Академический Документы
Профессиональный Документы
Культура Документы
Antidepressant Drugs
Загружено:
Ojambo FlaviaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Antidepressant Drugs
Загружено:
Ojambo FlaviaАвторское право:
Доступные форматы
Antidepressants drugs
Pharmacology
Department
Lecturer Genny Dominguez
BIBLIOGRAPHY
Goodman and Gilmans. The
pharmacological basis of therapeutics.
Basic and Clinical Pharmacology. Bertram
G. Katzung.
Pharmacology. H. P Rang, M. M. Dale, J.
M. Ritter, P. K. Moore.
Pharmacology. 3rd edition. Lippincotts.
SUMMARY
Antidepressants.
1. Tricyclic antidepressants.
2. Selective serotonin
reuptake inhibitors.
3. Serotonin/Norepinephrine
reuptake inhibitors.
4. Monoamine oxidase
inhibitors.
5. Atypical antidepressants.
It is the most common of the affective
disorders.
It may range from a very mild condition,
bordering on normality, to severe
(psychotic).
Its a major cause of disability and
premature death.
In addition to the significant suicide risk,
depressed individuals are more likely to die
from other causes, such as heart disease or
cancer.
Depression
Depression
Emotional symptoms:
Misery, apathy, and
pessimism, hopelessness.
Low self esteem.
Feelings of guilt, inadequacy
and ugliness.
Indecisiveness and loss of
motivation.
Biological symptoms:
Retardation of thought and
action.
Loss of libido.
Sleep disturbance and loss of
appetite.
Depression
The clinical syndromes are:
Unipolar depression:
Reactive depression
Endogenous depression.
Bipolar depression:
Manic depressive psychosis.
Monoamine theory for depression
Theory: Reduced monoamine transmission
(NA &/or 5HT) causes depression.
Evidence
Reserpine, which depletes neuronal monoamine
stores, causes depression.
Methyldopa, which reduces CNS NA release,
causes depression.
Note: Measurements of monoamine levels do
not clearly support the hypothesis.
Drugs which enhance monoamine transmission
improve depression.
Processes to remaind
The release of a monoamine
neurotransmitter from a nerve terminal.
Inhibition of transmitter release by an
inhibitory pre-synaptic receptor.
Elimination of neurotransmitter from the
synaptic cleft by:
a high affinity reuptake mechanism.
A low affinity reuptake mechanism.
Passive diffusion.
Release of Noradrenaline
1
-adrenoceptor
NA
NA
- NA is released in response to
depolarization of sympathetic
nerves.
- NA activates
1
-adrenoceptors
of the target tissue.
Release of Noradrenaline
1
-adrenoceptor
NA
NA
2
-adrenoceptor
_
- NA also activates
2
-
adrenoceptors of the
nerve terminal.
-
2
-adrenoceptors inhibit
release of NA.
- This a negative feed-
back system.
NOTE: THIS NOT A
SYSTEM FOR THE RE-
UPTAKE OF NA
Re-uptake of Noradrenaline
1
-adrenoceptor
NA
NA
NA
Uptake 1
Uptake 2
- NA is released in large
amounts from sympathetic
nerves, and requires to be
cleared from the synapse by
two uptake systems and by
diffusion in the circulation:
Uptake 1: is a high affinity, low
capacity system that permits
NA uptake by the nerve
terminal.
Uptake 2: is a low affinity, high
capacity system that permits
NA uptake into the target
tissue.
Noradrenaline Reuptake 1 Inhibitors
1
-adrenoceptor
NA
NA
NA
Uptake 1
Uptake 2
Anti-depressants are widely
used in medicine, and include
drugs such as amitriptyline
They stimulate nor-adrenergic
transmission within the CNS by
inhibiting the uptake 1 system,
which increases the synaptic
concentration of NA.
Amitriptyline
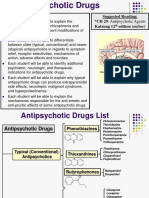
Antidepressants groups
Tricyclic antidepressants (TCAs).
Serotonin-selective reuptake inhibitors
(SSRIs).
Serotonin/Norepinephrine reuptake
inhibitors (SNRIs).
Non-selective MAOIs.
