Академический Документы
Профессиональный Документы
Культура Документы
Endocrine System
Загружено:
mirmodepon050 оценок0% нашли этот документ полезным (0 голосов)
583 просмотров68 страницEndocrine disorders may cause fatigue, weakness, weight change, appetite, sleep patterns, or psychiatric status. DIAGNOSTIC TESTS Total Thyroxine is an accurate index of thyroid function when T4binding globulin is normal. Low plasma-binding protein states (malnutrition, liver disease) may give low values.
Исходное описание:
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документEndocrine disorders may cause fatigue, weakness, weight change, appetite, sleep patterns, or psychiatric status. DIAGNOSTIC TESTS Total Thyroxine is an accurate index of thyroid function when T4binding globulin is normal. Low plasma-binding protein states (malnutrition, liver disease) may give low values.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
583 просмотров68 страницEndocrine System
Загружено:
mirmodepon05Endocrine disorders may cause fatigue, weakness, weight change, appetite, sleep patterns, or psychiatric status. DIAGNOSTIC TESTS Total Thyroxine is an accurate index of thyroid function when T4binding globulin is normal. Low plasma-binding protein states (malnutrition, liver disease) may give low values.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 68
General Effects of Hormone Action
Regulate the overall metabolic rate and the
storage, conversion, and release of energy.
Regulate fluid and electrolyte balance.
Initiate coping responses to stressors.
Regulate growth and development.
Regulate reproduction processes.
ASSESSMENT/HISTORY
Patients with diseases of the endocrine
system commonly report nonspecific
complaints.
Commonly, symptoms may reflect
changes in general well-being, such as
fatigue, weakness, weight change,
appetite, sleep patterns, or psychiatric
status.
PHYSICAL EXAMINATION
Objective findings may be obvious and
related to the patient's complaints or may be
silent signs of which the patient is completely
unaware.
Thorough physical examination of all body
systems, particularly the integumentary,
cardiovascular, and neurologic systems, may
reveal key findings for endocrine dysfunction
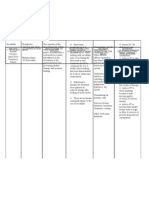
DIAGNOSTIC TESTS
Total Thyroxine
This is a direct measurement of the concentration of
total thyroxine (T4) in the blood, using a
radioimmunoassay technique.
It is an accurate index of thyroid function when T4-
binding globulin (TBG) is normal.
Low plasma-binding protein states (malnutrition,
liver disease) may give low values.
High plasma-binding protein values (pregnancy,
estrogen therapy) may give high values.
It is used to diagnose hypofunction and
hyperfunction of the thyroid and to guide and
evaluate thyroid hormone replacement therapy.
Free Thyroxine
Direct measurement of free T4 concentration in the blood
using a two-step radioimmunoassay method.
Accurate measure of thyroid function independent of the
variable influence of thyroid-binding globulin levels.
Used to aid in the diagnosis of hyperthyroidism and
hypothyroidism.
Used to monitor and guide thyroid hormone replacement
therapy, particularly with pituitary disease.
Thyroid-Binding Globulin
This measures the concentration of the
carrier protein for T4 in the blood.
Because most T4 is protein bound, changes
in TBG will influence values of T4.
Helpful in distinguishing between true
thyroid disease and T4 test abnormalities
caused by TBG excess or deficit.
Triiodothyronine
Directly measures concentration of triiodothyronine
(T3) in the blood using a radioimmunoassay
technique.
T3 is less influenced by alterations in thyroid-binding
proteins.
Useful to rule out T3 thyrotoxicosis, hyperthyroidism
when T4 is normal, and to evaluate effects of thyroid
replacement therapy.
T3 Resin Uptake
This is an indirect measure of thyroid function, based
on the available protein-binding sites in a serum
sample that can bind to radioactive T3.
The radioactive T3 is added to the serum sample in
the test tube and will bind with available protein
binding sites. The unbound T3 is added to resin for
T3 uptake, reflecting the amount of T3 left over
because of lack of binding sites.
Estrogen and pregnancy produce an increase in
binding sites, thus causing a lowered T3 uptake.
Free Thyroid Index
The free thyroid index is a laboratory
estimate of free T4 concentration with
calculated adjustment for variations in
patient's TBG concentration.
