Академический Документы
Профессиональный Документы
Культура Документы
Neonatal Hematology
Загружено:
Jay-Anne RapanoИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Neonatal Hematology
Загружено:
Jay-Anne RapanoАвторское право:
Доступные форматы
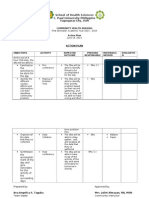
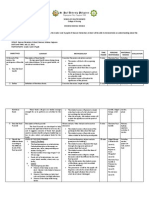
St Paul University College of
Nursing
GOOD morning !
Normal Hematologic Values
of Cord Blood in a Term Infants
Hemogloblin 16.8 gm%
Hematocrit 53%
Red Cells 5.25 mm
3
x 10
9
Reticulocyte 3.7%
Platelets 290.0
Blood Volume 50 100 cc/kg
= 85/kg
Hb in Neonates
(AOG > 34) = 16 gm %
Hb in Neonates
(AOG < 34) = 15 gm%
Hb of < 13 gm% = consider
ANEMIA
Level of Hemoglobin in the
Neonates is influenced by
several factors:
Age of Gestation
Time of Clamping of Cord
Site of Sampling
AGE OF GESTATI ON
Normal Hb for Neonates:
>34 weeks = 16 17 mg%
34 weeks = cord blood
<34 weeks = 15 mg %
SI TE OF SAMPLI NG
Capillary sampling in 1
st
48 hours:
2-3 gm% higher than cord
Factors Affecting Hemoglobin
Concentration
E Blood volume of infant may be
increased by up to 61% by allowing
complete emptying of placental vessels
before cord is clamped
E Blood vessels contain 75 125 ml of blood
E 50% of blood is transfused after 30 seconds
E 25% of placental blood transferred after 15
seconds from birth
CORD CLAMPING
Hemorrhage
Occult
Intranatal
Postnatal
Latrogenic
Hemolysis
Immune
Congenital
RBC Defects
Acquired
Under Production
of RBC
CAUSES OF ANEMIA
1. Feto-maternal
- 50% - ( + ) fetal cells in
maternal
circulation
- 8% - 0.8 40 cc blood
transfused
- 1% - > 40 cc transfused
Types of hemorrhage in Newborn
May follow
4Traumatic amniocentesis
4Spontaneous delivery
4External Cephalic version
Signs & Symptoms
4Volume and rapidity of loss
Diagnosis
4(+) Fetal cells in maternal circulation
Types of Hemmorhage in Newborn
occult hemorrhage, feto-maternal
Types of hemorrhage in Newborn
occult hemorrhage
2. Feto- fetal
13-33 % of monozygotic twins
with monochorial placenta
Anemia donor
Polycythemia recipient
Timing
20% Recent
20% Chronic
TWIN RECIPIENT
L Usually larger, up to
1000gm disparity
L Polycythemia
L Jaundice
L Cardiac hypertrophy
L Increased muscular
mass
L Polyhydramnios
L Large congested
placenta
TWIN DONOR
L Usually smaller
L Anemia
L Hypoglycemia
L Cardiac atrophy
L Decreased muscle
mass
L Oligohydramnios
L Small pale placenta
CRITERIA FOR DIAGNOSIS OF TWIN
TRANSFUSION SYNDROME
* Monochorial Placentation ( + )
+ Disparity in color ( + )
4 Difference in Hemoglobin of
greater than 5g/dl ( + )
^ Unexplained Hydramnios ( - )
= Marked weight difference (
- )
Table 1. Composite Definition of the Twin-Twin
Transfusion
Criteria Suggested Cut- off Values
I. Minor
1.) Sonographic Inter- twin abdominal
circumference
>1% mm
poly/oligohydramnios,
signs of monozygosity
2.) Doppler velocimetry Inter twin difference in S/D
(umbilical arteries) ratio > 0. 4
II. Major
1.) Transplacental shunt
2.) Birth weight Inter twin difference > 15 %
( heavier twin = 100% )
3.) Hemoglobin Inter twin difference > 5/dl
S/D = systolic / diastolic
* Two major criteria or one minor and one major criteria are
needed
* Criteria may be found by antenatal funipuncture or postnatally
Additional Criteria:
Same sex , disparity in size or in the number Of vessels in
the umbilical cords , single placenta Showing divergent
echogenecity of the Cotyledons supplying the two cords ,
and evidence Of hydrops in either twin or congestive Heart
failure in the recipient.
