Академический Документы
Профессиональный Документы
Культура Документы
Inborn Errors or Metabolism
Загружено:
saleema11Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Inborn Errors or Metabolism
Загружено:
saleema11Авторское право:
Доступные форматы
INBORN ERRORS
OF METABOLISM
INBORN ERRORS OF METABOLISM
IEM occur 1 in 5000 births collectively
Often treatable if diagnosed
Most difficult task for clinician is to know when to
consider IEM and which tests to order for
evaluation
Clues to presence of IEM may often be found in
FH
DIAGNOSING INBORN ERRORS OF
METABOLISM
Signs and symptoms are often
nonspecific
Routine childhood illnesses excluded 1st
Inborn errors considered only secondarily
Every child with unexplained . . .
Neurological deterioration
Metabolic acidosis
Hypoglycemia
Inappropriate ketosis
Hypotonia
Cardiomyopathy
Hepatocellular dysfunction
Failure to thrive
. . . should be suspected of having a
metabolic disorder
WHEN TO SUSPECT AN IEM
Infants have only a limited repertoire of symptoms-
-sxs non-specific
Vomiting, lethargy, FTT, szs, resp (tachypnea,
hyperpnea, apnea), coma, cardiomyopathy
Odor, abnormal hair, dysmorphology
Labs: metabolic acidosis, hypoglycemia,
hyperammonemia, reducing substances in urine,
ketonuria, pancytopenia
Not all infants with life threatening IEM have either
acidosis or hyperammonemia (i.e. non-ketotic
hyperglycinemia, mild lactate elevations).
Laboratory Assessment of Neonates
Suspected of Having an
Inborn Error of Metabolism
Routine Studies Special Studies
Blood lactate and
pyruvate
Complete blood count
and differential Plasma amino acids
Plasma ammonia Plasma carnitine
Plasma glucose Urine amino acids
Plasma electrolytes and
blood pH Urine organic acids
Urine ketones
Urine-reducing
substances
Clinical Symptomatology of Inborn Errors of Metabolism (IEM) in the
Neonate or Infant
Symptoms indicating possibility of an IEM (one or all)
Infant becomes acutely ill after period of normal behavior and feeding;
this may occur within hours or weeks
Neonate or infant with seizures and/or hypotonia, especially if seizures
are intractable
Neonate or infant with an unusual odor
Symptoms indicating strong possibility of an IEM, particularly when coupled
with the above symptoms
Persistent or recurrent vomiting
Failure to thrive (failure to gain weight or weight loss)
Apnea or respiratory distress (tachypnea)
Jaundice or hepatomegaly
Lethargy
Coma (particularly intermittent)
Unexplained hemorrhage
Family history of neonatal deaths, or of similar illness, especially in
siblings
Parental consanguinity
Sepsis (particularly Escherichia coli)
Physical Anomalies Associated With Acute-Onset Inborn Errors of Metabolism (IEM)
Anomaly Possible IEM
Ambiguous genitalia Congentital adrenal hyperplasia
Hair and/or skin problems (alope- Multiple carboxylase deficiency, biotinidase
cia, dermatitis) deficiency, argininosuccinic aciduria
Structural brain abnormalities Pyruvate dehydrogenase deficiency
(agenesis of corpus callosum,
cortical cysts)
Macrocephaly Glutaric aciduria, type I
Renal cysts, facial dysmorphia Glutaric aciduria, type II; Zellweger syndrome
Facial dysmorphia Peroxisomal disorders, (Zellweger syndrome)
Cataract Galactosemia, Lowe syndrome
Retinopathy Peroxisomal disorders
Lens dislocation, seizures Sulfite oxidase deficiency
Molybdenum cofactor deficiency
Facial dysmorphia, congenital heart 3-OH-isobutyric CoA deacylase deficiency
disease, vertebral anomalies
