Академический Документы
Профессиональный Документы
Культура Документы
Airway Stenosis Resection and LTP DChhetri 11-19-08
Загружено:
Sudeep MishraИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Airway Stenosis Resection and LTP DChhetri 11-19-08
Загружено:
Sudeep MishraАвторское право:
Доступные форматы
Etiology
External trauma (MVA, surf board, assault, etc.) Internal trauma (Endotracheal intubation,
tracheostomy) Other
Systemic diseases (vasculitis, etc.) Chemo/XRT Idiopathic
Trans-nasal Esophagoscope Expanded diagnostic endoscopy
Laryngoscopy Bronchoscopy Esophagoscopy
2.0 mm Working Channel
Biopsies Injections Procedures
TEP
Tracheal Anatomy
10-12 cm in length (adult) 13-16 mm width (females) and 16-20 mm width
(males) 16-20 horseshoe shaped cartilage Membranous:cartilaginous trachea::1:4.5
Blood supply
Cervical trachea
supplied by superior and inferior thyroid arteries Mediastinal trachea supplied by bronchial arteries Extensive dissection around trachea causes ischemia
2-3 cm (4-6 rings) may be resected and reanastomosed primarily Tracheal resection maneuvers allow resection of more rings
Suprahyoid release Infrahyoid release Intrathoracic tracheal mobilization
Suprahyoid release (Montgomery)
Muscle attachments to the superior aspect of
hyoid bone are severed and central hyoid cut Larynx and cervical trachea allowed to drop inferiorly Can give up to 2-3 cm in length Significant post-op dysphagia a possible major complication compared to infrahyoid release
Infrahyoid release (Dedo)
Inferior attachments to the hyoid are severed Especially the thyrohyoid muscle and thyrohyoid
membrane Can add up to 2.5 cm length
Grillo 1964 (Intrathoracic maneuvers)
Division of pulmonary ligament 3 cm (5.9 rings) Division of mainstem bronchus 2.7 cm (5.5
rings) Pericardial dissection 0.9 cm (1.6 rings)
Up to 6.4 cm trachea (about 13 rings) can be excised with the help of release maneuvers
Pearson
PRE-CTR
POST-CTR
Common scenarios
2-level stenosis (glottic + subglottic, subglottic +
tracheal, stenosis + tracheostomy tube) Typically involvement of the stenosis is 3 cm or more What are the options?
Reconstruct without removal of scar Reconstruct with removal of scar
Endoscopic
Laser Dilation Steroid injection, Mitomycin-C application
Open Surgical
Primary resection and anastomosis Laryngotracheoplasty (LTP) Grafts (cartilage, mucosa) Stenting Single stage versus multistage
Staged Laryngotracheoplasty
Resect scar and make an open trough Line scar with mucosa (buccal) Close trough in 2-3 weeks Place T-tube stent
LTP Stage 3 Without T-Tube
LTP Stage 3 With T-tube
Remove stent in 6- months Replace with trach tube If no recurrence of stenosis then decannulate 2-3 weeks later
Staged Expansion Laryngotracheoplasty
Stage I (laryngotracheofissure, resection of
stricture endoluminally, application of buccal mucosal graft, placement of prosthetic endoluminal bolster, open upper airway trough) Stage II (placement of lateral marlex mesh) Stage III (closure of anterior neotracheal wall incorporating mesh, advancement skin flaps)
Marlex Mesh
Trough
Purpose of stents
Stabilize the larynx or trachea after surgery to
prevent collapse of the lumen Counteract or prevent recurrent scar formation
Stent Trivia
The word stent is derived from Charles B. Stent, a
British dentist who practiced in the late 19th century
Laryngeal
Aboulker stents, silicone stents, Montgomery
laryngeal stents, endotracheal tubes, and laryngeal keels
SILICONE TRACHEAL STENT
METALLIC TRACHEAL STENT
Long-term tolerability Easily removable. Poor mucocilary clearance Can migrate
Incorporates into mucosa Difficult to remove Better mucociliary clearance More reaction and granulation tissue
Fig. 2. Technique to customize the T-tube by marking the suction corresponding to the level of the tracheostomy, stenosis, and true vocal cords.
Fig. 3. Grasping the silk suture through the laryngoscope to position it across the stenosis.
Fig. 5. Proper placement of the T-tube through the stoma, across the stenosis. The looped suture is then cut and removed.