Thyrotropin, Thyroid-Stimulating Hormone
Direct measure of TSH, the hormone secreted by
the pituitary gland that regulates the production
and secretion of T4 by the thyroid gland.
Blood sample is analyzed by radioimmunoassay.
Preferred test differentiates between thyroid
disorders caused by disease of the thyroid gland
itself and disorders caused by disease of the
pituitary or hypothalamus.
Thyrotropin-Releasing Hormone Stimulation Test
The thyrotropin-releasing hormone (TRH) stimulation
test evaluates the patency of the pituitary-
hypothalamic axis.
Its primary use is to distinguish between secondary
and tertiary hypothyroidism and evaluate
acromegaly.
A baseline sample is drawn, then TRH is injected I.V.
and blood samples are drawn to determine TSH
levels at 30, 90, and 120 minutes.
Parathyroid Hormone
Test is a direct measurement of parathyroid
hormone (PTH) concentration in the blood,
using radioimmunoassay technique.
Results are usually compared with results of
total serum calcium to determine likely cause
of parathyroid dysfunction.
Range of normal values may vary by
laboratory and method.
Serum Calcium, Total
This is a direct measurement of protein-bound
and free ionized calcium.
Ionized calcium fraction is best indicator of
changes in calcium metabolism.
Results can be affected by changes in serum
albumin, the primary protein carrier.
Used to detect alterations in calcium
metabolism caused by parathyroid disease or
malignancy.
Serum Phosphate
Test measures the level of inorganic
phosphorus in the blood.
Alteration in parathyroid function tends to
have opposite effects on calcium and
phosphorus metabolism.
Used to confirm metabolic abnormalities
that affect calcium metabolism.
Plasma Cortisol
This is direct measure of the primary secretory product
of the adrenal cortex by radioimmunoassay technique.
Serum concentration varies with circadian cycle so
normal values vary with time of day and stress level of
patient (8 a.m. levels typically double that of 8 p.m.
levels).
Useful as an initial step to assess adrenal dysfunction,
but further workup is usually necessary.
24-Hour Urinary Free Cortisol Test
Test measures cortisol production
during a 24-hour period.
Useful to establish diagnosis of
hypercortisolism.
Less influenced by diurnal variations in
cortisol.
Adrenocorticotropic Stimulation Test
ACTH stimulates the production and secretion of
cortisol by the adrenal cortex.
Demonstrates the ability of the adrenal cortex to
respond appropriately to ACTH.
This is an important test to evaluate adrenal
insufficiency, but may not distinguish primary
insufficiency from secondary insufficiency.
Corticotropin Releasing Hormone Stimulation Test
Test measures responsiveness of pituitary gland to
corticotropin-releasing hormone (CRH), a
hypothalamic hormone that regulates pituitary
secretion of ACTH.
Useful to differentiate the cause of excess cortisol
secretion when ectopic source of ACTH is suspected.
Urine Vanillylmandelic Acid and Metanephrine
Direct measure of metabolites of
catecholamines secreted by the adrenal
medulla.
Metanephrine is a more reliable measure of
catecholamine secretion.
Preferred method to diagnose
pheochromocytoma.
Aldosterone (Urine or Blood)
Direct measure, using radioimmunoassay technique,
of aldosterone, a hormone secreted by the adrenal
cortex, which regulates renal control of sodium and
potassium.
May be measured in the blood or in 24-hour urine
collection sample.
Urine test is more reliable because it is less
influenced by short-term fluctuations in the
bloodstream.
Useful to diagnose primary aldosteronism.
Serum Growth Hormone
Direct radioimmunoassay measurement of human
growth hormone (GH), secreted by the anterior
pituitary gland; useful to diagnose acromegaly,
gigantism, pituitary tumors, pituitary-related growth
failure in children or growth hormone deficiency in
adults.
Because GH secretion is episodic, single fasting
samples may not be reliable to detect GH excess or
deficiency.
Serum Prolactin
Direct radioimmunoassay
measurement of prolactin, secreted by
the anterior pituitary gland; helps
diagnose pituitary tumors.
Adrenocorticotropic Hormone
Direct measurement of ACTH concentration
in the bloodstream by radioimmunoassay
technique.
