Академический Документы
Профессиональный Документы
Культура Документы
2014 Curs Nefrologie-De Prezentat 4-Ian 2014
Загружено:
Violeta Malina Bîrsan Hodivoianu100%(1)100% нашли этот документ полезным (1 голос)
67 просмотров291 страницаThis document provides an overview of nephrology and renal structure and function. It discusses the anatomy of the kidney including the renal cortex, medulla, and sinus. It describes the nephron as the functional unit of the kidney and its roles in filtration, reabsorption, secretion and excretion. Common renal pathologies are also summarized such as glomerulonephritis, acute tubular necrosis, and nephrosclerosis.
Исходное описание:
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThis document provides an overview of nephrology and renal structure and function. It discusses the anatomy of the kidney including the renal cortex, medulla, and sinus. It describes the nephron as the functional unit of the kidney and its roles in filtration, reabsorption, secretion and excretion. Common renal pathologies are also summarized such as glomerulonephritis, acute tubular necrosis, and nephrosclerosis.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
100%(1)100% нашли этот документ полезным (1 голос)
67 просмотров291 страница2014 Curs Nefrologie-De Prezentat 4-Ian 2014
Загружено:
Violeta Malina Bîrsan HodivoianuThis document provides an overview of nephrology and renal structure and function. It discusses the anatomy of the kidney including the renal cortex, medulla, and sinus. It describes the nephron as the functional unit of the kidney and its roles in filtration, reabsorption, secretion and excretion. Common renal pathologies are also summarized such as glomerulonephritis, acute tubular necrosis, and nephrosclerosis.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 291
Titu Maiorescu University
Curs Medicina Interna
NEPHROLOGY- I
Prof univ dr Ion C Tintoiu
Characteristics of Renal Structure and
Function
I. Physiological Anatomy of the Kidney
Renal cortex
Cortical lobules - which
form caps over the
bases of the pyramids
Renal columns - which
dip in between the
pyramids
Renal medulla
has 10 conical masses
called renal pyramids,
their apices form renal
papillae
Renal sinus
Space that extends into kidney from hilus
Contains branches of renal artery and renal vein
Renal pelvis divides into 2-3 major calices and these in turn divide into 7-
13 minor calices, each minor calyx (cup of flower) ends in an expansion
which is indented by 1-3 renal papillae
Histologically, each kidney is composed 1-3 million
uriniferous tubules. Each consists of
Secretory part - which forms urine is called
nephron, functional unit of kidney
Nephrons open in to collecting tubules. Many such tubules
unite to form the ducts of Bellini which open into minor
calices
Arterial Supply
One renal artery on each side arising from abdominal
aorta
At or near hilus, renal artery divides into anterior and
posterior branches giving rise to segmental arteries
Lymphatics
Lateral aortic nodes
Major Functions of the Kidneys
1. Regulation of:
-body fluid osmolarity and volume
-electrolyte balance
-acid-base balance
-blood pressure
2. Excretion of
. metabolic products,drugs
.foreign substances (pesticides, chemicals etc.)
.excess substance (water, etc)
3. Secretion of
-erythropoitin
-1,25-dihydroxy vitamin D
3
(vitamin D activation)
- renin
-prostaglandin
-Nephron struc
and
Functions
Glomerulus
Proximal Tubule (PCT)
Loop of Henle
Distal tubule
Collecting tubule
Functions of the Nephron
Filtration
Reabsorption
Secretion
Excretion
Glomerular Filtration
Figure 26.10a, b
Proximal Tubule (PCT)
Reabsorption
NaCl
Water
Bicarbonate
Glucose
Proteins
Aminoacids
K
+
, Mg, PO
4
+
, uric acid,
urea
Secretion
Organic anions
Organic cations
Ammonia products
Reabsorption of solutes in PCT
Loop of Henle
25-30% ultrafiltrate reaches loop of Henle
15-20% filtered Na
+
load reabsorbed
Solute and water reabsorption is passive and follows
concentration and osmotic gradients (except thick
ascending loop)
Sodium reabsorption is coupled to both K
+
and Cl
-
reabsorption
Cl
-
in tubular fluid is rate limiting factor
Calcium and magnesium reabsorption
Parathyroid hormone calcium reabsorption at this
site
Loop diuretics inhibit Na and Cl reabsorption in TAL
compete with Cl- for its binding site on carrier protein
Distal tubule
Very tight junctions between tubular cells
relatively impermeable to water and Na
+
5% of filtered Na
+
load reabsorbed
Parathyroid hormone and vit D mediated
calcium reabsorption
The late distal segment (collecting segment)
Hormone mediated Ca
+
reabsorption
Aldosterone mediated Na
+
reabsorption
Collecting tubule
5-7% of filtered Na
+
load is reabsorbed
Cortical collecting tubule two types of
cells:
Principal cells secrete K
+
aldosterone
mediated Na
+
reabsorption
Intercalated cells acid base regulation
A Summary of Renal Function
Nephron symphony
.
Renal Pathology
Diseases of the kidney
1-Glomeruli
Glomerulonephritis
Primary
Secondary
Chronic
2-Tubulointerstitium
Acute tubular
necrosis
Pyelonephritis
Acute
chronic
3-Vessels
Nephrosclerosis
4-Urinary obstruction
Stones
Hydronephrosis
5- Cystic diseases of the
kidney
6-Tumors
Benign
Malignan
7-Litiazis
.
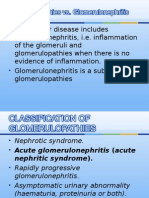
Glomerular diseases
GLOMERULONEPHRITIS
Acute Glomerulonephritis:
Rapidly Progressive
Glomerulonephritis
Chronic Glomerulonephritis
Nephrotic Syndrome
Asymptomatic urinary
abnormalities
Glomerular disease
Primary Glomerulonephritis
Minimal change GN
Membranous GN
Focal segmental GS
Membranoproliferative GN
Diffuse proliferative GN
Crescentic GN
Seconday
SLE, DM, Amyloidosis, Goodpasture, vasculitis
Hereditary
Albort syndrome
Secondary Glomerulonephritis
Diabetes most common cause
most common cause of renal failure
glycoproteins deposit in basement membrane
Vascular disease
atherosclerosis
HTN
vascultitis
Glomerular diseases:
Primary Glomerulonephritis
.
Acute
Glomerulonephritis
Acute glomerulonephritis is the
inflammation of the glomeruli which causes
the kidneys to malfunction
It is also called Acute Nephritis,
Glomerulonephritis and Post-Streptococcal
Glomerulonephritis
Predominantly affects children from ages 2
to 12
Incubation period is 2 to 3 weeks
Acute Glomerulonephritis
Definition
Fever
Headache
Malaise
Anorexia
Nausea and vomiting
High blood pressure
Pallor due to edema and/or anemia
Confusion
Lethargy
Loss of muscle tissue
Enlargement of the liver
Acute Glomerulonephritis
General Symptoms
Hematuria: dark brown or smoky urine
Oliguria: urine output is < 400 ml/day
Edema: starts in the eye lids and face
then the lower and upper limbs then
becomes generalized; may be migratory
Hypertension: usually mild to moderate
Hypoproteinemia,
hypercholesterolemia),
mixed
Acute Glomerulonephritis
Signs and Symptoms
Acute Glomerulonephritis
Etiology
Infectious
Streptococcal
Nonstreptococcal postinfectious
glomerulonephritis
Bacterial
Viral
Parasitic
Noninfectious
Multisystem systemic diseases
Primary glomerular diseases
Acute Glomerulonephritis
INVESTIGATIONS
Base line measurements:
- Urea
- Creatinine
- Urinalysis (MSU):
a) Urine microscopy (red cell cast)
b) proteinuria
Hypertensive encephalopathy,
Heart failure and acute
Pulmonary edema may occur in severe
cases
Acute renal necrosis due to injury of
capillary or capillary thrombosis
Acute Glomerulonephritis
Complications
proper hygiene
prompt medical assessment for
necessary antibiotic therapy should be
sought when infection is suspected
prophylactic immunizations
Acute Glomerulonephritis
Prevention
Treatment
Treat the underlying infections when acute GN is associated with chronic infections.
Antimicrobial therapy
Antibiotics (eg, penicillin) are used to control local symptoms and to prevent
spread of infection to close contacts.
Antimicrobial therapy does not appear to prevent the development of GN,
except if given within the first 36 hours.
Loop diuretic therapy
Loop diuretics may be required in patients who are edematous and
hypertensive in order to remove excess fluid and to correct hypertension.
Relieves edema and controls volume, thereby helping to control volume-
related elevation in BP.
Vasodilator drugs (eg, nitroprusside, nifedipine, hydralazine,
diazoxide) may be used if severe hypertension or encephalopathy is present
Diet:
Sodium and fluid restriction
Protein restriction for azotemic patients
Activity: Recommend bed rest until signs of glomerular inflammation and
circulatory congestion subside.
.
Chronic glomerulonephritis
Chronic glomerulonephritis
The condition is characterized
1 - irreversible and progressive glomerular
and tubulointerstitial fibrosis
2-ultimately leading to a reduction in the
glomerular filtration rate (GFR) and
3- retention of uremic toxins
.