Atypical antidepressants.
Tricyclic antidepressants
(TCAs)
Tertiary amines:
Amitriptyline
Imipramine
Clomipramine
Doxepin
Trimipramine
Secondary amines:
Desipramine
Nortriptyline
Amoxapine
Aprotiline
Protriptyline
Tricyclic antidepressants
Amitriptyline, imipramine, clomipramine are non-
selective inhibitors of both NA and 5HT.
Nortriptyline is moderately selective for NA.
Onset of antidepressant effect in 2-4 weeks, whereas
the receptor blocking effects are immediate.
Effective against unipolar depression, both reactive and
endogenous.
The drugs are taken orally and have a T1/2 of 10-20 h.
They are best suited to the treatment of mild or
moderate depression.
In overdose, these drugs are hazardous.
TCAs are also inhibitors of:
Muscarinic cholinergic receptors:
Dry mouth, mydriasis, blurred vision, tachycardia,
constipation, urinary retention.
Histamine H
1
receptors:
Sedation may help disturbed sleep if taken at night.
Cardiac K
+
channels:
In overdose, these drugs may cause life-threatening
ventricular arrhythmias.
Tricyclic antidepressants provide effective treatment for
neuropathic pain (results from damage to or dysfunction of
the peripheral or CNS, rather than stimulation of pain
receptors).
TCAs actions
Elevate mood (the onset is slow 2 weeks).
Improve mental alertness.
Increase physical activity.
Reduce morbid preocupation in individual with major
depression.
Physical and psychological dependence (should be
slowly withdrawal).
Can be used for prolonged treatment of depression.
TCAs therapeutic uses.
Severe major depression.
Panic disorders.
To control bed-wetting in
children (older than 6
years) by causing
contraction of the internal
sphincter of bladder.
Chronic pain (neuropathic
pain) amitriptyline.
PANIC
TCAs ADR
Antimuscarinic effects: Blurred vision,
Xerostomia (dry mouth), Urinary
retention, Constipation, Aggravation of
glaucoma and epilepsy.
Increased catecholamine activity:
Cardiac over stimulation (overdose).
Block adrenergic receptor: Orthostatic
hypotension and reflex tachycardia.
Block histamine H
1
receptors: Sedation.
Weight gain.
Sexual dysfunctions (erectile
dysfunction in men, anorgasmia in
women).
TCAs interactions
TCA
Direct-acting
Adrenergic
drugs
MAOI
Indirect-acting
Adrenergic drugs
Ethanol
CNS depressants
Toxic sedation
Mutual enhancement:
Hypertension
Hyperpyrexia
Convulsions
Coma
Block effects of
indirect-acting
symphatomimetic
drugs.
Potentiate effects of
biogenic amine drugs
by preventing their
removal from the
synaptic cleft.
TCAs Precautions
Should be used with caution in manic-
depressive patients, because they may
unmask maniac behaviour.
They have narrow therapeutic index: 5 to 6
fold the maximal daily dose of imipramine can
be lethal.
Serotonin-selective reuptake
inhibitors (SSRIs)
These drugs include fluoxetine, paroxetine, sertraline,
citalopram, escitalopram and fluvoxamine.
They are highly selective for 5HT reuptake.
They are taken orally and have a very long half life
(>24h).
SSRIs cause less anti-muscarinic effects than tricyclic
antidepressants.
They are much safer than tricyclic antidepressants in
overdose.
They appear to cause an increased suicidal risk in
children and teenagers, and so are avoided in these
groups.
SSRIs
The onset of the
antidepressant effect takes 2-4
weeks.
Maximum benefit may require
twelve weeks or more.
3 months
2 weeks
SSRIs Therapeutic uses.
They are effective in a variety of
psychiatric disorders:
Depression.
Obsessive-compulsive disorder (the
only indication of fluvoxamine).
Panic attacks.
Anxiety.
Premenstrual dysphoric disorder.
Bulimia nervosa.
SSRIs
Fluoxetine: Longer half-life (fifty hours).
Fluoxetine and paroxetine are inhibitors of the cytochrome
P450 responsible for the elimination of TCA, neuroleptics,
antiarrythmics and -adrenergic antagonist drugs.