Brennan et. al
Types of Hemorrhage in Newborn
B. Intranatal Hemorrhage
Obstetric accidents
Malformation of placenta / cord
Rupture of normal umbilical cord
Precipitous delivery; entanglement
Hematoma of cord or placenta
Rupture of an abnormal umbilical cord
Rupture of anomalous vessels
Aberrant vessels; velamentous insertions;
communication in multilobed placenta
Incision of placenta during CS
Placenta previa
Abruptio Placenta
Types of Hemmorhage in
Newborn
Hemorrhage
- caused by traumatic delivery
- Intracranaial hemorrhage
- Giant cephalhematoma
- Retroperitoneal
- Ruptured Liver
- Ruptured Spleen
Treatment of Hemorrhage
O General supportive measures
O Hypovolemic shock
whole blood 20 cc/ kg
6 ml / kg of whole blood Increases
3 ml / kg of packd RBC Hgb by 1
gm
Hemolysis
O Immune Hemolytic Anemia
Rh incompatibility
ABO incompatibility
Minor Blood groups
O Congenital Defects of RBC
Membrane
Hb synthesis
Enzyme Deficiency
O Acquired
Infection
Drugs
Hemolysis
A. Immune Hemolytic Anemia
1. Rh Incompatibility
Incidence: 0.06%
Perinatal morbidity: 17%
14% Stillbirths
+ Hemolysis more severe with second wherein
sensitization has occurred
q Isoimmunization more frequent in
Toxemia
Cesarean Section
Manual removal of placenta
Immune Hemolytic Anemia,Rh Incompatibility
PATHOPHYSIOLOGY
Antibody transfer from mother to infant
With increased breakdown, increased
production involving no-marrow sites
(liver,spleen,lungs)
organomegaly
Hydrops fetalis severe manifestation
Mild Manifestations:
* Jaundice in the first 24 hours
* Anemia
* Hepatomegaly
Rh incompatibility
O Laboratory Findings
>Rh mother, Rh + baby
>Anemia
> retic. count (6% or more)
( + ) Coombs Test
O Treatment
>Anti Rh Ig to Rh mother after birth to Rh +
baby or after an abortion
>exchange transfusion for bilirubin > 20mg %
Immune Hemolytic Anemia
2. ABO Incompatibility
+ Hemolysis results from the action of
maternal
anti-A or anti-B on fetal RBCs
+ Incidence of severe hemolysis is low
+ Anti A and Anti B antibodies are found
in the IgG,IgM,IgA fractions,but only IgG
cross the
placenta and cause hemolysis
+ Fewer A and B antigenic sites present in the
RBC
ABO Incompatibility Diagnosis
Mother Type O, baby type A/B
Anemia, reticulocytosis, spherocytosis
Weakly ( + ) Coombs Test
Anti -A or B antibody in maternal serum
TREATMENT
Phototherapy
Exchange Transfusion
CLINICAL AND LABORATORY FEATURES OF
RH AND ABO INCOMPATIBILITY
R H A B O
CLINICAL FEATURES
Frequency
Pallor
Jaundice
Hydrops
Hepatospenomegaly
Unusual
Marked
Marked
Common
Marked
Common
Minimal
Minimal
Moderate
Rare
Minimal
LABORATORY
Blood Type Mother
Baby
Anemia
Coombs Direct
Indirect Coombs
Bilirubin
RBC Morphology
RH
RH +
Marked
+
+
Marked
Nucleated
O
A or B
Minimal
Frequently
+
Variable
Shperocytes
Hemolysis
1. Enzymatic Deficiency
a. G 6 - P - D Deficiency
4 Incidence > highest in
Mediterranean,Africa,
and China
4 Sex - linked, male
4 Jaundice from 3
rd
to 5
th
day
B. Congenital RBC Defects
Predisposing Factors
L Infection
L Drugs
Pathophysiology (G6PD Deficiency)
Oxidants generate H
2
O
2
which assault
enzyme deficient RBC Hb insult results in
globin destruction with HEI NZ body
formation causing membrane injury and
hemolysis
G6PD needed for synthesis of reduced
glutathion which is an Intracellular buffer
against oxidant agents
G6PD Deficiency Diagnosis
same as other hemolytic disorders
> low glutathion levels
> low G6PD levels
Treatment
E Blood transfusion
E Remove drugs
E Folic Acid
Hemolysis
Congenital RBC defects, enzymatic deficiency
b. Pyruvate Kinase Deficiency
Low level of Pyruvate kinase
Impaired ATP generation
K
+
leakage from cell
Reduced life span
Pyruvate Kinase
DeficiencyDiagnosis
Assay of Pyruvate Kinase
TREATMENT
> Blood transfusion
> Splenectomy
Congenital RBC Defects
2. Membrane Abnormalities
Normal RBCs are biconcave
a. Hereditary Spherocytosis
( Congenital Hemolytic Anemia)
# Autosomal dominant
# Characterized by osmotically fragile
spherical cells (with ^ Na influx into
the cell)
# May present as anemia and jaundice in the
newborn; splenomegaly after
infancy
Hereditary Spherocytosis
- Osmotic fragility test
- Presence of microspherocytes on
peripheral blood smears
DIAGNOSIS
Membrane Abnormalities
A. Hereditary Elliptocytosis
Heterogenous Disorder
Oval or elliptical cells in blood
Decrease in membrane surface due to
disorder of membrane skeleton
May present as anemia and jaundice in
the newborn
TREATMENT