Clinical Manifestations of Inborn Errors Presenting
Neonatally
Neurologic Signs
Poor suck
Lethargy (progressing to coma)
Abnormalities of tone
Loss of reflexes
Seizures
Gastrointestinal Signs
Poor feeding
Vomiting
Diarrhea
Respiratory Signs
Hyperpnea
Respiratory failure
Organomegaly
Liver
Heart
Inborn Errors of Metabolism of Acute Onset: Nonacidotic,
Nonhyperammonemic Features
Neurologic Features Predominant (Seizures, Hypotonia, Optic
Abnormality)
Glycine encephalopathy (nonketotic hyperglycinemia)
Pyridoxine-responsive seizures
Sulfite oxidase/santhine oxidase deficiency
Peroxisomal disorders (Zellweger syndrome, neonatal adrenoleuko-
dystrophy, infantile refsum disease)
Jaundice Prominent
Galactosemia
Hereditary fructose intolerance
Menkes kinky hair syndrome
1
-antitrypsin deficiency
Hypoglycemia (Nonketotic): Fatty acid oxidation defects (MCAD, LCAD,
carnitine palmityl transferase, infantile form)
Cardiomegaly
Glycogen storage disease (type II phosphorylase kinase b deficiency
18
)
Fatty acid oxidation defects (LCAD)
Hepatomegaly (Fatty): Fatty acid oxidation defects (MCAD, LCAD)
Skeletal Muscle Weakness: Fatty acid oxidation defects (LCAD, SCAD,
multiple acyl-CoA dehydrogenase
defective enzyme
Substrate
(increased)
Product
(decreased)
action
Metabolites
(increased)
Co-factor A
Co-factor B
other
enzymes Metabolites
(decreased)
EFFECT ON OTHER METABOLIC ACTIVITY
e.g., activation, inhibition, competition
Theoretical consequences of an enzyme deficiency.
PROTEIN
GLYCOGEN FAT
AMINO ACIDS
FRUCTOSE
GALACTOSE
FREE FATTY ACIDS
AMMONIA
UREA
UREA CYCLE
ORGANIC ACIDS
GLUCOSE
PYRUVATE
ACETYL CoA
KREBS CYCLE
NADH
KETONES
ATP
LACTATE
An integrated view of the metabolic pathways
FIRST STEPS IN METABOLIC THERAPY
FOR INBORN ERRORS OF METABOLISM
Reduce precursor substrate load
Provide caloric support
Provide fluid support
Remove metabolites via dialysis
Divert metabolites
Supplement with cofactor(s)
THERAPEUTIC MEASURES FOR IEM
D/C oral intake temporarily
Usually IVFs with glucose to give 12-15
mg/kg/min glu and at least 60 kcal/kg to prevent
catabolism
Na benzoate/arginine/citrulline
Dialysis--not exchange transfusion
Vitamins--often given in cocktails after labs
drawn before dx is known
Biotin, B6, B12, riboflavin, thiamine, folate
TREATMENT OF THE ACUTELY SICK
CHILD
General Therapy
Maintain vital functions
Oxygenation
Hydration
Acid/Base balance
Specific Therapy
Treat infection
High dose I.V. glucose
Carnitine supplementation
TREATMENT OF GENETIC DISEASES
MODIFY ENVIRONMENT, e.g., diet, drugs
SURGICAL, correct or repair defect or
organ transplantation
MODIFY OR REPLACE DEFECTIVE GENE
PRODUCT, megadose vitamin therapy or
enzyme replacement
REPLACE DEFECTIVE GENE
CORRECT ALTERED DNA IN DEFECTIVE GENE
NEWBORN SCREENING
PKU - must do on all infants in NICU even if not
advanced to full feeds
Positive--transient HPA, tyr, liver disease,
benign HPA, classical PKU
Galactosemia-
Hypothyroidism
Hemoglobinopathies
Biotinidase def, CAH (21-OHase def),
MSUD
METABOLIC DISORDERS
PRESENTING AS SEVERE NEONATAL
DISEASE
1. Disorders of Carbohydrate Metabolism
Galactosemia - presents with severe liver disease,
gram negative sepsis, and/or cataracts
Enz deficiency: Gal-1-phos uridyl transferase, UDP-
gal-4-epimerase
Glycogen storage disease type 1a & 1b - presents as
hypoglycemia
Enz deficiency: Glucose-6 phosphatase
Lactic Acidosis - presents as lactic acidosis +/-
hypoglycemia
Enz deficiency: Pyruvate carboxylase, Pyr
dehydrogenase, etc.