One measure of pituitary gland function
useful to provide important information
regarding adrenal gland dysfunction.
Insulin Tolerance Test
Useful to diagnose functional hypopituitarism
that is caused by pituitary disease or that
appears after pituitary surgery.
Considered the gold standard for diagnosis of
GH deficiency.
Water Deprivation Test
Functional test of the adequacy of
posterior pituitary secretion of antidiuretic
hormone (ADH) and its ability to
concentrate urine and to maintain serum
osmolality in the face of water
deprivation.
Useful to determine the diagnosis and
etiology of diabetes insipidus (DI).
Radioactive 131I Uptake
Measures thyroid uptake patterns of iodine as
a whole or within specified areas of the
gland.
A solution of sodium iodide 131 (131I) is
administered orally to the fasting patient.
After a prescribed interval, usually 24 hours,
measurements of radioactive counts per
minute are taken with a scintillator.
Thyroid Scan
Rapid imaging of thyroid tissue, particularly
suspicious nodules, as contrast imaging
agent is rapidly taken up by functioning
tissue.
Useful to diagnose thyroid carcinoma.
Contrast media is usually administered I.V.
Images can be obtained from gamma
counter within 20 to 60 minutes.
STEROID THERAPY
Steroid therapy is a treatment used in
some endocrine disorders and in
various other conditions. Steroids are
hormones that affect metabolism and
many body processes.
STANDARDS OF CARE GUIDELINES
ENDOCRINE DISORDERS
When caring for a patient with an endocrine
disorder, remember that important metabolic
functions may be disrupted, such as fluid and
electrolyte balance, glucose and protein
metabolism, energy production, calcium
ionization, blood pressure (BP) control,
thermoregulation, cardiac contractility,
intestinal peristalsis, and ability of the body
to react to stress.
INSULIN SECRETION AND FUNCTION
Insulin is a hormone secreted by the beta cells of
the islet of Langerhans in the pancreas.
Small amounts of insulin are released into the
bloodstream in response to changes in blood
glucose levels throughout the day.
Increased secretion or a bolus of insulin, released
after a meal, helps maintain euglycemia.
Through an internal feedback mechanism that involves
the pancreas and the liver, circulating blood glucose
levels are maintained at a normal range of 60 to 110
mg/dL.
Insulin is essential for the utilization of glucose for
cellular metabolism as well as for the proper
metabolism of protein and fat.
-Carbohydrate metabolism - insulin affects the conversion
of glucose into glycogen for storage in the liver and
skeletal muscles, and allows for the immediate release
and utilization of glucose by the cells.
-Protein metabolism - amino acid conversion occurs in the
presence of insulin to replace muscle tissue or to
provide needed glucose (gluconeogenesis).
-Fat metabolism - storage of fat in adipose tissue and
conversion of fatty acids from excess glucose occurs
only in the presence of insulin.
Without insulin, plasma glucose
concentration rises and glycosuria results.
Absolute deficits in insulin result from
decreased production of endogenous
insulin by the beta cell of the pancreas.
Relative deficits in insulin are caused by
inadequate utilization of insulin by the
cell.
Type 1 Diabetes Mellitus
Type 1 diabetes mellitus was formerly known as insulin
dependent diabetes mellitus and juvenile diabetes mellitus.
Little or no endogenous insulin, requiring injections of insulin
to control diabetes and prevent ketoacidosis.
Five to 10% of all diabetic patients have type 1.
Etiology: autoimmunity, viral, and certain histocompatibility
antigens as well as a genetic component.
Usual presentation is rapid with classic symptoms of
polydipsia, polyphagia, polyuria, and weight loss.
Most commonly seen in patients under age 30 but can be
seen in older adults.
Type 2 Diabetes Mellitus
Type 2 diabetes mellitus was formerly known as
noninsulin dependent diabetes mellitus or adult onset
diabetes mellitus.
Caused by a combination of insulin resistance and
relative insulin deficiency.
Approximately 90% of diabetic patients have type 2.
Etiology: strong hereditary component, commonly
associated with obesity.
Usual presentation is slow and typically insidious with
symptoms of fatigue, weight gain, poor wound
healing, and recurrent infection.
Found primarily in adults over age 30; however, may
be seen in younger adults and adolescents who are
overweight.