Renal excretion, except paroxetine and sertraline (fecal).
Hepatic impairment (dosages should be adjusted).
SSRIs Adverse effects
They have fewer and less severe adverse effects than the
TCA and MAOIs.
GI effects: Nausea and diarrhoea.
Anxiety.
Weakness.
Sleep disturbances: Drowsiness, insomnia; Paroxetine and
fluvoxamine are sedating, may be useful in patient who have
difficulty sleeping.
Sexual dysfunction: Loss of libido, delayed ejaculation and
anorgasmia, if the SSRIs induce sexual dysfunction should
be replaced by bupropion or mirtazapine.
Rarely, SSRIs may precipitate aggressive or violent
behaviour.
SSRIs, Overdoses and interactions.
Fluoxetine: Seizures.
In combination with MAOIs, they may
cause the serotonin syndrome, which
comprises, tremor, hyperthermia and
cardiovascular collapse.
Serotonin/Norepinephrine
reuptake inhibitors (SNRIs)
These drugs inhibit the reuptake of both
serotonin and norepinephrine.
They include:
Duloxetine
Venlafaxine
SNRIs
May be effective in treating depression
in patients in which SSRIs are
ineffective.
Effective in depression accompanied by
chronic painful symptoms (neuropathic
pain), backache and muscle aches, this
pain is in part modulated by serotonin
and norephinephrine in the CNS.
Venlafaxine is used mainly in the
elderly. It is less sedative and has
fewer antimuscarinic effects than the
tricyclic antidepressants.
SSRIs
Monoamine oxidase
Monoamines are eliminated by enzymatic
degradation.
There are two principle enzymes:
Monoamine oxidase (MAO).
Catechol-O-methyltransferase (COMT).
There are two MAO isoenzymes:
MAO-A
MAO-B
The two enzymes have a different distribution
within the body:
MAO-A is found in the CNS, liver and gut wall.
MAO-B is found in the CNS alone.
Monoamine oxidase and its inhibitors
There are differences in the substrate
specificity of MAO-A and MAO-B:
MAO-A oxidises NA, 5HT, dopamine and
tyramine.
MAO-B oxidises dopamine and tyramine.
Inhibitors of monoamine oxidase divide into
two groups:
Non-selective MAO inhibitors (used in
depression).
MAO-B inhibitors (used in Parkinsons disease).
Non-selective MAO inhibitors
Non-selective MAOIs cause a rapid and
sustained increase in the CNS
concentration of NA, 5HT and dopamine.
They are very effective for the rapid
control of severe depression.
They are generally long lasting, due to the
irreversible inhibition of MAO.
They should not be given together with
tricyclic antidepressants or SSRIs.
Adverse effects of non-selective MAOIs
Adverse effects include:
Postural hypotension.
Atropine-like effects (antimuscarinic).
Weight gain.
Restlessness and insomnia.
Liver damage (rare, but MAOIs are avoided in
patients with abnormal LFTs).
In addition, non-selective MAOIs may cause severe
hypertension in the presence of tyramine-containing
foods. This is the cheese reaction.
The effect of tyramine on noradrenergic
transmission
1
-adrenoceptor
NA
Tyr
Uptake 1
Tyramine (from food) enters
peripheral adrenergic nerves via
the uptake 1 system. It is taken up
into vesicles, where it displaces NA
into the cytosol.
Cytosolic NA may then leak out of
the nerve via the uptake 1 system,
and activate post-synaptic
receptors.
Tyramine is normally destroyed by
MAO-A in the gut wall and liver.
NA
Tyramine
Uptake 1
The cheese reaction
Tyramine is a product of bacterial fermentation, and is
found in foods where such a reaction occurs (some beers
and wines, soft cheeses, and aged or cure meats, etc).
Tyramine is a substrate for both MAO-A and MAO-B, but as
tyramine does not cross the blood-brain barrier, its effects
are produced only by peripheral MAO-A.
Patients who ingest tyramine while taking non-selective
MAOIs, may develop life-threatening hypertension.
A dangerous hypertensive reaction can occur by a similar
mechanism in patients taking both non-selective MAOIs and
ephedrine or amphetamine.