Fructose intolerance - Needs fructose exposure,
hypoglycemia and acidosis
METABOLIC DISORDERS
PRESENTING AS SEVERE NEONATAL
DISEASE
2. Amino Acid Disorders
Maple syrup urine disease - presents with odor to
urine and CNS problems
Enz deficiency: Branched chain ketoacid
decarboxylase
Nonketotic hyperglycinemia - presents with CNS
problems
Enz deficiency: Glycine cleavage system
Tyrosinemia - Severe liver disease, renal tubular
dysfunction
Enz deficiency: Fumaryl acetate
Transient tyrosinemia of prematurity - progressive
coma following respiratory distress
METABOLIC DISORDERS
PRESENTING AS SEVERE NEONATAL
DISEASE
3. Urea Cycle Defects and Hyperammonemia
4. All present with lethargy, seizures, ketoacidosis,
neutroenia, and hyperammonemia
Ornithine carbamyl transferase (OTC) deficiency
Carbamyl phosphate synthetase deficiency
Citrullinemia
Arginosuccinic Aciduria
Argininemia
Transient tyrosinemia of prematurity
METABOLIC DISORDERS
PRESENTING AS SEVERE NEONATAL
DISEASE
All present with lethargy, seizures, ketoacidosis, neutropenia,
hyperammonemia, and/or hyperglycinemia
4. Organic Acid Defects
Methylmalonic acidemia
Proprionic acidemia
Isovaleric acidemia - odor of sweaty feet
Glutaric aciduria type II
Dicarboxylic aciduria
5. Miscellaneous
Peroxisomal disorders
Lysosomal storage disease
Pyridoxine dependent seizures
Вам также может понравиться
- Inborn Errors of MetabolismДокумент61 страницаInborn Errors of MetabolismVinay PatilОценок пока нет
- Inborn Errors of Metabolism (IEM) : IAP UG Teaching Slides 2015-16Документ25 страницInborn Errors of Metabolism (IEM) : IAP UG Teaching Slides 2015-16nikhilr krishnanОценок пока нет
- Inborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Документ4 страницыInborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Wen Jie LauОценок пока нет
- Lesson 7.1 Inborn Errors of MetabolismДокумент119 страницLesson 7.1 Inborn Errors of Metabolismmisaki06100% (2)
- Inborn Errors or MetabolismДокумент25 страницInborn Errors or MetabolismAnonymous 7dsX2F8nОценок пока нет
- Use of Carnitine in FOD's: Susan C. Winter, MDДокумент67 страницUse of Carnitine in FOD's: Susan C. Winter, MDBradley PostlethwaiteОценок пока нет
- Biomarkers in Inborn Errors of Metabolism: Clinical Aspects and Laboratory DeterminationОт EverandBiomarkers in Inborn Errors of Metabolism: Clinical Aspects and Laboratory DeterminationРейтинг: 5 из 5 звезд5/5 (2)
- Inborn Errors of Metabolism - Early Detection, Key Symptoms and Therapeutic OptionsОт EverandInborn Errors of Metabolism - Early Detection, Key Symptoms and Therapeutic OptionsОценок пока нет
- Infant Jaundice, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandInfant Jaundice, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsРейтинг: 5 из 5 звезд5/5 (1)
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Considering the Patient in Pediatric Drug Development: How Good Intentions Turned Into HarmОт EverandConsidering the Patient in Pediatric Drug Development: How Good Intentions Turned Into HarmОценок пока нет
- A Quick Guide to Metabolic Disease Testing Interpretation: Testing for Inborn Errors of MetabolismОт EverandA Quick Guide to Metabolic Disease Testing Interpretation: Testing for Inborn Errors of MetabolismОценок пока нет
- AntiepilepticsДокумент25 страницAntiepilepticsMurali Krishna Kumar MuthyalaОценок пока нет
- Problem-based Approach to Gastroenterology and HepatologyОт EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisОценок пока нет
- Physiology of DiabetesДокумент52 страницыPhysiology of DiabetesPhysiology by Dr RaghuveerОценок пока нет
