057 (0/26) UK010 (0/18) UK063 (0/37) UK058 (0/14) UK027 (0/16) UK080 (0/9) UK094 (0/40) UK048 (0/16) UK004 (0/29) UK052 (0/20) UK001 (0/31) UK050 (0/18) UK097 (0/18) UK060 (0/12) UK077 (0/17) UK049 (0/11) UK092 (0/31) UK051 (1/71) UK101 (1/62) UK069 (1/55) UK047 (2/105) UK007 (3/147) UK015 (1/43) UK059 (2/79) UK068 (2/77) UK098 (1/38) UK070 (1/35) UK066 (1/34) UK056 (1/32) UK054 (2/59) UK008 (1/29) UK045 (4/115) UK090 (2/55) UK017 (2/55) UK012 (4/92) UK055 (1/23) UK081 (1/21) UK031 (1/21) UK064 (3/60) UK023 (2/39) UK091 (2/38) UK032 (4/75) UK053 (2/36) UK020 (2/36) UK011 (2/31) UK076 (3/43) UK100 (1/14) UK099 (5/69) UK033 (2/27) UK044 (3/36) UK043 (8/95) UK093 (3/34) UK005 (4/42) UK042 (3/31) UK084 (6/37) UK038 (4/11)
N laboratories Minimum First quartile Median Third quartile Maximum
60 0 0 2.7 5.3 36.4
UK072X (1/25) UK100X (2/25) UK078B (2/23) UK078C (3/34) UK101X (16/154) UK010A (3/28) UK055X (4/35) UK092X (7/57) UK055A (2/14) UK090A (10/68) UK098X (11/74) UK001A (5/33) UK026C (5/33) UK076D (5/32) UK096X (10/62) UK059A (7/43) UK102X (7/42) UK046X (3/18) UK033X (10/57) UK093X (19/106) UK066X (10/55) UK044B (2/11) UK053X (8/41) UK007C (1/5) UK099X (28/140) UK057A (6/29) UK007A (24/115) UK097X (6/28) UK064A (9/42) UK060X (4/18) UK047B (2/9) UK015A (6/27) UK091X (21/94) UK026A (19/83) UK023A (16/69) UK012A (14/60) UK026B (19/80) UK015B (4/16) UK007B (21/83) UK050X (11/43) UK045X (43/168) UK064X (30/117) UK056A (17/64) UK020A (12/45) UK053D (11/40) UK076A (26/94) UK046A (5/18) UK081B (4/14) UK054X (18/63) UK059X (32/111) UK054A (11/37) UK048X (15/50) UK032A (15/50) UK047X (82/271) UK049X (10/33) UK011A (17/56) UK068X (57/186) UK027A (12/39) UK052X (9/29) UK063X (16/51) UK052A (8/25) UK059B (9/28) UK069X (34/105) UK057X (12/37) UK044D (6/18) UK017B (38/113) UK056X (31/92) UK084A (26/77) UK070X (25/74) UK044A (49/144) UK047A (66/193) UK005A (38/111) UK068B (45/129) UK008A (14/40) UK051A (27/77) UK069A (19/54) UK050A (12/34) UK017A (11/31) UK077A (16/45) UK051X (46/129) UK045A (47/130) UK084B (7/19) UK032B (13/34) UK072A (5/13) UK063A (9/23) UK031A (17/43) UK070B (4/10) UK045B (2/5) UK043A (57/137) UK078A (62/149) UK070A (16/38) UK080A (36/85) UK066A (9/21) UK048A (12/28) UK060A (16/36) UK083A (62/137) UK044C (8/17) UK049A (10/21) UK038C (3/6) UK081A (10/19) UK043C (4/7) UK084E (10/17) UK065X (3/5) UK043B (16/26) UK004A (5/7) UK058X (5/6) UK090X (17/17) UK094X (6/6)
N hospitals Minimum First quartile Median Third quartile Maximum
108 4 21.1 30.3 36.5 100
Laboratory codes
25
50
75
100
Hospital codes
25
50
75
100
188
SURVEILLANCE REPORT
Antimicrobial resistance surveillance in Europe 2009
Figure 3: Proportion (%) of fluoroquinolone-resistant E.coli by hospital (20082009)
Figure 4: Proportion (%) of third-generation cephalosporin-resistant K.pneumoniae by hospital (20082009)
N hospitals Minimum First quartile Median Third quartile Maximum 23 0 0 4.9 9.1 13.3
UK090X (1/58) UK001X (9/124) UK023X (51/572) UK033X (19/171) UK008X (16/143) UK032X (71/630)
N hospitals Minimum First quartile Median Third quartile Maximum
31 1.7 14.6 17.4 22.1 47.5
UK100X (0/14)
UK090X (0/5)
UK023X (0/43)
UK011X (0/31)
UK008X (0/16) UK098X (31/221) UK038X (22/151) UK091X (37/251) UK017X (70/455) UK015X (6/156) UK031X (8/52) UK102X (14/86) UK093X (3/18) UK096X (25/149) UK092X (1/25) UK098X (0/19)
