Академический Документы
Профессиональный Документы
Культура Документы
Optimal Operating Room Design: C Caatthhrryynn Bbaanngg
Загружено:
AldoSantИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Optimal Operating Room Design: C Caatthhrryynn Bbaanngg
Загружено:
AldoSantАвторское право:
Доступные форматы
OPTIMAL OPERATING ROOM DESIGN (3)
OPTIMAL OPERA TING ROOM DESIGN
Cathryn Bang /
Operating rooms planned and built today must be considered to have a working lifetime measured in decades. Predictions about the details of future ORs are neither accurate nor useful. However, principles can be followed to give any design a more successful working lifetime: Think about how practices have changed over the last ten years and then consider how design can accommodate a like amount of change. Flexibility is fundamental to robust design. Participation in future technologies should be phased.
Surgery Department become old and must modernize in order to improve the quality of patient care. Regardless of the age of a facility, healthcare facilities must continually change in order to meet patient demands, support new procedures and technologies, and remain competitive.
Like other healthcare design, operating room design is a multi-constituency environment. Under-standing the roles of key players is an
important part of success, involving: Steeling Committee Clinical Staff Surgical Services Managers Surgeons and Anesthesiologists Administration Contractors Architects Engineers Equipment Planners Bio-medical Personnel Infection Control Hospital Facilities Maintenance Early clinical input is important to the success of the project. All staffs involved directly in the design process must be made to realize that they must also act as ambassadors to all of the staff not able to participate directly. Who designed this place? are the last words planners, programmers, architects, engineers and contractors want to hear. Senior level staff should be engaged early in the process with line staff becoming involved as greater levels of detail are reached.
in the organization. Fundamental characteristics of the desired culture must be identified at the inception of the project. Organizational structure must be congruent with the proposed function of the new environment. This raises questions for each individual about their place in the new structure. These questions must be answered. The management challenge is to: Build consensus among competing interests Allocate resources Identify and harness existing expertise Communicate with multiple constituencies Change is encouraged by examining how everything is done and by researching best practice models. Enthusiasm for change can be developed by involving staff in data collection regarding existing conditions, data collection and analysis regarding utilization, and definition of operational assumptions. Guiding questions might include: What new services should the hospital offer? How can patient satisfaction be maximized through good departmental layout? What inconveniences and inefficiencies in the current department layout might be eliminated? New Processes must be created before moving into new space. The expectation must be that
Major projects represent an opportune time to implement culture change - although not without drawbacks. Changing both culture and environment is disruptive and unsettling to many
OPTIMAL OPERATING ROOM DESIGN (3)
changes will be implemented from opening day.
Telecom/Data Air Quality and Infection Control Each of these topics possesses its own trends and conventions. Each poses particular risks and challenges for the institution but in these challenges lies the opportunity to develop superior design solutions. The key characteristics are: Let s look at each of these individually before examining how they interact as design opportunities.
