Академический Документы
Профессиональный Документы
Культура Документы
38 - Hypofibrinogenaemia
Загружено:
dr_asaleh0 оценок0% нашли этот документ полезным (0 голосов)
213 просмотров8 страницIn late pregnancy, there is increased concentration of coagulation factors I (fibrinogen: level is 350-650 mg / dL), VII,VIII,IX and X. Other plasma factors and platelet count (150 000-400 000 / cmm) do not change remarkably. Common causes Massive blood loss with inadequate replacement. Rare causes Sepsis. Retained dead fetus (for more than 3-4 weeks). Autoimmune disease, hematological malign
Исходное описание:
Оригинальное название
38- Hypofibrinogenaemia
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документIn late pregnancy, there is increased concentration of coagulation factors I (fibrinogen: level is 350-650 mg / dL), VII,VIII,IX and X. Other plasma factors and platelet count (150 000-400 000 / cmm) do not change remarkably. Common causes Massive blood loss with inadequate replacement. Rare causes Sepsis. Retained dead fetus (for more than 3-4 weeks). Autoimmune disease, hematological malign
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
213 просмотров8 страниц38 - Hypofibrinogenaemia
Загружено:
dr_asalehIn late pregnancy, there is increased concentration of coagulation factors I (fibrinogen: level is 350-650 mg / dL), VII,VIII,IX and X. Other plasma factors and platelet count (150 000-400 000 / cmm) do not change remarkably. Common causes Massive blood loss with inadequate replacement. Rare causes Sepsis. Retained dead fetus (for more than 3-4 weeks). Autoimmune disease, hematological malign
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 8
HYPOFIBRINOGENEMIA
Disseminated Intravascular Coagulation
(DIC) or Consumptive Coagulopathy.
HYPOFIBRINOGENEMIA
PHYSIOLOGICAL BACKGROUND
In late pregnancy, there is increased concentration of
coagulation factors I (fibrinogen: level is 350-650 mg/dL),
VII,VIII,IX and X. Other plasma factors and platelet count
(150 000-400 000/cmm) do not change remarkably.
DEFINITION
A widespread hematological condition characterized by
accelerated fibrin formation and lyses. There is
consumption of platelets and coagulation factors in
variable quantities.
Signs of hypofibrinogenaemia develop when its level goes
below 100 mg/dL
Etiology (Pregnancy related)
Common causes
Massive blood loss with inadequate replacement. Massive
crystalloid or colloid replacement
Placental abruption.
Severe pre-eclampsia/eclampsia or HELLP syndrome.
Rare causes
Sepsis.
Retained dead fetus (for more than 3-4 weeks).
Amniotic fluid embolism.
Acute fatty liver of pregnancy.
Adult RDS, acute hemolytic transfusion reactions,
autoimmune disease, hematological malignancies and solid
tumors.
MECHANISM
Pathologically accelerated coagulation: occurs via the extrinsic
pathway (thromboplastin from tissue destruction) or the intrinsic
pathway (collagen and other tissue components when endothelial
integrity is lost). Finally factor X (Prothrombinase) is activated. The
formed thrombin (activated factor II) changes fibrinogen (factor I) to
fibrin (monomers and polymers-clot-). Factor X can be activated
directly by proteases present in mucin of amniotic fluid or
neoplasms.
Fibrinolysis: the fibrin monomers combine with tissue
plasminogen activator and plasminogen which release plasmin.
Plasmin lyses the fibrin mono and polymers to form a series of
fibrin degradation products (FDPs) including the D-dimer.
CLINICAL PICTURE
Postpartum or antepartum hemorrhage.
Persistent bleeding from venipuncture sites or
after catheter insertion.
Spontaneous bleeding from gums and nose.
Generalized oozing in surgical fields.
Purpuric areas at pressure sites
(thrombocytopenia and incoagulable blood).
Investigations
Aiming to detect fibrinolysis.
FDPs and fibrin D-dimer (normally absent).
Prolonged PT and PTT(PTT may be normal).
Low fibrinogen, falling antithrombin III & low platelet
count (CBC should be done).
Weiner test (clot observation test): 5-10 cc of blood in a
test tube are incubated at 37ºC. A) Normally a clot forms
within 3-8 minutes. B) a clot forms after a longer time
and dissolves within one hour = hypofibrinogenemia. C)
No clot is formed = afibrinogenemia.