L Splenectomy in older child
b. Hereditary Stomatocytosis
E Due to inherited disorder or red cell cation
permeability
E Cells are cup shaped
c. Hereditary Poikilocytosis
E Decrease membrane surface due to disorder
of membrane skeleton
E Presence of fragmented RBCs
Membrane Abnormalities
3. Defects in Hemoglobin Synthesis
A. Thalassemias
> Heterogenous group of heritable
hypochromic anemia
1) Beta Thalassemia
Impaired production of Beta chains
Prevalent among Mediterranean
people
Hemolysis
Congenital RBC Defects
B.) Beta Thalassemia ( Cooleys)
Homogenous transmission
Severe hemolytic anemia in the second 6
months of life
Repeated transfusion needed to maintain
life
Hypertrophy of extramedullary sites
THALASSEMIA
A.) Beta Thalassemia Minor ( Trait )
* Associated with mild anemia
+ High level of Hb A2 or Hb F
4 Mistaken for Iron Deficiency
Anemia
THALASSEMIA
2. ) Alpha Thalassemia
4 Impaired production of alpha chains
Hemolysis
Congenital RBC Defects
Thalassemia
Peripheral smear of microcytic,
hypochromic anemia with bizarre cells
Excess alpha chain in the RBCs
Anemia and Jaundice
D I A G N O S I S
B. Sickle Cell Anemia
C Product of abnormal B polypeptide
chain
C Severe chronic hemolytic anemia if
homozygous for sickle cell
trait
C Episodes of vaso-occlusive and
sequestration crisis
C RBC contains 90% HbS, 10% HbF
Defects in Hb Synthesis
Transfusion during vaso-occlusive
crisis where Hb S is reduced to 40%
Partial exchange transfusion
Sickle Cell Anemia
TREATMENT
C. Acquired Defects of RBC
Infections
> especially in septicemia
Drugs
> Arsenic
> Phenylhydrazine
Congenital RBC Defects
Defects in Hb Synthesis
Fundamental Basis of
Hemolytic Anemia
D Shortened survival time of RBC
D Increased activity of bone marrow
D Reticulocyte count of 3 8%
D Hyperplasia of erythropoietic marrow
elements
D Increased indirect bilirubin
D Formation of gallbladder stone
Onset:
Anemia occurs within the first year
of life25% at birth, 65% by 6
th
months
Male : Female = 1 : 1
Diamond Blackfan Anemia
Physical Examination
60% with congenital anomalies
Usually small in stature
Abnormal facies
Renal abnormalities
Congenital Heart Disease
( VSD, ASD, Coarctation )
Mental retardation
Hypogonadism
Diamond Blackfan Anemia
III. Congenital Red Cell Aplasia
( Diamond-Blackfan Anemia )
Diagnostic Criteria
O Normocytic, macrocytic anemia
O Reticulopenia
O Bone marrow with normal cellularity
and usually with a deficiency of red
cell precursor
O More WBC, platelets
Laboratory
Increase of fetal Hb
Normal cellurity of bone marrow
Erythroid hyperplasia
Pathology
Defective stem cell
Diamond Blackfan Anemia
- Blood transfusions
- Steroid therapy
- Splenectomy
- Androgen
Diamond Blackfan Anemia
Treatment
THE ANEMIC NEWBORN
History-family,maternal and obstetric Hb,
Retic Count, Blood Smear, Direct Coombs Test
Normal Subnormal
( + ) ( - )
Isoimmunization
Rh , Minor grp.
Peripheral
Blood Smear
Normochromic
Normocytic
Hypochromic
Microcytic
Specific morphologic
abnormality
Consider Congenital
hypoplatic anemia
perform bone marrow
Perform blood typing
Of mother and infant
And look for maternal
antibodies
Consider:
Chronic fetomaternal
Transfusion of twin to
Twin transfusion
Examine maternal
blood for fetal cells
Coombs Test
the anemic newborn
Peripheral Blood Smear
Normochromic, Normocytic
No jaundice or
hepatospenomegaly
Consider Acute blood lloss
Obstetric accident
Fetomaternal hemorrhage
Internal hemorrhage
(+) Jaundice
Congenital
Enzymatic defect
Of RBC
G 6 PD
Pyruvate Kinase
And others
Infectious
Bacterial
Viral
Cytomegalic Inclusion Ds
Congenital Syphilis
Toxoplasmosis
Galactosemia
Respiratory
Distress
Osteoporosis
Leukemia
Oski and naiman,1972
(Avery)
0
0000
COAGULATION PROFILE OF NB
NORMAL
CHILDREN
TF PREMIE
Platelet count 200 400,000 200 400,000 150 - 350,000
Bleeding Time 2.5 5.5 sec 2.5 5.5 2.5 5.5
Prothrombin
Time
12- 14 sec 13 20 sec 13 21 sec
PTT 37 50 sec 45 65 sec 45 75 sec
Activated PTT 25 35 35 - 45 35 - 55
Clotting factors
Normal
Slight
Moderate
All
-
-
Fibrinogen, V,
VIII, XII,XIII
Fibrinogen,
V,VII, XII,
XIII,
II,VII,IX,X
Physiologic Variables in Neonates
Which Influence Hemostasis
1. Platelets
> Platelet counts of 150,000 to 400,000 /
mm
2
present in a 30 week old fetus
> Abnormal platelet aggregation noted in
both normal and premature newborn
2. Coagulation Proteins
- Formation of a firm, insoluble clot
accompanies primary platelet plug and results