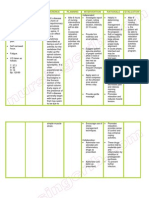
During the design of Surgery Department project, following six topics should be significant design decisions: Patient Needs Equipment Utilities Space and Room Sizes
TOPIC Patient
TREND or CONVENTION RISK/CHALLENGE Sicker but expecting Patients are in more Every-larger health gains critical condition, Procedures more aggressive More of it, most Mounted on carts for Increased congestion, entrapment
OPPORTUNITY Gains in health of community served, distinction and reputation of the hospital Rethink the conventional ergonomic solutions View data as part of OR infrastructure, as infrastructure need
Equipment
Data
More objects generate data that needs to be transmitted, displayed and recorded Expanding number of types, increasing quantities Ever-larger rooms
Fragments, proprietary systems
Utilities
Room walls as utility infrastructure no longer serves well Costly, does not serve to put needed items in optimum locations Costly energy usage, little assurance of effectiveness
Find alternatives to delivering utilities to point of use Use "Human Factors" approach to reorganize the OR workplace Apply objective analysis to improve performance and reduce cost
Space/Room
Heating, Greater air volumes, Ventilation, empirical design rules Air Conditioning
Patients In design projects, it is a good general practice to periodically and intentionally bring together all points of view for a decision validation review - balance is the goal. In these reviews and in the day-to-day decision making, particularly where there is intense competition for resources, it becomes easy to overlook the patient s point of view. If patients don t have the designated advocates, then appoint one. Never forget that all of this effort is ultimately about the patient and doing the best that can be done for them. From the standpoint of judgments patients will make, the spaces most relevant to them are the intake waiting and registration spaces, the prep or pre-operative space and to a less extent the recovery space. Undersized or poorly designed pre-operative spaces can significantly impact the throughput of operating rooms. With the possible exception of the Perioperative Manager, it is patients who suffer the most stress when operating rooms are delayed. Therefore the size, capacity and efficiency of the pre and postoperative spaces impact the patient experience as much as do finishes, lighting and color. Other important characteristics of the pre and postoperative spaces are: Patient Bays that are hard wall on three
sides. Division of the PACU (Post Anesthesia Care Unit) into 10-12 bed modules. Planning for the use of beds instead of stretchers. Individually controlled lighting in each patient bay. Provisions for companions before and after surgery. Patients are sicker, and surgical aspirations are more ambitious, which combine to keep average inpatient case times from declining much if at all. Companions are going to be guests in your waiting rooms for longer durations. In addition to a pre-registration system which will hopefully speed patients through registration and on to prep and holding, thought has been given to support for families and companions who will later help form the overall opinion of the quality of the stay. Amenities include: Higher Level of Finish. A Business Center with desk space for individuals to make calls, work on laptops, etc. Sequestered Television Areas. A Coffee and Refreshment Bar Lockers large enough to hold the suitcases many patients still bring with them. Video-Consult Booths to reduce travel, particularly for intra-operative updates.
OPTIMAL OPERATING ROOM DESIGN (3)
Equipment Regardless of the size of the room, the limitations of doctors and nurses convenient reach and vision have not increased over the last hundred years. To be used efficiently by the surgical team, instruments, supplies and equipment must enter a zone immediately adjacent to the operating room table. Anything outside this reach zone must be remotely operated or must be moved before being put into use. The space within reach is the most valuable real estate in the operating room. To enhance flexibility, the conventional practice of instrument and equipment manufacturers has been to place equipment on a cart. Low-density, cart-mounted equipment wastes the most valuable real estate in the operating room, the space within reach . Common operating room equipment such as IV poles, light sources, suction canisters and electrocautery can waste as much as one-third to one-half of the space within reach . A design approach which recognizes human factors and which raises the density of equipment around the operating room table is a key factor in designing efficient operating rooms. Utilities Remember when placing that one, specialvoltage outlet was a key design decision?