UK033X (1/31)
UK096X (1/25)
Hospital codes
UK027X (24/143) UK015X (171/982) UK097X (16/91) UK011X (42/225) UK100X (11/55) UK101X (79/391) UK092X (32/157)
Hospital codes 0 25 50 75 100
UK017X (3/66)
UK099X (3/61)
UK027X (1/19)
UK042X (1/15)
UK026X (3/33)
UK091X (5/55) UK042X (19/90) UK099X (82/383) UK012X (86/390) UK005X (28/105) UK020X (1/11) UK020X (20/74) UK026X (35/128) UK043X (37/105) UK094X (16/40) UK032X (18/147) UK007X (9/20) UK003X (19/40) UK038X (2/15) UK097X (1/9) UK101X (7/77)
UK102X (2/22)
UK012X (5/44)
25
50
75
100
189
HOW TO OBTAIN EU PUBLICATIONS
Free publications:
via EU Bookshop (http://bookshop.europa.eu); at the European Commissions representations or delegations. You can obtain their contact details on the Internet (http://ec.europa.eu) or by sending a fax to +352 2929-42758.
Priced publications:
via EU Bookshop (http://bookshop.europa.eu). Priced subscriptions (e.g. annual series of the Official Journal of the European Union and reports of cases before the Court of Justice of the European Union): via one of the sales agents of the Publications Office of the European Union(http://publications.europa.eu/others/agents/index_en.htm).
TQ-AM-10-580-EN-C
European Centre for Disease Prevention and Control (ECDC) Postal address: ECDC, 171 83 Stockholm, Sweden Visiting address: Tomtebodavgen 11a, Solna, Sweden Phone +46 (0)8 58 60 1000 Fax +46 (0)8 58 60 1001 www.ecdc.europa.eu An agency of the European Union www.europa.eu
Вам также может понравиться
- 2012 EU Legislation General Food LawДокумент5 страниц2012 EU Legislation General Food Lawmais_bОценок пока нет
- Eat Well PlateДокумент1 страницаEat Well PlatePathan Imran KhanОценок пока нет
- Eurostatistics-Food-From Farm To Fork Statistics-2008 EdДокумент199 страницEurostatistics-Food-From Farm To Fork Statistics-2008 EdCIO-CIOОценок пока нет
- Comparison of International Food Guide Pictorial RepresentationsДокумент7 страницComparison of International Food Guide Pictorial Representationsmais_bОценок пока нет
- Tatfar Report ARДокумент47 страницTatfar Report ARmais_bОценок пока нет
- Socio-cultural Determinants of Innovation in the Food and Drink SectorДокумент56 страницSocio-cultural Determinants of Innovation in the Food and Drink Sectormais_bОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Nama: Yetri Muliza Nim: 180101152 Bahasa Inggris V Reading Comprehension A. Read The Text Carefully and Answer The Questions! (40 Points)Документ3 страницыNama: Yetri Muliza Nim: 180101152 Bahasa Inggris V Reading Comprehension A. Read The Text Carefully and Answer The Questions! (40 Points)Yetri MulizaОценок пока нет
- Pom Final On Rice MillДокумент21 страницаPom Final On Rice MillKashif AliОценок пока нет
- Biagioli Did Galileo Copy The TelescopeДокумент28 страницBiagioli Did Galileo Copy The TelescopeGregory HooОценок пока нет
- PESO Online Explosives-Returns SystemДокумент1 страницаPESO Online Explosives-Returns Systemgirinandini0% (1)
- Casting Procedures and Defects GuideДокумент91 страницаCasting Procedures and Defects GuideJitender Reddy0% (1)
- Katie Tiller ResumeДокумент4 страницыKatie Tiller Resumeapi-439032471Оценок пока нет