from a complex interaction of coagulation
proteins
- Many coagulation factors present in reuced
concentration
- Factors requiring Vitamin K for activity are
present in reduced concentration ( II,VII,IX,X )
- Fibrinogen, Factors V,VIII,XIII are normal
- Factors XI,XII
Physiologic variables
O Inherited Defects of Coagulation Mechanism
A. Hemophilia A
B. Hemophilia B
C. Hemophilia C
O Accentuation of normally occuring transitory
mechanism:
Hemolytic Disease of the Newborn
O Transitory disturbance secondary to associated
disease:
Disseminated I ntravascular Coagulation
CAUSES OF BLEEDING
O Quantitative/ Qualitative abnormalities of platelets:
A. Immune
1. Maternal ITP
2. Isoimmunization
3. Drugs
B. Infection
C. DIC
Inherited Defects of Coagulation
Hemophilia A Factor VIII
Hemophilia B Factor IX
Hemophilia C - Factor XI
CAUSES OF BLEEDING
Hemophilia maybe manifest in the newborn
since neither Factor VIII nor Factor IX cross
the placenta
However, few babies develop serious
bleeding
May have oozing from umbilical stump
Surgical Trauma ( Circumcision )
Recurrent bleeding episodes occur by mid-
to late infancy
Hemophilia
Screening Test Abnormality
- Prolonged Partial Thromboplastin
Time( PTT )
- Low assay of Factors VIII or IX
Hemophilia
Exaggeration of Normally Occuring Transitory Disease
(Hemorrhagic Disease of the Newborn)
w All infants are born with deficient vitamin K stores
but only a minority develop generalized bleeding
w Bleeding may be in the form of cephalhematoma,
GIT,umbilical and oozing from the puncture
sites
w Relatively rare because of routine administration
of vitamin K
CAUSES OF BLEEDING
Etiology of Vitamin K deficiency in the
Newborn Period
TIME
At birth
TYPE
1. Severe early
deficiency
A. Normal Infant
B. Infants whose mothers
received drugs impairing
Vit. K acitvity
(Warfarin,Phenytoin,
Phenobarbital)
COMMENTS
Spontaneous
cephalhematoma
Scalp hemorrhage at
monitor sites
Frequent occurrence
of intracranial
hemorrhage
Vitamin K deficiency
TYPE
3. Delayed hemorrhagic
disease of the newborn
a.) Otherwise normal
infants
b.) Infants with disorders of
intestinal absorption
TIME
4 12 weeks of
age
COMMENT
Failure to receive
Vit.K prophylaxis at
birth
Breastfed infants,had
diarrhea,received
broad spectrum
antibiotics
Cystic Fibrosis
Abetalipo-proteinemia
Vitamin K deficiency
Delayed hemorrhagic disease of the NB
TYPE
C. Infants who received
broad spectrum
antibiotics
D. Infants who received
perenteral
hyperalimentation
(without Vitamin K)
COMMENT
Particularly if other
factors are present
(breastfeeding,
diarrhea,no vitamin K
at birth)
TYPE
2. Classic
hemorrhagic
disease of he
newborn
Vitamin K deficiency
TIME
2-3 days of life
COMMENT
Failure to
receive
Vitamin K
prophylaxis at
birth
Infant usually
breastfed
LABORATORY
DIAGNOSIS
Normal platelet count
Prolonged PTT, PT time
Abnormal clotting and clot
retraction time
Normal bleeding time
III. Bleeding Associated with a Disease
Process (DIC)
1. Infection
p Bacterial
p Viral
2. Asphyxia
p Severe Birth Asphyxia
p Hypothermia
p Respiratory Distress Syndrome
p Severe Congestive Heart Failure
3. Obstetric Complication
p Abruptio Placenta
p Retained Dead Term Fetus
p Pre-eclampsia
4. Vascular / Neoplastic Lesion
pCavernous Hemangioma
pChorangioma
pNephroblastoma
5. Necrotizing Enterocolitis
6. Severe Hemolysis Rh I mmunization
7. Sick Premature, Dysmature
8. Miscellaneous
pSurgery
pCongenital Malformation
pTrauma
Bleeding with Disease Process
1. During accelerated coagulation, certain
clotting factors ( II, V, VII &
Fibrinogen ) are consumed at a rate
they are synthesized
2. Persistent stimulation of clotting
activates fibrinolysis with production of
fibrin split products. The FSP cause
hemorrhage by inhibiting the normal
conversion of fibrinogen to fibrin
BLEEDING IN DIC due to
1. Decreased platelets
2. Prolonged PT and PTT
3. Decreased factors V, VIII, fibrinogen
4. Increased fibrin split products
5. Microangiopathic RBC changes
LABORATORY DIAGNOSIS IN DIC
1. Vigorous treatment of underlying condition
2. Plasma and Platelet infusion
3. If serious bleeding occurs:
a. consider exchange transfusion
b. continue platelet and plasma infusion
4. If clinical presentation is mainly thrombotic
a. administer heparin intravenously
b. after Heparinization, give plasma and
platelets
THERAPY IN DIC
C Most frequent cause of
generalized hemorrhage in sick
infants is DIC
C More than half of all cases of
childhood DIC occur during the