. The diagnosis of CKD can be made without
knowledge of the specific cause.
Chronic glomerulonephritis
Etiology
Nearly all forms of acute glomerulonephritis have a
tendency to progress to chronic
glomerulonephritis.
The progression from acute glomerulonephritis to
chronic glomerulonephritis is variable.
Whereas complete recovery of renal function is the
rule for patients with poststreptococcal
glomerulonephritis, several other
glomerulonephritides, such as
immunoglobulin A (IgA) nephropathy, often
have a relatively benign course and many do not
progress to ESRD.
Chronic glomerulonephritis
Pathogenesis
Reduction in nephron mass from the initial injury
reduces the GFR.
This reduction leads to hypertrophy and
hyperfiltration of the remaining nephrons and to
the initiation of intraglomerular hypertension.
These changes occur in order to increase the GFR of
the remaining nephrons, thus minimizing the
functional consequences of nephron loss.
The changes, however, are ultimately detrimental
because they lead to glomerulosclerosis and
further nephron loss.
Chronic glomerulonephritis
Histologic Findings
In early stages, the glomeruli may still
show some evidence of the primary
disease.
In advanced stages, the glomeruli are
hyalinized and obsolescent.
The tubules are disrupted and atrophic,
and marked interstitial fibrosis and
arterial and arteriolar sclerosis occur.
Chronic glomerulonephritis
Histologic Findings
1-Minimal-Change Disease
2-Focal segmental
glomerulosclerosis
3-Mesangiocapillary GN
4-Membranous nephropathy
.
Mesangial proliferative MPGN
1-Hypercellularity,
2-Mesangial proliferation,
3-Inflammatory cell infiltrate,
4-Positive IF for IgG and C3 and
5-Subepithelial deposits on EM.
Chronic glomerulonephritis
Clinical Manifestations
Uremia-specific findings
Edemas
Hypertension
Jugular venous distension (if severe volume
overload is present)
Pulmonary rales (if pulmonary edema is
present)
Pericardial friction rub in pericarditis
Tenderness in the epigastric region or blood
in the stool (possible indicators for uremic
gastritis or enteropathy)
Chronic glomerulonephritis
Lab Studies
Urinalysis
Urinary protein excretion
Serum chemistry
Serum creatinine and urea nitrogen levels
are elevated.
Impaired excretion of potassium, free water, and
acid results in hyperkalemia, hyponatremia, and
low serum bicarbonate levels, respectively.
Impaired vitamin D-3 production results in
hypocalcemia, hyperphosphatemia, and high levels
of parathyroid hormone.
Low serum albumin levels may be present if
uremia interferes with nutrition or if the patient is
nephrotic.
Renal ultrasonogram
Obtain a renal ultrasonogram to
determine renal size, to assess for the
presence of both kidneys, and to
exclude structural lesions that may
be responsible for azotemia.
Small kidneys often indicate an
irreversible process.
Kidney biopsy
Chronic glomerulonephritis
Imaging Studies
Chronic glomerulonephritis
Treatment
The target pressure for patients with proteinuria greater
than 1 g/d is less than 125/75 mm Hg; for patients with
proteinuria less than 1 g/d, the target pressure is less
than 130/80 mm Hg.
Angiotensin-converting enzyme inhibitors (ACEIs)
angiotensin II receptor blockers (ARBs)
Diuretics are often required because of decreased
free-water clearance, and high doses may be required
to control edema and hypertension when the GFR
falls to less than 25 mL/min.
Beta-blockers, calcium channel blockers, central
alpha-2 agonists (eg, clonidine), alpha-1 antagonists,
and
direct vasodilators (eg, minoxidil, nitrates) may be
used to achieve the target pressure.
Chronic glomerulonephritis
Treatment
Minimal change glomerulonephritis
1-Corticosteroids induce remission in >90% of
children and 80% of adults (slower response).
2-immunosuppression: (cyclophosphamide,
ciclosporin (=cylosporin)): early/ frequent
relapses; steroid SEs/dependence.
Prognosis: 1% progress to ESRF.
Chronic glomerulonephritis
Treatment
Focal segmental glomerulosclerosis
Poor response to corticosteroids (10
30%). Cyclophosphamide or ciclosporin
(=cylosporin) may be used in steroid-resistant
cases.
Prognosis: 3050% progress to ESRF.
Chronic glomerulonephritis
Treatment
Mesangial proliferative GN
1-Antibiotics,
2-Diuretics, and
3-Antihypertensives as necessary.
4-Dialysis is rarely required.
Prognosis: Good.
Chronic glomerulonephritis
Treatment
Membranous nephropathy
If renal function deteriorates, consider
corticosteroids and chlorambucil.
Prognosis: Untreated, 15% complete
remission, 9% ESRF at 25yrs and 41% at
15yrs.
.
Rapidly Progressive
Glomerulonephritis
Rapidly Progressive Glomerulonephritis
Rapidly progressive
glomerulonephritis (RPGN) is a
disease of the kidney that results in
a rapid decrease in the glomerular
filtration rate of at least 50% over
a short period, from a few days to 3
months.
The cause of RPGN is unknown. A
genetic predisposition may exist for the
development of this disease.
Multiple studies have demonstrated that
ANCA- (antineutrophil cytoplasmic
antibodies) activated neutrophils
attack vascular endothelial cells.
ANCA-associated vasculitis.
A viral etiology is possible.
Rapidly Progressive Glomerulonephritis
Etiology
Rapidly Progressive Glomerulonephritis
Pathology
Renal biopsshow
A diffuse, proliferative,
necrotizing
glomerulonephritis with
crescent formation.
The main pathologic
finding is fibrinoid
necrosis (>90% of biopsy
specimens); extensive
crescent formation is
present in at least 50% of
glomeruli.
Rapidly Progressive Glomerulonephritis
Clinical Manifestations
Symptoms and signs of renal
failure,
pain,
haematuria,
systemic symptoms (fever, malaise,
myalgia, weight loss).
Rapidly Progressive Glomerulonephritis
Lab Studies
The most important requirement in the diagnosis of
antineutrophil cytoplasmic antibodies (ANCA) ANCA-
associated disease is a high index of suspicion. Rapid
diagnosis is essential for organ preservation. Laboratory
studies include the following:
Routine chemistry: The most common abnormality is
an increased serum creatinine level.
Urinalysis with microscopy:
Antinuclear antibody (ANA) titer:
ANCA
Urine and serum protein electrophoresis: Perform this in
any middle-aged or elderly person presenting with RPGN
to exclude the presence of light-chain disease or overt
multiple myeloma as a cause of the clinical findings.
Rapidly Progressive Glomerulonephritis
Treatment
1-High-dose corticosteroids;
cyclophosphamide plasma
exchange/ renal
2-Transplantation.
Prognosis:
Poor if initial serum creatinine
>600mol/L.
Proteinurea
3.5 g/day
(protein: creatinine
ratio >3-3.5)
Generalized
Oedema
Hypoalbuminaeia
<3g/L
The Nephrotic Syndrome
Is not a disease but a group of signs and
symptoms seen in patients with heavy
proteinuria
presents with oedema
proteinuria usually > 3.5g / 24hrs (>0.05g
/ kg / 24hrs in children)
serum albumin < 30g/l
other features: hyperlipidaemia, and
hypercoaguable state
The Nephrotic Syndrome
Pathophysiology
proteinuria: due to an increase in glomerular
permeability
hypoalbuminuria: occurs when liver synthesis cannot
keep up with urine losses
oedema mechanism is complex and still in dispute:
primary salt and water retention associated with
reduced renal function as well as reduced plasma
oncotic pressure are primary factors (overfill and
underfill)
minimal change disease fits the underfill theory best
hyperlipidaemia: increased liver synthesis
hypercoagulation: increased fibrinogen and loss of
antithrombin III
DAMAGED
Proteinuria
Primary (idiopathic):
Minimal change disease
Most common cause in children
Membranous Nephropathy
Most common cause in Adults
Focal Segmental Glomerulosclerosis
MembranoProliferative
Glomerulonephritis
Secondary to:
DM (the leading cause of secondary nephrotic syndrome)
SLE
Amyloidosis
Infections:
Hepatitis B and C, HIV,syphilis, post-streptococcal
Malignancy:
multiple myloma , Hodgkin lymphoma, solid tumor
Drugs
(NSAIDs, gold, penicillamine ,heavy metals etc).
Generalized Odema
-The predominant feature
-The face, particularly the
periorbital area, is swollen
in the morning& lower extremities
and genital area later in the day
-In advanced disease: the whole body
(anasarca) shortness of breath
Frothy urine and urine dipstick
proteinuria value of 3+
Symptoms & signs for secondary cause if present
24-hour urine collection >3,5 g/day (nephrotic-range proteinuria)
Alternative : calculating the total protein-to-creatinine ratio (mg/mg)
on a random urine specimen.
The history and physical examination Systemic disease
Serologic studies (ANA), complement, hepatitis B and hepatitis C
serologies and the measurement of cryoglobulins ,serum or urine protein
electrophoresis.
Renal biopsy required to establish the diagnosis in most of times.
