Академический Документы
Профессиональный Документы
Культура Документы
Diabetes Mellitus CPG
Загружено:
ejikieru03100%(3)100% нашли этот документ полезным (3 голоса)
2K просмотров157 страницClinical Practice Guidelines for the Diagnosis and Management of Diabetes Mellitus in Pediatric, Adult and Pregnant age group
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документClinical Practice Guidelines for the Diagnosis and Management of Diabetes Mellitus in Pediatric, Adult and Pregnant age group
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
100%(3)100% нашли этот документ полезным (3 голоса)
2K просмотров157 страницDiabetes Mellitus CPG
Загружено:
ejikieru03Clinical Practice Guidelines for the Diagnosis and Management of Diabetes Mellitus in Pediatric, Adult and Pregnant age group
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 157
CLINICAL PRACTICE
GUIDELINES FOR THE
DIAGNOSIS AND
MANAGEMENT OF DIABETES
MELLITUS
Ezekiel Arteta, M.D.
Charlene Bularan, M.D.
Department of Family and Community Medicine
Ospital ng Maynila Medical Center
OUTLINE
Definition of Diabetes Mellitus
Classification
Spectrum
Summary of the Clinical Practice
Guidelines for each Specialty:
Pediatrics (AAP)
Medicine (ADA and PSEM)
Obstetrics (POGS)
Pharmacology of Anti-Diabetic Drugs
DIABETES MELLITUS
Complex metabolic disorder characterized
by persistent hyperglycemia resulting from:
o Reduced insulin secretion
o Decreased glucose utilization
o Increased glucose production
CLASSIFICATION OF
DIABETES MELLITUS
Type 1 Diabetes (insulin-dependent/
Juvenile DM)
o Complete or near-total insulin deficiency
o Caused by the autoimmune destruction of -
cells of the pancreatic islets
o May be idiopathic
Type 2 Diabetes (noninsulin-dependent
DM)
o Variable degrees of insulin resistance, impaired
insulin secretion, and increased glucose
production
Gestational Diabetes Mellitus (Type 4)
o DM that is diagnosed for the first time in
pregnancy
DIFFERENTIATION BETWEEN
TYPE 1 AND TYPE 2 DM
DEFINITION OF DIABETES
MELLITUS
TEST WHO ADA Philippine
CPG
AACE IDF
Fasting
Plasma
Glucose
126 mg/dL (7.0 mmol/L)
2-h Plasma
Glucose
after 75-g
OGTT
200 mg/dL (11.1 mmol/L)
HbA1c 6.5%
Random
Plasma
Glucose
200 mg/dL (11.1 mmol/L) + symptoms
PRE-DIABETES
Impaired Fasting Glucose
o FPG of 100125 mg/dL (5.66.9
mmol/L) ADA, AACE, Phil. CPG
o FPG of 110125 mg/dL (6.16.9
mmol/L) WHO:
Impaired Glucose Tolerance
o 2h 75-g OGTT of 140199 mg/dL (7.8
11.0 mmol/L) ADA, WHO, AACE, Phil. CPG
Increased HbA1c (ADA)
o HbA1c level of 5.7 6.4% ADA, WHO, Phil. CPG
o HbA1c level of 5.5 6.4% AACE
DIABETES MELLITUS
IN THE PEDIATRIC
AGE GROUP
Sources:
American Academy of Pediatrics CPG on DMT2
American Diabetes Association CPG on DM
UNITE Philippines CPG on DM
SCREENING FOR DIABETES
MELLITUS
Screening for Type 1 diabetes among
children is NOT recommended because
the disease appears to be of low
prevalence; screening tests using
serologic markers are not readily available
and do not appear to be cost-effective; and
there are as yet no clearly effective
preventive approaches.
SCREENING FOR DIABETES
MELLITUS
Screening for pre-diabetes and Type 2 DM
is recommended among asymptomatic
children commencing at age10 years or at
onset of puberty , if puberty occurs at a
younger age (ADA) with the following risk
factors: (Grade C, Level 4):
o Overweight (BMI > 85
th
percentile for age and
sex, weight-for-height > 85
th
percentile, or
weight > 120% of ideal for height) OR
o Obese: BMI >95th centile or > +2SD
SCREENING FOR DIABETES
MELLITUS
Screening for pre-diabetes and Type 2 DM
is recommended among asymptomatic
children commencing at age10 years or at
onset of puberty , if puberty occurs at a
younger age (ADA) with the following risk
factors: (Grade C, Level 4):
o Plus any 2 of the following risk factors
Family history (especially parents and
grandparents) of Type 2 DM
Signs of insulin resistance (Acanthosis nigricans,
hypertension, dyslipidemia, PCOS, or small for
gestational age birth weight)
Maternal history of diabetes or GDM during the
childs gestation
SCREENING FOR DIABETES
MELLITUS
Should screening for Type 2 DM be done
in children?
o Screening for pre-diabetes and Type 2 DM is
recommended among asymptomatic children
commencing at age10 years or at onset of
puberty, if puberty occurs at a younger age
(ADA) with the following risk factors: (Grade C,
Level 4):
SCREENING FOR DIABETES
MELLITUS
DIABETES MELLITUS
IN THE ADULT AND
THE ELDERLY
Sources:
American Diabetes Association CPG on DM, 2013
UNITE Philippines CPG on DM
SCREENING
All individuals being seen at any
physicians clinic or by any healthcare
provider should be evaluated annually for
risk factors for type 2 diabetes and pre-
diabetes. (Table 2) (Grade D, Level 5)
Obesity, pre-diabetes, components of the
metabolic syndrome, PCOS, previous
GDM, family history and schizophrenia are
some of the risk factors for DM.
Universal screening using laboratory tests
is not recommended as it would identify
very few individuals who are at risk.
(Grade D, Consensus)
SCREENING
Laboratory testing for diabetes and
prediabetes is recommended for individuals
with any of the risk factors for Type 2 diabetes
mellitus. (Table 2) (Level 3-4, Grade B)
SCREENING
Testing should ideally be carried out within
the health \care setting (clinics, hospitals,
local health centers) because of the need
for follow-up and discussion of abnormal
results by qualified health care
professionals (nurse, diabetes educator,
physician). (Grade B, Level 3)
Testing at any setting should be
supervised by a qualified health care
professional. (Grade D, Level 5)
SCREENING
If initial test/s are negative for diabetes,
repeat testing should ideally be done
annually. (Grade D, Level 5)
DIAGNOSIS
The diagnosis of Diabetes Mellitus can be
made based on the following criteria*:
(Grade B, Level 2)
o Plasma glucose > 126 mg/dL (7.0 mmol/L) after
an overnight fast
o Two-hour plasma glucose > 200 mg/dl (11.1
mmol/l) during an Oral Glucose Tolerance Test
o A random plasma glucose > 200 mg/dl (11.1
mmol/l) in a patient with classic symptoms of
hyperglycemia (weight loss, polyuria,
polyphagia, polydipsia) or with signs and
symptoms of hyperglycaemic crisis.
