Академический Документы
Профессиональный Документы
Культура Документы
Spontaneous Bacterial Peritonitis (SBP) & Ascitic
Загружено:
Febi RahmadinАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Spontaneous Bacterial Peritonitis (SBP) & Ascitic
Загружено:
Febi RahmadinАвторское право:
Доступные форматы
Spontaneous Bacterial Peritonitis (SBP) & Ascitic Fluid Infection
Spontaneous bacterial peritonitis (SBP) is an acute bacterial infection of ascitic fluid.
Patients with cirrhosis and ascites carry a 10% annual risk of ascitic fluid
infection. Of patients with cirrhosis who have SBP, 70% are Child-Pugh class C. In these patients, the development of SBP is associated with a poor long-term prognosis.
Pathophysiology
Bacterial seeding of ascitic fluid is the principle of ascitic fluid infection. The most two likely roots are translocation and hematogenous spread
In cirrhotic patients, bacterial translocation was significantly increased only in Child C patients (30%) compared with 8% in Child B and 3% in Child A patients. In fact, the only independent predictor of translocation was Child-Pugh class.
Predisposing factor may be :
Intestinal bacterial overgrowth (attributed to decreased intestinal transit time) Impaired phagocytic function Low serum and ascites complement levels Decreased activity of the reticuloendothelial system
Etiologic agents (>90% intestinal flora)
Three forth of infections are due to aerobic gram-negative organisms (50% of these being Escherichia coli)
One fourth are due to aerobic gram-positive organisms (19% streptococcal species). However, recent data suggest the
percentage of gram-positive infections may be increasing due to
quinolone resistance among gram-positive bacteria.
Anaerobic organisms are rare (1%) because of the high oxygen tension of ascitic fluid.
Risk factors for ascitic fluid infection
severity of liver disease deficient AF bactericidal activity (AF total protein <1 g/dl, and/or AF C3 <13 mg/dl)
acute GI bleeding urinary tract infection urinary catheters, IV catheters previous episode(s) of SBP
Clinical presentation and diagnosis of ascitic fluid infection
A broad range of symptoms and signs are seen in SBP. A high index of suspicion must be maintained when caring for patients with ascites, particularly those with acute clinical deterioration.
Completely asymptomatic cases in as many as 30% of patients. Fever and chills occur in as many as 80% of patients. Abdominal pain or discomfort is found in 70% of patients.
Worsening or unexplained encephalopathy
Diarrhea
Ascites that does not improve following administration of diuretic medication
Worsening or new-onset renal failure Ileus Abdominal tenderness (50%). Hypotension (5-14%) Signs of hepatic failure such as jaundice and angiomata
Diagnostic paracentesis and direct inoculation of routine blood
culture bottles at the bedside with 10 mL of ascitic fluid must be performed. The results of aerobic and anaerobic bacterial cultures, used in conjunction with the cell count, prove the most useful in guiding therapy for those with SBP.
An ascitic fluid neutrophil count of >500 cells/mL is the single
best predictor of SBP, with a sensitivity of 86% and specificity of 98%. Lowering the ascitic fluid neutrophil count to >250 cells/mL results in an increased sensitivity of 93% but a lower specificity of 94%.
Combining these results yields the following subgroups:
SBP exists when the polymorphonuclear neutrophil (PMN) count is >250 cells/mL in conjunction with a positive bacterial culture result.
Culture-negative neutrocytic ascites (probable SBP) exists when the ascitic fluid culture results are negative, but the PMN count is >250 cells/mL. It may be the result of poor culturing techniques or late-stage resolving infection. Nonetheless, these patients should be treated just as aggressively as those with positive culture results.
Monomicrobial nonneutrocytic bacterascites exists when
a positive culture result coexists with a PMN count <250 cells/mL. Although this may often be the result of
contamination of bacterial cultures, 38% of these patients
develop SBP. Therefore, monomicrobial nonneutrocytic
bacterascites may represent an early form of SBP. For this reason, any patient suspected clinically of having SBP in this setting must be treated.
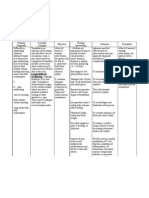
Variants of ascitic fluid infections include:
Variant of ascitic fluid (AF) infection Spontaneous bacterial peritonitis (SBP) Culture-negative neutrocytic ascites (CNNA) Secondary bacterial peritonitis* AF culture monomicrobial negative AF PMNs (per mm3) 250 250
polymicrobial
250
Monomicrobial nonneutrocytic bacterascites (MNB)
monomicrobial
< 250
Polymicrobial bacterascites**
polymicrobial
< 250
*a surgically treatable intraabdominal focus of infection exists ** a rare iatrogenic variant occurring as a result of accidental intestinal puncture during paracentesis
Other studies of ascitic fluid to be considered
Cytology Lactate: An ascites lactate level of >25 mg/dL was found to be 100% sensitive and specific in predicting active SBP in a retrospective analysis.
pH: In the same study, the combination of an ascites fluid pH of <7.35 and PMN count of >500 cells/mL was 100% sensitive and 96% specific.