BUN, creatinine, creatinin clearnce.Na,
K,bicarbonates,chloride
CBC , serum albumin, serum proteins, calcium,
Lipid profile, Coagulation tests
Renal biopsy
69
Disease-
spesific
Compli
cation
symptoms
Oedema
Low salt diet
Diuretics
serial measurement of body weight
Proteinuria
ACE inhibitors or ARBs
Hypoalbuminaemia
High protein diet not indicated
0.81 g/kg/day
Ref: Up to date online 17.3.
Hyperlipidaemia
Regular Lipid profile
Statin if severe long lasting nephrotic syndrome
Control other CVD risk factorstarget blood pressure
125/75
Thromboembolic risk
Routin Prophylactic anticoagulation not recommend
High index of suspicion for thromboemboli
Infections
High index of suspicion
Antipneumococcal and influenza vaccinations
Ref: Up to date online 17.3.
Management of the nephrotic
syndrome
Na+< 60 mmol/24 hrs
water restriction
diuretics (if not volume depleted)
reduced protein diet (controversial)
treat infections
prophylaxis for thrombosis
specific therapy
corticosteroids
Immunosuppression
Diabetic Nephropathy
aggressive glucose control and aggressive BP control
with ACE
Titu Maiorescu University
Curs Medicina Interna
NEPHROLOGY-II
Prof univ dr Ion C Tintoiu
.
Other Renal Diseases
Other Renal Diseases
1. 1-Interstitial Nephritis
2. 2-Diabetic Nephropathy
3. 3-Microscopic Vasculitis and SLE
4. 4-Gout and the Kidney
5. 5-Myeloma Kidney
.
1-Interstitial Nephritis
Causes of interstitial nephritis
Drugs
Infection
Autoimmune
Metabolic
Radiation
Neoplastic infiltration
Mechanical
Drugs and interstitial nephritis
methicillin 17%
other penicillins <1%
cephalosporins <1%
rifampicin 1%
ciprofloxacin 1%
cotrimoxazole
fenoprofen <1%
frusemide <1%
bumetanide <1%
cimetidine <1%
allopurinol <1%
5 aminosalicylates
omeprazole ? ranitidine (rare)
Bacterial infection
bacterial infection of the renal parenchyma
causes interstitial nephritis
infection without anatomical abnormality
seldom produces permanent damage
obstruction (stones, prostate etc) in
combination with infection can cause
progressive disease
tuberculosis causes extensive destruction from
granulomata, fibrosis and caseation
Autoimmune
systemic lupus
erythematosus
transplant
rejection
deposition of :
calcium salts
uric acid
Infiltration in neoplastic and other
diseases
lymphoma and leukaemias
myeloma
Bence-Jones protein (light chains from
malignant plasma cell clone) causes interstitial
nephritis, tubular obstruction(cast nephropathy)
and amyloid deposition
called myeloma kidney
sarcoidosis
mechanical causes of interstitial
nephritis
reflux nephropathy
calculi
ureteric fibrosis
prostatic hypertrophy
urethral stenosis
tumours
pathophysiolgical changes in
interstitial nephritis
hypertension (50%)
proteinuria (~1-2 g/24hrs)
reduced urinary concentrating ability
salt wasting
renal tubular acidosis
Diagnosis and Treatment
renal impairment
inactive urine sediment common (cf nephritis)
eosinophils in urine and interstitium in acute
hypersensitivity reactions
renal biopsy
improvement after withdrawal of drugs and toxins
use of corticosteroids (prednisone)
water and and electrolyte
treatment of hypertension
.
2-Diabetic nephropathy
Diabetic Nephropathy
Pathological lesions:
diffuse glomerular sclerosis
nodular sclerosis (Kimmelstiel -Wilson lesion)
arteriolar hyalinisation
Associated lesions:
Papillary necrosis
Pyelonephritis
Bladder dysfunction
Radio contrast renal failure
hyporeninaemic hypoaldosteronism with
hyperkalaemia
Pathophysiology of Diabetic Nephropathy
renal hypertrophy and hyperfiltration
microalbuminuria (< 100mg/24hrs and negative to
protein test strip-albustix)
hypertension
hyperfiltration and microalbuminuria can be improved
by good diabetic control
microalbuminuria is a predictor of diabetic
nephropathy and mortality in diabetics - it probably
has no predictive value for other renal diseases
.
3- Lupus Nephritis
Vasculitis
WHO classification
Lupus Nephritis Type I no pathology
T
y
p
e
V
:
m
e
m
b
r
a
n
o
u
s
Type II : mesangial
T
y
p
e
I
I
I
:
f
o
c
a
l
p
r
o
l
i
f
e
r
a
t
i
v
e
T
y
p
e
I
V
:
d
i
f
f
u
s
e
p
r
o
l
i
f
e
r
a
t
i
v
e
Lupus nephritis
Hematuria and proteinuria
HTN common
Active urine sediment: rbc casts
Decreased C3 and C4
anti-double stranded DNA antibody specific for
active nephritis
Prognosis varies greatly based on initial
pathology, usually guarded
Type IV greatest risk of progressing to CKD stage 5
Treatment with steroids, cytoxan
Systemic Lupus Erythematosus
Diagnosis:
clinical presentation - rash, arthralgia, fever,
tiredness, anaemia etc
hypocomplementaemia - (low C3 and C4)
antinuclear antibodies and anti DNA antibodies
Treatment:
depends on histological severity (WHO class I - V)
nearly all get corticosteroids
WHO Class IV usually get corticosteroids and
cyclophosphamide
.
Gout, Uric Acid and Renal
Disease
Gout, Uric Acid and Renal Disease
uric acid calculi, parenchymal deposits of
uric acid and tubular obstruction with
urate can cause renal damage
an elevated plasma uric acid does not in
itself seem to cause renal damage
1/4 of patients with gout get uric acid
stones
1/4 of patients with uric acid stones will
have gout
Acute and Chronic urate nephropathy
acute nephropathy with overproduction of uric acid
and kidney obstruction with uric acid crystals
can occur with treatment of malignant disease with
cytotoxics, heat stroke and status epilepticus
treat with fluids and prophylaxis with allopurinol
role of uric acid in chronic renal failure disputed but
does occur with some familial disorders
association between hyperuricaemia, hypertension
vascular disease, hyperlipidaemia and diabetes
.
Amyloidosis and Myeloma
Kidney
Amyloidosis and Myeloma Kidney
amyloid represents a family of proteins which
polymerize to produce the beta pleated sheet of
amyloid and deposit in tissues
AL amyloid (primary amyloid) made from
light chains associated with plasma cell
disorders, mostly overt myeloma
AA amyloid (secondary amyloid) is made from
A protein and is an acute phase reactant
associated with chronic inflammatory diseases
like rheumatoid arthritis and bronchiectasis
Titu Maiorescu University
Curs Medicina Interna
NEPHROLOGY-III
Prof univ dr Ion C Tintoiu
.
Acute and chronic
Renal Failure
.
Acute Renal Failure
Acute renal failure -ARF
Deterioration of renal
function over a period of hours to days,
resulting in
the failure
of the kidney to excrete nitrogenous
waste products and
to maintain
fluid and electrolyte homeostasis
ARF Rapid deterioration of renal function
(increase of creatinine of >0.5 mg/dl in <72hrs.)
azotemia (accumulation of nitrogenous wastes)
elevated BUN and Creatinine levels
decreased urine output (usually but not always)
Oliguria: <400 ml urine output in 24 hours
Anuria: <100 ml urine output in 24 hours
Hilton, R. BMJ 2006;333:786-790
Causes of acute renal failure
Pre-renal
Volume depletion
Renal losses (diuretics, polyuria)
GI losses (vomiting, diarrhea)
Cutaneous losses (burns, Stevens-Johnson syndrome)
Hemorrhage
Pancreatitis
Decreased cardiac output
Heart failure
Pulmonary embolus
Acute myocardial infarction
Severe valvular heart disease
Abdominal compartment syndrome (tense ascites)
Renal
Glomerular
Antiglomerular basement membrane (GBM) disease (Goodpasture
syndrome)
Antineutrophil cytoplasmic antibody-associated
glomerulonephritis (ANCA-associated GN) (Wegener
granulomatosis, Churg-Strauss syndrome, microscopic polyangiitis)
Immune complex GN (lupus, postinfectious, cryoglobulinemia,
primary membranoproliferative glomerulonephritis)
Tubular
Ischemi
Totoxic
Heme pigment (rhabdomyolysis, intravascular hemolysis)
Crystals (tumor lysis syndrome, seizures, ethylene glycol
poisoning, megadose vitamin C, acyclovir, indinavir,
methotrexate)
Drugs (aminoglycosides, lithium, amphotericin B,
pentamidine, cisplatin, ifosfamide, radiocontrast agents)
Post-renal
Ureteric obstruction
Stone disease,
Tumor,
Fibrosis,
Ligation during pelvic surgery
Bladder neck obstruction
Benign prostatic hypertrophy [BPH]
Cancer of the prostate
Neurogenic bladder
Drugs(Tricyclic antidepressants, ganglion blockers,
Bladder tumor,
Stone disease, hemorrhage/clot)
Urethral obstruction (strictures, tumor)
Clinical feature-1
Signs and symptoms resulting from loss of
kidney function:
decreased or no urine output, flank pain,
edema, hypertension, or discolored urine
Asymptomatic
elevations in the plasma creatinine
abnormalities on urinalysis
Clinical feature-2
Symptoms and/or signs of renal failure:
weakness and
easy fatiguability (from anemia),
anorexia,
vomiting, mental status changes or
Seizures
edema
Systemic symptoms and findings:
fever
arthralgias,
pulmonary lesions
Acute Renal Failure
Diagnosis
Blood urea nitrogen and serum creatinine
CBC, peripheral smear, and serology
Urinalysis
Urine electrolytes
U/S kidneys
Serology: ANA,ANCA, Anti DNA, HBV, HCV, Anti
GBM, cryoglobulin, CK, urinary Myoglobulin
Acute Renal Failure
Diagnosis
Urinalysis
Unremarkable in pre and post renal causes
Differentiates ATN vs. AIN. vs. AGN
Muddy brown casts in ATN
WBC casts in AIN
RBC casts in AGN
Hansel stain for Eosinophils
Acute Renal Failure
Diagnosis
Laboratory Evaluation:
Scr, More reliable marker of GFR
Falsely elevated with Septra, Cimetidine
small change reflects large change in GFR
BUN, generally follows Scr increase
Elevation may be independent of GFR
Steroids, GIB, Catabolic state, hypovolemia
BUN/Cr helpful in classifying cause of ARF
ratio> 20:1 suggests prerenal cause
Treatment of
acute renal failure
Optimization of hemodynamic and
volume status
Avoidance of further renal insults
Optimization of nutrition
If necessary, institution of renal
replacement therapy
The function has to be temporarily
replaced by dialysis
Indication for dialysis
Symptoms of uremia (
encephalopathy,)
Uremic pericarditis
Refractory volume over load
Refractory hyperkalemia
Refractory metabolic acidosis
.