- Clinical Biochemistry V3: Contemporary Theories and TechniquesОт EverandClinical Biochemistry V3: Contemporary Theories and TechniquesHerbert SpiegelОценок пока нет
- Pae-Central Nervous SystemДокумент17 страницPae-Central Nervous SystemMegha ProjectsОценок пока нет
- Pediatric ImmunologyДокумент12 страницPediatric ImmunologyCharles BayogОценок пока нет
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionОт EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionОценок пока нет
- Failure To ThriveДокумент53 страницыFailure To Thrivesciatic100% (2)
- Hormon GDSДокумент23 страницыHormon GDSBRI KUОценок пока нет
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Lecture 34 - Hypoglycemia in ChildrenДокумент32 страницыLecture 34 - Hypoglycemia in ChildrenjohnsonkkuriakoseОценок пока нет
- Metabolic OR Endocrine Disorders: Amanda Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistДокумент124 страницыMetabolic OR Endocrine Disorders: Amanda Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistLyn LynОценок пока нет
- Inborn Error of MetabolismДокумент33 страницыInborn Error of MetabolismAlmiraОценок пока нет
- 1.genetic Disorders & Inborn Errors of MetabolismДокумент17 страниц1.genetic Disorders & Inborn Errors of MetabolismAhmed Ali Mohammed AlbashirОценок пока нет
- Neonatal JaundiceДокумент76 страницNeonatal JaundiceSara YousefОценок пока нет
- Concise Paediatric BookДокумент561 страницаConcise Paediatric BookWai Kwong Chiu100% (1)
- Neonatal Jaundice Clinical Presentation - History, Physical Examination PDFДокумент5 страницNeonatal Jaundice Clinical Presentation - History, Physical Examination PDFPaola Méndez NeciosupОценок пока нет
- Sickle Cell Anaemia: The Indian PerspectiveДокумент29 страницSickle Cell Anaemia: The Indian PerspectivePadma KannanОценок пока нет
- Obesity and Esophageal DisordersОт EverandObesity and Esophageal DisordersDhyanesh PatelОценок пока нет
- Sumber CPДокумент9 страницSumber CPArie RezaОценок пока нет
- Principles and Practice of Child Neurology in Infancy, 2nd EditionОт EverandPrinciples and Practice of Child Neurology in Infancy, 2nd EditionОценок пока нет
- Selected Topics in the History of Biochemistry. Personal Recollections. Part IIIОт EverandSelected Topics in the History of Biochemistry. Personal Recollections. Part IIIРейтинг: 1 из 5 звезд1/5 (1)
- Caring for Children with Special Healthcare Needs and Their Families: A Handbook for Healthcare ProfessionalsОт EverandCaring for Children with Special Healthcare Needs and Their Families: A Handbook for Healthcare ProfessionalsLinda L. EddyОценок пока нет
- Pediatric Clinical Pharmacology 2011Документ384 страницыPediatric Clinical Pharmacology 2011Cristina Gilca100% (1)
- Clinical Pearls in Pediatric CardiologyДокумент8 страницClinical Pearls in Pediatric CardiologySunjon JondhleОценок пока нет
- ThalassemiaДокумент9 страницThalassemiaHanady NaeemОценок пока нет
- Approach To Hematuria and Proteinuria in ChildrenДокумент52 страницыApproach To Hematuria and Proteinuria in ChildrenMysheb SS100% (1)
- Cellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsОт EverandCellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsCharles G. CochraneОценок пока нет
- Clinical PediatricДокумент214 страницClinical PediatricRogerОценок пока нет
- Paediatrics PDFДокумент44 страницыPaediatrics PDFNeha OberoiОценок пока нет
- 06.2 Inborn Error of Metabolism - Iii B - Trans PDFДокумент10 страниц06.2 Inborn Error of Metabolism - Iii B - Trans PDFAshim AbhiОценок пока нет