Blood and urine cultures should be obtained in all patients suspected of having SBP.
Вам также может понравиться
- K21-Fever With RashДокумент76 страницK21-Fever With RashMarisa Perucana SinambelaОценок пока нет
- Clinical Manifestations and Diagnosis of Acute PancreatitisДокумент31 страницаClinical Manifestations and Diagnosis of Acute PancreatitisBrian WilliamОценок пока нет
- Hemorrhagic Conditions in Neonates: DR Hodan Ahmed, Department of Pediatrics and Child Health, Amoud Medical School, AUДокумент27 страницHemorrhagic Conditions in Neonates: DR Hodan Ahmed, Department of Pediatrics and Child Health, Amoud Medical School, AUAbdisalan hassanОценок пока нет
- Bartter SyndromeДокумент3 страницыBartter SyndromeEnny Andriani100% (1)
- Abdominal TuberculosisДокумент12 страницAbdominal TuberculosisBimlesh ThakurОценок пока нет
- CMLДокумент28 страницCMLjourey08Оценок пока нет
- Rickets of Vitamin D DeficiencyДокумент70 страницRickets of Vitamin D Deficiencyapi-19916399Оценок пока нет
- VOD - SOS in HSCTДокумент25 страницVOD - SOS in HSCTKim-Thinh Nguyen ThiОценок пока нет
- Approach To FeverДокумент80 страницApproach To FeverRaditia AbrahamОценок пока нет
- Ricardo A. Caicedo, MD: Pediatric Gastroenterology University of FloridaДокумент20 страницRicardo A. Caicedo, MD: Pediatric Gastroenterology University of FloridaAsma SikanderОценок пока нет
- Abdominal Pain in ChildrenДокумент48 страницAbdominal Pain in ChildrenSurin Jayawardene100% (1)
- Masalah Gastrointestinal KolestasisДокумент21 страницаMasalah Gastrointestinal KolestasisMuthi'ah Ramadhani AgusОценок пока нет
- Status Asthmaticus: Triwahju AstutiДокумент41 страницаStatus Asthmaticus: Triwahju AstutirianiОценок пока нет
- Anatomic Disorders of Female Reproductive SystemДокумент42 страницыAnatomic Disorders of Female Reproductive SystemNelly AstikaОценок пока нет
- Hisprung DiseaseДокумент12 страницHisprung DiseaseEky Madyaning NastitiОценок пока нет
- Acute Gastroenteritis (AGE)Документ37 страницAcute Gastroenteritis (AGE)Sari HariyaniОценок пока нет
- Celiac DiseaseДокумент25 страницCeliac DiseaseMateen ShukriОценок пока нет
- Approach To The Child With Anemia - UpToDateДокумент41 страницаApproach To The Child With Anemia - UpToDateDaniel Enrique CardenasОценок пока нет
- Intestinal Obstruction in Paediatrics - James GathogoДокумент21 страницаIntestinal Obstruction in Paediatrics - James GathogoMalueth Angui100% (1)
- TB MeningitisДокумент11 страницTB MeningitisMontserrat ÁlvarezОценок пока нет
- RabiesДокумент10 страницRabiesWinda LiraОценок пока нет
- CASE REPORT Hepatitis EditedДокумент42 страницыCASE REPORT Hepatitis EditedpernandaselpiaОценок пока нет
- Diarrhea 2016Документ37 страницDiarrhea 2016oli garkiОценок пока нет
- Hirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshДокумент48 страницHirschsprun G'S Disease: Dr. Manish Kumar Gupta Assistant Professor Department of Paediatric Surgery AIIMS, RishikeshArchana Mahata100% (1)
- Management of Diabetic Ketoacidosis in Children and AdolescentsДокумент8 страницManagement of Diabetic Ketoacidosis in Children and AdolescentsnurlatifahОценок пока нет
- Di, Siadh, CSWДокумент17 страницDi, Siadh, CSWNyomanGinaHennyKristiantiОценок пока нет
- ALL Pulmonary Leukostasis2Документ6 страницALL Pulmonary Leukostasis2Pratita Jati PermatasariОценок пока нет
- Problem-based Approach to Gastroenterology and HepatologyОт EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisОценок пока нет
- Viral ExanthemsДокумент67 страницViral ExanthemsKay HanОценок пока нет
- Necrotizing Enterocolotis (NEC)Документ2 страницыNecrotizing Enterocolotis (NEC)JDRN14Оценок пока нет
- Diabetes MellitusДокумент17 страницDiabetes MellitusRuqayya KobatteОценок пока нет