- Forensic Science From The Crime Scene To The Crime Lab 2nd Edition Richard Saferstein Test BankДокумент36 страницForensic Science From The Crime Scene To The Crime Lab 2nd Edition Richard Saferstein Test Bankhilaryazariaqtoec4100% (25)
- Lecture02 NoteДокумент23 страницыLecture02 NoteJibril JundiОценок пока нет
- Write UpДокумент5 страницWrite Upmourad baОценок пока нет
- 8.1 Interaction Diagrams: Interaction Diagrams Are Used To Model The Dynamic Aspects of A Software SystemДокумент13 страниц8.1 Interaction Diagrams: Interaction Diagrams Are Used To Model The Dynamic Aspects of A Software SystemSatish JadhaoОценок пока нет
- Exp 8 - GPG - D12B - 74 PDFДокумент4 страницыExp 8 - GPG - D12B - 74 PDFPRATIKSHA WADIBHASMEОценок пока нет
- Data Sheet: Experiment 5: Factors Affecting Reaction RateДокумент4 страницыData Sheet: Experiment 5: Factors Affecting Reaction Ratesmuyet lêОценок пока нет
- Simply Put - ENT EAR LECTURE NOTESДокумент48 страницSimply Put - ENT EAR LECTURE NOTESCedric KyekyeОценок пока нет
- Origins and Rise of the Elite Janissary CorpsДокумент11 страницOrigins and Rise of the Elite Janissary CorpsScottie GreenОценок пока нет
- Theory of Linear Programming: Standard Form and HistoryДокумент42 страницыTheory of Linear Programming: Standard Form and HistoryJayakumarОценок пока нет
- UAPPДокумент91 страницаUAPPMassimiliano de StellaОценок пока нет
- Skuld List of CorrespondentДокумент351 страницаSkuld List of CorrespondentKASHANОценок пока нет
- Family Service and Progress Record: Daughter SeptemberДокумент29 страницFamily Service and Progress Record: Daughter SeptemberKathleen Kae Carmona TanОценок пока нет
- Rubber Chemical Resistance Chart V001MAR17Документ27 страницRubber Chemical Resistance Chart V001MAR17Deepak patilОценок пока нет
- Attributes and DialogsДокумент29 страницAttributes and DialogsErdenegombo MunkhbaatarОценок пока нет
- Marketing Plan for Monuro Clothing Store Expansion into CroatiaДокумент35 страницMarketing Plan for Monuro Clothing Store Expansion into CroatiaMuamer ĆimićОценок пока нет
- Resume of Deliagonzalez34 - 1Документ2 страницыResume of Deliagonzalez34 - 1api-24443855Оценок пока нет
- SQL Guide AdvancedДокумент26 страницSQL Guide AdvancedRustik2020Оценок пока нет
- CIT 3150 Computer Systems ArchitectureДокумент3 страницыCIT 3150 Computer Systems ArchitectureMatheen TabidОценок пока нет
- DC Motor Dynamics Data Acquisition, Parameters Estimation and Implementation of Cascade ControlДокумент5 страницDC Motor Dynamics Data Acquisition, Parameters Estimation and Implementation of Cascade ControlAlisson Magalhães Silva MagalhãesОценок пока нет
- Insider Threat ManagementДокумент48 страницInsider Threat ManagementPatricia LehmanОценок пока нет
- Resume Template & Cover Letter Bu YoДокумент4 страницыResume Template & Cover Letter Bu YoRifqi MuttaqinОценок пока нет
- Philippine Coastal Management Guidebook Series No. 8Документ182 страницыPhilippine Coastal Management Guidebook Series No. 8Carl100% (1)
- ISO 9001:2015 Explained, Fourth Edition GuideДокумент3 страницыISO 9001:2015 Explained, Fourth Edition GuideiresendizОценок пока нет
- Annamalai International Journal of Business Studies and Research AijbsrДокумент2 страницыAnnamalai International Journal of Business Studies and Research AijbsrNisha NishaОценок пока нет