TREATMENT
It must be directed to the underlying cause to reverse
defibrination. Two wide-bore IV cannulas are inserted.
If PT is > 1.5 times the control value, transfuse fresh
frozen plasma (FFP). The goal is to keep PT within 2-3
sec. of the control value.
If fibrinogen level is < 100 mg/dL, transfuse
cryoprecipitate. Ten units of cryoprecipitate are usually
given after every 2 to 3 units of plasma. Each unit of
cryoprecipitate increases the fibrinogen by 10 mg/dL.
OR give Fibrinogen 4-10 g IV.
TREATMENT
Platelets should be transfused if the count is < 20 000/cmm or if
clinically significant bleeding occurs with a platelet count between
20 000 and 50 000/cmm. Each platelet unit increases count by
10,000/cmm. The usual rate of platelet transfusion is 1-3 U/ 10Kg/
day.
Antifibrinolytics as Epsilon Amino Caproic Acid (EACA) 4-6 g IV
OR trasylol 2-4 ampules IV ( 5 ml ampoule contains 25 000 U), is
not recommended in most types of obstetric coagulopathy to avoid
organ ischemia and infarction unless all above mentioned
measures fail to control bleeding.
Heparin infusion trying to stop coagulation is condemned when the
vascular system integrity is compromised.
Вам также может понравиться
- Disseminated Intravascular Coagulopathy: D.I.C Specific Learning ObjectivesДокумент15 страницDisseminated Intravascular Coagulopathy: D.I.C Specific Learning ObjectivesmartinОценок пока нет
- 15581coagulation Defects in ObstetricsДокумент33 страницы15581coagulation Defects in ObstetricsdindacОценок пока нет
- 25. Coagulation Disorders in PregnancyДокумент35 страниц25. Coagulation Disorders in PregnancyMuwanga faizoОценок пока нет
- Bleeding in A NeonateДокумент36 страницBleeding in A NeonateDrBibek AgarwalОценок пока нет
- AssignmentДокумент11 страницAssignmentrehamoh1997Оценок пока нет
- Path Hematology ReviewДокумент19 страницPath Hematology ReviewChristopher MuellerОценок пока нет
- Disseminated Intravascular CoagulationДокумент37 страницDisseminated Intravascular CoagulationhipoclaudioОценок пока нет
- Cogulation Profile: Bleeding Time, Clotting Time, PT, and PTTДокумент49 страницCogulation Profile: Bleeding Time, Clotting Time, PT, and PTTDorin PathakОценок пока нет
- Disseminated Intravascular CoagulationДокумент37 страницDisseminated Intravascular CoagulationMuhammad Adeeb100% (1)
- Disseminated Intravascular CoagualationДокумент47 страницDisseminated Intravascular CoagualationIshaBrijeshSharmaОценок пока нет
- A. 24 Hours Pre-Operatively B. 2 Hours Pre-Operatively C. Whilst Making The Skin IncisionДокумент75 страницA. 24 Hours Pre-Operatively B. 2 Hours Pre-Operatively C. Whilst Making The Skin Incision5alifa55Оценок пока нет
- Complex Process Terminates Blood Loss From The Intravascular SpaceДокумент25 страницComplex Process Terminates Blood Loss From The Intravascular SpaceDewi YukinohanaОценок пока нет
- Care of HemophiliaДокумент7 страницCare of HemophiliaBasant karn100% (4)
- Key Terms: Chapter 19: Coagulation DisordersДокумент16 страницKey Terms: Chapter 19: Coagulation DisordersDarryl Betts100% (1)
- Blood and Blood ComponentsДокумент51 страницаBlood and Blood ComponentsMinlun ChongloiОценок пока нет
- Disseminated Intravascular Coagulation (DIC)Документ24 страницыDisseminated Intravascular Coagulation (DIC)Atiya HajjajОценок пока нет
- Disseminated Intravascular Coagulopathy Disseminated Intravascular Coagulation (DIC) Is A PathologicalДокумент6 страницDisseminated Intravascular Coagulopathy Disseminated Intravascular Coagulation (DIC) Is A PathologicalValarmathiОценок пока нет