Contemporary operating rooms demand enormous amounts of power, special circuitry, easily a half-dozen different medical gases, data, communications, video, just to name the basics. As operating rooms become larger, continuing to use the walls of the room as the infrastructure to carry all of these utilities simply means that what you need is further and further away from the operating room table. Draping dozens of cords and hoses across the floor is neither a safe nor efficient workplace. Changing the physical location of those utility connections requires the involvement of the contractor, creation of dust and closure of an operating room. Even the conventional medical gas column is limited in its ability to meet current demands. Materials and methods, and design techniques that deliver what you need where it is needed, is another key factor in designing efficient operating rooms. Data Take a minute for a mental count of the number of different systems that carry information to, from and through the operating room suite. How many come to mind? A dozen? Two dozen? For a recent project, knowledgeable constituents were asked to assemble a comprehensive list; it has 52 systems listed. It is time to quit thinking of data as a few wires snaking through the walls or even as your data network. Data should be thought of as part of the
infrastructure and should be addressed as such by the design and construction teams. Further, there is growing recognition of the need within the operating room to record data, to receive data from outside the operating room and to send data to other points in the hospital. Potential data sources include: Anesthesia Equipment Physiological Monitoring Minimally Invasive Equipment Archived Images Real-Time Images Cameras Coaxial with Operating Room Lights (and in other locations in the room) Pathology (video from microscope) Lab Information System Hospital Information System Clinical Documentation Data destinations include: On-Service Boom Monitors Wall-Mounted Monitors Recording Devices (DVD, CD and a VCR) Pathology (view of the surgical site) Teaching Clinical Conferences Consultation In-Room Documentation A few manufacturers have recognized that collecting, routing and recording both data and
video presents a growing need in the operating room. A more comprehensive view which takes into account the multiple relationships operating rooms have with the hospital and which attempts to project recent trends into the future quickly comes to the conclusion that a digital switching system will become a requirement of designing an effective operating rooms. Room Size The growth of cart-mounted equipment in the operating room has already been remarked upon. This equipment is important because it has been a factor supporting new and evolving surgical techniques. Placing equipment on a cart has been both a convenience and an economic response. New (highly specialized and often expensive) equipment was not always intended to be used one procedure after another in the same room. Moving it from the room when not in use was a clear need, as was the ability to relocate a special item from one room to another. Even though the usage pattern of many types of equipment has changed, the practice of placing it all on individual carts has not. This has two consequences: 1) this places all of the equipment at roughly the same working plane across the room, and 2) the volume of each cart sequesters space that is then typically unusable for other purposes. This creates the low-density
OPTIMAL OPERATING ROOM DESIGN (3)
arrangement described earlier. One response to this trend has been to make operating rooms increasingly larger. In turn, larger operating rooms trigger other conditions: 1) all the utilities and other items mounted on walls keep moving farther and farther away from the table, and 2) poor, low-density use of the space within reach around the operating room table fosters inefficient design and function. After description of just one more issue, we will begin discussion of design approaches that turn these dilemmas into opportunities. Ventilation and Air Quality A couple of years ago, Dr. Farhad Memarzadeh of the US National Institute of Health presented his use of computed flow dynamics to analyze the optimum ventilation design for an operating room. Computed flow dynamics was used to track the path of airborne particles, establish clearance rates and tabulate the number of times airborne particles landed on critical locations - the surgical site and the instrument table. In addition to heating and cooling the room, optimum ventilation design has several distinct characteristics: The optimum exchange rate is approximately 20 changes per hour and the surface area of the delivery plane must be sized to discharge air at 30 to 35 feet per minute. Air should be supplies from a laminar flow field in the ceiling that has minimum
interruption and fully covers the operating room table. (We have concluded that this air will also be HEPA filtered.) Return air is taken from grilles located both in the conventional position close to the floor and from high returns at or near the ceiling. This additional return location reduces reentrainment of suspended particles. It is important to note that controlled velocity allows laminar flow to carry particles around solid objects and prevents simple momentum from driving particles onto the surgical site. This arrangement represents best practices in ventilation design. It places some constraints on the geometry of items in and near the ceiling. I will now discuss the integration of this into operating room design.