Chronic Renal Failure
Definitions
Chronic Renal Failure
Results form gradual, progressive loss of renal
function
Occasionally results from rapid progression of
acute renal failure
Symptoms occur when 75% of function is lost
but considered cohrnic if 90-95% loss of
function
Dialysis is necessary D/T accumulation or
uremic toxins, which produce changes in major
organs
Subjective symptoms
Chronic Renal Failure
Subjective symptoms are relatively same as
acute
Objective symptoms
Renal
Hyponaturmia
Dry mouth
Poor skin turgor
Confusion, salt overload, accumulation of K with
muscle weakness
Fluid overload and metabolic acidosis
Proteinuria, glycosuria
Urine = RBCs, WBCs, and casts
Chronic Renal Failure
Objective symptoms
Cardiovascular
Hypertension
Arrythmias
Pericardial effusion
CHF
Peripheral edema
Neurological
Burning, pain, and
itching, parestnesia
Motor nerve dysfunction
Muscle cramping
Shortened memory span
Apathy
Drowsy, confused,
seizures, coma, EEG
changes
Chronic Renal Failure
Objective symptoms
GI
Stomatitis
Ulcers
Pancreatitis
Uremic fetor
Vomiting
consitpation
Respiratory
^ chance of
infection
Pulmonary edema
Pleural friction
rub and effusion
Dyspnea
Kussmauls
respirations from
acidosis
Chronic Renal Failure
Objective symptoms
Endocrine
Stunted growth in
children
Amenorrhea
Male impotence
^ aldosterone secretion
Impaired glucose levels
R/T impaired CHO
metabolism
Thyroid and parathyroid
abnormalities
Hemopoietic
Anemia
Decrease in RBC
survival time
Blood loss from dialysis
and GI bleed
Platelet deficits
Bleeding and clotting
disorders purpura and
hemorrhage from body
orifices , ecchymoses
Chronic Renal Failure
Objective symptoms
Skeletal
Muscle and bone pain
Bone demineralization
Pathological fractures
Blood vessel
calcifications in
myocardium, joints,
eyes, and brain
Skin
Yellow-bronze skin
with pallor
Puritus
Purpura
Uremic frost
Thin, brittle nails
Dry, brittle hair, and
may have color
changes and alopecia
Chronic Renal Failure
Lab findings
BUN indicator of glomerular filtration rate and is
affected by the breakdown of protein. Normal is 10-
20mg/dL. When reaches 70 = dialysis
Serum creatinine waste product of skeletal muscle
breakdown and is a better indicator of kidney
function. Normal is 0.5-1.5 mg/dL. When reaches 10
x normal, it is time for dialysis
Creatinine clearance is best determent of kidney
function. Must be a 12-24 hour urine collection.
Normal is > 100 ml/min
K+ -
Hypocalcemia = tetany
Chronic Renal Failure
Other abnormal findings
Metabolic acidosis
Fluid imbalance
Insulin resistance
Anemia
Immunoligical problems
Chronic Renal Failure
Medical treatment
IV glucose and insulin
Na bicarb, Ca, Vit D, phosphate binders
Fluid restriction, diuretics
Iron supplements, blood, erythropoietin
High carbs, low protein
Dialysis - After all other methods have failed
Chronic Renal Failure
Hemodialysis
Vascular access
Temporary subclavian or femoral
Permanent shunt, in arm
Care post insertion
Can be done rapidly
Takes about 4 hours
Done 3 x a week
Chronic Renal Failure
Peritoneal dialysis
Semipermeable
membrane
Catheter inserted through
abdominal wall into
peritoneal cavity
Cost less
Fewer restrictions
Can be done at home
Risk of peritonitis
3 phases inflow, dwell
and outflow
Automated peritoneal
dialysis
Done at home at night
Maybe 6-7 times /week
CAPD
Continous ambulatory
peritoneal dialysis
Done as outpatient
Usually 4 X/d
Chronic Renal Failure
Transplant
Must find donor
Waiting period long
Good survival rate 1 year 95-97%
Must take immunosuppressants for life
Rejection
Watch for fever, elevated B/P, and pain over site
of new kidney
Transplant Meds
Patients have decreased resistance to infection
Corticosteroids anti-inflammarory
Deltosone
Medrol
Solu-Medrol
Cytotoxic inhibit T and B lymphocytes
Imuran
Cytoxan
Cellcept
T-cell depressors - Cyclosporin
Titu Maiorescu University
Curs Medicina Interna
NEPHROLOGY-IV
Prof univ dr Ion C Tintoiu
.
RENAL TUMOURS
.
CYSTIC DISEASES OF
THE KIDNEY
Fluid filled spaces within the kidney
May involve cortex or medulla or both
May be unilateral or bilateral
May be unilocular or multilocular
May be congenital or acquired
May be sporadic or genetically
determined
Clinical significance may be trivial or
grave
CLASSIFICATIONS OF
RENAL CYSTIC DISEASES
Polycystic kidney diseases:
1. Autosomal recessive (ARPKD)
classic infantile polycystic disease
with congenital hepatic fibrosis
2. Autosomal dominant (ADPKD)
Simple renal cysts
Acquired renal cystic disease
RENAL CYSTIC DISEASES
Enlarged but normally shaped pelvi-calyceal
system
Normal reniform shape complete with fetal
lobation & normal sized (undilated) ureter
Normal glomeruli and tubules
Normal interstitium and no dysplasia
Congenital hepatic fibrosis is almost always
present
Normal numbers of nephrons, no interstitial
fibrosis and no dysplasia
RENAL CYSTIC DISEASES
Pathological Features
Bilaterally enlarged kidneys (up to 4000 gms)
Diffuse cystic (1-2% cystic nephrons) change
with uninvolved intervening parenchyma
Varying sized, numerous to innumerable
generally spherical unilocular cysts, distributed
in cortex and medulla obscuring normal
reniform shape and corticomedullary junction,
containing yellowish to turbid to brown to black
colored fluid
Distorted pelvi-calyceal system
Cysts arising from any part of nephron or
collecting duct
Simple Renal Cysts
Extremely common as age advances
Incompletely understood pathogenesis
Commonly associated with scarred
kidneys
Asymptomatic with normal renal function
May be
solitary/multiple/unilateral/bilateral
Generally unilocular, round to oval of
varying sizes
Adult polycystic kidney disease
Renal cancer
.