DIAGNOSIS
*Among ASYMPTOMATIC individuals with
positive results, any of the three tests
should be REPEATED within two weeks
for confirmation. (Grade C, Level 4)
DIAGNOSIS
A 75-gram OGTT is preferred as the first
test in the following individuals who have:
(Grade B, Level 3)
A previous FBS showing Impaired Fasting
Glucose (100 to 125 mg/dL or 5.6 to 6.9
mmol/L)
Previous diagnosis of Cardiovascular Disease
(Coronary Artery Disease, Stroke, Peripheral
Arteriovascular Disease) or who are at high risk
for cardiovascular disease.
A diagnosis of Metabolic Syndrome
DIAGNOSIS
At the present time, we cannot
recommend the routine use of the
following tests for the diagnosis of
diabetes: (Grade C, Level 3)
o HBA1c (because of poor access and lack of
standardiazation)
o Capillary Blood Glucose
o Fructosamine
However, if a result is available upon consultation due to
prior testing, it should be interpreted with caution and should
be confirmed by any of the 3 tests that are considered
standard: fasting plasma glucose, oral glucose tolerance test
or random plasma glucose. (Grade B, Level 2)
DIAGNOSIS
We do not recommend the following tests
for the diagnosis of diabetes (Grade B,
Level 3):
o Urine glucose
o Plasma Insulin
MANAGEMENT AND
MONITORING
Initial evaluation - comprehensive medical
history and PE
o Coronary heart disease risk assessment
o Foot evaluation: assess risk for foot ulcer
(identify high-risk feet)
o Eye exam: fundoscopy on diagnosis
o Dental history or oral health history
MANAGEMENT AND
MONITORING
Minimal initial tests to be requested
Fasting blood glucose, complete lipid profile
HbA1c
Liver function tests
Urinalysis; spot urine albumin-to-creatinine ratio
Serum creatinine and calculated GFR
Optional tests
ECG and TET
TSH in type 1 diabetes, dyslipidemia or women
over age 50 y
GLUCOSE CONTROL
IDF AACE ADA
HBA1c 6.5% 6.5% < 7%
Preprandial plasma
glucose
< 110
mg/dL
< 110
mg/dL
70-130
mg/dL
Peak postprandial
glucose
NA < 140
mg/dL
< 180 mg/dL
Bedtime plasma
glucose
NA NA 110-150
mg/dL
*Goals should be individualized
*Certain populations require special considerations
*Less intensive glycemic goals may be individualized in
patients with frequent or severe hypoglycemia
MANAGEMENT AND
MONITORING
Glycemic targets
should be achieved
within 6 months of
diagnosis or first
prescription.
MANAGEMENT
The major components of the treatment of
diabetes are:
Diet and Exercise
A
Oral hypoglycaemic
therapy
B
Insulin Therapy
C
MANAGEMENT
Diet is a basic part of management in
every case. Treatment cannot be effective
unless adequate attention is given to
ensuring appropriate nutrition.
Dietary treatment should aim at:
Ensuring weight control
Providing nutritional requirements
Allowing good glycaemic control with blood
glucose levels as close to normal as possible
Correcting any associated blood lipid
abnormalities
Controlling of blood pressure
MANAGEMENT
Protein:
o Intake can range between 10-15% total energy
(0.8-1 g/kg of desirable body weight)
o Should be derived from both animal and
vegetable sources.
Recommended: One serving of protein from
animal sources every other day
MANAGEMENT
Carbohydrates:
Should be 50-60% of total caloric content of the
diet
Has the greatest effect on blood glucose
Enough Glucose available throughout the day
(not so much not little)
Consistent timing and composition of meals and
snacks from day to day
Evening snack helps prevent nocturnal
hypoglycemia
Whole grain
bread
Cereals
Legumes
Fruits and Vegetables
GI can raise Blood
glucose faster
GI can raise Blood
glucose slower
MANAGEMENT
Fats:
o Should provide 25-35% of total intake of
calories
o Saturated fat intake should not exceed 10% of
total energy.
o Cholesterol consumption should be restricted
and limited to 300 mg or less daily
o With elevated LDL and overweight
Saturated fat: limit to 7%
Cholesterol: limit to less than 200 mg daily
MANAGEMENT
Fats:
o Low intake of unsaturated fat + high
carbohydrate + low total fat + energy intake =
help lower LDL and cholesterol
o High monounsaturated fat diet
Lower postprandial rise in blood glucose, insulin,
and triglycerides
Does not improve fasting blood glucose
MANAGEMENT
Salt
o Excessive salt intake is to be avoided,
particularly in people with hypertension and
those with nephropathy.
MANAGEMENT AND
MONITORING
Initiate treatment with metformin for
monotherapy unless with contraindications
or intolerance of its ADEs
o Diarrhea
o Severe nausea
o Abdominal pain
MANAGEMENT AND
MONITORING
When optimization of therapy is needed,
choose the second drug according to the
following -
o Degree of HbA1c lowering
o Hypoglycemia risk
o Weight gain/loss
o Patient profile (dosing complexity,
renal/hepatic problems, other
contraindications and age)
Sequence of Antihyperglycemic Therapy (ADA, 2012)
MANAGEMENT AND
MONITORING
Since HbA1c reduction is the overriding
goal, the precise combination used may
not be as important as the glucose level
achieved.
There is no evidence that a specific
combination is any more effective in
lowering glucose levels or preventing
complications than another.
o SU + Pio = SU + Metformin (Hanefield et al, 2004 & Nagasaka et al, 2004)
o SU + Met = SU + DPP-IV inhibitors (?)
MANAGEMENT AND
MONITORING
The goal BP for most persons with
diabetes is <140/90 mm Hg.
o Lifestyle therapy alone for 3 months if pre-
hypertensive (SBP 130-139 mm Hg or DBP 80-
89 mm Hg)
o Pharmacologic + lifestyle therapy if SBP>140
mm Hg or DBP >90 mm Hg, or pre-
hypertensive uncontrolled with lifestyle therapy
alone
MANAGEMENT AND
MONITORING
ACE inhibitors & ARBs are generally
recommended as initial therapy. If one
class is not tolerated, the other should be
substituted.
Multiple drug therapy (>2 agents at
maximal doses) is generally required to
achieve BP targets. Thiazide-type
diuretics, calcium channel blockers and B-
blockers may be given as additional
agents.
MANAGEMENT AND
MONITORING
Recommendations are consistent with
Philippine Practice Guidelines for the
Treatment of Dyslipidemia.