Prediabetes
Prediabetes is an abnormality in
glucose values intermediate between
normal and overt diabetes.
1. Impaired Fasting Glucose
A new category adopted by the
American Diabetes Association in 1997
and redefined in 2004.
Occurs when fasting blood glucose is
greater than or equal to 100 but less
than 126 mg/dL.
2. Impaired Glucose Tolerance
Defined as blood glucose measurement on a
glucose tolerance test greater than or equal to
140 mg/dl but less than 200 in the 2-hour
sample.
Asymptomatic; it can progress to type 2
diabetes or remain unchanged.
May be a risk factor for the development of
hypertension, coronary heart disease, and
hyperlipidemias.
Gestational Diabetes Mellitus
Gestational diabetes mellitus (GDM) is defined as
carbohydrate intolerance occurring during
pregnancy.
Occurs in approximately 4% of pregnancies and
usually disappears after delivery.
Women with GDM are at higher risk for diabetes at a
later date.
GDM is associated with increased risk of fetal
morbidity.
Screening for GDM for all pregnant women other
than those at lowest risk (under age 25, of normal
body weight, have no family history of diabetes, are
not a member of an ethnic group with high
prevalence of diabetes) should occur between the
24th and 28th weeks of gestation.
Diabetes Associated with Other Conditions
Certain drugs can decrease insulin activity
resulting in hyperglycemia -- corticosteroids,
thiazide diuretics, estrogen, phenytoin.
Disease states affecting the pancreas or
insulin receptors - pancreatitis, cancer of the
pancreas, Cushing's disease or syndrome,
acromegaly, pheochromocytoma, muscular
dystrophy, Huntington's chorea.
DIAGNOSTIC TESTS/ LABORATORY TESTS
Blood Glucose
Fasting blood sugar (FBS), drawn after
at least an 8-hour fast, to evaluate
circulating amounts of glucose;
postprandial test, drawn usually 2
hours after a well-balanced meal, to
evaluate glucose metabolism;
and random glucose, drawn at any
time, nonfasting.
Oral Glucose Tolerance Test
The oral glucose tolerance test (OGTT)
evaluates insulin response to glucose
loading.
FBS is obtained before the ingestion of
a 50- to 200-g glucose load (usual
amount is 75 g), and blood samples are
drawn at ½, 1, 2, and 3 hours (may be
4- or 5-hour sampling).
GENERAL
PROCEDURES AND
TREATMENT MODALITIES
BLOOD GLUCOSE MONITORING
Accurate determination of capillary blood
glucose assists patients in the control and
daily management of diabetes mellitus.
Blood glucose monitoring helps evaluate
effectiveness of medication; reflects
glucose excursion after meals; assesses
glucose response to exercise regimen; and
assists in the evaluation of episodes of
hypoglycemia and hyperglycemia to
determine appropriate treatment.
INSULIN THERAPY
Insulin therapy involves the subcutaneous
injection of immediate-, short-, intermediate-,
or long-acting insulin at various times to
achieve the desired effect.
Short-acting regular insulin can also be given
I.V.
NPH Only (Neutral Protamine Hagedorn)
Used alone only in type 2 diabetes when patients are
capable of producing some exogenous insulin as a
supplement for better glucose control.
NPH can also be given twice daily (morning and
bedtime) to eliminate afternoon hypoglycemia yet
provide nighttime coverage.
NPH/Regular or NPH/Lispro
Short-acting regular insulin or immediate-acting lispro
(Humalog) or aspart (Novolog) insulin is added to NPH to
promote postprandial glucose control
Short- or immediate-acting insulin added to morning NPH
controls glucose elevations after breakfast.
Increased blood glucose levels after supper can be controlled
by the addition of short- or immediate-acting insulin before
supper.
Intensive Insulin Therapy
Designed to mimic the body's normal insulin
responses to glucose.
Uses multiple daily injections of insulin.
NPH or ultralente or glargine (Lantus) insulin is
used for basal insulin control.
Regular insulin acts as a premeal bolus given 30
minutes before each meal. Lispro or aspart insulin
may be used instead of regular and is taken just
before eating.
24-hour insulin coverage designed in this way can
be flexible to accommodate mealtimes and
physical activity.