- Pathophysiology and Etiology of PCP: HIV InfectionДокумент20 страницPathophysiology and Etiology of PCP: HIV InfectionJehan Sendix100% (1)
- Pathophysiology of MalariaДокумент20 страницPathophysiology of Malariamelia100% (1)
- CEBM Levels of EvidenceДокумент2 страницыCEBM Levels of EvidenceBellatriix Bonisa MadarjaОценок пока нет
- Maternal Sepsis and Sepsis ShockДокумент17 страницMaternal Sepsis and Sepsis ShockAlvaro Andres Flores JimenezОценок пока нет
- AppendicitiesДокумент58 страницAppendicitiesGAURAV50% (2)
- Diagnosis of Gastrointestinal Bleeding in AdultsДокумент8 страницDiagnosis of Gastrointestinal Bleeding in AdultsSaeed Al-YafeiОценок пока нет
- NN Jaundice - MoteeДокумент70 страницNN Jaundice - MoteeMhmОценок пока нет
- MeningitisДокумент34 страницыMeningitispriska maniesОценок пока нет
- Diarrhea PPTДокумент82 страницыDiarrhea PPTIshwar HavaragiОценок пока нет
- Nelson JaundiceДокумент7 страницNelson JaundiceJesly CharliesОценок пока нет
- Abdominal Wound Dehiscence: DR - Nazmoon Nahar Honorary Medical Officer Surgery Unit IIIДокумент18 страницAbdominal Wound Dehiscence: DR - Nazmoon Nahar Honorary Medical Officer Surgery Unit IIIMashrufОценок пока нет
- DiarrheaДокумент38 страницDiarrheaSTEPHANIE SOR100% (1)
- Infective Endocarditis: Ainal Fadly Adigama PF Enny SuryantiДокумент50 страницInfective Endocarditis: Ainal Fadly Adigama PF Enny SuryantiFaisal Reza AdiebОценок пока нет
- CholestasisДокумент39 страницCholestasisMukhtar JamacОценок пока нет
- Pyogenic Liver AbscessДокумент10 страницPyogenic Liver AbscessErnesto Sebastian GarcíaОценок пока нет
- Inflammatory Bowel DiseaseДокумент51 страницаInflammatory Bowel DiseaseTeena Chandran100% (1)
- Gastroenteritis PPT Cha Dengan DiareДокумент75 страницGastroenteritis PPT Cha Dengan DiareJoshua Pattinson LegiОценок пока нет
- Gastric Outlet Obstruction: Its Surgical ManagementДокумент40 страницGastric Outlet Obstruction: Its Surgical ManagementGudeta shegerОценок пока нет
- Pancytopenia Secondary To Bacterial SepsisДокумент16 страницPancytopenia Secondary To Bacterial Sepsisiamralph89Оценок пока нет
- Laporan ThalassemiaДокумент30 страницLaporan ThalassemiaYama Sirly PutriОценок пока нет
- GERD DR Hegar Dec2015Документ52 страницыGERD DR Hegar Dec2015nur_betaОценок пока нет
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutОт EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutРейтинг: 5 из 5 звезд5/5 (1)
- Hereditary Spherocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHereditary Spherocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- New Concepts in the Management of Septic Perianal ConditionsОт EverandNew Concepts in the Management of Septic Perianal ConditionsОценок пока нет
- DAFTAR KELULUSAN MCQ CBT Nov 2020Документ80 страницDAFTAR KELULUSAN MCQ CBT Nov 2020Glen LazarusОценок пока нет
- Clinical Study: Detection of Glaucoma in A Cohort of Chinese Subjects With Systemic HypertensionДокумент6 страницClinical Study: Detection of Glaucoma in A Cohort of Chinese Subjects With Systemic HypertensionFebi RahmadinОценок пока нет
- Foc 2007 22 5 13Документ12 страницFoc 2007 22 5 13Febi RahmadinОценок пока нет
- Foc 2007 22 5 13Документ12 страницFoc 2007 22 5 13Febi RahmadinОценок пока нет
- ISO 9001 14001 OverviewДокумент30 страницISO 9001 14001 OverviewMusabe EdwinОценок пока нет
- Foc 2007 22 5 13Документ12 страницFoc 2007 22 5 13Febi RahmadinОценок пока нет
- Bab IДокумент29 страницBab IFebi RahmadinОценок пока нет
- Jurnal Reading 5Документ10 страницJurnal Reading 5Febi RahmadinОценок пока нет
- Jurnal Reading 5Документ10 страницJurnal Reading 5Febi RahmadinОценок пока нет
- ISO 9001 14001 OverviewДокумент30 страницISO 9001 14001 OverviewMusabe EdwinОценок пока нет
- ISO 9001 14001 OverviewДокумент30 страницISO 9001 14001 OverviewMusabe EdwinОценок пока нет