Renal cancer
In infants and children :
Nephroblastoma ( Wilms
tumour )
In adults :
Renal cell carcinoma
Renal cell adenoma
Renal oncocytoma
NEPHROBLASTOMA ( Wilms
tumour )
Embryonal tumour arising from nephrogenic
blastemal cells
can differentiate in to several cell lines - blastemal,
epithelial and stromal
many replicate developing kidneys
Common in young children / uncommon in
neonates and infants
90% in < 6yrs. old ( mean: 3yrs. in boys and
3.5yrs. in girls )
NEPHROBLASTOMA
Clinical Features
Most common genitourinary cancer
Age: 1-3yrs., 98% in <10yrs
Abdominal mass, pain, & hematuria
Usually unicentric, may be multicentric (7%)
or bilateral (5%)
Imaging technique to reveal smaller lesions
No specific tumor markers identified
NEPHROBLASTOMA
prognosis and treatment
Depends upon :
stage, age and histology
Surgery with chemotherapy for :
stage I & II with favorable histology
surgery with chemotherapy and
radiotherapy for higher stages and
unfavorable histology
RENAL CELL CARCINOMA
Hypernephroma / Grawitzs
tumour
seems to be arising from mature
renal tubules
RENAL CELL CARCINOMA
Clinical Features & Diagnosis
classic triad :
hematuria, flank pain and abdominal
mass
may be clinically occult, 30% presents
with metastatic lesion
Polycythemia due to erythropoietin
constitutional symptoms
imaging techniques - useful
RENAL CELL
CARCINOMA
prognosis
Influenced by multiple factors :
tumour size
infiltrative margins
histological type
tumour stage - most important
Can be expressed in terms of histological
types
Renal cell carcinoma
RENAL CELL
ADENOMA
Incidental findings at autopsy (22%)
Well demarcated, unencapsulated
Pale yellow-gray, discrete cortical mass
Up to 2 cms. in maximum dimension
Bladder Carcinoma
Derived from transitional epithelium
Present with painless hematuria
Prognosis depends on grade and depth of invasion
Overall 5y survival = 50%
.
DIALYSIS
Dialysis
Definition
Artificial process that partially replaces renal
function
Removes waste products from blood by
diffusion (toxin clearance)
Removes excess water by ultrafiltration
(maintenance of fluid balance)
Wastes and water pass into a special liquid
dialysis fluid or dialysate
Types
Haemodialysis (HD)
Peritoneal Dialysis (PD)
They work on similar principles: Movement
of solute or water across a semipermeable
membrane (dialysis membrane)
Diffusion
Movement of solute
Across semipermeable membrane
From region of high concentration to one of
low concentration
Ultrafiltration
Made possible by osmosis
Movement of water
Across semipermeable membrane
From low osmolality to high osmolality
Osmolality number of osmotically active
particles in a unit (litre) of solvent
Haemodialysis
Dialysis process occurs outside the body in a
machine
The dialysis membrane is an artificial one:
Dialyser
The dialyser removes the excess fluid and
wastes from the blood and returns the filtered
blood to the body
Haemodialysis needs to be performed three
times a week
Each session lasts 3-6 hrs
AV Fistula Access
Matures in about 6 weeks
Ensure good working order
Avoid tight clothing or wrist watch on fistula arm
Assess fistula daily; notify immediately if not working
Avoid BP cuff on fistula arm
Avoid blood sampling on fistula arm (except daily
HD Rx)
Avoid sleeping on fistula arm
Grafts (synthetic) may be used to create an AV fistula
AV Fistula
AV Fistula
Vascular Access Catheter
Hemodialysis
3-4 times a week
Takes 2-4 hours
Machine filters
blood and
returns it to
body
Problems with HD
Rapid changes in BP
fainting, vomiting, cramps, chest pain, irritability, fatigue, temporary loss
of vision
Fluid overload
esp in between sessions
Fluid restrictions
more stringent with HD than PD
Hyperkalaemia
esp in between sessions
Problems with access
poor quality, blockage etc. Infection (vascular access catheters)
Bleeding
from the fistula during or after dialysis
Infections
during sessions; exit site infections; blood-borne viruses e.g. Hepatitis,
HIV
Peritoneal Dialysis (PD)
Uses natural membrane (peritoneum) for
dialysis
Access is by PD catheter, a soft plastic tube
Catheter and dialysis fluid may be hidden
under clothing
Suitability
Excludes patients with prior peritoneal scarring e.g.
peritonitis, laparotomy
Excludes patients unable to care for self
Peritoneal Dialysis
.
Principles of Peritoneal Dialysis (PD)
Standard dialysis solution contains:
Na
+
132 mEq/l
Cl
-
96 -102 mEq/l
Ca
2+
2.5 3.5 mEq/l
Mg
2+
0.5 -1.5 mEq/l
Dialysis solution buffer:
Sodium lactate
Pure HCo
3
-
HCo
3
-
/Lactate combinations
Lactate is absorbed and converted to HCo
3
-
by
the liver
Dextrose solution strengths: 1.5%, 2.5%, 4.25%
Types
Continuous Ambulatory Peritoneal Dialysis
(CAPD)
Automated peritoneal Dialysis (APD)
Continuous cyclical
Intermittent
Continuous Ambulatory Peritoneal Dialysis
(CAPD)
CONTROLLING YOUR
DIET
Foods to control are those containing:
Protein
Potassium
Sodium
Phosphorous
Fluid
FLUIDS
Healthy kidneys remove fluids as urine
Check for fluid and sodium retention
Need to restrict fluid intake
VITAMINS
Folic acid
Iron supplements
Do not take OTCs without consulting the
doctor.
MANAGING YOUR DIET
INDICATORS OF GOOD CONTROL:
Weight loss or gain
Blood pressure
Swelling of hands and feet
Blood samples
Plasmapheresis:
plasma exchange and immunoadsorption
An adult donor kidney transplanted to the left iliac
fossa of an adult recipient.
.
.
Kidney Stones
ETIOLOGY
HYPEREXCRETI ON OF RELATI VELY INSOLUBLE URI NARY
CONSTI TUENTS
1. Oxalate Though oxalate is the major component of 70%
of all renal stones, yet hyperoxaluria as a cause of formation of such
stone is relatively rare. Cabbage, rhubarb, spinach, tomatoes, black tea and cocoa
contain large amount of oxalate. Ingestion of excessive amounts of ascorbic acid
and orange juice also increase urinary oxalate excretion.
2. Calcium - On regular diets normal urinary excretion of calcium ranges
between 200 mg to 300 mg per day. The major calcium in foods are in milk and
cheese. Milk and dietary protein also cause increased absorption of calcium from
the gut.
3. Uric acid - Many patients with gout form uric acid calculi
particularly when under treatment. If the urine is made alkaline and
dilute while treating this disease chance of uric acid stone formation is less
4. Cystine
Cystinuria is an herditary disease which is more common
in infants and children. Only a small percentage of patients with
Cystinuria form stones.
5. Drug induced stones
In rare cases, the long term use of magnesium trisilicate in
the treatment of peptic ulcer has produced radio opaque silicon
stones.
LOCATION OF STONES IN KIDNEY
EFFECTS OF STONE
The size and position of the stone usually govern the development
of secondary pathologic changes in the urinary trace.
A. SAME KI DNEY
1. Obstruction
2. Infection
B OPPOSITE KIDNEY
1. Compensatory hypertrophy
2. Stone formation may be bilateral
3. Infection
4. Calculus anuria
.
CLINICAL FEATURES
Symptoms - Symptom wise cases can be divided into 4 groups :-
1. Quiescent calculus A few stones, particularly the phosphate
stones, may lie dormant for quite a long period.
These stone are also discovered due to symptoms of Urinary
Infection
2. Pain - Plain is the leading symptom of renal calculus in majority of
cases (80%). Three types of pain .
a) Fixed renal pain
b) Ureteric colic
c) Referred pain
3. Hydronephrosis
4. Occasionally haematuria is the leading and only symptom.
(iii) Swelling - When there is Hydronephrosis or
pyonephrosis associated with renal calculus, a swelling may be felt
in the flank.
The characteristic of a renal swelling are :-
(a) Oval or reniform in shape
(b) Swelling is almost fixed and cannot be moved.
(c) A kidney lump is ballot able.
3.Radiography
A) STRAIGHT X-RAY - Before taking straight X-ray for KUB region (both
kidneys, ureters and bladder), the bowels must be made empty by giving laxative.
B) Excretory Urogram
4 Ultrasonography
Helpful to distinguish between opaque and non-opaque stones. It is also of
value in locating the stones for treatment with extra corporeal shock wave therapy.
5 Computed topography
Particularly helpful in the diagnosis of non-opaque stones.
6 Renal Scan
7 I nstrumental examination :- Cystoscopy
8 Examination of the stone
MANAGEMENT OF
NEPHROLITHIASIS
.
ASYMPTOMATIC CALCULI
TREATMENT
Solitary kidney
Occupation (pilot, business traveler
Simultaneous contralateral treatment
Its difficult to make an asymptomatic patient
feel any better !
STONE MANAGEMENT
OPTIONS
Open surgery
Percutaneous
nephrolithotomy
Ureteroscopy
Shock wave lithotripsy
Medical therapy
STONE MANAGEMENT
OPEN surgery NEPHROLITHOTOMY
SHOCK WAVE LITHOTRIPSY
.
SHOCK WAVE LITHOTRIPSY
STONE FRAGMENTATION
SHOCK WAVE
LITHOTRIPSY
INDICATIONS
Surgical stone
No obstruction
Reasonable chance
of expeditious removal
SHOCK WAVE
LITHOTRIPSY
RELATIVE CONTAINDICATIONS
Large stones
Calcium oxalate > 20 mm
Struvite > 30
mm
Cystine stones
Distal obstruction
Poorly informed patients
SHOCK WAVE LITHOTRIPSY
CLINICAL SIDE-EFFECTS
Hematuria
Pain
Obstruction
(Steinstrasse)
SHOCK WAVE
LITHOTRIPSY
IDEAL CANDIDATES
Small stone (< 1.5 cm)
Mid or upper pole location
Normal renal anatomy
No distal obstruction
SHOCK WAVE
LITHOTRIPSY
LIMITATIONS
Completeness of stone fragmentation
Completeness of fragment elimination
STONE MANAGEMENT
PERCUTANEOUS NEPHROLITHOTOMY
SURGICAL STONE
MANAGEMENT
CURRENT ROLE OF PNL
SURGICAL STONE
MANAGEMENT
STAY OUT OF TROUBLE
Pre-op KUB Pre-op IVP
URETERAL CALCULI
URETERAL CALCULI
TREATMENT OPTIONS
Observation
Shock wave lithotripsy
Ureteroscopy
Blind basket extraction
Percutaneous approach
Open surgery
.