LDL is the primary target for
dyslipidemia management in persons with
diabetes
MANAGEMENT AND
MONITORING
Statin therapy should be added to lifestyle
therapy, regardless of baseline levels for
diabetics
o With overt CVD (A)
o Without CVD who are >40 y and have 1 more
other CVD risk factors (A)
For patients at lower risk (e.g. without
overt CVD and <40 y), statin therapy
should be considered in addition to
lifestyle therapy if
LDL-C remains >100 mg/dL
Those with multiple risk factors (hypertension,
familial hypercholesterolemia, LVH, smoking, family history
of premature CAD, male sex, age >55 y, proteinuria,
albuminuria, BMI>25)
MANAGEMENT AND
MONITORING
The 100-70 rule
Without overt CVD, goal is LDL-C <100
mg/dL (2.6 mmol/L) [A]
With overt CVD, goal is LDL-C <70 mg/dl
(1.8 mmol/L). Use of high dose statin is an
option. [B]
MANAGEMENT AND
MONITORING
Insufficient evidence to recommend aspirin
for primary prevention in lower risk
individuals
o Men < 50 y
o Women <60 y
Clinical judgment if with multiple risk
factors
MANAGEMENT AND
MONITORING
Use aspirin therapy for secondary
prevention strategy in those with DM and a
history of CVD [A].
For patients with CVD and documented
aspirin allergy, clopidogrel (75 mg/day)
should be used.
Combination therapy of ASA (75-162
mg/day) and clopidogrel (75 mg/day) is
reasonable up to a year after an acute
coronary syndrome [B].
LIPID PROFILE, BLOOD
PRESSURE AND BMI TARGET
Parameter Ideal Acceptable Bad
TG <1.5 mmol/L
(150 mg/dl)
<2.2mmol/L > 2.2 mmol/L
TC < 4.5mmol/L
(200 mg/dl)
>4.5 mmol/L > 6.0 mmol/L
LDL < 2.5 mmol/L (100 mg/dl) < 4.4mmol/L > 4.4 mmol/L
HDL > 1.1 mmol/L
(40 mg/dl in men; 50
mg/dl in women)
0.9-1.1mmol/L < 0.9 mmol/L
BP < 130/80mmHg >130/80-
<140/90
> 140/90
BMI (Males) < 25 <27 27
BMI (Females) < 24 <26 26
MANAGEMENT AND
MONITORING
The following patients must be referred to
internists or diabetes specialists
(endocrinologists or diabetologists) -
o Type 1 diabetes
o Moderate to severe hyperglycemia
o Co-morbid conditions (infections, acute
CV events i.e. CHF or acute MI)
o Significant hepatic and renal
impairment
o Women with diabetes who are pregnant
CLINICAL PRACTICE
GUIDELINES FOR THE
DIAGNOSIS AND
MANAGEMENT OF DIABETES
MELLITUS
Ezekiel Arteta, M.D.
Charlene Bularan, M.D.
Department of Family and Community Medicine
Ospital ng Maynila Medical Center
CASE 3
A 29 y/o G1P0 26 weeks AOG by LMP, NIL
came in for pre-natal check-up.
VS: 140/90 (done twice) 89 20 37.0C
Patients FBS = 91 mg/dl at 26 weeks AOG.
Test was repeated at 32 weeks AOG which
revealed 114 mg/dl. UA revealed +1 albumin,
+1 sugar.
Diagnosis?
DIABETES MELLITUS
IN PREGNANCY
Source:
Philippine Obstetrics and Gynecology Society CPG
on DM
EPIDEMIOLOGY
7% of all pregnancies are complicated with
GDM worldwide
In PH, 1.9% of pregnant women admitted
have GDM
5.1% of Filipinas had DMT2 or GDM
according to POGS, Inc.
RISK FACTORS
Increase overall and abdominal obesity
Sedentary lifestyle and change in diet
(caloric diet)
Cigarette smoking
Inadequate cell response as seen
among Japanese population
LBW and undernutrition in utero
Genes (SEA descent)
Chronic infections (HBV and PTB)
Exposure to environmental irritants
Moderate Fe
++
overload i.e.,
hemoglobinopathies
ASSOCIATED DISEASES
Childhood autism
Fetal overnutrition (macrosomia) and
insulin resistance
COMPLICATIONS
COMPLICATIONS
SCREENING AND DETECTION
Recommendations for Filipino Pregnant
Women
DM recognized during pregnancy may be classified
as either GDM or overt DM based on plasma
glucose levels (Level III, Grade C)
Universal screening for GDM is recommended
among Filipino Gravidas (Level III, Grade B)
At 1
st
PNCU determine if gravida is high risk accdg
to history and risk factors (Level III, Grade B)
If low risk, with normal intial test (FBS, HBA1c or
RBS), screening should be done at 24-28 weeks
AOG using 2 hr 75g OGTT
SCREENING AND DETECTION
Recommendations for Filipino Pregnant
Women
If OGTT is normal at 24-28 weeks AOG, re-test at
32 wks AOG or earlier if there are sx of
hyperglycemia (3 Ps, plus polyhydramnios,
accelerated fetal growth)
OGTT should be performed in the morning after an
overnight fasting of 8-14 hours.
o Have an unrestricted diet 3 days or more prior
to testing, i.e., >/ 150 g of CHO per day
o Do not smoke and remain seated during the
test
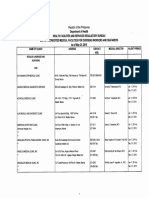
GDM WHO ADA POGS
FBS >125 mg/dL (6.9
mmol/L)
>92 mg/dL
(5.1
mmol/dL)
>92 mg/dL
(5.1
mmol/dL)
Overt: >/126
mg/dl (7
mmol/L)
1 hr >180 mg/dL (10
mmol/dL)
2 hr >140 mg/dL (7.8
mmol/dL)
>153 mg/dL
(8.5
mmol/dL)
>140 mg/dL
(7.8
mmol/dL)
Overt: >/
200mg/dL
(11.1
mmol/L)
TREATMENT
DIET! Medical Nutrition therapy
o For normal-weight women (BMI: 20-25
kg/m
2
) 30 kcal/kg should be prescribed;
o For overweight and obese women (BMI
> 24-34 kg/m
2
) calories should be
restricted to 25 kcal/kg,
o For morbidly obese women (BMI > 34
kg/m
2
) calories should be restricted to
20 kcal/kg or less
TREATMENT
Weight Management weight gain
recommendations for women with GDM
who had normal weight or were
underweight prepregnancy is the same as
for those without GDM
Energy intake for overweight or obese
women with GDM may be modestly
restricted as long as weight gain is
appropriate while minimizing risk of
ketosis.
TREATMENT
Lifestyle changes cessation of smoking
and counseling about alcohol
consumption.
The most important
thing in the reduction
of complications
among women with
GDM is glycemic
control
GOALS OF MANAGEMENT
OUTPATIENT GLUCOSE TRAGETS FOR
PREGNANT WOMEN
For GDM treatment goals are:
- Pre-prandial glucose concentration of
95mg/dL (5.3 mmol/L)
- 1-hour postmeal glucose value of
140mg/dL (7.8 mmol/L)
- 2-hour post meal glucose value of
120mg/dL (6.7 mmol/L)
GOALS OF MANAGEMENT
For women with pre-existing DM type I or
II who become pregnant, goals are:
- Premeal, bedtime, and overnight glucose
values of 60-99mg/dL (3.3-5.4 mmol/L)
- Peak post prandial glucose value of 100-
129mg/dL (5.4- 7.1 mmol/L)
- HbA1c of 6%
TREATMENT
The optimal treatment for
women with GDM or type 2
DM who are not able to
maintain normoglycemia with
CHO restricted diet
INSULIN
TREATMENT
Dosages:
- 0.7-0.8 U/kg BW on 1
st
trimester
- 1.0 U/kg BW on 2
nd
trimester
- 1.2 U/kg BW on 3
rd
trimester
- 2/3 given before breakfast, 1/3 given before dinner
(NPH insulin)
- Regular insulin and rapid acting insulin are best
dosed with each meal
TREATMENT
Oral Hypoglycemic Agents use?
o ACOG and the ADA do not currently
recommend oral hypoglycemic
agents.