- ThesisДокумент30 страницThesisSimran JosanОценок пока нет
- Farmakologi Cns Stimulants DrugsДокумент15 страницFarmakologi Cns Stimulants DrugsRifqiОценок пока нет
- PSM Images Based QuestionsДокумент27 страницPSM Images Based QuestionsKannan KannanОценок пока нет
- Wurzel 2016Документ8 страницWurzel 2016prolanis pkmmulyoharjoОценок пока нет
- Preliminary Report of Hiv and Toxoplasma Gondii Occurrence in Pregnant Women From MozambiqueДокумент5 страницPreliminary Report of Hiv and Toxoplasma Gondii Occurrence in Pregnant Women From MozambiqueBla BlaОценок пока нет
- PRE ICF N2017 Ans KeyДокумент15 страницPRE ICF N2017 Ans KeyJonas Marvin Anaque100% (3)
- Spex Practice Test1Документ29 страницSpex Practice Test1nowОценок пока нет
- Screening For Psychological Burden of Vitiligo Using Vitiligo Impact ScaleДокумент6 страницScreening For Psychological Burden of Vitiligo Using Vitiligo Impact ScaleNadaaFahmiShofiОценок пока нет
- Assignment/ Tugasan NBHS1112 Biochemistry/ Biokimia September 2022Документ11 страницAssignment/ Tugasan NBHS1112 Biochemistry/ Biokimia September 2022iqra Harooon0% (1)
- Anaphylactic Shock: AntihistamineДокумент5 страницAnaphylactic Shock: AntihistamineAl DavidОценок пока нет
- Small PDFДокумент589 страницSmall PDFskilmagОценок пока нет
- Brugada SyndromeДокумент5 страницBrugada SyndromevitriaОценок пока нет
- Sleep Consult TemplateДокумент5 страницSleep Consult Templatesbonvallet3912100% (1)
- Ilovepdf MergedДокумент34 страницыIlovepdf MergedSheen LegsОценок пока нет
- Exercise No. 26 The Blood GroupsДокумент8 страницExercise No. 26 The Blood GroupsPATRICIA ROSE SORIANOОценок пока нет
- Physical Fitness Test Body Composition/Cardiovascular Tests: Lesson 2 For 1 Hour Day 2 Week 2 Quarter 1Документ36 страницPhysical Fitness Test Body Composition/Cardiovascular Tests: Lesson 2 For 1 Hour Day 2 Week 2 Quarter 1Elmar MariñasОценок пока нет
- Assessment of The Nutritional Status of The CommunityДокумент29 страницAssessment of The Nutritional Status of The CommunitySarad Chand YadavОценок пока нет
- ACE Personal Trainer Manual Chapter 13Документ59 страницACE Personal Trainer Manual Chapter 13Đạt NguyễnОценок пока нет
- Function of Platelets 1Документ13 страницFunction of Platelets 1deput_rprОценок пока нет
- DISEASE AGE RANGE Sex Crosstabulation: CountДокумент66 страницDISEASE AGE RANGE Sex Crosstabulation: CountchanlalОценок пока нет
- Pregnancy TestДокумент13 страницPregnancy TestAbdirahman YznОценок пока нет
- Application and Resignation LetterДокумент5 страницApplication and Resignation LetterEricka Jordan AberinОценок пока нет
- Jurnal 3Документ4 страницыJurnal 3Arum RaniОценок пока нет
- PB-00823 - Rev001 - SuperSonic MACH 40 BrochureДокумент8 страницPB-00823 - Rev001 - SuperSonic MACH 40 Brochuresoyuzmedimaging and diagnostics ltdОценок пока нет
- Advanced Life Support (Training Manual)Документ74 страницыAdvanced Life Support (Training Manual)Matt100% (25)
- Unit 6: Resistance of The Body To Infection: II. Immunity and AllergyДокумент34 страницыUnit 6: Resistance of The Body To Infection: II. Immunity and AllergyEsteban Tabares GonzalezОценок пока нет
- Threats of Vector-Borne Zoonotic Disease in Europe: Dogs, Drosophilids, and Oriental Eye WormДокумент3 страницыThreats of Vector-Borne Zoonotic Disease in Europe: Dogs, Drosophilids, and Oriental Eye WormGustavo AndresОценок пока нет
- The Canadian Etextbook of Eye MovementsДокумент10 страницThe Canadian Etextbook of Eye Movementsrinitis123Оценок пока нет
- Difficulty in SwallowingДокумент1 страницаDifficulty in SwallowingmawelОценок пока нет
- Guidelines On Dental Record KeepingДокумент8 страницGuidelines On Dental Record KeepingXubair AhmedОценок пока нет