- Coagulation Disorders in ICUДокумент72 страницыCoagulation Disorders in ICUMadhusudan H C Gowda100% (1)
- Disseminated Intravascular CoagulationДокумент29 страницDisseminated Intravascular Coagulationvarun tmОценок пока нет
- Hemostasis 1Документ34 страницыHemostasis 1diyoba100% (1)
- Coagulation DisordersДокумент26 страницCoagulation DisordersLia pramitaОценок пока нет
- Approach To Bleeding Child: Moderator: Dr. Ayal (MD, Pediatrician) Presenters: Wubshet K. & Yihenew D. (C-I Students)Документ92 страницыApproach To Bleeding Child: Moderator: Dr. Ayal (MD, Pediatrician) Presenters: Wubshet K. & Yihenew D. (C-I Students)woldemariamОценок пока нет
- Disseminated Intravascular CoagulationДокумент22 страницыDisseminated Intravascular Coagulationanaeshkl100% (2)
- Treatment of DicДокумент11 страницTreatment of DicSarang LeeОценок пока нет
- Disseminated Intravascular CoagulationДокумент4 страницыDisseminated Intravascular CoagulationHendra SshОценок пока нет
- Blood Transfusion Guidelines for NICU BabiesДокумент8 страницBlood Transfusion Guidelines for NICU BabiesanuОценок пока нет
- 14-Coagulation DisorderДокумент51 страница14-Coagulation Disorderqjf7p2pstdОценок пока нет
- Coagulation DisordersДокумент26 страницCoagulation DisordersLia pramita0% (1)
- 401 Part 2 B - WДокумент23 страницы401 Part 2 B - WqweadwfawdawОценок пока нет
- Hellp Syndrome - Therapeutic ChallengeДокумент40 страницHellp Syndrome - Therapeutic Challengeysh_girlОценок пока нет
- CoA Dis - RevДокумент60 страницCoA Dis - RevAzra Al AmanahОценок пока нет
- HemophiliaДокумент62 страницыHemophiliamuhirwa Samuel100% (1)
- Coagulation Disorders in Obstetrics MD5Документ51 страницаCoagulation Disorders in Obstetrics MD5gloriashirima8Оценок пока нет
- Dic - MNJДокумент36 страницDic - MNJmaibejoseОценок пока нет
- Blood ProductsДокумент41 страницаBlood ProductsrijjorajooОценок пока нет
- Coagulation Disorders in ObsДокумент33 страницыCoagulation Disorders in Obsapule geraldhumbleОценок пока нет
- Blood Product Replacement For Postpartum HemorrhageДокумент7 страницBlood Product Replacement For Postpartum HemorrhageAlberto LiraОценок пока нет
- Group 9Документ21 страницаGroup 9Dyenadel M. OrataОценок пока нет
- Imuune Thrombocytopenia (Itp)Документ34 страницыImuune Thrombocytopenia (Itp)Roshandiep GillОценок пока нет
- Hemostasis, Clotting Disorder and AnticoagulantsДокумент87 страницHemostasis, Clotting Disorder and AnticoagulantsSomit Jain100% (1)
- Blood Dr. Devesh Palharya FBДокумент4 страницыBlood Dr. Devesh Palharya FBAkash MittalОценок пока нет
- Approach To The Adult With A Suspected Bleeding DisorderДокумент9 страницApproach To The Adult With A Suspected Bleeding DisorderMirasol AbogaОценок пока нет
- Fourth Stage HemostasisДокумент9 страницFourth Stage HemostasisAli MOОценок пока нет
- Disseminated Intravascular CoagulationДокумент27 страницDisseminated Intravascular CoagulationMouhammad DawoudОценок пока нет
- Lecture 4. Bleeding Disorders Part 2Документ35 страницLecture 4. Bleeding Disorders Part 2Kekelwa Mutumwenu SnrОценок пока нет
- Postpartum CollapseДокумент54 страницыPostpartum Collapsemedical chroniclesОценок пока нет
- G G G G G GДокумент16 страницG G G G G Gpreeti19987Оценок пока нет
- Disseminated Intravascular CoagulationДокумент2 страницыDisseminated Intravascular CoagulationVince100% (1)
- ITP LectureДокумент20 страницITP LectureReza MajidiОценок пока нет
- Bleeding DisorderДокумент56 страницBleeding DisorderPriya Singh100% (1)