PHARMACOLOGY OF
ANTI-DIABETIC
DRUGS
Source:
Pharmacotherapy 101 by Dr. Agnes Cruz
Sequence of Antihyperglycemic Therapy (ADA, 2012)
ORAL
HYPOGLYCEMIC
AGENTS
Source: Pharmacotherapy 101 by Dr. Agnes Cruz
There are currently six classes of oral anti-
diabetic agents:
Biguanides
Insulin Secretagogues Sulphonylureas
Insulin Secretagogues Non-sulphonylureas
-glucosidase inhibitors
Thiazolidinediones (TZDs)
DPP-IV Inhibitors
Drug Class Agents Mechanism of Action
Alpha-glucosidase
inhibitors
Acarbose
Voglibose
Delay intestinal
carbohydrate absorption
Biguanides Metformin
Hepatic glucose
production
Liver and muscle insulin
sensitivity
Insulin
secretagogues
sulfonylureas
Glimepiride
Glipizide
Glyclazide
Glibenclamide (glyburide)
insulin secretion
Insulin
secretagogues
Meglitinides
Nateglinide, Repaglinide insulin secretion
DPP-IV Inhibitors
Sitagliptin
Vildagliptin
Saxagliptin
Postrandial insulin
secretion,
glucagon secretion,
Delay gastric emptying
Thiazolidinediones
Pioglitazone
Rosiglitazone
Adipose and muscle
insulin sensitivity
Biguanide: METFORMIN
Primary effects are to decrease hepatic
glucose production and increase insulin-
mediated peripheral glucose uptake
Efficacy:
HbA1c
1-2%
11-22 mmol/mol
FPG
40-70 mg/dl
2.2-3.9 mmol/mol
METFORMIN
SIDE EFFECTS
CONTRAINDICATIONS
DRUG
INTERACTION
Preparation
Lactic acidosis
(rare; in patients
with CHF)
Diarrhea and
abdominal
discomfort
Weight loss
Kidney failure
Liver disease
Lactic acidosis
Cimetidine
Furosemide
Nifedipine
Tablets: 500, 850,
and 1000 mg.
Tablets (extended
release): 500, 750,
and 1000 mg.
Solution: 500 mg/5
ml
Usual dose:
o 500 mg BID to TID
Max dose:
o 850 mg TID to 3g/day
Max effective dose:
o 1000 mg BID
METFORMIN
BRAND
NAME
STOCK
DOSE
PRICE
RiteMed 500 3.09
Gludin 500 3.20
Neoform 500 3.35
Diamet 500 500 3.50
Pharex 500 3.75
Nidcor 500 4.32
Winthrop 500 4.50
Diafat 500 5.19
Glucoform 500 5.60
I-Max 500 5.60
BRAND
NAME
STOCK
DOSE
PRICE
Melta-SE 500 6.00
Neomet 500 6.00
Panfor SR 500 6.50
Ansures
MR
500 7.00
Glumet 500 7.22
Fornidd 500 7.40
Euform
Retard
850 8.90
Humamet 500 9.40
Glucophage 500, 750,
850
Secretagogues
These medications try to replace
the natural stimulus for beta
cells to secrete insulin.
SULFONYLUREAS
Efficacy:
HbA1c
1-2%
11-22 mmol/mol
FPG
40-70 mg/dl
2.2-3.9 mmol/mol
Short-acting:
o Tolbutamide
Intermediate-acting:
o Tolazamide
o Glipizide
o Glyburide/ Glibenclamide
Long-acting:
o Chloropropamide
o Glimepiride
SULFONYLUREAS
SIDE EFFECTS CONTRAINDICATIONS DRUG INTERACTION
Hypoglycemia
Weight gain
IDDM
DKA
Diabetic Coma
Pregnancy, Lactation
(next slide)
Short-acting:
o Tolbutamide: not available
Intermediate-acting:
o Tolazamide: not available
o Glipizide: Minidiab 5,10mg OD max: 40mg/d
o Glyburide/ Glibenclamide: Daonil 5mg Maintenance: 5-10 mg/day
Long-acting:
o Chloropropamide: not available
o Glimepiride: Aforglim 2, 3 mg OD
o Glicazide: Diamicron 30, 80mg OD
SULFONYLUREAS
BRAND
NAME
GENERIC
NAME
STOCK
DOSE
PRICE
Benmide Glibenclamide 5 0.75
Azukon
MR
Gliclazide 30 3.95
Euglodin Glibenclamide 5 4.00
Glazide Gliclazide 80 4.00
Euglotab Glibenclamide 5 4.50
Zebet Gliclazide 80 4.50
Glicla Gliclazide 30 5.00
Gliget MR Gliclazide 30 5.45
Daonil Glibenclamide 5 5.48
Getz Gliclazide 30 6.00
Clibite Gliclazide 80 6.00
Allase Glibenclamide 5 6.09
Orabetic Glibenclamide 5 6.16
Gluconil Gliclazide 80 6.28
BRAND
NAME
GENERIC STOCK
DOSE
PRICE
Clizid Gliclazide 80 7.00
Gluban Glibenclamide 5 7.00
Glubitor Gliclazide 80 7.08
Glimax Glipizide 5 7.43
Dianorm Gliclazide 80 7.62
Brilizid Glipizide 5 7.80
Diaberid Glimepiride 2 8.00
Lodulce Glibenclamide 5 8.00
Rimepril Glimepiride 2 9.00
Diamicron Gliclazide 80 9.10
Diamicron
MR
Gliclazide 30 9.10
Acotril Glimepiride 2 9.61
SULFONYLUREAS
BRAND
NAME
GENERIC
NAME
STOCK
DOSE
PRICE
Arya Glimepiride 2 9.90
Aforglim 2 Glimepiride 2 9.96
Neoglim Glimepiride 2 10.50
Euglucon Glibenclamide 5 10.81
Glipiren Glimepiride 2 11.83
Euglim Glimepiride 2 12.00
Glimesyn Glimepiride 2 12.00
Diaglim Glimepiride 2 12.33
Glimed Glimepiride 2 14.00
Getryl Glimepiride 2 14.15
Winthrop Glimepiride 2 14.60
Azulix Glimepiride 2 15.00
Glimarex Glimepiride 2 15.00
Mira Glimepiride 2 15.00
Norizec Glimepiride 2 15.11
BRAND
NAME
GENERIC STOCK
DOSE
PRICE
Sulfast Glimepiride 2 15.40
Amara 4 Glimepiride 4 15.75
Soladin Glimepiride 2 16.00
Minidiab Glipizide 5 19.35
Solosa Glimepiride 2 21.93
MEGLITINIDES
Efficacy:
HbA1c
0.5-1.5%
5.5-16.5 mmol/mol
FPG
20-60 mg/dl
1.1-3.3 mmol/mol
PPG
75-100 mg/dl
4.2-5.6 mmol/mol
MEGLITINIDES
SIDE EFFECTS CONTRAINDICATIONS DRUG INTERACTION
Hypoglycemia (less)
Weight gain
DKA
T1DM
Pregnancy and Lactation
NSAIDs
Salicylates
MAOIs
Nonselective -blockers
Thiazides
Corticosteroids
Thyroid preparation
Sympathomimetics
Oral antidiabetic agents
CYP2C9 inhibitors
MEGLITINIDES
BRAND
NAME
GENERIC
NAME
STOCK
DOSE
PRICE
Novonorm Repaglinide 0.5 15.67
Starlix Nateglinide 120 31.27
Nateglinide: Starlix 120mg/tab TID
Repaglinide Novonorm 0.5,1.2mg- TID
ALPHA-GLUCOSIDASE
INHIBITORS
Efficacy:
HbA1c
0.5-1%
5.5-11 mmol/mol
FPG
10-20 mg/dl
0.5-1.1 mmol/mol
PPG
40-50 mg/dl
2.2-2.8 mmol/mol
ALPHA-GLUCOSIDASE
INHIBITORS
SIDE EFFECTS CONTRAINDICATIONS DRUG INTERACTION
Flatulence
Abdominal discomfort
Chronic intestinal
disorders associated w/
distinct disturbances of
digestion & absorption,
conditions which may
deteriorate as a result of
increased intestinal gas
formation.