.
FINAL
ACUTE AND CHRONIC
INTERSTITIAL NEPHRITIS
.
Morphology of the interstitium
Fibrosis develops after infiltration by
mononuclear cells (lymphocytes) which is
accompanied by deposition of fibronectin,
collagen type I, III, VI and IV.
There is a physiological balance between
ongoing matrix formation and - degradation.
Morphology of the interstitium
Composed of a loosely organized matrix
consisting of the collagen types I and III,
proteoglycans containing the interstitial
cells:
matrix producing fibroblasts
macrophages
dendritic reticulum cells
endothelial cells
Importance of interstitial cells
Interstitial fibroblasts:
Fibrogenesis
Production of erythropoietine (they lose this function
during the process of fibrogenesis)
Can transform into myofibroblasts (expression of SMA)
Changes in the interstitial area play an important negative
predictive value on the long term follow up of the primary
kidney disease. Important and determining factors are
interstitial volume (=fibrosis) and inflammation
Interferences with the
interstitium: broad
spectrum
Infection:
direct (BK virus, TBC, acute pyelonephritis),
indirect( Streptococci)
Immunologic
Allergic: drug induced
Auto-immune: Sjgren syndrome
Alloimmune: acute cellular allograft rejection
Unknown: IgG4- associated acute interstitial nephritis
Toxic: Pb poisoning, cadmium poisoning, Balkan endemic
nephropathy
Metabolic: oxalosis secondary to malabsorbtion , gout
Obstruction: ureteral- pelvic junction stenosis:
Radiation: radiation interstitial nephritis
Idiopathic: sarcoidosis
Different entities of interstitial disease
Acute interstitial nephritis
Chronic interstitial nephritis
Acute pyelonephritis
Chronic pyelonephritis (reflux related)
Xanthogranulomatous pyelonephritis
Malakoplakie
Myeloma kidney
IgG4 interstitial nephritis
Lead induced interstitial nephritis
Urate nephropathy
TX related Polyoma induced interstitial nephritis
Balkan interstitial nephritis
Acute interstitial nephritis
Most common etiologies are:
a) those related to the use of medications: 85%
b) those related to infectious agents: 10%
c) those associated to systemic disease or
glomerular diseases: 1%
d) idiopathic disease: 4%
Acute interstitial nephritis:
drugs
Etiology: AB (penicillins and cephalosporins, methicillin),
diuretics, NSAIDs, chinese herbs, lithium
Pathogenesis:
T cell mediated allergic - immune reaction on drug or drug-self
protein conjugate (hapten) later followed by accumulation of
lymphocytes, plasmocytes and histiocytes
Histology:
Early signs: oedema, lymphocytes focally
Later: eosinophils, lymphocytes, plasmocytes and histiocytes with
granuloma formation(with giant cells) in 30 %, especially after AB
Tubulitis (distal tubules): with breaks of TBM, necrosis of tubular
cells and atrophy and loss of tubules.
Tamm Horsfall may find its way to the interstitium (DD
obstruction of nephron).
Acute drug induced interstitial
nephritis
Granuloma
Oedema and focal inflammation
EOS
Granuloma
Acute drug induced interstitial
nephritis
Normally are the glomeruli not afflicted.
One exception: use of NSAIDs: can
combine ARF with Nephrotic Syndrome
(effect of cell- mediated lymphokine
directed reaction) inducing Minimal
Lesions (effacement of foot processes of
podocytes)
Acute interstitial nephritis:
clinics
Acute Renal Failure and
reduced glomerular
filtration rate:
- depends on the severity of
inflammation
- interstitial oedema causes
elevated intratubular pressure
- intratubular obstruction through
intra luminal cells
- tubular backleak
- vasoconstriction
- tubuloglomerular feedback
Outcome of drug- induced
interstitial nephritis
Recovery?
Drug withdrawal: 60-
90% in 1 to 12 mths
Irreversible with
analgesics, NSAIDs,
longterm use
Adverse prognostic
features
Marked interstitial
inflammation
Granuloma (50%
irreversible)
Tubular atrophy
Fibrosis
Acute interstitial infectious
nephritis
Infectious:direct invasion or remote infections
bacteria ( hemolytic streptococci), parasites
(Leishmania) and viruses (EBV, measles)
Pathogenesis: immunological hypersensitivity
reaction to the infectious agent, effect of
chemokines produced by the kidney in response
Histology:
Early signs: invasion by lymphocytes, eosinophils around the veins
In casu there is tubular destruction: histiocytes accumulate
Tubulitis with disappearance of the brush border in proximal
tubules
ACUTE INTERSTITIAL INFECTIOUS NEPHRITIS
Acute interstitial nephritis:
systemic
Association with: Goodpasture syndrome,
lupus nephritis, mixed cryoglobulinemia,
membranoproliferative glomerulonephritis
Chronic interstitial nephritis
Etiology: chronic drug intake (analgesics,
lithium), urinary obstruction, chronic reflux,
Pathogenesis: persistence of damageing factor:
ischemia, chronic immune reaction
Histology: fibrosis + diffuse infiltration by
lymphos, plasmos, histiocytes (with
granuloma). Tubular changes (atrophy,
compensatory hypertrophy with microcystic
changes)
Beware of:
Papillary necrosis, - sclerosis and- calcification: due to sclerosis
of the capillaries under the urothelial epithelium
Tumor development: papillary tumors, multifocal
Chronic interstitial nephritis
Papillary sclerosis
CIN
Interstitium in transplants
Calcineurin inhibitors:
Heart, liver, pancreas, kidney transplants in
different doses
Different levels of interstitial damage
Most structural nephrotoxic effects in arterioles
and glomeruli are manifestations of Thrombotic
MicroAngiopathy(TMA) with different patterns
of severity. The interstitial fibrosis has an
uncertain pathogenesis but is probably vascular.
Toxicity of calcineurin
inhibitors
Cellular rejection in kidney Tx
Histology:
Very early: eosinophils
Followed by T lymphocytes
Later: Plasmocytes IgG+ if IgM+ : be aware of
polyoma infection
In peritubular capillaries (PTC):
lymphocytes++
Cellular rejection
Tubulitis
CD3
Acute pyelonephritis
Etiology: ascending infection from the pyelon
Pathogenesis: microbial release of degradative
enzymes and toxic molecules, direct contact or
penetration of the host cell by the infectious agent
and the inflammatory response mediated by
antibodies, T cells
Histology:
Tubules are damaged by neutrophils (Congored)
Acute pyelonephritis
Chronic pyelonephritis
Etiology: reflux
Histology:
- wedge shaped interstitial fibrosis(follows the
traject of the papillae and ascending tubules)
accompanied by tubular atrophy, vascular
atheromatosis, glomerular sclerosis, inflammation
- outside the wedges: normal parenchyma but
with secondary changes in the glomeruli:
glomerular hypertrophy, FSGS
Chronic pyelonephritis
Chronic pyelonephritis
Tamm Horsfall protein
Tubular disease
Acute tubular damage:
Ischemia: vasoconstriction with endothelial activation
will determinate the extent of the tubular cell loss:
cellular, geographic, focal
Toxins:
Myoglobinuria
Heavy metal exposure (Pb, Cd)
Oxalate crystal deposits: ethylene glycol toxicity
Calcineurin inhibitors: megamitochondria, isometric
vacuolisation
Tubular damage
URETERAL CALCULI
Stone-free is not everything !!
PARAMETERS FOR COMPARISON
URETERAL CALCULI
Effectiveness
Morbidity
Convalescence
Cost
PARAMETERS FOR COMPARISON
SWL FOR
URETERAL CALCULI
Upper Middle Lowe
r
N=
33 N=248 N=381
Success
of 94.8% 85.9% 98.2
%
1
O
procedure
Re-tx rate 6.8% 15.7% 1.8%
Complications 10% 15.3% 8.4%
DORNIER HM-3
Lingeman, et al, 1993
DISTAL URETERAL CALCULI
URS is 10 - 18% more effective than SWL
(depending on type of SWL unit)
Morbidity / convalescence reduced with SWL
Need for stents 40-60% less with SWL
Cost issues not addressed in monotherapy studies
COMPARISON OF
MONOTHERAPY STUDIES
DISTAL URETERAL CALCULI
SWL URS
Effectiveness Slightly better
Morbidity Less
Hospitalization Less
Cost Slightly less
OVERVIEW OF HISTORICAL
CONTROL STUDIES
DISTAL URETERAL CALCULI
80 patients randomized to receive SWL or URS 40
patients had stones > 5 mm
40 patients had stones < 5 mm
SWL performed on Dornier MFL 5000
URS performed with 6.5F or 9.5F semi-rigid
ureteroscopes (basket vs. pneumatic lithotripsy)
PROSPECTIVE, RANDOMIZED TRIAL
Peschel & Bartsch, 1999
DISTAL URETERAL CALCULI
URS SWL
OR time (min) 19 63
Fluoro time (min) 0.8 5.1
Stone-free (days) 0.2 10.8
Stent (days) 7.2 0
Re-treatment
rate 0 1
5%
PROSPECTIVE, RANDOMIZED TRIAL
STONES < 5 MM
Peschel & Bartsch, 1999
*
*
*
*
*
SWL OF DISTAL
URETERAL CALCULI
Initial animal studies suggest ovarian trauma
Impaired fertility
Mutagenesis
Subsequent animal investigations demonstrate no
impact on fertility or offspring
Mice Rats Rabbits
ADVERSE EFFECTS TO
FEMALE REPRODUCTIVE TRACT?
