Академический Документы
Профессиональный Документы
Культура Документы
Infectious Skin Diseases
Загружено:
ማላያላም ማላያላምАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Infectious Skin Diseases
Загружено:
ማላያላም ማላያላምАвторское право:
Доступные форматы
INFECTIOUS SKIN DISEASES
Walid Nabil Fouad HamdAllah Mohamed MICROBIOLOGY DEPARTMENT MEDICAL RESEARCH INSTITUTE
Humans are natural hosts for many bacterial species that colonize the skin as normal flora. Staphylococcus aureus and Streptococcus pyogenes are infrequent resident flora, but they account for a wide variety of bacterial pyodermas (pus in skin infections). Predisposing factors to infection include minor trauma, preexisting skin disease, poor hygiene, and, rarely, impaired host immunity.
List of some bacterial skin infections:
1. 2. 3.
4.
5. 6. 7.
Impetigo Folliculitis, Furunculosis, and Carbunculosis Erythrasma Ecthyma Erysipelas Cellulitis Necrotizing Fasciitis
1. Impetigo
Impetigo is a common superficial skin infection usually caused by S. aureus and occasionally by S. pyogenes. Mixed infections caused by both bacteria are common and result when a primary infection is invaded by the other bacteria. Infection is highly contagious and usually treated with a topical antibiotic. Two clinical types of impetigo exist: nonbullous and bullous. Both types have a distinct appearance and cause: The nonbullous type is more common (70% of impetigo infections), and typically occurs on the face and extremities, initially with vesicles or pustules on reddened skin. The vesicles or pustules eventually rupture to leave the characteristic honeycolored (yellow-brown) crust. Bullous impetigo, almost exclusively caused by S. aureus, exhibits flaccid bullae with clear yellow fluid that rupture and leave a golden-yellow crust.
Nonbullous impetigo (S. aureus)
Bullous impetigo (S. aureus)
2. Folliculitis, Furunculosis, and Carbunculosis
Folliculitis is another very common bacterial skin infection caused by S. aureus. It is an infection in the hair follicle, which is a pretty small structure. It makes sense that this infection looks like a group of small little red bumps that can be filled with a small amount of pus. Folliculitis usually heals without scarring. Hot tub folliculitis is an infection of the hair follicles caused by the bacteria Pseudomonas aeruginosa. This bacterium is commonly found in contaminated whirlpools, hot tubs, water slides, physiotherapy pools, or even loofah sponges. Children tend to get hot tub folliculitis more often (probably because they stay in the water longer). A furuncle is an infection of the pilosebaceous unit, therefore is more extensive than a folliculitis because the infection also involves the sebaceous gland. A furuncle frequently occurs on the neck, face, armpits, and buttocks. It begins as a small, tender, red nodule that becomes painful and fluctuant. Frequently, pus will spontaneously drain, and often the furuncle will resolve on its own. A carbuncle can simply be defined as a multiple furuncles grouped together. A carbuncle usually involves the deeper layers of the skin - the subcutaneous fat. It looks like a large, red nodule that is hot and may have visible layers of pus just beneath the surface of the skin.
Folliculitis
Hot tub folliculitis
Furuncle
Carbuncle
3. Erythrasma
Erythrasma is a bacterial skin infection caused by the gram-positive bacterium Corynebacterium minutissimum. It occurs most often between the third and fourth toes, but it can also frequently be found in the groin, armpits, and under the breasts. Because of its color and location, it's often confused with a fungal infection like jock itch. Erythrasma starts as a pink to red patch with well-defined edges. This patch has a finely wrinkled appearance with a very fine scale on it. After some time, the rash fades from pink to a uniform brown color. This consistent brown color with the fine scale distinguishes it from jock itch or other fungal infections which are typically redder around the edges with thicker scaling on the edges.
Erythrasma is more common in the following populations: Overweight people, Elderly, Diabetics, People in warm, moist climates.