newborn period
Differential Features of Hemorrhage of
the newborn
FEATURES VITAMIN K
DEFICIENCY
DIC
Uniformity of
clotting defect
Capillary fragility
Bleeding Time
Clotting Time
One stage
prothrombin
PTT
Constant
Normal
Normal
Prolonged
Very prolonged
< 5 %
Prolonged
Variable
Usually
abnormal
Often prolonged
Variable
Mod. Prolonged
Prolonged
Features of Hemorrhagic Disease
FEATURES
Response to
vitamin K
Associated
Disease
Previous History
VITAMIN K
DEFICIENCY
Spectacular
Usually trivial
(Trauma)
No vitamin K;
Anticonvulsants
DIC
Absent
Severe
Vitamin K given
FEATURES
Thrombin Time
Fibrin degradation
products
Factor V
Fibrinogen
Platelets
Red cell
fragmentation
Features of Hemorrhagic Disease
VITAMIN K
DEFICIENCY
Normal
Not present
Normal
Normal
Normal
Not present
DIC
Usually
prolonged
Present
Depressed
Often decreased
Often decreased
Usually present
Qualitative / Quantitative Abnormalities
of Platelets
Causes of Platelet Dysfunction
A. IMMUNE
1. Maternal ITP 50 to 85% of babies will
develop ITP
2. Isoimmunization
3. Drugs
a. Quinine
b. Quinidine
c. Digitoxin
d. Sulfas
Immune Related Platelet Abnormalities
2. Isoimmune Neonatal Thrombocytopenia
Newborn has platelet-specific antigen which crosses
placenta to platelet - negative antigen mother
production of antibodies
1:5000 births, first born affected
Diagnosis: Clinical history
Exclusion of other entities
- Should be instituted if platelet count falls
below 30 40,000 as CNS bleeding may occur
in 10% of cases
- Usually exchange transfusion followed by
maternal platelet transfusion
- Recurrence of thrombocytopenia may be 75
85% in subsequent offsprings
Treatment
3. Drug Induced
) Quinidine
) Quinine
) Sulfas
Immune Related Platelet Abnormalities
B. Infection
may cause ^ platelet destruction
Bacterial Agents
> Cytomegalic Inclusion Disease
> Toxoplasmosis
> Syphilis
> Rubella
> Herpes
Platelet Abnormalities
* Inhibition of megakaryocytes by causative
agents or metabolites
+ Reticuloendothelial hypoplasia may lead to
platelet sequestration
4 Presence of endothelial damage and
vasculitis,stagnant blood flow and hypoxia
may cause direct aggregates of platelets by
viruses or bacterial products
Platelet Abnormalities, Infection
C. Giant Hemangioma
D. With Massive Splenomegaly
E. Bone Marrow Involvement
Congenital leukemia
Congenital neuroblastoma
Leterrer-Siwe DiseaseOsteoporosis
I nborn Errors of Metabolism
Platelet Abnormalities
L Transfusion of fresh platelet
concentrate
I unit raises platelet count to
> 1000,000 / mm
3
L Treatment of underlying cause
Platelet Abnormalities
Treatment
Вам также может понравиться
- VWD AdvancesДокумент11 страницVWD Advancesمحمد شاهين100% (1)
- CPH Lab Activity 7: Automated HematologyДокумент44 страницыCPH Lab Activity 7: Automated HematologyChelsea Padilla Delos Reyes100% (1)
- The Clinical Relevance of Nucleated Red Blood Cell CountsДокумент5 страницThe Clinical Relevance of Nucleated Red Blood Cell CountspaconscribdОценок пока нет
- Blood Cell Morphology TutorialДокумент176 страницBlood Cell Morphology TutorialCharles Jebb Belonio JuanitasОценок пока нет
- Management - Guidelines - of - Malaria - in - Malaysia - (Final) v2 PDFДокумент63 страницыManagement - Guidelines - of - Malaria - in - Malaysia - (Final) v2 PDFaiyuanОценок пока нет
- Lipemia: Causes, Interference Mechanisms, Detection and ManagementДокумент16 страницLipemia: Causes, Interference Mechanisms, Detection and ManagementkartikaparamitaОценок пока нет
- Blood Morphometry or Blood Film CommentДокумент103 страницыBlood Morphometry or Blood Film CommentYangnuu TitusОценок пока нет
- Optimization of Prothrombin INR Testing Through The Fabrication of Integrated Microfluidic StripsДокумент20 страницOptimization of Prothrombin INR Testing Through The Fabrication of Integrated Microfluidic StripsFiras QureshiОценок пока нет
- Automated Capillary Electrophoresis in The ScreeningДокумент9 страницAutomated Capillary Electrophoresis in The Screeningsomething privateОценок пока нет
- Lab Activity No. 5 - Slide PresentationДокумент24 страницыLab Activity No. 5 - Slide PresentationChelsea Padilla Delos ReyesОценок пока нет
- Red Blood Cell Morphology: A Seminar on RBC AbnormalitiesДокумент11 страницRed Blood Cell Morphology: A Seminar on RBC AbnormalitiesChabОценок пока нет
- Ana IfДокумент101 страницаAna Ifshrikrishnapathlab100% (1)
- A Review of Thromboelastography PDFДокумент5 страницA Review of Thromboelastography PDFWAGNER AUGUSTO POLESОценок пока нет