Note: MAO-B inhibitors, which are used in Parkinsons
disease, do not produce a cheese reaction. They selectively
increase the neuronal dopamine concentration.
Non-selective MAOIs
Drugs in this class (irreversible non-selective
inhibitors of MAO) include:
Phenelzine
Tranylcypromine
Isocarboxazid
There is a reversible non-selective inhibitor of
MAO moclobemide.
Moclobemide appears to cause less severe cheese
reactions, but tyramine containing food is still best
avoided.
The less severe cheese reaction is probably related to
the less sustained inhibition of the enzyme.
Non-selective MAO Inhibitors
The use of these drugs is limited due to the
complicated dietary restrictions required of
patients taking MAOIs.
Non-selective MAOIs therapeutic
uses
Depressed patients who are
unresponsive or allergic to
TCAs or who experience
strong anxiety.
Low psychomotor activity
(have mild stimulant effect).
Phobic states.
Atypical depression: Labile
mood, rejection sensitivity,
and appetite disorders.
TCAs
Non-selective MAOIs
Antidepressant effects
required 2-4 weeks of
treatment.
The enzymatic
regeneration when is
irreversibly inactivate
occurs several weeks
after termination of
the drug.
2- 4 weeks
Non-selective MAOIs ADR
Severe and unpredictable effects.
Patients that ingest tyramine-contained foods,
causes the release of large amounts of
catecholamines (tachycardia, headache, nausea,
hypertension, cardiac arrhythmias and stroke)
because the tyramine normally is inactivated by
MAO in the gut. Phentolamine and prazosin are
helpful in the management of tyramine-induced
hypertension.
May be dangerous in severely depressed patients
with suicidal tendencies.
Drowsiness, orthostatic hypotension, blurred
vision, dry mouth, dysuria and constipation.
Should not be coadministered with SSRIs
(serotonin syndrome) (six weeks before).
SSRI MAOI
Atypical antidepressants
They are not more
efficacious than the
TCAs or SSRIs.
Bupropion
Mirtazapine
Nefazodone
Trazodone
Atypical antidepressants
Bupropion:
Extended release formulation.
Is unique in that it decreases the
craving for nicotine in tobacco
abusers.
ADR: Dry mouth, sweating,
tremor, and seizures at high
doses.
Atypical antidepressants
Mirtazapine:
Block 5-HT
2
and
2
receptors.
Antihistaminic activity
(sedative) may be
used in depressed
patients having
difficulty sleeping.
Increased appetite
and weight gain.
Atypical antidepressants
Nefazodone and trazodone:
Inhibitors of the serotonin reuptake, block the
5-HT
1
presynaptic autoreceptors and increase
serotonin release.
Block H
1
activity (sedating).
Cause priapism.
Other antidepressant drugs
Flupenthixol (a neuroleptic) has anti-depressant
effects, and is used in depression at low doses.
Reboxetine, a selective inhibitor on NA reuptake.
Tryptophan, the amino acid precursor of 5HT,
may be used as adjunctive therapy.
St Johns wort (a plant extract). It contains
hyperformin, a monoamine transport inhibitor. It
is a potent inducer of cytochrome P
450
, and will
interact with the metabolism of many other
drugs.
P450 interactions the critical list
The plasma concentration of many drugs may be
affected by drugs that induce or inhibit cytochrome P
450
.