An effective operating room design springs from these observations: Best use must be made of the most valuable space in the room - the space within reach immediately adjacent to the operating room table. Utilities must be available within reach without creating a snake s nest of tripping
hazards. Attributes of ventilation design place some constraints on room and ceiling geometry. Technologies to enhance flexibility can be borrowed from other industries. As I worked through design solutions for projects, it became clear that the issues of equipment, utilities, technology infrastructure, room size and spatial efficiency were interrelated. The use of service (utility) booms has increased steadily over the last half-dozen years. During visits to other facilities, I noted configurations that began to address the issues of equipment, utilities, technology infrastructure and spatial efficiency. Configurations which were rich in appropriate utilities and which took as many small pieces of equipment as possible off of carts and stacked them on shelves represented particular potential for increasing the planning density. Intelligent use of utility or service booms is an important aspect of effective operating room design because: They serve to recapture space lost to carts, IV poles, canister stands, electrocautery and other small, common devices. They can route utilities directly to the point of use, keeping floors clear. They can also bring data, communi-cations
and imaging to the point of use. They can be configured to move assemblies of bulky items to and from the reach zone while hovering over floor interferences. Mounts for operating room lights can also hold one or more booms appropriate for lightweight, flat panel displays. Lights can be configured with coaxial video cameras in order to capture images that can also be displayed in the space immediately surrounding the operating room table. The key characteristics of optimal operating rooms are: Ability to carry multiple surgical lights as well as service booms for flat panel displays. Air delivery is via a laminar air-flow field which covers the table and immediately adjacent spaces. In addition to the common, central mounting point, every room will have installed at least four additional mounting points, positioned on the axes of the room. In almost every case, the mounting point at the patient head location will receive an anesthesia boom. Almost every operating room will also receive at least one additional service boom, configured to carry equipment common to the specialty and located to support that specialty s particular set up.
OPTIMAL OPERATING ROOM DESIGN (3)
General illumination surrounds the operating room table. In addition, the size of the operating room mandates separately controlled perimeter lighting.
locating myriad communication systems. Modern operating rooms that are expected to be a good chassis for future processes need to be designed in the 600 to 650 square foot range. With high-density arrangements immediately adjacent to the operating room table, sufficient space exists in most plans to create three zones that are sometimes literally marked by changes in the flooring: A central zone centered on the table to denote the surgical area. It serves as a prompt to be certain there is a purpose in approaching the operating room table. A 30 to 36 zone along the walls which is the parking place for items not immediately engaged in the operation such as specialty carts, imaging equipment, and students. The annular space between these two becomes the circulation zone of the room. It should be clear of most, if not all, tripping hazards. Lastly, no single idea will lead to the creation of an effective operating room. Maintain a comprehensive view of everything, from culture to carts, and continually assess how all elements function together.