SWL OF DISTAL
URETERAL CALCULI
Analyzed Rx data and radiation exposure
in 84 women of reproductive age
7 children born to 6 patients with no
malformations or chromosomal
anomalies
Miscarriages in 3 patients (but occurred
at least 1 year after SWL)
ADVERSE EFFECTS TO
FEMALE REPRODUCTIVE TRACT?
Viewig & Miller, 1992
URETEROSCOPY
URETERAL CALCULI
FLEXIBLE URETEROSCOPY
ANTEGRADE MANIPULATION OF
URETERAL CALCULI
Large stone burden
Body habitus
Urinary diversion
Transplant kidney
INDICATIONS
URETERAL CALCULI
PERCUTANEOUS APPROACH
URETERAL STONE
MANAGEMENT
Advantages
Minimal anesthesia requirements
Non-invasive procedure
No stenting/less complications
Similar approach for all ureteral
calculi
Disadvantages
Lower success rate than URS
Higher re-treatment rate
IN SITU SWL
URETERAL STONE
MANAGEMENT
URETEROSCOPY
Advantages
Highest success rate
Definitive Rx - No waiting for stone
passage
Disadvantages
More invasive than SWL
Higher complication rate
Requires greater technical expertise
URETERAL CALCULI: CURRENT
OPTIONS
PROX AND MID URETERAL STONES
Approach Invasive Stent S-F Rate Re-
RxRate
URS +++ 100% 75-90% 10-15%
Push/Smash ++ Rarely 92% 9%
SWL + Stent + 100% 75-80% 20-25%
In situ SWL 0 No 75-80% 20-25%
*
Defined as complete stone removal with single procedure
URETERAL CALCULI: CURRENT
OPTIONS
DISTAL URETERAL STONES
Approach Invasive Stent S-F Rate Re-
RxRate
URS +++ 100% 98-100% 0-2%
Push/Smash ++ Rarely 92% 9%
SWL + Stent + 100% 75-80% 20-25%
In situ SWL 0 No 75-80% 20-25%
*
Defined as complete stone removal with single procedure
SURGICAL STONE
MANAGEMENT
CHANGING TREATMENT
PHILOSOPHIES
1980s 1990s 2000s 20
10s
Shock wave lithotripsy 95% 85% 75% ???
Endoscopic procedures 5% 15% 25% ???
Open stone surgery < 1% < 1% < 1% 0
NEPHROLITHIASIS
Peak incidence age 30 - 60
Gender (Male : Female) 3 : 1
Family history 3 - fold risk
Body size risk with weight
Recurrence after first stone:
Year 1 10 - 15%
Year 5 50 - 60%
Year 10 70 - 80%
NATURAL HISTORY & RISK FACTORS
SHOCK WAVE LITHOTRIPSY
RECURRENT STONE
FORMATION
One Year Two Years
Post SWL Post SWL
Stone Free
New stones 8% 10%
Residual Stones
Stone growth 22% 21%
Lingeman, et al, 1989
SHOCK WAVE LITHOTRIPSY
EFFECT ON STONE RISK
FACTORS
Urine Values Pre- 3 Mo Post-
(mg/day) Lithotripsy Lithotripsy
Calcium 254 261
Uric Acid 552 548
Citrate 249 257
Oxalate 42 41
Brown, et al, 1989
MEDICAL MANAGEMENT OF
NEPHROLITHIASIS
PROGRESS
Elucidation
Urinary environment conducive to stone formation
Diagnosis
Detection of underlying physiologic abnormalities
Medical Therapy
Development of new treatment strategies
STONE FORMATION
Concentration / solubility of stone-forming
salts
Promoters of crystallization and aggregation
Inhibitors of crystallization and aggregation
MAJOR FORCES
DIETARY CALCIUM
Early recommendations suggest that low calcium diet
will decrease urinary Ca
++
excretion, thereby reducing
risk of stone formation
Potential risk factors involving low calcium diet:
Reduced bone mass
Increased urinary oxalate
IMPACT OF LOW CALCIUM DIET
DIETARY CALCIUM
Moderate calcium restriction in patients with
AH
Limit dietary intake of oxalate
Spinach, tea, chocolate, nuts
Limit dietary sodium intake
RECOMMENDATIONS
CALCIUM SUPPLEMENTS
Calciuric response to calcium supplementation
Depends on duration of treatment and patient
population
PHYSIOLOGICAL EVIDENCE
CALCIUM SUPPLEMENTS
Give HCTZ during initial three months to prevent
hypercalciuria, then discontinue for one month
If urinary calcium up at 4 months, re-start HCTZ
Alternative: Significantly increase fluid intake for
first three months and then check 24-hour urinary
calcium
RECOMMENDATIONS:
PREMENOPAUSAL WOMEN
Henoch Schnlein Purupura
Answer 1.
Renin Angiotensin II- ACE- ADH Aldosterone
That is not correct
Please try again
Peritoneal Dialysis
Is performed as an
intracorporeal (inside the
body) therapy making use of
the peritoneal membrane.
Is the process of cleaning the
blood by using the lining of
the peritoneal cavity
(peritoneum) as a filter the
peritoneum acts as a
dialyzing membrane,
permitting wastes from the
body to cross it and empty
into the instilled dialysate
fluid .
Is a type of dialysis usually
done by the patient at home.
Hemodialysis
3-4 times a week
Takes 2-4 hours
Machine filters
blood and
returns it to
body
Peritoneal Dialysis
Abdominal lining filters blood
3 types
Continuous ambulatory
Continuous cyclical
Intermittent
Вам также может понравиться
- Kidney Function and DiseasesДокумент70 страницKidney Function and DiseasesGovind SharmaОценок пока нет
- 01.introduction To Renal DiseaseДокумент55 страниц01.introduction To Renal DiseaseMusaОценок пока нет
- CHRONIC KIDNEY DISEASE Secondary To Chronic GlomerulonephritisДокумент31 страницаCHRONIC KIDNEY DISEASE Secondary To Chronic GlomerulonephritisJerwin Jade Bolor33% (3)
- GlomerulonephritisДокумент59 страницGlomerulonephritistressОценок пока нет
- Acute GlomerulonephritisДокумент17 страницAcute GlomerulonephritisBayanSecond WardОценок пока нет
- Glomerulonefritis Akut Dan Kronis: DR - Hasan Basri, Sppd-Kgh-FinasimДокумент53 страницыGlomerulonefritis Akut Dan Kronis: DR - Hasan Basri, Sppd-Kgh-FinasimnadddОценок пока нет
- Concept of CKDДокумент14 страницConcept of CKDMuhammad Aulia RahmanОценок пока нет
- t2 Kidney DiseaseДокумент52 страницыt2 Kidney Diseasewany.fyza54Оценок пока нет
- Glo Me Rulo NefritisДокумент58 страницGlo Me Rulo NefritisFany SholehaОценок пока нет
- F Kuliah-Nephritic Syndrome-FK UiSUДокумент40 страницF Kuliah-Nephritic Syndrome-FK UiSUandreОценок пока нет
- Triệu Chứng - Hội Chứng Bệnh Thận Y3Документ58 страницTriệu Chứng - Hội Chứng Bệnh Thận Y3trungОценок пока нет
- Chronic Kidney Disease NotesДокумент13 страницChronic Kidney Disease NotesSwathi MathiazhaganОценок пока нет
- OUM Tutorial 1 SBNS3504 RenalДокумент51 страницаOUM Tutorial 1 SBNS3504 RenalMashanimy HoneyОценок пока нет
- Presentation مسنين عمليДокумент19 страницPresentation مسنين عمليzoubia209Оценок пока нет
- NephrologyДокумент54 страницыNephrologyAndarge ImperialОценок пока нет
- Week 8 Activity Renal DiseasesДокумент3 страницыWeek 8 Activity Renal DiseasesHANNA CASANDRA GARCIAОценок пока нет
- Renal Diseaseppt2789Документ112 страницRenal Diseaseppt2789Sundeep SharmaОценок пока нет
- Nephrotic SyndromeДокумент23 страницыNephrotic SyndromeDivina Francia JovenОценок пока нет
- HTTPДокумент10 страницHTTPkasmiatiОценок пока нет
- Nephrotic SyndromeДокумент12 страницNephrotic SyndromePutra Fatkhul Rizqi QoroidОценок пока нет
- End Stage Renal Disease (ESRD)Документ39 страницEnd Stage Renal Disease (ESRD)siarahОценок пока нет
- Renal PathologyДокумент34 страницыRenal PathologyShanaz ShaxawanОценок пока нет
- Presented By: Sonia Dagar: Renal FailureДокумент40 страницPresented By: Sonia Dagar: Renal FailureRavanshi ThakurОценок пока нет
- 01 Renal System NotesДокумент22 страницы01 Renal System NotesLexanCantorFermoОценок пока нет