Do not forget the following critical list is drugs whose
metabolism may be altered by P
450
inducers or inhibitors
Warfarin
Anticonvulsants (phenytoin, carbamazepine, others)
Anti-AIDS drugs
Protease inhibitors
Non-nucleoside RT inhibitors
Cyclosporine A
Oral contraceptives
Sedating, useful
for agitation
GI
distress
Orthostatic
hypotension
Weight
gain
SSRIs Citalopram - + - -
Escitalopram - + - -
Fluoxetine - + - -
Fluvoxamine + + - -
Paroxetine + + - -
Sertraline - + - -
SNRIs Venlafaxine - + - -
Duloxetine - + - -
Atypicalantidepressants Bupropion - - - -
Mirtazapine + - - +
Nefazodone + + - -
Trazodone + - - -
TCA Amitriptyline + - + +
Amoxapine + - - -
Clomipramine + + - +
Desipramine - - - -
Doxepin + - + +
Imipramine + - - +
Maprotiline + - - -
Nortriptyline + - - -
Potriptyline - - - -
Trimipramine + - - +
MAOI Phenelzine - - + -
Tranylcypromine - - + -
Вам также может понравиться
- Psychiatry Practice Boosters 2016: Insights from research to enhance your clinical workОт EverandPsychiatry Practice Boosters 2016: Insights from research to enhance your clinical workОценок пока нет
- Antidepressant DrugsДокумент41 страницаAntidepressant DrugsSashaKay100% (5)
- AntidepressantsДокумент4 страницыAntidepressantsSalman HabeebОценок пока нет
- AntidepressantsДокумент12 страницAntidepressantsSubiVictorОценок пока нет
- Anti PsychoticsДокумент34 страницыAnti Psychotics88AKKОценок пока нет
- AntidepressantsДокумент33 страницыAntidepressantsAde Habibie100% (1)
- Anti Depressants FinalДокумент61 страницаAnti Depressants FinalAuthor Nauman Shad100% (1)
- Mental Health and Psychiatric Nursing: Vernalin B. Terrado, RNДокумент35 страницMental Health and Psychiatric Nursing: Vernalin B. Terrado, RNverna100% (1)
- Antidepressant DrugsДокумент21 страницаAntidepressant DrugsKashis SharmaОценок пока нет
- Antidepressant Drugs: Presented By-K.Vinod Dept. of PharmacologyДокумент38 страницAntidepressant Drugs: Presented By-K.Vinod Dept. of PharmacologyVinod GuruОценок пока нет
- Antidepressants AntidepressantsДокумент38 страницAntidepressants AntidepressantsjaneОценок пока нет
- PsychopharmacologyДокумент50 страницPsychopharmacologyapi-3703352Оценок пока нет
- Handbook of Psychiatric DrugsДокумент68 страницHandbook of Psychiatric Drugsbson100% (13)
- Antipsychotic DrugsДокумент44 страницыAntipsychotic DrugsPaulus Widjanarko Brotosaputro0% (1)
- PsychopharmacologyДокумент32 страницыPsychopharmacologyCms CSU100% (1)
- NeurotransmittersДокумент5 страницNeurotransmittersJoezerk Jhon Biel100% (1)
- NeurotransmittersДокумент29 страницNeurotransmittersashupathakaОценок пока нет
- B2B Psychopharmacology 2015Документ128 страницB2B Psychopharmacology 2015Soleil DaddouОценок пока нет
- SchizophreniaДокумент58 страницSchizophreniaArpit AroraОценок пока нет
- Pathophysiology of DepressionДокумент10 страницPathophysiology of DepressionPrashant ChettriОценок пока нет
- PsychopharmacologyДокумент148 страницPsychopharmacologyAsther Mantua100% (2)
- Antipsychotic Drugs: (Neuroleptics, Major Tranquillizer Ataractic)Документ63 страницыAntipsychotic Drugs: (Neuroleptics, Major Tranquillizer Ataractic)Muhammad Masoom Akhtar100% (1)
- Antipsychotic DrugsДокумент3 страницыAntipsychotic DrugsArtt1975Оценок пока нет
- AntidepressantsДокумент31 страницаAntidepressantsIzhaan AkmalОценок пока нет
- Soumya Mary 1 Year MSC (N)Документ24 страницыSoumya Mary 1 Year MSC (N)Salman HabeebОценок пока нет
- Anxiety DisorderДокумент23 страницыAnxiety DisorderOliver Miguel ChavezОценок пока нет