Erythrasma
4. Ecthyma
Ecthyma is a deep infection of the skin that resembles impetigo. S. aureus or S. pyogenes is the usual pathogen of ecthyma. The most common site of infection is the legs. Infection is characterized by thickly crusted erosions or ulcerations, which begins with vesicles and bullae. Untreated staphylococcal or streptococcal impetigo can extend more deeply, penetrating the dermis, producing a shallow crusted ulcer.
Ecthyma
5. Erysipelas
Erysipelas is a superficial infection of the skin, which typically involves the dermal lymphatic system. Erysipelas is also known as St. Anthony's fire, an accurate description of the intensity of this rash. Erysipelas is most often caused by the Group A -hemolytic Streptococcus. In a few cases, it can be caused by other types of Streptococcus or Staphylococcus bacteria. Erysipelas was previously found mainly on the face. However, now it is seen most commonly on the lower extremities. Erysipelas tends to occur in areas where the lymphatic system is obstructed. A cluster of symptoms typically precede the appearance of the rash by 4 to 48 hours. These symptoms include fever, chills, fatigue, anorexia, and vomiting. The rash then quickly appears as a bright red, hot, swollen, shiny patch that has clearly defined borders.
Erysipelas
6. Cellulitis
Cellulitis is a bacterial infection of the deeper layers of the skin, the dermis and the subcutaneous tissue. In adults and children, cellulitis is most often caused by Streptococcus and S. aureus bacteria. Sometimes Haemophilus influenzae type B can cause cellulitis in children younger than 3, but this has become less common since we've been vaccinating against this bacteria. Children often get cellulitis on the head and neck, and adults often get cellulitis on the arms or legs. Before skin changes occur, someone with cellulitis can have fever, chills, and fatigue.
The typical skin infection of cellulitis is usually erythematous (red), edematous (swollen), tender, warm to touch, and painful plaque that expands rapidly. It's often difficult to tell exactly where the border is between normal and infected skin (ill-defined borders). Red streaks coming out of the area and swollen lymph nodes can sometimes occur.
Left untreated, cellulitic skin can become bullous and necrotic, and an abscess or fasciitis, or both, can occur.
Cellulitis
7. Necrotizing Fasciitis
Necrotizing fasciitis is a rare infection of the subcutaneous tissues and fascia that eventually leads to necrosis. Predisposing factors include injuries to soft tissues, such as abdominal surgery, abrasions, surgical incisions, diabetes, alcoholism, cirrhosis, and intravenous drug abuse. S. pyogenes can be the sole pathogen responsible for necrotizing fasciitis, but most patients have a mixed infection with other aerobes (groups B and C streptococci, MRSA) and anaerobes (Clostridium spp). Infection begins with warm, tender, reddened skin and inflammation that rapidly extends horizontally and vertically. Necrotizing fasciitis commonly occurs on the extremities, abdomen, or perineum or at operative wounds.
Within 48 to 72 hours, affected skin becomes dusky, and bullae form, followed by necrosis and gangrene, often with crepitus. Without prompt treatment, fever, systemic toxicity, organ failure, and shock can occur, often followed by death.
Necrotizing fasciitis
Fungal skin infections are caused by microscopic fungus that proliferate due to ideal conditions . Fungal skin infections in humans occur on nails, skin and hair, as it sustains itself on protein keratin which is abundantly found in these areas.
Although several species of fungi are potentially pathogenic in humans, Candida (esp. Candida albicans) is the organism responsible for most fungal infections. Candida, which is normally present within the human body, is usually harmless. However, it can cause symptoms when a weakened immune system or other factors allow it to grow unabated.