Several types of adjunct spaces are conventional in OR design: Sub-Sterile Scrub Sinks In-room Storage New spaces/uses are evolving and are crucial to effective design: Equipment and Supply Storage space adjacent to but outside the operating room. In-room documentation station for procedure records, real-time information and electronic recording. Area within the operating room is being marked explicitly to indicate working zones. Ample and handy storage (think of an area onefourth to one-third of the OR square footage) aids in focusing the operating room as a procedural space and avoids marking it a storeroom. In-room documentation provides a dedicated and wellequipped space for manual as well as electronic record keeping and provides a physical focus for
Вам также может понравиться
- Optimal Operating Room Design IIIДокумент9 страницOptimal Operating Room Design IIIMinhОценок пока нет
- Planning Hospitals of The FutureДокумент24 страницыPlanning Hospitals of The FutureutkОценок пока нет
- Research Fifty (50) Bed Level 1 Government General Hospital: College of ArchitectureДокумент29 страницResearch Fifty (50) Bed Level 1 Government General Hospital: College of ArchitectureGerardo, Liano Ezekiel N.Оценок пока нет
- FreemanWhite Hybrid Operating Room Design GuideДокумент11 страницFreemanWhite Hybrid Operating Room Design GuideFaisal KhanОценок пока нет
- Trend 14 FlexibilityДокумент3 страницыTrend 14 FlexibilityBingDelaCruzОценок пока нет
- The Modern Oral and Maxillofacial Surgery O Ce: W. Scott Jenkins, DMD, MDДокумент10 страницThe Modern Oral and Maxillofacial Surgery O Ce: W. Scott Jenkins, DMD, MDГулпе АлексейОценок пока нет
- Hospital Planning and DesignДокумент12 страницHospital Planning and DesignBa Nyar SoeОценок пока нет
- Learning Module NUMBER 3 Establishing and Managing A HIM Department ServiceДокумент25 страницLearning Module NUMBER 3 Establishing and Managing A HIM Department ServiceHalema AlnahdiОценок пока нет
- Within This Page: Building Attributes Emerging Issues Relevant Codes and Standards Additional ResourcesДокумент8 страницWithin This Page: Building Attributes Emerging Issues Relevant Codes and Standards Additional ResourcesMarlon AlanoОценок пока нет
- An Architectural Brief For A Proposed 100 Bedded HospitalДокумент111 страницAn Architectural Brief For A Proposed 100 Bedded Hospitalgshiva1123Оценок пока нет
- Design To OperationДокумент4 страницыDesign To OperationbiomedmaulikОценок пока нет
- Hospital: New Era UniversityДокумент8 страницHospital: New Era UniversityDessa TauroОценок пока нет
- FreemanWhite Hybrid Operating Room Design Guide PDFДокумент11 страницFreemanWhite Hybrid Operating Room Design Guide PDFNana AkwaboahОценок пока нет
- HospitalДокумент11 страницHospitalRafael Martin MusaОценок пока нет
- Hospital: Building AttributesДокумент7 страницHospital: Building AttributesPatricia ParinasОценок пока нет
- Rowland and RowlandДокумент6 страницRowland and RowlandBhell MendiolaОценок пока нет
- General HospitalДокумент12 страницGeneral HospitalSajay PajarillagaОценок пока нет
- Project Title: Hospital Management System Description: Hospital Management System Is A Web Based Project. It Consists of Client RegistrationДокумент68 страницProject Title: Hospital Management System Description: Hospital Management System Is A Web Based Project. It Consists of Client Registrationshahid198950% (2)
- An Automated Medical Duties Scheduling System Using Queing Techniques (Chapter 1-5)Документ19 страницAn Automated Medical Duties Scheduling System Using Queing Techniques (Chapter 1-5)ABUBSAKAR SIDIQ AMINUОценок пока нет
- Research Paper On Hospital DesignДокумент7 страницResearch Paper On Hospital Designj1zijefifin3100% (1)
- Narrative: Section 2Документ6 страницNarrative: Section 2eng_waleed2008Оценок пока нет
- Hospital DefДокумент8 страницHospital DefMaeDaphneYapОценок пока нет
- Griffiths Et Al For PublicationДокумент16 страницGriffiths Et Al For PublicationkrishnavkkОценок пока нет