- AntipsychoticsДокумент51 страницаAntipsychoticsShailja SharmaОценок пока нет
- Drugs in Psychiatric NursingДокумент38 страницDrugs in Psychiatric NursingJSeasharkОценок пока нет
- Drugs Used in Mental IllnessДокумент60 страницDrugs Used in Mental IllnessDixa MeОценок пока нет
- Psychopharmacology in PsychiatryДокумент94 страницыPsychopharmacology in PsychiatryOslo SaputraОценок пока нет
- Neurotransmitters-Classification, Relevance in The Etiology and Treatment of Mental IllnessДокумент22 страницыNeurotransmitters-Classification, Relevance in The Etiology and Treatment of Mental Illnessneethus10Оценок пока нет
- Mood Disorders: Depressive Disorders: Bipolar DisordersДокумент4 страницыMood Disorders: Depressive Disorders: Bipolar DisordersWen Jie LauОценок пока нет
- Presented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Документ17 страницPresented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Akanksha KapoorОценок пока нет
- Antipsychotic DrugsДокумент47 страницAntipsychotic DrugsIkram UddinОценок пока нет
- Lecture 4, Antipsychotics, AntidepressantsДокумент94 страницыLecture 4, Antipsychotics, Antidepressantsj.doe.hex_87100% (3)
- Case Study Presentation On Catatonic SchizophreniaДокумент7 страницCase Study Presentation On Catatonic Schizophreniadinesh100% (1)
- Psycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsДокумент29 страницPsycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsPoonam RanaОценок пока нет
- Antidepressant DrugsДокумент11 страницAntidepressant DrugsDedy SantosoОценок пока нет
- SchizophreniaДокумент22 страницыSchizophrenianabeelОценок пока нет
- First Rank Symptoms of SchizophreniaДокумент65 страницFirst Rank Symptoms of Schizophreniadrkadiyala2Оценок пока нет
- Syndrome in PsychiatryДокумент12 страницSyndrome in Psychiatryrahul KumarОценок пока нет
- Sedative-Hypnotic Drugs: Anita Q. Sangalang, MD, FPOGSДокумент43 страницыSedative-Hypnotic Drugs: Anita Q. Sangalang, MD, FPOGSdave_1128Оценок пока нет
- Quiz PsychopharmacologyДокумент1 страницаQuiz PsychopharmacologySolsona Natl HS MaanantengОценок пока нет
- Current Clinical Strategies: Handbook of Psychiatric DrugsДокумент72 страницыCurrent Clinical Strategies: Handbook of Psychiatric Drugsmike116Оценок пока нет
- Psychiatry NotesДокумент123 страницыPsychiatry NotesKyoheirwe vanessaОценок пока нет
- Common Psychiatric TermsДокумент6 страницCommon Psychiatric TermsKatrina Heart Rauto AvilaОценок пока нет
- Treatment Modalities For Mood DisordersДокумент55 страницTreatment Modalities For Mood DisordersGlory MimiОценок пока нет
- Bms166 Slide Antipsychotic AntidepressantДокумент52 страницыBms166 Slide Antipsychotic AntidepressantErmanto D'PhytoxzОценок пока нет
- NeurosisДокумент11 страницNeurosisSharika sasiОценок пока нет
- Psychotic DisordersДокумент38 страницPsychotic DisordersMala Rasaily100% (2)
- Reviewer On PsychopharmacologyДокумент28 страницReviewer On PsychopharmacologyKristine Ann Hernandez100% (1)
- ANTIPSYCHOTICSДокумент25 страницANTIPSYCHOTICSCheetahboi Shopee100% (4)
- Psychiatric Nursing: Lecturer: Roselily Coquilla, RNДокумент79 страницPsychiatric Nursing: Lecturer: Roselily Coquilla, RNRoselily Flores Coquilla100% (1)
- Antidepressants: I. Cyclic AntidepressantДокумент17 страницAntidepressants: I. Cyclic AntidepressantVaibhav KrishnaОценок пока нет
- Anxiolytics & HypnosedativesДокумент18 страницAnxiolytics & Hypnosedativesrey martino100% (1)