Increased use of antibiotics and immunosuppressive drugs such as corticosteroids are major factors contributing to higher frequency of fungal infections. Antibiotics and immunosuppressive drugs, by disrupting normal bacterial colonization and suppressing the immune system, create an environment within the body in which fungi can thrive
1. Dermatophytosis
Dermatophytosis or ringworm infection is an infection of keratinized tissue (skin, hair, and claws) by one of the 3 genera of fungi collectively called dermatophytes Epidermophyton, Microsporum, and Trichophyton. Fungal reservoirs for these organisms include soil, animals, and infected humans. Dermatophytes feed on keratin, the material found in the outer layer of skin, hair, and nails. These fungi thrive on skin that is warm and moist, but may also survive directly on the outsides of hair shafts or in their interiors. Dermatophytosis is common in most adult people, with up to 20 percent of the population having one of these infections at any given moment. It is especially common among people who play sports, wrestling in particular. Different types of dermatophytosis include:
Tinea pedis (athlete's foot) affects the feet Tinea unguium affects the fingernails and toenails Tinea corporis affects the arms, legs, and trunk
Different types of dermatophytosis include (cont.):
Tinea cruris (jock itch) affects the groin area Tinea manuum affects the hands and palm area Tinea capitis affects the scalp Tinea barbae affects facial hair Tinea faciei (face fungus) affects the face
Tinea pedis
Tinea cruris Tinea unguium Tinea corporis Tinea capitis
2. Candidiasis
Candidiasis refers to a diverse group of infections caused by Candida albicans or by other members of the genus Candida. These organisms typically infect the skin, nails, mucous membranes, and gastrointestinal tract, but they also cause systemic disease. Infection is common in immunocompromised patients, diabetics, the elderly, and patients receiving antibiotics. Candida albicans accounts for 70% to 80% of all candidal infections. C. albicans commonly resides on skin and mucosal surfaces. Alterations in the host environment can lead to its proliferation and subsequent skin disease. List of some of the most common types of skin candidiasis:
Candidal intertrigo: A specific infection of the skin folds (axillae, groin), characterized by reddened plaques, often with satellite pustules. Thrush: An oropharyngeal candidiasis, characterized by white nonadherent plaques on the tongue and buccal mucosa.
List of some of the most common types of skin candidiasis (cont.):
Paronychia: An acute or chronic infection of the nail characterized by tender, edematous, and erythematous nail folds, often with purulent discharge (this disease is common in diabetics). Candidal vulvovaginitis: An acute inflammation of the perineum characterized by itchy, reddish, scaly skin and mucosa; creamy discharge; and peripheral pustules. (The counterpart in men is balanitis, characterized by shiny reddish plaques on the glans penis, which can affect the scrotum).
Candidal intertrigo
Paronychia Thrush
Candidal vulvovaginitis
3. Tinea versicolor
Tinea versicolor is a common opportunistic superficial infection of the skin caused by the ubiquitous yeast Malassezia furfur. Prevalence is high in hot, humid climates. Purported risk factors include oral contraceptive use, heredity, systemic corticosteroid use, Cushing's disease, immunosuppression, and malnutrition. M. furfur may filter the rays of the sun and also produces phenolic compounds that inhibit tyrosinase, which can produce hypopigmentation in many patients. Infection produces discrete and confluent, fine scaly, well-demarcated, hypopigmented or hyperpigmented plaques on the chest, back, arms, and neck. Pruritus is mild or absent.
Tinea versicolor
Viral skin infections typically cause a skin rash, sore or lesion. And these skin problems may be accompanied by other symptoms if the skin infecting virus is capable and able to spread to other parts of your body.
Viral skin infections tend to be more aggressive if your immunity is impaired, especially a problem with lymphocyte production. An example is increased incidence of skin rashes, sores and lesions in those suffering from HIV because of a weakened immune system. Three principal virus types cause the majority of viral skin infections rash, sore and lesion problems, they are: poxvirus, herpes simplex virus and human papillomavirus. There are many different types of viral skin infections, ranging from common to rare and mild to severe. Several of the commonly known viral infections that may cause rashes, sores, lesions or other skin problems are: cold sores, genital herpes, chickenpox, shingles, warts, and molluscum contagiosum.
1. Herpes Simplex
Herpes simplex virus (HSV) infection is a painful, self-limited, often recurrent dermatitis, characterized by small grouped vesicles on an erythematous base. Disease is often mucocutaneous. Infection with the herpes virus is categorized into 2 distinct disorders based on the site of infection: Oral herpes, the visible symptoms of which are colloquially called cold sores or fever blisters, is an infection of the face or mouth caused by HSV type 1. Genital herpes, known simply as herpes, is the second most common form of herpes caused by HSV type 2.