- Chronic Renal FailureДокумент54 страницыChronic Renal FailureAkia Cayasan BayaОценок пока нет
- GlomerulonephritisДокумент58 страницGlomerulonephritisJosa Anggi Pratama0% (1)
- Kidney Pathophysiology 2023Документ19 страницKidney Pathophysiology 2023Xerox and CompService Xerox and CompServiceОценок пока нет
- Glomerulonephritis-1 (Dr. Soffa)Документ58 страницGlomerulonephritis-1 (Dr. Soffa)Rahmailla Khanza Diana FebriliantriОценок пока нет
- Chronic Kidney Disease. GolwallaДокумент8 страницChronic Kidney Disease. GolwallaAbdul QuyyumОценок пока нет
- Nephrology Notes 2015Документ81 страницаNephrology Notes 2015Mahmoud Hussien100% (1)
- Nephrotic SyndromeДокумент5 страницNephrotic SyndromeAnjhiene CambaОценок пока нет
- Renal Failure PresentationДокумент110 страницRenal Failure PresentationMusa yohana100% (1)
- CKD - For Concept MappingДокумент7 страницCKD - For Concept MappingKennette Lim0% (1)
- CKD Part 2Документ49 страницCKD Part 2Pao AliОценок пока нет
- PART 9 Disorders of The Kidney and Urinary TractДокумент357 страницPART 9 Disorders of The Kidney and Urinary TractPhương HuỳnhОценок пока нет
- Nephritic Syndrome: Pyuza, MDДокумент41 страницаNephritic Syndrome: Pyuza, MDawadh mbaroukОценок пока нет
- Renal Physiology IIДокумент22 страницыRenal Physiology IIسمية صالحОценок пока нет
- NephritisДокумент16 страницNephritisyikesОценок пока нет
- Nephrologi NotesДокумент43 страницыNephrologi NotesSigit Harya HutamaОценок пока нет
- RenalДокумент36 страницRenalDumitru BrînzaОценок пока нет
- Renal Faliure 1Документ50 страницRenal Faliure 1180045Оценок пока нет
- Glomerulonephritis 10Документ5 страницGlomerulonephritis 10Eden Jay Calija AgoyОценок пока нет
- Multiple Organ Dysfunction Syndrome (MODS) : Inayatur Rosyidah., S.Kep - NsДокумент62 страницыMultiple Organ Dysfunction Syndrome (MODS) : Inayatur Rosyidah., S.Kep - Nsmahendra-kurniahОценок пока нет
- Renal Chart 2Документ21 страницаRenal Chart 2fortheloveofmedicineОценок пока нет
- IRC EngДокумент89 страницIRC EngMadalina SercaianuОценок пока нет
- Leg 5 Renal DisordersДокумент82 страницыLeg 5 Renal DisordersAleli DoОценок пока нет
- Nephrotic Syndrome - Armando HasudunganДокумент18 страницNephrotic Syndrome - Armando HasudunganzahraaОценок пока нет
- Renal Function TestsДокумент23 страницыRenal Function TestsKer YehunОценок пока нет
- Anatomical Position: Kidney StructureДокумент9 страницAnatomical Position: Kidney StructureRiny KhurshidОценок пока нет
- Renal Pathophysiology by GPTДокумент3 страницыRenal Pathophysiology by GPTphilipcОценок пока нет
- Chronic Kidney DiseaseДокумент7 страницChronic Kidney DiseaseLardel Balbiran LafortezaОценок пока нет
- ReferatДокумент53 страницыReferatHendri SaputraОценок пока нет
- Management: DiagnosisДокумент6 страницManagement: DiagnosisAhmed El-MalkyОценок пока нет
- Nephrotic Syndrome Case PresentationДокумент18 страницNephrotic Syndrome Case Presentationpritidinda3070Оценок пока нет
- NephritisДокумент5 страницNephritisPooja ChapdiОценок пока нет
- Chronic Kidney DiseaseДокумент40 страницChronic Kidney DiseasePaul SinsОценок пока нет
- Physiology for General Surgical Sciences Examination (GSSE)От EverandPhysiology for General Surgical Sciences Examination (GSSE)S. Ali MirjaliliОценок пока нет
- Potential Prospect 1.7Документ6 страницPotential Prospect 1.7Joshua M. GenoviaОценок пока нет
- 08 163 4 JPL ScheickДокумент50 страниц08 163 4 JPL ScheickSaqib Ali KhanОценок пока нет
- Clipsal RCD Tester 486D PDFДокумент4 страницыClipsal RCD Tester 486D PDF322399mk7086Оценок пока нет
- Child-Centered and Progressive EducationДокумент2 страницыChild-Centered and Progressive EducationDibyendu ChoudhuryОценок пока нет
- Case Diagnosis For RomanДокумент4 страницыCase Diagnosis For RomanChris Marie JuntillaОценок пока нет
- Broza Saric Kundalic - Ethnobotanical Study On Medicinal +Документ16 страницBroza Saric Kundalic - Ethnobotanical Study On Medicinal +turdunfloranОценок пока нет
- Adult Survivors Act Summons Against Mayor Eric AdamsДокумент3 страницыAdult Survivors Act Summons Against Mayor Eric AdamsCity & State New York100% (1)
- Narrative Pathophysiology of PregnancyДокумент2 страницыNarrative Pathophysiology of PregnancyMarvin ChulyaoОценок пока нет
- Nepal Health Research CouncilДокумент15 страницNepal Health Research Councilnabin hamalОценок пока нет
- COLLOIDAL GOLD RECIPE - CitrateДокумент9 страницCOLLOIDAL GOLD RECIPE - CitrateDevon Narok100% (4)
- Quarter 2 Week 5Документ54 страницыQuarter 2 Week 5rixzylicoqui.salcedoОценок пока нет
- Scenario of Shale Gas Exploration in IndiaДокумент24 страницыScenario of Shale Gas Exploration in IndiaManish TiwariОценок пока нет
- Phyilosophy of Midwifery Care 2Документ13 страницPhyilosophy of Midwifery Care 2Noella BezzinaОценок пока нет
- CR-7iA CR-4iA Installation and Setup Guide (B-83774JA-1 01)Документ1 страницаCR-7iA CR-4iA Installation and Setup Guide (B-83774JA-1 01)lidiia.pavlkukОценок пока нет
- Well Being Journal December 2018 PDFДокумент52 страницыWell Being Journal December 2018 PDFnetent00100% (1)
- NACH FormДокумент2 страницыNACH FormShreyas WaghmareОценок пока нет
- Network Access Control Quiz3 PDFДокумент2 страницыNetwork Access Control Quiz3 PDFDaljeet SinghОценок пока нет
- Final Plant Diversity Lab ReportДокумент6 страницFinal Plant Diversity Lab Reportapi-508660724Оценок пока нет
- 2 Avaliação Edros 2023 - 7º Ano - ProvaДокумент32 страницы2 Avaliação Edros 2023 - 7º Ano - Provaleandro costaОценок пока нет
- Vulnerability of The Urban EnvironmentДокумент11 страницVulnerability of The Urban EnvironmentKin LeeОценок пока нет
- Recognizing Fractures and Dislocations: Corpuz, Rachella Nicole PДокумент46 страницRecognizing Fractures and Dislocations: Corpuz, Rachella Nicole PRachella Nicole CorpuzОценок пока нет
- Music Recognition, Music Listening, and Word.7Документ5 страницMusic Recognition, Music Listening, and Word.7JIMENEZ PRADO NATALIA ANDREAОценок пока нет
- Boge FLEX PET SystemsДокумент4 страницыBoge FLEX PET SystemsAir Repair, LLCОценок пока нет
- Ens TecДокумент28 страницEns TecBorja CanalsОценок пока нет
- Supply Chain Logistics Manager in Dallas FT Worth TX Resume Calvin HarperДокумент2 страницыSupply Chain Logistics Manager in Dallas FT Worth TX Resume Calvin HarperCalvinHarperОценок пока нет
- TestДокумент233 страницыTestye rightОценок пока нет
- Structral DatasheetДокумент254 страницыStructral DatasheetdeepakОценок пока нет
- Review Factors Contributing To Medication Errors: A Literature ReviewДокумент9 страницReview Factors Contributing To Medication Errors: A Literature Reviewsoul_0602Оценок пока нет
- Voca-Book (This Must Be The Place)Документ13 страницVoca-Book (This Must Be The Place)Анастасия ВознесенскаяОценок пока нет
- Interview Questionaries (Cont.)Документ27 страницInterview Questionaries (Cont.)shubha christopherОценок пока нет