Patients w/ CrCl <25
mL/min/1.73 mL, hepatic
impairment.
Pregnancy & lactation.
Patients <18 yr.
Cholestyramine, intestinal
absorbents & digestive
enzymes may attenuate
its effect
ALPHA-GLUCOSIDASE
INHIBITORS
BRAND
NAME
GENERIC
NAME
STOCK
DOSE
PRICE
Basen Voglibose 0.2 12.35
Glucobay Acarbose 50 12.96
Acarbose: 50, 100mg/tab, TID
Miglitol (glyset) NA
Voglibose (Basen)- 0.2-0.3 mg/ TID
THIAZOLIDINEDIONES
Increase the sensitivity of muscle and
adipose cells to insulin and suppressing
hepatic glucose production
Inhibit hepatic gluconeogenesis
Stabilize beta cell dysfunction
Efficacy:
HbA1c
0.5-1.5%
5.5-16.5 mmol/mol
FPG
20-55 mg/dl
1.1-3.1 mmol/mol
THIAZOLIDINEDIONES
SIDE EFFECTS CONTRAINDICATIONS DRUG INTERACTION
Weight gain
Edema
Risk of fractures
Patients with abnormal
liver function
CHF patients
Other antidiabetic agents
-blockers
Salicylic acid preparation
MAOIs
Fibrate derivatives
Warfarin
Epinephrine
Adrenocortical & thyroid
hormone
CYP2C8 inducer eg
rifampicin & inhibitor eg
gemfibrozil
Pioglitazone - 15mg, 30mg/tab, OD
Rosiglitazone - not available inc risk for CVD
Troglitazone (Rezulin), which was withdrawn from the market
due to an increased incidence of drug-induced hepatitis.
THIAZOLIDINEDIONES
BRAND
NAME
GENERIC
NAME
STOCK
DOSE
PRICE
Pioglon Pioglitazone 15 3.50
Insulact Pioglitazone 15 14.18
Prialta Pioglitazone 15 15.88
Glitaz Pioglitazone 15 15.92
Piozone Pioglitazone 15 16.98
Diabetone Pioglitazone 15 17.25
Zolid Pioglitazone 15 17.75
Ppar Pioglitazone 30 18.00
Piozar Pioglitazone 30 18.50
Actos Pioglitazone 15 67.58
DPP-4 INHIBITORS
Efficacy:
HbA1c
0.5-1%
5.5-11 mmol/mol
FPG
20 mg/dl
1.1 mmol/mol
PPG
45-55 mg/dl
2.5-3.1 mmol/mol
DPP-4 INHIBITORS
SIDE EFFECTS CONTRAINDICATIONS DRUG INTERACTION
Generally well tolerated
Low risk of hypoglycemia
Not associated with weight
gain
Upper respiratory tract
infection has been
reported in clinical studies
Type 1 DM
Diabetic ketoacidosis
Digoxin
Cyclosporine
Sitagliptin (Januvia): 25, 50,100mg/film
coated tab OD
Vildagliptin (Galvus): 50mg/tab OD-BID
Saxaglitpin (Onglyza): 2.5, 5mg OD
Linagliptin (Trajenta): 5mg OD
DPP-4 INHIBITORS
BRAND
NAME
GENERIC
NAME
STOCK
DOSE
PRICE
Galvus Vildagliptin 50 27.15
Onglyza Saxagliptin 5 52.04
Trajenta Linagliptin 5 52.07
Januvia Sitagliptin 25, 50,
100
52.14
Glucagon-like Peptide 1
agonist
Aka incretin mimetics
is an insulin secretagogue, with
glucoregulatory effects.
for patients whose diabetes was not well-
controlled on other oral medications.
GLUCAGON-LIKE PEPTIDE 1
AGONISTS
Efficacy:
HbA1c
1-2%
11-22 mmol/mol
FPG
5.76-11.7 mg/dl
0.32-0.65 mmol/mol
PPG
6.12-17.28 mg/dl
0.34-0.96 mmol/mol
GLUCAGON-LIKE PEPTIDE 1
AGONISTS
SIDE EFFECTS CONTRAINDICATIONS DRUG INTERACTION
Moderate and transient
nausea, vomiting and
diarrhea
Low risk of hypoglycemia
and no evidence of
increased CV risk
Not for type 1 DM or
diabetic ketoacidosis.
Do not use in end-stage
renal disease or severe
renal impairment (<30
mL/min), severe GI
disease
May increase
hypoglycemia when used
w/ a sulfonylurea. OC,
antibiotics, warfarin
Exenatide (Byetta): 250mcg/mL
5mcg/dose bid SC
Liraglutide (Victoza): 6mg/mL , 3mL 0.6ml
SC daily
COMBINATION THERAPY
BRAND NAME GENERIC NAME STOCK
DOSE
PRICE
Azulix MF Glimepiride + Metformin 1+500 8.00
Euglo Plus Glibenclamide + Metformin 2.5+400 9.28
Glimet Glimepiride + Metformin 2+500 14.00
Zolid Plus Pioglitazone + Meformin 15+500 16.98
Pioplus Pioglitazone + Meformin 15+500 16.98
Prialta-Met Pioglitazone + Meformin 15+500 17.57
Solozamet Glimepiride + Metformin 2 +500 21.93
Zoliget Pioglitazone + Glimepiride 30+2 24.55
Galvusmet Metformin + Vildagliptin 500+50 28.18
Janumet Sitagliptin + Metformin 50+500 28.57
Velmetia Sitagliptin + Metformin 50+500 29.43
Actosmet Pioglitazone + Metformin 15+850 33.93
INSULIN THERAPY
Insulin Therapy
Characteristics
Onset is the length of time before insulin
reaches the bloodstream and begins
lowering blood glucose.