Disease follows implantation of the virus via direct contact at mucosal surfaces or on sites of abraded skin. After primary infection, the virus travels to the adjacent dorsal ganglia, where it remains dormant unless it is reactivated by psychological or physical stress, illness, trauma, menses, or sunlight.
Oral Herpes (HSV-1)
Genital Herpes (HSV-2)
2. Chickenpox
Chickenpox is a highly contagious disease caused by primary infection with the varicellazoster virus, a member of the herpesvirus family. The same virus also causes herpes zoster shingles in adults. Chickenpox usually starts with vesicular skin rash mainly on the body and head rather than at the periphery and becomes itchy, raw pockmarks, which mostly heal without scarring. Most cases of chickenpox occur in children younger than 10. The disease is usually mild, although serious complications sometimes occur. Most children with chickenpox have the following symptoms before the rash appears: Fever, Headache, and Stomach ache. The chickenpox rash occurs about 10 to 21 days after coming into contact with someone who had the disease. The average child develops 250 to 500 small, itchy, fluid-filled blisters over red spots on the skin.
Chickenpox
3. Herpes Zoster
Herpes zoster (shingles) is an acute, painful dermatitis that affects approximately 10% to 20% of adults, often in the presence of immunosuppression. It is caused by the varicella zoster virus (VZV), and characterized by a painful skin rash with blisters in a limited area on one side of the body, often in a stripe. The initial infection with VZV causes the acute (short-lived) illness chickenpox which generally occurs in children and young people. Once an episode of chickenpox has resolved, the virus is not eliminated from the body but can go on to cause shinglesan illness with very different symptomsoften many years after the initial infection. During the course of varicella, the virus travels from the skin and mucosal surfaces to the sensory ganglia, where it lies dormant for a patient's lifetime. Reactivation often follows immunosuppression, emotional stress, trauma, and irradiation or surgical manipulation of the spine, producing a dermatomal dermatitis.
Herpes Zoster (Shingles)
4. Warts
Warts are common and benign epithelial growths caused by human papillomavirus (HPV). Warts affect approximately 10% of the population. Anogenital warts are a sexually transmitted infection, and partners can transfer the virus with high efficiency. Immunosuppressed patients are at increased risk for developing persistent HPV infection. HPV infection follows inoculation of the virus into the epidermis through direct contact, usually facilitated by a break in the skin. After inoculation, a wart usually appears within 2 to 9 months. The rough surface of a wart can disrupt adjacent skin and enable inoculation of virus into adjacent sites, leading to the development and spread of new warts. The common wart is the most common type: It is a hyperkeratotic, flesh-colored papule or plaque studded with small black dots (thrombosed capillaries). Other types of warts include flat warts (verruca plana), plantar warts, and condyloma acuminatum (venereal warts).
Plantar Warts
Common Warts
Flat Warts
Venereal Warts
5. Molluscum Contagiosum
Molluscum contagiosum is a viral skin infection that causes raised, pearl-like papules or nodules on the skin. It is caused by a DNA poxvirus called the molluscum contagiosum virus (MCV), a member of the poxvirus family. The disease is a common infection in children and occurs when a child comes into direct contact with a lesion. It is frequently seen on the face, neck, armpit, arms, and hands but may occur anywhere on the body except the palms and soles. The virus can spread through contact with contaminated objects, such as towels, clothing, or toys.