Curved hemostats Know which limb is shorter
Take this side out first
Grasp as low as possible Pull it out like a banana
Principles
Subglottic/tracheal stenosis No trach, not-intubatable LMA Endoscopic Balloon Dilation with CRE catheter system CTR vs. staged LTP if serial dilations not sufficient or desired Or CTR vs LTP, trach through stenosis under visualization
Principles Subglottic lesion, tracheostomy present Assess location of tracheotomy and distance from stenosis Then perform CTR versus staged LTP Need repeated procedures
Principles
Tracheal Stenosis soft web Do LMA (allows one to visualize stenosis
endoscopically), balloon dilation
If severe, Do LMA, then trach, then assess lesion
If severe tracheal lesion then do trach through
stenosis
Primary resection with anastomosis Tracheoplasty (staged)
For severe stenosis best to perform awake trach,
then as above
Вам также может понравиться
- Test BatteryДокумент8 страницTest BatterySudeep MishraОценок пока нет
- Critical Analysis of ThyroidДокумент10 страницCritical Analysis of ThyroidSudeep MishraОценок пока нет
- Critical Analysis of ThyroidДокумент10 страницCritical Analysis of ThyroidSudeep MishraОценок пока нет
- 25-3-12 Psychiatric MGT of H & N Cancer PatientsДокумент15 страниц25-3-12 Psychiatric MGT of H & N Cancer PatientsSudeep MishraОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Journal Homepage: - : IntroductionДокумент3 страницыJournal Homepage: - : IntroductionIJAR JOURNALОценок пока нет
- Jha For Painting of EquipmentДокумент1 страницаJha For Painting of EquipmentShahid RazaОценок пока нет
- Being A Medical DoctorДокумент14 страницBeing A Medical DoctorMichael Bill GihonОценок пока нет
- ASP ProductsДокумент33 страницыASP ProductsSerghei Barba100% (1)
- GENETIC DISORDERS AND CYTOGENETICSДокумент7 страницGENETIC DISORDERS AND CYTOGENETICSsmilechance8Оценок пока нет
- Google CardboardДокумент3 страницыGoogle CardboardMartínJiménezОценок пока нет
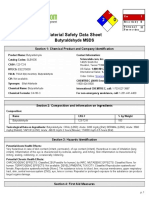
- MsdsДокумент6 страницMsdsJackyОценок пока нет
- 2020 DWTC Event Calendar EnglishДокумент4 страницы2020 DWTC Event Calendar EnglishMustazhar0% (1)
- Family Nursing Care PlanДокумент1 страницаFamily Nursing Care PlanDersly LaneОценок пока нет
- Annotated Bibliography Final DraftДокумент3 страницыAnnotated Bibliography Final Draftcchurc13Оценок пока нет
- Thesis-Android-Based Health-Care Management System: July 2016Документ66 страницThesis-Android-Based Health-Care Management System: July 2016Noor Md GolamОценок пока нет
- Posters Whofic 2020Документ107 страницPosters Whofic 2020Kristel HurtadoОценок пока нет
- Mindvalley - Superbrain Quest - SummaryДокумент17 страницMindvalley - Superbrain Quest - SummaryMagdy El ID100% (3)
- Lester Desjarlais Inquest Parts I and IIДокумент108 страницLester Desjarlais Inquest Parts I and IIJames Turner100% (1)
- Birth Injuries: Causes, Types and TreatmentДокумент9 страницBirth Injuries: Causes, Types and TreatmentshailaОценок пока нет
- MANAGEMENT AND PREVENTIONДокумент6 страницMANAGEMENT AND PREVENTIONIrina BalutaОценок пока нет
- Psychological Impact of COVID-19 Pandemic in The Philippines PDFДокумент13 страницPsychological Impact of COVID-19 Pandemic in The Philippines PDFAndrea KamilleОценок пока нет
- Hvis Msds PDFДокумент6 страницHvis Msds PDFsesbasar sitohangОценок пока нет
- College of Medicine & Health SciencesДокумент56 страницCollege of Medicine & Health SciencesMebratu DemessОценок пока нет
- Success Manual and Cheat Sheet Notes To Pass Your Basic Life Support (BLS) CourseДокумент11 страницSuccess Manual and Cheat Sheet Notes To Pass Your Basic Life Support (BLS) CourseanthonyОценок пока нет
- AgraLi The Low Chloride Liquid Fertilizer For Sensitive Crops enДокумент2 страницыAgraLi The Low Chloride Liquid Fertilizer For Sensitive Crops enASHОценок пока нет
- UNIT-I (A) - Hospital and It's OrganizationДокумент25 страницUNIT-I (A) - Hospital and It's Organizationrajeshwari ninaweОценок пока нет
- Reviews of Two Works by Dr. Amy Baker.Документ9 страницReviews of Two Works by Dr. Amy Baker.Talia SchwartzОценок пока нет
- PORNOGRAPHICДокумент13 страницPORNOGRAPHICcarlos ortizОценок пока нет
- Effectiveness of exercise therapy and infrared therapy for shoulder dislocationДокумент11 страницEffectiveness of exercise therapy and infrared therapy for shoulder dislocationhobi kitaОценок пока нет
- Ethics in Practice - at End of Life - Part 1Документ20 страницEthics in Practice - at End of Life - Part 1anushavergheseОценок пока нет
- Do Your Genes Make You A CriminalДокумент39 страницDo Your Genes Make You A CriminalParisha SinghОценок пока нет
- Cancer Bathinda's Dubious DistinctionДокумент2 страницыCancer Bathinda's Dubious DistinctionPardeepSinghОценок пока нет
- Congenital LaryngomalaciaДокумент8 страницCongenital LaryngomalaciaRettha SigiroОценок пока нет
- Carlin Smith Child Abuse FinalДокумент12 страницCarlin Smith Child Abuse FinalCarlin SmithОценок пока нет