Combination Oral Agent and Insulin Therapy
Appropriate only in type 2 diabetes.
Intermediate-acting insulin (NPH) is given in the
evening and an oral sulfonylurea agent in the
morning called BIDS therapy (Bedtime Insulin,
Daytime Sulfonylurea).
Combination therapy may also include the use of
a thiazolidinedione (pioglitazone [Actos],
rosiglitazone [Avandia]), metformin (Glucophage),
or other agents.
DIABETES MELLITUS
Diabetes mellitus is a metabolic
disorder characterized by
hyperglycemia and results from
defective insulin production, secretion,
or utilization.
Onset is abrupt with type 1 and insidious with
type 2.
1. Hyperglycemia
Weight loss, fatigue
Polyuria, polydipsia, polyphagia
Blurred vision
2. Altered Tissue Response
Poor wound healing
Recurrent infections, particularly of the skin
1. Diet
Dietary control with caloric restriction
of carbohydrates and saturated fats to
maintain ideal body weight.
The goal of meal planning is to control
blood glucose and lipid levels
2. Exercise
Regularly scheduled, moderate exercise
performed for at least 30 minutes most days
of the week promotes the utilization of
carbohydrates, assists with weight control,
enhances the action of insulin, and improves
cardiovascular fitness.
3. Medication
Oral antidiabetic agents for patients with type
2 diabetes who do not achieve glucose
control with diet and exercise only
Complications
Hypoglycemia occurs as a result of an imbalance in food,
activity, and insulin/oral antidiabetic agent.
Diabetic ketoacidosis (DKA) occurs primarily in type 1
diabetes during times of severe insulin deficiency or
illness, producing severe hyperglycemia, ketonuria,
dehydration, and acidosis.
Hyperosmolar hyperglycemic nonketotic syndrome
(HHNKS) affects patients with type 2 diabetes, causing
severe dehydration, hyperglycemia, hyperosmolarity,
and stupor.
Nursing Diagnoses
Imbalanced Nutrition: More than Body Requirements
related to intake in excess of activity expenditures
Fear related to insulin injection
Risk for Injury (hypoglycemia) related to effects of
insulin, inability to eat
Activity Intolerance related to poor glucose control
Deficient Knowledge related to use of oral hypoglycemic
agents
Risk for Impaired Skin Integrity related to decreased
sensation and circulation to lower extremities
Ineffective Coping related to chronic disease and
complex self-care regimen
Teaching About Insulin – avoiding
lipodystrophy
Assess patient for the signs and symptoms of
hypoglycemia.
Treat hypoglycemia promptly with 15 to 20 g
of fast-acting carbohydrates.
- Half cup (4 oz) juice, 1 cup skim milk, three
glucose tablets, four sugar cubes, five to six
pieces of hard candy may be taken orally.
Encourage patient to carry a portable
treatment for hypoglycemia at all times.
Between-meal snacks as well as extra
food taken before exercise should be
encouraged to prevent hypoglycemia.
Encourage patients to wear an
identification bracelet or card that may
assist in prompt treatment in a
hypoglycemic emergency.
Assess feet and legs for skin temperature, sensation,
soft tissue injuries, corns, calluses, dryness, hammer
toe or bunion deformation, hair distribution, pulses,
deep tendon reflexes.
Use heel protectors, special mattresses, foot cradles for
patients on bed rest.
Avoid applying drying agents to skin (eg, alcohol).
Apply skin moisturizers to maintain suppleness and
prevent cracking and fissures.
Advise the patient who smokes to stop
smoking or reduce if possible, to
reduce vasoconstriction and enhance
peripheral blood flow.