Molluscum Contagiosum
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Simple Shingles CureДокумент26 страницSimple Shingles CureSpencer Shupe0% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Rife Frequencies by NumberДокумент90 страницRife Frequencies by Numbernepretip100% (5)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- 35 Facts and Reasons Why I Became An Avid Ex-Vaxxer and No Longer Vaccinate PDFДокумент39 страниц35 Facts and Reasons Why I Became An Avid Ex-Vaxxer and No Longer Vaccinate PDFmvrosuОценок пока нет
- ImmunologyДокумент8 страницImmunologyማላያላም ማላያላም89% (9)
- Immuno Histo ChemistryДокумент26 страницImmuno Histo Chemistryማላያላም ማላያላም100% (3)
- All Pediatric Seminars - AsemДокумент356 страницAll Pediatric Seminars - AsemAsem Shadid100% (1)
- Care of Older Adults: Health Promotion, Maintenance, and Home ConsiderationsДокумент15 страницCare of Older Adults: Health Promotion, Maintenance, and Home ConsiderationsKirsten ChavezОценок пока нет
- Viral Latency: Walid Nabil FouadДокумент49 страницViral Latency: Walid Nabil Fouadማላያላም ማላያላምОценок пока нет
- Oral Pathology ModuleДокумент31 страницаOral Pathology ModuleDenee Vem MatorresОценок пока нет
- Pathogenesis of Fungal InfectionsДокумент70 страницPathogenesis of Fungal Infectionsማላያላም ማላያላም100% (15)
- Dermatophytes - Medical Research Institute - Alexandria UniversityДокумент129 страницDermatophytes - Medical Research Institute - Alexandria Universityማላያላም ማላያላምОценок пока нет
- Laboratory Diagnosis of Smallpox VirusДокумент25 страницLaboratory Diagnosis of Smallpox Virusማላያላም ማላያላምОценок пока нет
- MCQs InfectionsДокумент6 страницMCQs InfectionsNaeem NawazОценок пока нет
- 144 Diagnosa FKTPДокумент5 страниц144 Diagnosa FKTPpuskesmas100% (1)
- AspergillusДокумент53 страницыAspergillusማላያላም ማላያላም100% (1)
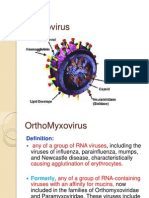
- OrthomyxovirusesДокумент39 страницOrthomyxovirusesማላያላም ማላያላምОценок пока нет
- HematocritДокумент2 страницыHematocritማላያላም ማላያላምОценок пока нет
- Diagnosis of Fungemia in Immunosuppressed Patients Using Blood Culture TechniquesДокумент25 страницDiagnosis of Fungemia in Immunosuppressed Patients Using Blood Culture Techniquesማላያላም ማላያላምОценок пока нет
- Role of Chlamydia Pneumoniae in The Pathogenesis of Asthma Airway RemodelingДокумент27 страницRole of Chlamydia Pneumoniae in The Pathogenesis of Asthma Airway Remodelingማላያላም ማላያላምОценок пока нет
- Molecular Diagnosis of HMPVДокумент21 страницаMolecular Diagnosis of HMPVማላያላም ማላያላምОценок пока нет
- Ax SYMДокумент3 страницыAx SYMማላያላም ማላያላምОценок пока нет
- Occurrence of Infections in LaboratoriesДокумент53 страницыOccurrence of Infections in Laboratoriesማላያላም ማላያላምОценок пока нет
- Aspergillus (Summary)Документ2 страницыAspergillus (Summary)ማላያላም ማላያላምОценок пока нет
- PicornavirusesДокумент144 страницыPicornavirusesማላያላም ማላያላምОценок пока нет
- Some Fungal PathogensДокумент31 страницаSome Fungal Pathogensማላያላም ማላያላምОценок пока нет
- Filamentous Fungi and YeastДокумент26 страницFilamentous Fungi and Yeastማላያላም ማላያላምОценок пока нет
- Bio-Safety and Infection Control - Questions and AnswersДокумент8 страницBio-Safety and Infection Control - Questions and Answersማላያላም ማላያላምОценок пока нет
- Anti FungalsДокумент44 страницыAnti Fungalsማላያላም ማላያላምОценок пока нет