- AntipsychoticsДокумент29 страницAntipsychoticsTyler Lawrence Coye100% (5)
- PSYCHOPHARMACOLOGY HndoutДокумент12 страницPSYCHOPHARMACOLOGY HndoutMhae TabasaОценок пока нет
- Nicotine Related DisordersДокумент74 страницыNicotine Related DisordersKuldeep singhОценок пока нет
- Neurotransmitters AVДокумент5 страницNeurotransmitters AVDr. Hashibu SsekweyamaОценок пока нет
- Chapter 21 Antidepressant AgentsДокумент4 страницыChapter 21 Antidepressant AgentsNicolle Lisay IlaganОценок пока нет
- Macrocytic Anemia May Be Classified As MegaloblasticДокумент5 страницMacrocytic Anemia May Be Classified As MegaloblasticOjambo FlaviaОценок пока нет
- Acute Renal FailureДокумент31 страницаAcute Renal FailureOjambo FlaviaОценок пока нет
- Antenatal CareДокумент22 страницыAntenatal CareOjambo Flavia100% (1)
- Hepatitis BДокумент10 страницHepatitis BOjambo FlaviaОценок пока нет
- Information From MicrographsДокумент4 страницыInformation From MicrographsOjambo FlaviaОценок пока нет
- Lecture - 1 Hematological StainingДокумент20 страницLecture - 1 Hematological StainingOjambo FlaviaОценок пока нет
- Genital UlcersДокумент4 страницыGenital UlcersOjambo FlaviaОценок пока нет
- Antepartum HaemorrhageДокумент18 страницAntepartum HaemorrhageOjambo Flavia100% (1)
- Taking A Gynaecological HistoryДокумент20 страницTaking A Gynaecological HistoryOjambo FlaviaОценок пока нет
- Malaria in PregnancyДокумент19 страницMalaria in PregnancyOjambo FlaviaОценок пока нет
- Billiary DiseaseДокумент13 страницBilliary DiseaseOjambo FlaviaОценок пока нет
- Ante-Partum HaemorrhageДокумент15 страницAnte-Partum HaemorrhageOjambo FlaviaОценок пока нет
- Prescription WritingДокумент30 страницPrescription WritingOjambo FlaviaОценок пока нет
- Dr. Odawa - Anaemia in Pregnancy OdwДокумент33 страницыDr. Odawa - Anaemia in Pregnancy OdwOjambo Flavia100% (1)
- Managing A Patient in CastДокумент79 страницManaging A Patient in Castagentlara28Оценок пока нет
- Management of Anaemia in PregnancyДокумент22 страницыManagement of Anaemia in PregnancyOjambo FlaviaОценок пока нет
- Antenatal CareДокумент13 страницAntenatal CareOjambo Flavia50% (2)
- Salicylate & Paracetamol PoisoningДокумент13 страницSalicylate & Paracetamol PoisoningOjambo FlaviaОценок пока нет
- Dysregulation of Calcium Homeostasis After Severe Burn Injury in ChildrenДокумент2 страницыDysregulation of Calcium Homeostasis After Severe Burn Injury in ChildrenOjambo FlaviaОценок пока нет
- 5 3 Obstetrical Emergency MДокумент74 страницы5 3 Obstetrical Emergency MOjambo FlaviaОценок пока нет
- Basic Principles of MS InjuriesДокумент40 страницBasic Principles of MS InjuriesOjambo FlaviaОценок пока нет
- Asepsis NotesДокумент39 страницAsepsis NotesOjambo FlaviaОценок пока нет
- Basal Cell CДокумент7 страницBasal Cell COjambo FlaviaОценок пока нет
- Traumatic Brain InjuryДокумент20 страницTraumatic Brain InjuryOjambo FlaviaОценок пока нет
- IntussusceptionДокумент24 страницыIntussusceptionOjambo Flavia100% (1)
- Acute AbdomenДокумент21 страницаAcute AbdomenOjambo FlaviaОценок пока нет
- Fluid Replacement in Burned PatientsДокумент4 страницыFluid Replacement in Burned PatientsOjambo FlaviaОценок пока нет
- Fluid & ElectrolytesДокумент8 страницFluid & ElectrolytesOjambo FlaviaОценок пока нет
- 13.2 Testicular Torsion - 1 Lecture-TZДокумент29 страниц13.2 Testicular Torsion - 1 Lecture-TZOjambo FlaviaОценок пока нет