THE END
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Cardiac Dysrhythmia Chart Med-Surg NUR4Документ3 страницыCardiac Dysrhythmia Chart Med-Surg NUR4ktfosterfd2096% (96)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Pathophysiology Test Bank CH 6-9Документ33 страницыPathophysiology Test Bank CH 6-9Joyy86% (7)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Case Study of Alcohol DependenceДокумент31 страницаCase Study of Alcohol Dependenceilakkiya ilakkiya100% (8)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Sicle Cell Concept MapДокумент1 страницаSicle Cell Concept MapRosa100% (1)
- NCM104 - Midterms Recovered)Документ12 страницNCM104 - Midterms Recovered)mirmodepon05Оценок пока нет
- Integumentary SystemДокумент66 страницIntegumentary Systemmirmodepon05Оценок пока нет
- Renal and Urinary DisordersДокумент134 страницыRenal and Urinary Disordersmirmodepon05100% (1)
- Understanding Cancer - PPT LectureДокумент169 страницUnderstanding Cancer - PPT Lecturemirmodepon05100% (15)
- Caso Clinico 5Документ5 страницCaso Clinico 5Manuel IbarraОценок пока нет
- KROK2 2010 Paper (200Qs)Документ62 страницыKROK2 2010 Paper (200Qs)Ali Zeeshan100% (1)
- 2023 Bai Use of Albumin Infusion For Cirrhosis Related Complications An International Position StatementДокумент16 страниц2023 Bai Use of Albumin Infusion For Cirrhosis Related Complications An International Position StatementFranc DechiaОценок пока нет
- Apendicitis CrnicaДокумент5 страницApendicitis CrnicaJefferson JCОценок пока нет
- NatPro - Isolation of Flavonoids From The Fruits of Cornus Kousa BurgДокумент19 страницNatPro - Isolation of Flavonoids From The Fruits of Cornus Kousa BurgCassandraMillsОценок пока нет
- Vazirani-Akinosi TechniqueДокумент9 страницVazirani-Akinosi TechniqueChelo Jan GeronimoОценок пока нет
- Information 1Документ2 страницыInformation 1Nazish RafiqueОценок пока нет
- Pharmacology SlidesДокумент114 страницPharmacology Slidesbrandon15000100% (9)
- USMLE Flashcards: Biochemistry - Side by SideДокумент137 страницUSMLE Flashcards: Biochemistry - Side by SideMedSchoolStuffОценок пока нет
- Strangles and GlandersДокумент26 страницStrangles and Glandersanil regmiОценок пока нет
- Gastro MCQsДокумент14 страницGastro MCQsvaegmundigОценок пока нет
- Practice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenДокумент35 страницPractice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenMelodia Turqueza GandezaОценок пока нет
- Canine Distemper: Hard Pad Disease, Canine InfluenzaДокумент11 страницCanine Distemper: Hard Pad Disease, Canine InfluenzaDr-Hassan SaeedОценок пока нет
- Drug Study CHDCДокумент1 страницаDrug Study CHDCIannBlancoОценок пока нет
- Symptoms PDFДокумент3 страницыSymptoms PDFVita AmiliaОценок пока нет
- AlzheimerДокумент1 страницаAlzheimerZeti HusseinОценок пока нет
- Ent Notes For PGДокумент12 страницEnt Notes For PGSHAKEEL1991Оценок пока нет
- Case Study on Residual SchizophreniaДокумент37 страницCase Study on Residual SchizophreniaKevin AlonzoОценок пока нет
- Extracts From More Energy & Less Disease With Vitamin C and MSMДокумент5 страницExtracts From More Energy & Less Disease With Vitamin C and MSMromalfioОценок пока нет
- Searching The Evidence (PDL - Fadel Fikri Suharto)Документ7 страницSearching The Evidence (PDL - Fadel Fikri Suharto)IPD Unsri JAN 21Оценок пока нет
- Lofnac Suppo Diclofenac Sodium Tablets 100MG PilДокумент7 страницLofnac Suppo Diclofenac Sodium Tablets 100MG PilepakerryОценок пока нет
- Antepartum Hemorrhage Causes and TypesДокумент25 страницAntepartum Hemorrhage Causes and TypesdeangamaОценок пока нет
- Complications After Heart Transplantation - Hope For The Best, But Prepare For The WorstДокумент11 страницComplications After Heart Transplantation - Hope For The Best, But Prepare For The WorstJorge AlvarezОценок пока нет
- Lumbar PunctureДокумент6 страницLumbar PunctureMitkoОценок пока нет
- Dengue and Chikungunya Infections in ChildrenДокумент9 страницDengue and Chikungunya Infections in ChildrenAl-Harits OctaОценок пока нет
- HES 005 P2 Coverage and Drug Study GuideДокумент4 страницыHES 005 P2 Coverage and Drug Study GuideXander Jake Asturias TangcalaganОценок пока нет