- Food Poisoning Caused by BacteriaДокумент2 страницыFood Poisoning Caused by Bacteriaማላያላም ማላያላምОценок пока нет
- CryptococcusДокумент57 страницCryptococcusማላያላም ማላያላምОценок пока нет
- Antigens and ImmunogensДокумент41 страницаAntigens and Immunogensማላያላም ማላያላምОценок пока нет
- Candida IdentificationДокумент17 страницCandida Identificationማላያላም ማላያላምОценок пока нет
- DermatophytesДокумент42 страницыDermatophytesማላያላም ማላያላም100% (1)
- ArbovirusesДокумент4 страницыArbovirusesማላያላም ማላያላምОценок пока нет
- Anti-Fungal MedicationsДокумент25 страницAnti-Fungal Medicationsማላያላም ማላያላምОценок пока нет
- Bcl-2 Family ProteinsДокумент25 страницBcl-2 Family Proteinsማላያላም ማላያላም100% (1)
- Cell InjuryДокумент29 страницCell Injuryማላያላም ማላያላምОценок пока нет
- Important Vaccines for SeniorsДокумент13 страницImportant Vaccines for SeniorsNazly VargasОценок пока нет
- Biology Investigatory ProjectДокумент14 страницBiology Investigatory Projectdesaipiyush1234Оценок пока нет
- Benefits and Contributions Schedule 2021Документ72 страницыBenefits and Contributions Schedule 2021MarcoОценок пока нет
- ArthritisДокумент69 страницArthritisKavya sriОценок пока нет
- 01 Pediatrics in Review - Jan2008Документ51 страница01 Pediatrics in Review - Jan2008Alejandra Cienfuegos LopezОценок пока нет
- Nejm Herpes ZosterДокумент7 страницNejm Herpes ZosterAlexander TegarОценок пока нет
- Test Bank For Oral Pathology 7th Edition by RegeziДокумент11 страницTest Bank For Oral Pathology 7th Edition by RegeziSteve Isola100% (23)
- Herpesvirus Infections in ChildrenДокумент23 страницыHerpesvirus Infections in ChildrenShafiq NezatОценок пока нет
- Undergraduate Pathology NotesДокумент77 страницUndergraduate Pathology Notesraul sinatoОценок пока нет
- Ramsay Hunt SyndromeДокумент3 страницыRamsay Hunt SyndromeAnish RajОценок пока нет
- Engleza Sinonime An 2Документ18 страницEngleza Sinonime An 2Andrei RadulescuОценок пока нет
- MG II S3-The Hospital-Medical VocabularyДокумент4 страницыMG II S3-The Hospital-Medical VocabularyIuliana RaduОценок пока нет
- Lec 8 Ulcerative Vesicular & Bullous LesionsДокумент6 страницLec 8 Ulcerative Vesicular & Bullous LesionsAbd 9961Оценок пока нет
- Slide 7 - Patient - Nursing Care Plan (NCP)Документ27 страницSlide 7 - Patient - Nursing Care Plan (NCP)Gilang Cahyo Kumolo100% (2)
- Herpes HSV & HZVДокумент11 страницHerpes HSV & HZVLal RuattlingaОценок пока нет
- Antiretroviral Therapy Guidelines For HIV-Infected Adults and AdolescentsДокумент122 страницыAntiretroviral Therapy Guidelines For HIV-Infected Adults and AdolescentsManoj Kumar MeenaОценок пока нет
- How to look 「皮疹」Документ50 страницHow to look 「皮疹」Satoshi KobayashiОценок пока нет
- Jurnal Case Control UTS (Idrus) 5Документ8 страницJurnal Case Control UTS (Idrus) 5Reny NapitupuluОценок пока нет
- Neonatal InfectionДокумент9 страницNeonatal InfectionnishaОценок пока нет
- Varicella Zoster Virus: Two Lives of A Pathogen: Clinical ReviewДокумент5 страницVaricella Zoster Virus: Two Lives of A Pathogen: Clinical ReviewVICKI ANDREANОценок пока нет
- Pertanyaan ReferatДокумент2 страницыPertanyaan ReferatBuydh BfdsfsОценок пока нет
- Ulcerative Vesicular Bullous Lesions 1Документ32 страницыUlcerative Vesicular Bullous Lesions 1Mustafa AliОценок пока нет