- Techtalk August2010Документ2 страницыTechtalk August2010Abu KhalidОценок пока нет
- 11auto Unit Cell Counting Instruments HandoutДокумент15 страниц11auto Unit Cell Counting Instruments HandoutyoraikarОценок пока нет
- 1.anaemia Intro, Retic, IndicesДокумент69 страниц1.anaemia Intro, Retic, IndicesInaGargОценок пока нет
- Advia 120 Troubleshooting GuideДокумент21 страницаAdvia 120 Troubleshooting GuideJaime Elias100% (1)
- Interpretation of Peripheral SmearДокумент34 страницыInterpretation of Peripheral Smearswathi bs100% (1)
- Haematopathology 3:: Leucocytosis/LeucopeniaДокумент113 страницHaematopathology 3:: Leucocytosis/LeucopeniaarwaОценок пока нет
- The Peripheral Blood FilmДокумент5 страницThe Peripheral Blood FilmanggaririnОценок пока нет
- HEMA LAB Reticulocyte Study ESR OFT RBC CountДокумент17 страницHEMA LAB Reticulocyte Study ESR OFT RBC CountJam RamosОценок пока нет
- ADVIA-2120i Hematology TrainingДокумент73 страницыADVIA-2120i Hematology TrainingLoay TibiОценок пока нет
- ICSH Guidelines For The Evaluation of Blood Cell AnalysersДокумент16 страницICSH Guidelines For The Evaluation of Blood Cell Analyserssellappan marappanОценок пока нет
- Laboratory Hematology CriteriaДокумент7 страницLaboratory Hematology CriteriaRosОценок пока нет
- Flight ExplainedДокумент8 страницFlight Explainedapi-253153921Оценок пока нет
- Sysmex SEED 4 2013 Automated Haematology Sample Interferences Flagging and Results Interpretation - Part 1 enДокумент8 страницSysmex SEED 4 2013 Automated Haematology Sample Interferences Flagging and Results Interpretation - Part 1 enPieter Du Toit-Enslin50% (2)
- LHB2017Документ238 страницLHB2017haslinda84100% (2)
- Lab Handbook Sickle Cell Thalassaemia ScreeningДокумент74 страницыLab Handbook Sickle Cell Thalassaemia Screeningpieterinpretoria391Оценок пока нет
- Hematology OncologyДокумент476 страницHematology OncologySukumar SubramaniОценок пока нет
- BLS MCQ CoagulationДокумент4 страницыBLS MCQ CoagulationsssajiОценок пока нет
- Automation in HaematologyДокумент67 страницAutomation in Haematologyk11a1r18Оценок пока нет
- Statistical Approach in HematologyДокумент33 страницыStatistical Approach in HematologycandiddreamsОценок пока нет
- MTY 1211 Chapter 1 Overview Clinical Lab HematologyДокумент68 страницMTY 1211 Chapter 1 Overview Clinical Lab Hematologychris andrieОценок пока нет
- Kaplan: Clinical Chemistry, 5 Edition: Clinical References - Methods of AnalysisДокумент9 страницKaplan: Clinical Chemistry, 5 Edition: Clinical References - Methods of AnalysispudjoОценок пока нет
- Hemophilia and Factor Assay PDFДокумент17 страницHemophilia and Factor Assay PDFSumaira JunaidОценок пока нет
- Automated Cell Counting InstrumentationДокумент33 страницыAutomated Cell Counting InstrumentationCecille AnnОценок пока нет
- Top 5 Leukogram Patterns 22976 Article PDFДокумент3 страницыTop 5 Leukogram Patterns 22976 Article PDFAl MisbahОценок пока нет
- Hematological Investigation or Quantitative Evaluation of The Hematopoietic SystemДокумент21 страницаHematological Investigation or Quantitative Evaluation of The Hematopoietic SystemMAMA LALAОценок пока нет
- Blood Film AbnormalitiesДокумент26 страницBlood Film AbnormalitiesSana Bushra100% (2)
- Pre-Analytical Variables in Coagulation TestingДокумент20 страницPre-Analytical Variables in Coagulation TestingTaylorОценок пока нет
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFДокумент16 страницHarrisADVIA2120methods LabHema2005 11 47-61 PDFedu_14cОценок пока нет
- Praktikum MDTДокумент16 страницPraktikum MDTnanda andhyka100% (1)
- Metodo, Entrenamiento y Principios Del ADVIA 120Документ64 страницыMetodo, Entrenamiento y Principios Del ADVIA 120Jaime Elias100% (3)
- Department of Pathology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu, IndiaДокумент14 страницDepartment of Pathology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu, IndiaaishaОценок пока нет
- RBC Disorders 2019 - 190619134512Документ217 страницRBC Disorders 2019 - 190619134512Yohannes MeridОценок пока нет
- TLC DLCДокумент67 страницTLC DLCchandra shekharОценок пока нет
- Blood Smear Examination 1معدل Документ74 страницыBlood Smear Examination 1معدل Kenesa100% (1)
- Mixing Studies 1pp 08-13-15.pptx 0 PDFДокумент49 страницMixing Studies 1pp 08-13-15.pptx 0 PDFKholifah LintangОценок пока нет