- Saxons: Sahson Seaxan, Old Saxon: Sahson, Low German: Sassen, Dutch: Saksen) Were A Group of GermanicДокумент15 страницSaxons: Sahson Seaxan, Old Saxon: Sahson, Low German: Sassen, Dutch: Saksen) Were A Group of GermanicNirmal BhowmickОценок пока нет
- GR 14078 - Rubi v. PB MindoroДокумент2 страницыGR 14078 - Rubi v. PB MindoroChelsea CatiponОценок пока нет
- General KnowledgeДокумент29 страницGeneral KnowledgeSadiq AdnanОценок пока нет
- COHEN v. PBPP Et Al - Document No. 6Документ1 страницаCOHEN v. PBPP Et Al - Document No. 6Justia.comОценок пока нет
- Elvis Wayne Jones v. The Texas Beaumont U.S. District Courts, 4th Cir. (2016)Документ2 страницыElvis Wayne Jones v. The Texas Beaumont U.S. District Courts, 4th Cir. (2016)Scribd Government DocsОценок пока нет
- dd214 RДокумент1 страницаdd214 Rapi-255779612Оценок пока нет
- Case DigestДокумент4 страницыCase DigestRussel SirotОценок пока нет
- Presentación Departamento de ValleДокумент13 страницPresentación Departamento de ValleMelissa MendozaОценок пока нет
- Facts:: Tunay Na Pagkakaisa NG Manggagawa Sa Asia Brewery V. Asia Brewery August 3, 2010Документ2 страницыFacts:: Tunay Na Pagkakaisa NG Manggagawa Sa Asia Brewery V. Asia Brewery August 3, 2010Cj NightsirkОценок пока нет
- HUP Africa Slave Trade10Документ41 страницаHUP Africa Slave Trade10tmkusterОценок пока нет
- AttemptedДокумент2 страницыAttemptedDaniel Klint Richter CareОценок пока нет
- Civ Ii - SC - Sales and LeaseДокумент46 страницCiv Ii - SC - Sales and Leasewesternwound82Оценок пока нет
- Defending Jacob: & The Hermeneutic CodeДокумент12 страницDefending Jacob: & The Hermeneutic CodeTamara EzquerraОценок пока нет
- Griggs v. Ford Motor Company, 983 F.2d 238, 11th Cir. (1993)Документ1 страницаGriggs v. Ford Motor Company, 983 F.2d 238, 11th Cir. (1993)Scribd Government DocsОценок пока нет
- Canon 11 Bugaring Vs EspanyolДокумент2 страницыCanon 11 Bugaring Vs EspanyolOne TwoОценок пока нет
- QuitclaimДокумент2 страницыQuitclaimKrizzy Gayle0% (1)
- Five Year LLB Course of Nuals Assignment TopicsДокумент3 страницыFive Year LLB Course of Nuals Assignment TopicsYedu KrishnaОценок пока нет
- Legal Ethics - Notarial Practice CasesДокумент24 страницыLegal Ethics - Notarial Practice CasesMercy Lingating100% (1)
- Mini-Dungeon - HMD-004 The Grand Basilisk Egg HuntДокумент5 страницMini-Dungeon - HMD-004 The Grand Basilisk Egg HuntАлексей ЖуравлевОценок пока нет
- Gender and EducationДокумент8 страницGender and EducationRosheil Ramos100% (1)
- Gonzales Cannon September 6 IssueДокумент30 страницGonzales Cannon September 6 IssueGonzales CannonОценок пока нет
- Gregoria de Jesus Version of The FirstДокумент4 страницыGregoria de Jesus Version of The FirstPauline Shane LaborceОценок пока нет
- Data 011015Документ61 страницаData 011015Vuong PhamОценок пока нет
- E20240310 4TH Lent BДокумент4 страницыE20240310 4TH Lent BDodong CardosaОценок пока нет
- Unit 2 Higher TestДокумент2 страницыUnit 2 Higher Testvanu1986Оценок пока нет
- Buruanga MTF Resolution-3-2020Документ3 страницыBuruanga MTF Resolution-3-2020Badidz Ong SucoОценок пока нет
- Acleda Bank Aml 2009Документ60 страницAcleda Bank Aml 2009Jeevann Goldee Shikamaru100% (1)
- So He Was Right Then - David IrvingДокумент2 страницыSo He Was Right Then - David Irvingscribmem88% (8)
- Background Verification Form With LOA. v.2.1.1Документ7 страницBackground Verification Form With LOA. v.2.1.1selvanОценок пока нет
- Historical Simulation and The Civil WarДокумент206 страницHistorical Simulation and The Civil WarRA LeahОценок пока нет