- Managing the HELLP Syndrome Therapeutic ChallengeДокумент41 страницаManaging the HELLP Syndrome Therapeutic ChallengeDiena HarisahОценок пока нет
- NCMMCA2Документ12 страницNCMMCA2Romm JacobОценок пока нет
- Post Partum HaemorrhageДокумент6 страницPost Partum Haemorrhagenancy jeyakumarОценок пока нет
- HemophiliaДокумент60 страницHemophiliavibhurocksОценок пока нет
- Lecture 5Документ48 страницLecture 5Ahed ShaerОценок пока нет
- Fast Facts: Familial Chylomicronemia Syndrome: Raising awareness of a rare genetic diseaseОт EverandFast Facts: Familial Chylomicronemia Syndrome: Raising awareness of a rare genetic diseaseОценок пока нет
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?От EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?Оценок пока нет
- Fast Facts: Deficit di piruvato chinasi: Per una maggiore sensibilizzazione su questa rara malattia geneticaОт EverandFast Facts: Deficit di piruvato chinasi: Per una maggiore sensibilizzazione su questa rara malattia geneticaОценок пока нет
- Breast LumpДокумент26 страницBreast Lumpdr_asaleh100% (2)
- Knee.www.1aim.netДокумент34 страницыKnee.www.1aim.netdr_asalehОценок пока нет
- How To Deal WithДокумент65 страницHow To Deal Withdr_asalehОценок пока нет
- TrunkДокумент86 страницTrunkdr_asalehОценок пока нет
- NeckДокумент67 страницNeckdr_asaleh100% (1)
- Examination of TheДокумент29 страницExamination of Thedr_asalehОценок пока нет
- LongДокумент64 страницыLongdr_asalehОценок пока нет
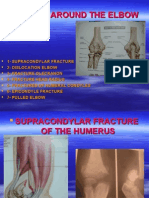
- Injuries Around TheДокумент48 страницInjuries Around Thedr_asalehОценок пока нет
- Paediatric OrthopaedicДокумент77 страницPaediatric Orthopaedicdr_asalehОценок пока нет
- BoneДокумент68 страницBonedr_asaleh100% (2)
- OrthopedicДокумент71 страницаOrthopedicdr_asalehОценок пока нет
- Hip.www.1aim.netДокумент60 страницHip.www.1aim.netdr_asaleh100% (1)
- Contents of PelvisДокумент38 страницContents of Pelvisdr_asalehОценок пока нет
- Bone JointДокумент57 страницBone Jointdr_asalehОценок пока нет
- Upper ExtremityДокумент33 страницыUpper Extremitydr_asalehОценок пока нет
- Head and NeckДокумент41 страницаHead and Neckdr_asalehОценок пока нет
- Elbow WristДокумент59 страницElbow Wristdr_asalehОценок пока нет
- Skull, Brain, CNДокумент60 страницSkull, Brain, CNdr_asaleh100% (1)
- Thoracic CavityДокумент30 страницThoracic Cavitydr_asalehОценок пока нет
- The Lower Limb: Pelvis, Thigh, Leg and FootДокумент27 страницThe Lower Limb: Pelvis, Thigh, Leg and Footdr_asaleh100% (1)
- Head and NeckДокумент41 страницаHead and Neckdr_asalehОценок пока нет
- Bones, Joints, MusclesДокумент37 страницBones, Joints, Musclesdr_asalehОценок пока нет
- Urinary IncontinenceДокумент66 страницUrinary Incontinencedr_asaleh100% (1)
- Anatomy Lecture1Документ47 страницAnatomy Lecture1dr_asalehОценок пока нет
- Artries and VeinsДокумент25 страницArtries and Veinsdr_asalehОценок пока нет
- Menstrual Disorder and Abnormal BleedingДокумент9 страницMenstrual Disorder and Abnormal Bleedingdr_asalehОценок пока нет
- Infertility IVДокумент46 страницInfertility IVdr_asalehОценок пока нет
- AbdomenДокумент11 страницAbdomendr_asalehОценок пока нет
- Infertility IIIДокумент72 страницыInfertility IIIdr_asalehОценок пока нет
- Infertility IIДокумент58 страницInfertility IIdr_asalehОценок пока нет
- Biological Activities of Stilbenoids: Molecular SciencesДокумент25 страницBiological Activities of Stilbenoids: Molecular SciencesAna PaulaОценок пока нет
- Basics of Electric Motor PDFДокумент89 страницBasics of Electric Motor PDFRajeevAgrawal100% (3)