Peaktime is the time during which insulin is
at maximum strength in terms of lowering
blood glucose.
Duration is how long insulin continues to
lower blood glucose.
INSULIN
Insulin Therapy Indications
o Short-Term Use:
Acute illness, surgery, stress and
emergencies
Pregnancy
Breast-feeding
Insulin may be used as initial therapy in type
2 diabetes in marked hyperglycaemia
Severe metabolic decompensation (diabetic
ketoacidosis, hyperosmolar nonketotic
coma, lactic acidosis, severe
hypertriglyceridaemia)
INSULIN
Insulin Therapy
o Long-Term Use:
If targets have not been reached after
optimal dose of combination therapy or
BIDS, consider change to multi-dose insulin
therapy. When initiating this, insulin
secretagogues should be stopped and
insulin sensitisers e.g. Metformin or TZDs,
can be continued.
Dosing: 0.3 1.5/kg BW
Rapid-acting Insulin: Lispro 100IU/ml 3mL
(P705.00/cartridge or pen); aspart
100IU/ml 3mL (P724.00/pen): immediately
before meals
Short-acting: Humulin-R 100IU/mL, 3mL
vial (P1,200): 30 mins before meals
Intermediate-acting: Humulin-N 100IU/mL,
3mL (P526.00/cartridge): AM and PM
Long-acting: glargine 100IU/mL, 10mL
(P2303.00/vial); detemir 100IU/mL, 3ml
(P844.00/pen) PM or bedtime
Pre-mixed
Humulin 70/30 (70% NPH 30% regular
insulin) Combination of int. acting + SA
Novomix 30 (70% aspart protamine 30%
aspart )
Humalog mix 25 (75% lispro protamine,
25% lispro)
Insulin Regimen
To augment beta cell function (0.3
U/kg) prevents gluconeogenesis during
bedtime
- BIDS (Bedtime Insulin dailytime SU)
- Example: Gliclazide 80mg OD + Humulin
N 10U SC at bedtime
To replace beta cell function (0.6-1.0
U/kg) basal and meal-related (bolus)
requirements
- Split dose 2/3 1/3 rule given before
breakfast/dinner respectively
- Split-mixed: Insulatard (int.) 20U +
Actrapid (S.A) 6U before breakfast then
Insulatard (int.) 10U + Actrapid (S.A) 6U
before dinner
- Modified split-mixed: Humulin N 16U
(intermediate acting) + Humulin R 4 U
(short acting) before breakfast then
Humulin R 6 U at lunch then Humulin N 8U
(intermediate acting) + Humulin R 4 U
(short acting) before dinner
- Basal plus Regimen: Lantus 20U (basal
insulin) OD + Humalog (S.A) 10U before
lunch
- Basal Bolus Regimen: Pre-meal SA +
basal insulin i.e., Actrapid 10U SC premeals
TID + Humulin N 20U at bedtime
TREATMENT ALGORITHM FOR
PEOPLE WITH T2DM (IDF)
THANK YOU!
Вам также может понравиться
- Aub Pogs CPGДокумент39 страницAub Pogs CPGVenz Timothy Wesley LandichoОценок пока нет
- FM Cases OpdДокумент13 страницFM Cases Opdejikieru03Оценок пока нет
- CC Silva - Rationalization 2022: # Rationale Answer: C. Contained in The Vestibule RationaleДокумент34 страницыCC Silva - Rationalization 2022: # Rationale Answer: C. Contained in The Vestibule RationaleNicole Xyza JunsayОценок пока нет
- Internal Medicine Quiz 4 DiabetesДокумент13 страницInternal Medicine Quiz 4 DiabetesenzocruzinОценок пока нет
- 1) Benign Gynecologic Lesions - FINALДокумент121 страница1) Benign Gynecologic Lesions - FINALJed Mostajo100% (1)
- CPG POGS Cesarean SectionДокумент65 страницCPG POGS Cesarean SectionAngela Caguitla100% (4)
- CPG UrogynecologyДокумент71 страницаCPG UrogynecologyDjurizzaBustamanteGadin100% (2)
- 2022 Pogs Annual Convention SP Rev3 Final - CompressedДокумент292 страницы2022 Pogs Annual Convention SP Rev3 Final - CompressedKaye HernandezОценок пока нет
- OB - Normal Labor and DeliveryДокумент51 страницаOB - Normal Labor and DeliveryJosh Matthew Rosales33% (3)
- OBGYN Revalida Review 2019Документ74 страницыOBGYN Revalida Review 2019anonymous100% (1)
- Philippine Clinical Practice Guidelines UTIДокумент95 страницPhilippine Clinical Practice Guidelines UTIToy Gallo100% (2)
- CPG AbortionДокумент40 страницCPG AbortionKatharine Nerva75% (12)
- FCM - The Impact of Illness To The FamilyДокумент4 страницыFCM - The Impact of Illness To The FamilyEzekiel Arteta50% (2)
- Air Augmented Rocket (285pages) Propulsion ConceptsДокумент285 страницAir Augmented Rocket (285pages) Propulsion ConceptsAlexandre PereiraОценок пока нет
- Preeclampsia UpToDateДокумент60 страницPreeclampsia UpToDateMauricio Marin MontoyaОценок пока нет
- Mcu-Fdt Medical Foundation Hospital Out Patient Services: Chief Complaint: History of Present IllnessДокумент2 страницыMcu-Fdt Medical Foundation Hospital Out Patient Services: Chief Complaint: History of Present IllnessvinbОценок пока нет
- Peptic Ulcer DiseaseДокумент75 страницPeptic Ulcer DiseaseSarah Gaile Tio Inac100% (4)
- Saptamsa - D7Документ4 страницыSaptamsa - D7Nabeel IrfanОценок пока нет
- Sgop CPGДокумент93 страницыSgop CPGjojolilimomo100% (2)
- Sgop CPG 2008 FinalДокумент105 страницSgop CPG 2008 FinalVia Alip100% (2)
- AUB Case DiscussionДокумент42 страницыAUB Case DiscussionHafsah G.100% (1)
- Hypertension in Pregnancy (Pogs-Cpg)Документ60 страницHypertension in Pregnancy (Pogs-Cpg)Ivy Combista Baya100% (1)
- CPG-Abnormal Labor and Delivery 2009Документ29 страницCPG-Abnormal Labor and Delivery 2009lovelots123488% (8)
- CPG DM PDFДокумент110 страницCPG DM PDFLisa KriestantoОценок пока нет
- Hypertension in Pregnancy (Pogs-Cpg)Документ55 страницHypertension in Pregnancy (Pogs-Cpg)Philip Piolo Fuego67% (3)
- SGOP 2008 (Guidelines On Management)Документ87 страницSGOP 2008 (Guidelines On Management)Via Alip100% (1)
- Rite BlueprintДокумент11 страницRite BlueprintTal Lagura100% (1)