- A Guide in Practical Psychrometrics for Students and EngineersОт EverandA Guide in Practical Psychrometrics for Students and EngineersОценок пока нет
- Hospital Facility Layout: Design Advisor SponsorДокумент5 страницHospital Facility Layout: Design Advisor Sponsorvangtrangbac_vtОценок пока нет
- MunendraДокумент47 страницMunendrajeetu sharmaОценок пока нет
- Unit 3 Facility Layout PlanningДокумент31 страницаUnit 3 Facility Layout Planningnagpal0384Оценок пока нет
- Final Assigment Operations Management Dec22Документ7 страницFinal Assigment Operations Management Dec22Le JagОценок пока нет
- CRC Handbook of Laboratory SafetyДокумент117 страницCRC Handbook of Laboratory SafetyYovana Parra ParionaОценок пока нет
- Health Facilities Management-February 2015Документ48 страницHealth Facilities Management-February 2015MichaelОценок пока нет
- Assignment 6 Chapter 6Документ3 страницыAssignment 6 Chapter 6Abeba GselassieОценок пока нет
- Chapter 1 Sample ThesisДокумент6 страницChapter 1 Sample ThesisIan Ignacio AgngarayngayОценок пока нет
- Online Clinic Management System ThesisДокумент4 страницыOnline Clinic Management System ThesisBuyEssaysOnlineForCollegeNewark100% (2)
- Operations Management V2 83701Документ9 страницOperations Management V2 83701Vivek SharmaОценок пока нет
- Cooper2010 PDFДокумент13 страницCooper2010 PDFInês AntunesОценок пока нет
- Hospital Design TipsДокумент7 страницHospital Design TipsnidhithackerОценок пока нет
- Operations ManagementДокумент8 страницOperations ManagementAkshatОценок пока нет
- E-Health Care ManagementДокумент92 страницыE-Health Care ManagementbsudheertecОценок пока нет
- Digital Workflows in Contemporary OrthodonticsДокумент7 страницDigital Workflows in Contemporary OrthodonticsAndreaVanoyMartinОценок пока нет
- A Mixed Integer Linear Programing ApproaДокумент30 страницA Mixed Integer Linear Programing ApproaDeepali KoiralaОценок пока нет
- Clinic Management System FinalДокумент6 страницClinic Management System FinalIan Paul Valeza Alberto93% (44)
- Concha - Research On Barangay Hall and Health Center DesignДокумент7 страницConcha - Research On Barangay Hall and Health Center DesignCHRISTINE DIANNE CONCHAОценок пока нет
- Sample Assignment Grade AДокумент26 страницSample Assignment Grade ARakesh Nuguri0% (1)
- Operations ManagementДокумент10 страницOperations ManagementAkshatОценок пока нет
- Significant of Lab Equipment Size and Location On Lab DesignДокумент5 страницSignificant of Lab Equipment Size and Location On Lab DesignMohd Naim Abdul HalimОценок пока нет
- Computer Patient Record System: Lecaros, Langeras, Linaac, Llorente, Macapayad, Polistico, Pasion BSNB-2 NCM 110Документ12 страницComputer Patient Record System: Lecaros, Langeras, Linaac, Llorente, Macapayad, Polistico, Pasion BSNB-2 NCM 110Ashley Jane MacapayadОценок пока нет
- Shaping The Future of HealthcareДокумент24 страницыShaping The Future of HealthcaresriramvsОценок пока нет
- Thesis Documentation Ordering SystemДокумент7 страницThesis Documentation Ordering Systemgj6sr6d7100% (2)
- These Are Examples Where You Can Base Your Business Case This Is Not A Complete DocumentДокумент12 страницThese Are Examples Where You Can Base Your Business Case This Is Not A Complete DocumentCyLo PatricioОценок пока нет
- HMIS Project Report PDFДокумент25 страницHMIS Project Report PDFAther100% (1)
- Sound Engineering Dissertation IdeasДокумент5 страницSound Engineering Dissertation IdeasApaPapersForSaleAtlanta100% (1)
- Value Stream Mapping CaseДокумент13 страницValue Stream Mapping Casesteve.steinОценок пока нет
- Dissertation Building MaintenanceДокумент5 страницDissertation Building MaintenanceBuyCheapPaperCanada100% (1)
- Medical Information SystemsДокумент449 страницMedical Information SystemsavertebrateОценок пока нет
- Some Pointers To Successful Hospital Planning: Good Planning Is Critical To The Hospitals SuccessДокумент16 страницSome Pointers To Successful Hospital Planning: Good Planning Is Critical To The Hospitals SuccesssandeepОценок пока нет