- Hematology Performance Verification Manual: Beckman Coulter, IncДокумент122 страницыHematology Performance Verification Manual: Beckman Coulter, IncanggaririnОценок пока нет
- Blood Cell Morphology Controversies and Alternativ PDFДокумент137 страницBlood Cell Morphology Controversies and Alternativ PDFWa Nur Arlin RahmadhantyОценок пока нет
- Preparation of Blood Smear With Different Staining Method: Dr. Ankur Patel Ankurvety001@gmail.c OmДокумент56 страницPreparation of Blood Smear With Different Staining Method: Dr. Ankur Patel Ankurvety001@gmail.c OmPravin AmbadeОценок пока нет
- Prepartion of Blood Smear Hematology PresentationДокумент44 страницыPrepartion of Blood Smear Hematology PresentationArslan ArshadОценок пока нет
- Color Atlas of Haematology 2000Документ20 страницColor Atlas of Haematology 2000Zahraa Al-Sayed100% (1)
- Molecular Diagnosis in HaematologyДокумент23 страницыMolecular Diagnosis in HaematologyUmar'Farouq Oni100% (1)
- HB Electrophoresis and HPLC StudyДокумент55 страницHB Electrophoresis and HPLC Studyapi-243480627Оценок пока нет
- White Blood Cell Disorders: Neoplastic Diseases of The BloodДокумент81 страницаWhite Blood Cell Disorders: Neoplastic Diseases of The BloodMiguel Cuevas Dolot100% (1)
- Certification From Hospital/ Institution Form: Last Name, First Name, Middle InitialДокумент1 страницаCertification From Hospital/ Institution Form: Last Name, First Name, Middle InitialJay-Anne RapanoОценок пока нет
- Office: of The SecretaryДокумент1 страницаOffice: of The SecretaryJay-Anne RapanoОценок пока нет
- Virtual LearningДокумент6 страницVirtual LearningJay-Anne RapanoОценок пока нет
- Unpaid Solar Streetlight Obligation NoticeДокумент1 страницаUnpaid Solar Streetlight Obligation NoticeJay-Anne RapanoОценок пока нет
- articleCritiqueKey 1Документ7 страницarticleCritiqueKey 1Jay-Anne RapanoОценок пока нет
- DR Elizabeth Paz-Pacheco 4 - 1 - 2020 Coping With DM During The COVID CrisisДокумент32 страницыDR Elizabeth Paz-Pacheco 4 - 1 - 2020 Coping With DM During The COVID CrisisJay-Anne RapanoОценок пока нет
- Manulife Affluence-Max-Elite BrochureДокумент2 страницыManulife Affluence-Max-Elite BrochureJay-Anne RapanoОценок пока нет
- 3Документ1 страница3Jay-Anne RapanoОценок пока нет
- CertificationДокумент6 страницCertificationJay-Anne RapanoОценок пока нет
- 4Документ1 страница4Jay-Anne RapanoОценок пока нет
- Supply and Installation of 100w Solar Street LightДокумент2 страницыSupply and Installation of 100w Solar Street LightJay-Anne RapanoОценок пока нет
- This Is How To Do It!: WebinarДокумент1 страницаThis Is How To Do It!: WebinarJay-Anne RapanoОценок пока нет
- Saint Paul University Philippines: Objectives Activity Time Frame Expected Outcome Materials Persons ResponsibleДокумент2 страницыSaint Paul University Philippines: Objectives Activity Time Frame Expected Outcome Materials Persons ResponsibleJay-Anne RapanoОценок пока нет
- MAN 202 Assignment (RAPANO, MAESTRE)Документ13 страницMAN 202 Assignment (RAPANO, MAESTRE)Jay-Anne RapanoОценок пока нет
- Nurses' knowledge and practices regarding prevention of surgical site infectionsДокумент5 страницNurses' knowledge and practices regarding prevention of surgical site infectionsJay-Anne RapanoОценок пока нет
- Saint Paul University Philippines: Tuguegarao City, Cagayan, 3500 A.Y. 2011-2012Документ2 страницыSaint Paul University Philippines: Tuguegarao City, Cagayan, 3500 A.Y. 2011-2012Jay-Anne RapanoОценок пока нет
- RAPANO - MSN - Ass-3Problem-Identification-1Документ2 страницыRAPANO - MSN - Ass-3Problem-Identification-1Jay-Anne RapanoОценок пока нет
- Thyroid Cancer Case StudyДокумент6 страницThyroid Cancer Case StudyJay-Anne RapanoОценок пока нет
- First PageДокумент6 страницFirst PageJay-Anne RapanoОценок пока нет
- CHN Action Plan for St. Paul UniversityДокумент2 страницыCHN Action Plan for St. Paul UniversityJay-Anne RapanoОценок пока нет
- School of Health Sciences St. Paul University Philippines: Tuguegarao City, 3500Документ2 страницыSchool of Health Sciences St. Paul University Philippines: Tuguegarao City, 3500Jay-Anne RapanoОценок пока нет
- Saint Paul University Philippines: Tuguegarao City, Cagayan, 3500 A.Y. 2011-2012Документ2 страницыSaint Paul University Philippines: Tuguegarao City, Cagayan, 3500 A.Y. 2011-2012Jay-Anne RapanoОценок пока нет
- Session Design (Revised)Документ5 страницSession Design (Revised)Jay-Anne RapanoОценок пока нет