- (Durt, - Christoph - Fuchs, - Thomas - Tewes, - Christian) Embodiment, Enaction, and Culture PDFДокумент451 страница(Durt, - Christoph - Fuchs, - Thomas - Tewes, - Christian) Embodiment, Enaction, and Culture PDFnlf2205100% (3)
- ThermodynamicsДокумент341 страницаThermodynamicsjonathan2788100% (4)
- Gyne Onco Interns NotesДокумент54 страницыGyne Onco Interns NotesCoy NuñezОценок пока нет
- Benign Prostatic Hyperplasia: Philippine Urological Association, IncДокумент7 страницBenign Prostatic Hyperplasia: Philippine Urological Association, Incsam_llamzon100% (1)
- CPG-3rd Trimester Bleeding and Postpartum Hemorrage 2009Документ107 страницCPG-3rd Trimester Bleeding and Postpartum Hemorrage 2009lovelots1234100% (8)
- Pedia Notes Compilation MKDoseДокумент18 страницPedia Notes Compilation MKDosemefav7778520Оценок пока нет
- Diabetes Mellitus: Investagtion, Diagnosis & Management: DR - Vivek Reddy 1 M.D.SДокумент36 страницDiabetes Mellitus: Investagtion, Diagnosis & Management: DR - Vivek Reddy 1 M.D.SBHEEMREDDY VIVEKREDDY100% (1)
- Philippine Obstetrical and Philippine Obstetrical and Gynecological Society (POGS), Foundation, Inc. Gynecological Society (POGS), Foundation, IncДокумент51 страницаPhilippine Obstetrical and Philippine Obstetrical and Gynecological Society (POGS), Foundation, Inc. Gynecological Society (POGS), Foundation, IncJanna Janoras ŰОценок пока нет
- Clinical Practice Guidelines On: TetanusДокумент45 страницClinical Practice Guidelines On: TetanusHighDee FilmsОценок пока нет
- Clincal Practice Guidelines For Diabetes in The PhilippinesДокумент40 страницClincal Practice Guidelines For Diabetes in The PhilippinesRans NosceОценок пока нет
- Resident'S Review: A Webinar Series: PRENATAL CARE by Dr. Cagayan Goals of Prenatal CareДокумент12 страницResident'S Review: A Webinar Series: PRENATAL CARE by Dr. Cagayan Goals of Prenatal CareAngela SaldajenoОценок пока нет
- Topnotch Mnemonics September 2016Документ6 страницTopnotch Mnemonics September 2016Lian BaylosisОценок пока нет
- Introduction To E-Business SystemsДокумент19 страницIntroduction To E-Business SystemsArtur97% (79)
- POGS CPG Abnormal Uterine BleedineДокумент36 страницPOGS CPG Abnormal Uterine Bleedinejandale57% (7)
- CPG PSSTDДокумент40 страницCPG PSSTDotartil_niman100% (2)
- Creating Literacy Instruction For All Students ResourceДокумент25 страницCreating Literacy Instruction For All Students ResourceNicole RickettsОценок пока нет
- CPG Gestational Trophoblastic DiseasesДокумент31 страницаCPG Gestational Trophoblastic DiseasesSMR50% (2)
- Clinical Practice Guidelines For The Obstetrician - GynecologistДокумент79 страницClinical Practice Guidelines For The Obstetrician - GynecologistAngela Caguitla67% (3)
- Sample Internship PPTДокумент19 страницSample Internship PPTSangeeta JamadarОценок пока нет
- Diabetes MellitusДокумент181 страницаDiabetes MellitusrogerОценок пока нет
- Arif Dirlik - The Origins of Chinese Communism-Oxford University Press, USA (1989)Документ335 страницArif Dirlik - The Origins of Chinese Communism-Oxford University Press, USA (1989)Denisa FeisalОценок пока нет
- Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino WomenДокумент7 страницOb 1.05 Clinical Practice Guidelines On Immunization For Filipino Womenotartil_niman50% (2)
- LET Facilitating Learning EDITED3Документ12 страницLET Facilitating Learning EDITED3Likhaan PerformingArts HomeStudio100% (5)
- CPG Anemia Pogs 2009Документ38 страницCPG Anemia Pogs 2009Mark Cristopher JoaquinОценок пока нет
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Clinical Practice Guidelines Einc 2014Документ52 страницыClinical Practice Guidelines Einc 2014dennisreveni100% (1)
- Diabetes Mellitus CPGДокумент90 страницDiabetes Mellitus CPGKristine-Joy Legaspi FrancoОценок пока нет
- GTDДокумент56 страницGTDRendy Adhitya PratamaОценок пока нет
- Sample Case ProtocolДокумент6 страницSample Case ProtocoljheyfteeОценок пока нет
- Chap 8 Prenatal CareДокумент10 страницChap 8 Prenatal CareRem AlfelorОценок пока нет
- Planes and Diameters of The PelvisДокумент32 страницыPlanes and Diameters of The PelvisRumelle ReyesОценок пока нет
- Febrile SeizuresДокумент5 страницFebrile SeizuresJulmajir Salipmugdar100% (1)
- Ectopic Pregnancy April 2018 1Документ6 страницEctopic Pregnancy April 2018 1Avindya RarasatiОценок пока нет
- FInal Anemia in PregnancyДокумент57 страницFInal Anemia in PregnancyAiszel Angeli Pepito LigoОценок пока нет
- Endometriosis O&g PresentationДокумент31 страницаEndometriosis O&g PresentationChauthiran Agamudaiyar100% (1)
- Diabetes Mellitus CPGДокумент137 страницDiabetes Mellitus CPGKristine-Joy Legaspi FrancoОценок пока нет
- Oral Glucose Tolerance TestДокумент6 страницOral Glucose Tolerance TestIka HabelОценок пока нет
- DM ScreeningДокумент13 страницDM ScreeningRupesh MohandasОценок пока нет
- Clinical Practice Guidelines For Diabetes ManagementДокумент5 страницClinical Practice Guidelines For Diabetes ManagementIqbal Fida MaulanaОценок пока нет
- Diabetes Phils ReportДокумент89 страницDiabetes Phils ReportRold Brio SosОценок пока нет
- Konsensus DM Ada Esda & PerkeniДокумент31 страницаKonsensus DM Ada Esda & PerkeniWindy SuryaОценок пока нет
- 2.CHAPTER 2 Making The DiagnosisДокумент8 страниц2.CHAPTER 2 Making The DiagnosisGautam ManoharОценок пока нет
- Diabetes Mellitus: Zenebe N. (B Pharm, M Pharm) May, 2022Документ93 страницыDiabetes Mellitus: Zenebe N. (B Pharm, M Pharm) May, 2022The AbyssinicansОценок пока нет