- Thesis of Hospital Management SystemДокумент7 страницThesis of Hospital Management SystemMonica Waters100% (2)
- TopicДокумент2 страницыTopicsimi bhatОценок пока нет
- Chemical Engineering Design: Principles, Practice and Economics of Plant and Process DesignОт EverandChemical Engineering Design: Principles, Practice and Economics of Plant and Process DesignРейтинг: 4 из 5 звезд4/5 (16)
- Hospital DissertationДокумент8 страницHospital DissertationCustomPaperServiceUK100% (1)
- Case Study Presentation-Mindy Duran-FinalДокумент30 страницCase Study Presentation-Mindy Duran-Finalapi-278622211Оценок пока нет
- Non - Food Meher Final Report (2023)Документ87 страницNon - Food Meher Final Report (2023)atakltigebertsadikОценок пока нет
- VBAC MCQsДокумент3 страницыVBAC MCQsHanaОценок пока нет
- An Introduction To Volunteering at Camphill DevonДокумент3 страницыAn Introduction To Volunteering at Camphill DevonjohnyОценок пока нет
- From Outrage To Courage: The Unjust and Unhealthy Situation of Women in Poorer Countries and What They Are Doing About It PDFДокумент97 страницFrom Outrage To Courage: The Unjust and Unhealthy Situation of Women in Poorer Countries and What They Are Doing About It PDFNadine Avila100% (2)
- Hallie Berger Resume 11-2Документ2 страницыHallie Berger Resume 11-2api-281008760Оценок пока нет
- Dermatology NotesДокумент59 страницDermatology NotesAbdullah Matar Badran50% (2)
- Control of Pandemic Infectious Disease Procedure - Landkap - Gitt 00Документ25 страницControl of Pandemic Infectious Disease Procedure - Landkap - Gitt 00ahar85Оценок пока нет
- Growth and DevelopmentДокумент64 страницыGrowth and DevelopmentRahul Dhaker100% (1)
- Mekong TMBO 02 Maret 2021Документ14 страницMekong TMBO 02 Maret 2021Yolanda RahayuОценок пока нет
- Lecture 32 - Nutritional DisordersДокумент43 страницыLecture 32 - Nutritional Disordersapi-3703352100% (3)
- Scenihr o 046Документ116 страницScenihr o 046Ana NicoletaОценок пока нет
- 1 PPT Bioethics Lecture N1Документ44 страницы1 PPT Bioethics Lecture N1h.a.r.ade.v.ierОценок пока нет
- Clinical Manual of OtolaryngologyДокумент49 страницClinical Manual of Otolaryngologygamecockusc1992100% (3)
- Cacophony BurnTheGroundДокумент32 страницыCacophony BurnTheGroundLeo HurtadoОценок пока нет
- Deeper Trial - Asco 2021Документ26 страницDeeper Trial - Asco 2021Vuong Dinh Thy HaoОценок пока нет
- Kjadjk BkjbasjdДокумент23 страницыKjadjk BkjbasjdzaenalОценок пока нет
- Autism Spectre DisorderДокумент13 страницAutism Spectre DisorderJesus Hurtado100% (2)
- Yoga Poses For Acid RefluxДокумент6 страницYoga Poses For Acid RefluxKirit JhaОценок пока нет
- Fever of Unknown OriginДокумент26 страницFever of Unknown OriginFiona Yona Sitali100% (1)
- Nursing Care Plan Pott's DiseaseДокумент2 страницыNursing Care Plan Pott's Diseasederic95% (21)
- Home Quarantine Compliance 2022 1Документ1 страницаHome Quarantine Compliance 2022 1Puting KahoyОценок пока нет
- Documents 34-51Документ3 страницыDocuments 34-51api-575141270Оценок пока нет
- Neurology & Pupils (No 467)Документ231 страницаNeurology & Pupils (No 467)Mohamed GaberОценок пока нет
- Cerebral PalsyДокумент21 страницаCerebral PalsyEMily AbastaОценок пока нет
- Dark Souls 5eДокумент17 страницDark Souls 5ebite_clown_437074191Оценок пока нет
- Zybio Company Profile 20211109CДокумент46 страницZybio Company Profile 20211109CĐức Hòa100% (1)
- Wvgrd5c40vivpeavmmpsf3cvДокумент4 страницыWvgrd5c40vivpeavmmpsf3cvVishav Jindal100% (1)
- Inventarisasi Dan Identifikasi Hama Dan Penyakit Utama Tanaman Jagung (Zea Mays L.), Yustina M. S. W. Pu'u, Sri WahyuniДокумент11 страницInventarisasi Dan Identifikasi Hama Dan Penyakit Utama Tanaman Jagung (Zea Mays L.), Yustina M. S. W. Pu'u, Sri WahyuniJefri DwiОценок пока нет
- AllRefer Health - PerichondritisДокумент2 страницыAllRefer Health - PerichondritisandosaputraОценок пока нет