- How To Prevented False Breakouts?: Breakout TradingДокумент3 страницыHow To Prevented False Breakouts?: Breakout Tradingimzee25Оценок пока нет
- The Fungal Kingdom by Joseph Heitman Pedro W. Crous Timothy Y. James Barbara J. Howlett Eva H. Stukenbrock Neil A. R. Gow PDFДокумент1 161 страницаThe Fungal Kingdom by Joseph Heitman Pedro W. Crous Timothy Y. James Barbara J. Howlett Eva H. Stukenbrock Neil A. R. Gow PDFIsworo Rukmi100% (3)
- Ampling Sing Atlab: BjectivesДокумент4 страницыAmpling Sing Atlab: BjectivesMBIEDA NGOMEGNI FRANK GAETANОценок пока нет
- GstarCAD Mechanical 2020 User Guide PDFДокумент238 страницGstarCAD Mechanical 2020 User Guide PDFlgfldfxhz9Оценок пока нет
- Email Security StandardsДокумент2 страницыEmail Security StandardsPeng GuinОценок пока нет
- Literature Study of HospitalДокумент18 страницLiterature Study of HospitalJasleen KaurОценок пока нет
- FET Static CharacteristicДокумент4 страницыFET Static CharacteristicAzim Kamal0% (1)
- Key Financial Ratios Checklist: Analyze Performance & SolvencyДокумент2 страницыKey Financial Ratios Checklist: Analyze Performance & SolvencyLATIFОценок пока нет
- QUIZ ONE Learning DisabilitiesДокумент22 страницыQUIZ ONE Learning DisabilitiesAbednego AckomОценок пока нет
- Notes 2. Decision Theory - ToДокумент13 страницNotes 2. Decision Theory - Tostephen mwendwaОценок пока нет
- Toyota TVIP System ProgrammingДокумент11 страницToyota TVIP System Programmingcheerios353Оценок пока нет
- Poetry Potion 09 Infinite WondersДокумент86 страницPoetry Potion 09 Infinite WondersBlack-Letter-MediaОценок пока нет
- CHAPTER 2: Ebook HomeworkДокумент2 страницыCHAPTER 2: Ebook HomeworkCHRISTINA HANAVI MILLANОценок пока нет
- Connecting Semiotics and Cultural GeograДокумент816 страницConnecting Semiotics and Cultural GeograManuel HerreraОценок пока нет
- BCM Nano Materials PDFДокумент1 страницаBCM Nano Materials PDFruchira prathyushaОценок пока нет
- Ten Million Trees Later - First ChapterДокумент14 страницTen Million Trees Later - First ChapterLarsОценок пока нет
- E-Viva Werkplaatshandboek PDFДокумент76 страницE-Viva Werkplaatshandboek PDFAntónio PedrosaОценок пока нет
- 2022 CiДокумент22 страницы2022 CiK60 Lâm Nguyễn Minh TấnОценок пока нет
- 13 Chapter7Документ19 страниц13 Chapter7Bharg KaleОценок пока нет
- Informatica Bhaskar20161012Документ90 страницInformatica Bhaskar20161012Bhaskar ReddyОценок пока нет
- TO: Belverd E. Needles, JR., PH.D., CPA, CMA From: Melanie Patton Date: May 9, 2013 SUBJECT: Evaluation of Comptronix CorporationДокумент6 страницTO: Belverd E. Needles, JR., PH.D., CPA, CMA From: Melanie Patton Date: May 9, 2013 SUBJECT: Evaluation of Comptronix CorporationjasminekalraОценок пока нет
- Kareem Shagar Formation An Oil Field Located in Ras Gharib DevelopmentДокумент53 страницыKareem Shagar Formation An Oil Field Located in Ras Gharib Developmentwisam alkhooryОценок пока нет
- Soil Classification PDFДокумент12 страницSoil Classification PDFbishry ahamedОценок пока нет
- Order To Cash SAP SDДокумент15 страницOrder To Cash SAP SDWanderAndradeОценок пока нет
- 14902-37163-1-PB JPVДокумент12 страниц14902-37163-1-PB JPVridwanОценок пока нет
- Articulator Selection For Restorative DentistryДокумент9 страницArticulator Selection For Restorative DentistryAayushi VaidyaОценок пока нет
- Industrial Gases and AcidsДокумент5 страницIndustrial Gases and AcidscarlОценок пока нет
- Gondar University 2022/23 Academic CalendarДокумент8 страницGondar University 2022/23 Academic CalendarFasil KebedeОценок пока нет