- Ofw Clinic May202015Документ14 страницOfw Clinic May202015ejikieru03Оценок пока нет
- Skin Physical ExamДокумент10 страницSkin Physical ExamVenkatesan VidhyaОценок пока нет
- AnatomyДокумент18 страницAnatomyeОценок пока нет
- AДокумент1 страницаAejikieru03Оценок пока нет
- Uy CheatsДокумент10 страницUy Cheatsejikieru03Оценок пока нет
- Our Proforma Invoice Mbli/04/07/M-891: FOR: Our Lady of Mercy General HospitalДокумент3 страницыOur Proforma Invoice Mbli/04/07/M-891: FOR: Our Lady of Mercy General Hospitalejikieru03Оценок пока нет
- Instilling Purpose in Your ChoirДокумент3 страницыInstilling Purpose in Your Choirejikieru03Оценок пока нет
- 47.taxability of Productivity Incentive Bonuses.07.10.08.GACДокумент2 страницы47.taxability of Productivity Incentive Bonuses.07.10.08.GACEumell Alexis PaleОценок пока нет
- MS Definition and AnatomyДокумент9 страницMS Definition and Anatomyejikieru03Оценок пока нет
- MSДокумент8 страницMSejikieru03Оценок пока нет
- PB Guangzhou 2012Документ6 страницPB Guangzhou 2012ejikieru03Оценок пока нет
- Nueva Ecija Doctors Hospital: Our Proforma Invoice Mbli/04/11/M-1445Документ3 страницыNueva Ecija Doctors Hospital: Our Proforma Invoice Mbli/04/11/M-1445ejikieru03Оценок пока нет
- MS MriДокумент22 страницыMS Mriejikieru03Оценок пока нет
- Equipment For Ophthalmology: FOR: Amang Rodriguez Medical Center Attention: Roland L. Cortez, M.DДокумент2 страницыEquipment For Ophthalmology: FOR: Amang Rodriguez Medical Center Attention: Roland L. Cortez, M.Dejikieru03Оценок пока нет
- Proforma Invoice 13Документ3 страницыProforma Invoice 13ejikieru03Оценок пока нет
- Proforma Invoice 14Документ2 страницыProforma Invoice 14ejikieru03Оценок пока нет
- Proforma Invoice 15Документ5 страницProforma Invoice 15ejikieru03Оценок пока нет
- Proforma Invoice 15Документ5 страницProforma Invoice 15ejikieru03Оценок пока нет
- Proforma Invoice 14Документ2 страницыProforma Invoice 14ejikieru03Оценок пока нет
- Proforma Invoice 7Документ3 страницыProforma Invoice 7ejikieru03Оценок пока нет
- Proforma Invoice 11Документ3 страницыProforma Invoice 11ejikieru03Оценок пока нет
- Proforma Invoice 10Документ3 страницыProforma Invoice 10ejikieru03Оценок пока нет
- FOR: Ospital NG Maynila and Medical Center: Our Proforma Invoice Mbli/04/06/M-797Документ4 страницыFOR: Ospital NG Maynila and Medical Center: Our Proforma Invoice Mbli/04/06/M-797ejikieru03Оценок пока нет
- Proforma Invoice 3Документ6 страницProforma Invoice 3ejikieru03Оценок пока нет
- Proforma Invoice 8Документ3 страницыProforma Invoice 8ejikieru03Оценок пока нет
- Proforma Invoice 4Документ3 страницыProforma Invoice 4ejikieru03Оценок пока нет
- FOR: Paulino J. Garcia Mem. Medical Center: Our Proforma Invoice Mbli/04/06/M-804Документ3 страницыFOR: Paulino J. Garcia Mem. Medical Center: Our Proforma Invoice Mbli/04/06/M-804ejikieru03Оценок пока нет
- Proforma Invoice 2Документ2 страницыProforma Invoice 2ejikieru03Оценок пока нет
- Proforma InvoiceДокумент2 страницыProforma Invoiceejikieru03Оценок пока нет
- AS 1 Pretest TOS S.Y. 2018-2019Документ2 страницыAS 1 Pretest TOS S.Y. 2018-2019Whilmark Tican MucaОценок пока нет
- Ang Tibay Vs CAДокумент2 страницыAng Tibay Vs CAEarl LarroderОценок пока нет
- Software Project Management PDFДокумент125 страницSoftware Project Management PDFUmirОценок пока нет
- Fortune 2010Документ14 страницFortune 2010Stefan JenkinsОценок пока нет
- Week 6 Starbucks Leading Change 2023Документ10 страницWeek 6 Starbucks Leading Change 2023Prunella YapОценок пока нет
- CHAPTER 4 (B)Документ6 страницCHAPTER 4 (B)Jon Lester De VeyraОценок пока нет
- RegressionДокумент16 страницRegressionchinusccОценок пока нет
- INTRODUCTIONДокумент1 страницаINTRODUCTIONNabila Gaming09Оценок пока нет
- Mathematicaleconomics PDFДокумент84 страницыMathematicaleconomics PDFSayyid JifriОценок пока нет
- Unsung Ancient African Indigenous Heroines and HerosДокумент27 страницUnsung Ancient African Indigenous Heroines and Herosmsipaa30Оценок пока нет
- TOEIC® Practice OnlineДокумент8 страницTOEIC® Practice OnlineCarlos Luis GonzalezОценок пока нет
- Character Formation 1: Nationalism and PatriotismДокумент11 страницCharacter Formation 1: Nationalism and Patriotismban diaz100% (1)
- Friedman LawsuitДокумент12 страницFriedman LawsuitChris GothnerОценок пока нет
- International Human Rights LawДокумент21 страницаInternational Human Rights LawRea Nica GeronaОценок пока нет
- Commercial CrimesДокумент3 страницыCommercial CrimesHo Wen HuiОценок пока нет
- A Study of The Concept of Future-Proofing in Healtcare Building Asset Menagement and The Role of BIM in Its DeliveryДокумент285 страницA Study of The Concept of Future-Proofing in Healtcare Building Asset Menagement and The Role of BIM in Its DeliveryFausto FaviaОценок пока нет
- COMM 103 Floyd Chapters Study GuideДокумент4 страницыCOMM 103 Floyd Chapters Study GuideMad BasblaОценок пока нет
- 2022BusinessManagement ReportДокумент17 страниц2022BusinessManagement ReportkianaОценок пока нет
- 15 Melodic Uses of Non-Chord TonesДокумент3 страницы15 Melodic Uses of Non-Chord TonesonlymusicaОценок пока нет
- Acidity (As Acetic Acid) On Undenatured and Denatured EthanolДокумент10 страницAcidity (As Acetic Acid) On Undenatured and Denatured EthanolVinh NguyenОценок пока нет
- Amtek Auto Analysis AnuragДокумент4 страницыAmtek Auto Analysis AnuraganuragОценок пока нет