- St. Paul University Philippines: Tuguegarao City, Cagayan 3500 School of Health Sciences College of NursingДокумент1 страницаSt. Paul University Philippines: Tuguegarao City, Cagayan 3500 School of Health Sciences College of NursingJay-Anne RapanoОценок пока нет
- Anatomy and Physiology of The Respiratory SystemДокумент4 страницыAnatomy and Physiology of The Respiratory SystemJay-Anne RapanoОценок пока нет
- IEEE Device NumbersДокумент3 страницыIEEE Device NumbersJuan Antonio Sosa MirandaОценок пока нет
- RH Control - SeracloneДокумент2 страницыRH Control - Seraclonewendys rodriguez, de los santosОценок пока нет
- Effect of warm water foot bath therapy on blood pressure reductionДокумент8 страницEffect of warm water foot bath therapy on blood pressure reductionPutraОценок пока нет
- Blood Bank Unit Pretest GuideДокумент9 страницBlood Bank Unit Pretest GuideMary CabalceОценок пока нет
- Technical Report On Biochemistry SIWSДокумент23 страницыTechnical Report On Biochemistry SIWSUmar Ridwan sani100% (2)
- GANGGUAN HEMODINAMIK, TROMBOSIS DAN SYOKДокумент67 страницGANGGUAN HEMODINAMIK, TROMBOSIS DAN SYOKmarsal25Оценок пока нет
- Initial Management of Moderate To Severe Hemorrhage in The Adult Trauma Patient - UpToDateДокумент38 страницInitial Management of Moderate To Severe Hemorrhage in The Adult Trauma Patient - UpToDateiustin loghinОценок пока нет
- Thromboelastography: Clinical Application, Interpretation, and Transfusion ManagementДокумент7 страницThromboelastography: Clinical Application, Interpretation, and Transfusion ManagementAbhishek PandeyОценок пока нет
- Order of DrawДокумент8 страницOrder of DrawVincent ReyesОценок пока нет
- Blood DДокумент1 страницаBlood DEsther Elizabeth GualanОценок пока нет
- Tube CHG Coag Test Jul 1Документ2 страницыTube CHG Coag Test Jul 1Muse GobiОценок пока нет
- Blood Typing Lab Activity FinalДокумент3 страницыBlood Typing Lab Activity FinalMrRightОценок пока нет
- Blood Physiology and Circulation, 2011, PGДокумент241 страницаBlood Physiology and Circulation, 2011, PGherphi67% (3)
- Manual Hematological Procedures Frequently Forgotten Concepts and MethodologiesДокумент8 страницManual Hematological Procedures Frequently Forgotten Concepts and MethodologiesWynlor AbarcaОценок пока нет
- Capacity of Hospita101 2Документ45 страницCapacity of Hospita101 2kneou dojolesОценок пока нет
- Fluid Resuscitation and Organ Perfusion EvaluationДокумент66 страницFluid Resuscitation and Organ Perfusion EvaluationDewiRatnasariОценок пока нет
- Fluid Management & Blood Component TherapyДокумент48 страницFluid Management & Blood Component TherapySinta AgustinaОценок пока нет
- Blood TransfusionДокумент5 страницBlood TransfusionMoustafa Hazzaa100% (1)
- Pediatric Hemolytic Uremic Syndrome Case PresentationДокумент29 страницPediatric Hemolytic Uremic Syndrome Case PresentationRupesh MohandasОценок пока нет
- Biology Notes Chpter 10Документ8 страницBiology Notes Chpter 10Wan HasliraОценок пока нет
- Clinical For PracticalДокумент72 страницыClinical For PracticalYogendra SinghОценок пока нет
- Blood GroupДокумент13 страницBlood GroupShanJishmaОценок пока нет
- Test 1 - PSE Model Answers-1Документ3 страницыTest 1 - PSE Model Answers-1Matsiri ImmanuelОценок пока нет
- Hematology 1 (Laboratory) - Week 10-11 ModuleДокумент8 страницHematology 1 (Laboratory) - Week 10-11 ModuleJam RamosОценок пока нет
- 7 Platelet Additive Solutions A Review of The Latest Developments and Their Clinical ImplicationsДокумент5 страниц7 Platelet Additive Solutions A Review of The Latest Developments and Their Clinical ImplicationsVincent ReyesОценок пока нет
- Low hemoglobin and red blood cell countДокумент1 страницаLow hemoglobin and red blood cell countHush PereraОценок пока нет
- Autoimmune Hemolytic AnemiaДокумент55 страницAutoimmune Hemolytic AnemiaNicky SebastianОценок пока нет
- Blood Donar SelectionДокумент16 страницBlood Donar SelectionSiva KeerthanaОценок пока нет
- Guide to Crossmatch Testing PhasesДокумент4 страницыGuide to Crossmatch Testing PhasesEl Marie SalungaОценок пока нет
- Bleeding and Coagulation Time:: 1-Procedure of Duke MethodДокумент2 страницыBleeding and Coagulation Time:: 1-Procedure of Duke MethodAnonymous 59sx7W4Оценок пока нет
- Profil Pemeriksaan Pada Sedimen Urin Pasien Infeksi Saluran Kemih Menggunakan Alat Dirui Fus-100Документ6 страницProfil Pemeriksaan Pada Sedimen Urin Pasien Infeksi Saluran Kemih Menggunakan Alat Dirui Fus-100eko zuliantoОценок пока нет