- Pediatric Nutrition Handbook: An Algorithmic ApproachОт EverandPediatric Nutrition Handbook: An Algorithmic ApproachDavid SuskindОценок пока нет
- MRCPCH SyllabusДокумент3 страницыMRCPCH SyllabusKanthi Sagar100% (1)
- Approach To Sick NeonateДокумент47 страницApproach To Sick NeonateblitheleevsОценок пока нет
- Acute Upper Gastrointestinal Bleeding Acute Upper Gastrointestinal Bleeding OverviewДокумент11 страницAcute Upper Gastrointestinal Bleeding Acute Upper Gastrointestinal Bleeding OverviewAnty Dewi Sarty RanyabarОценок пока нет
- Calendar Printable A Little Pinch of Perfect PDFДокумент11 страницCalendar Printable A Little Pinch of Perfect PDFSherah MayeОценок пока нет
- AMC Recalls 2014Документ99 страницAMC Recalls 2014saleema1175% (4)
- 100 Commonly Tested Facts For MRCP Part 1 ExamДокумент3 страницы100 Commonly Tested Facts For MRCP Part 1 Examsaleema11Оценок пока нет
- Neeraj S Notes Step3Документ0 страницNeeraj S Notes Step3Mrudula Rao100% (1)
- 19-11-14 RecallДокумент2 страницы19-11-14 Recallsaleema11Оценок пока нет
- Hypoglycemia 508Документ12 страницHypoglycemia 508saleema11Оценок пока нет
- Dia Care 2015 Inzucchi 140 9Документ10 страницDia Care 2015 Inzucchi 140 9Daniela MuñozОценок пока нет
- WHO DisasterДокумент26 страницWHO Disastersaleema11Оценок пока нет
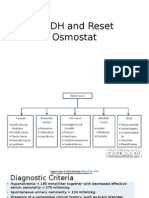
- SIADH and Reset OsmostatДокумент7 страницSIADH and Reset Osmostatsaleema11Оценок пока нет
- HyponatremiaДокумент10 страницHyponatremiasaleema11Оценок пока нет
- 1179 Full PDFДокумент10 страниц1179 Full PDFSonia RogersОценок пока нет
- HyponatremiaДокумент10 страницHyponatremiasaleema11Оценок пока нет
- TakafulДокумент1 страницаTakafulsaleema11Оценок пока нет
- Quiz Behavioral ScienceДокумент91 страницаQuiz Behavioral ScienceMedShare92% (13)
- PsoriasisДокумент5 страницPsoriasissaleema11Оценок пока нет
- Quiz Behavioral ScienceДокумент91 страницаQuiz Behavioral ScienceMedShare92% (13)
- Recommendations For Prescribing Exercise To Overweight and Obese PatientsДокумент5 страницRecommendations For Prescribing Exercise To Overweight and Obese PatientsashkenadaharsaОценок пока нет
- Pelvic Traction SlingДокумент3 страницыPelvic Traction SlingArturo Jr Garces RNОценок пока нет
- Feasibility Study CompiledДокумент22 страницыFeasibility Study CompiledGianne Clarice LopezОценок пока нет
- Guidelines & Protocols: Advisory CommitteeДокумент9 страницGuidelines & Protocols: Advisory CommitteeeddcitoОценок пока нет
- Leana Abusneineh ResumeДокумент2 страницыLeana Abusneineh ResumeLeana AbusneinehОценок пока нет
- Persuasive Outline Exercise Problem SoДокумент4 страницыPersuasive Outline Exercise Problem SomiyaОценок пока нет
- Britannia - The Entry Into OATSДокумент3 страницыBritannia - The Entry Into OATSmpitchОценок пока нет
- Anemia and Nutritional Status of Pre School Children in North Gaza, PalestineДокумент6 страницAnemia and Nutritional Status of Pre School Children in North Gaza, PalestineDera JuliaОценок пока нет
- 5kg5weeks English 1.3Документ36 страниц5kg5weeks English 1.3periukkualiОценок пока нет
- Bands of Wando: Upcoming EventsДокумент8 страницBands of Wando: Upcoming EventsAlexxTastesMetallicОценок пока нет
- Reading Journal 1: Student: Ghassan Mousa Adam Eissa Teacher: Monika Szelag IFP ES Group 1Документ6 страницReading Journal 1: Student: Ghassan Mousa Adam Eissa Teacher: Monika Szelag IFP ES Group 1Ghassan MousaОценок пока нет
- Locally Fermented Foods in Nigeria and Their Significance To National EconomyДокумент12 страницLocally Fermented Foods in Nigeria and Their Significance To National EconomyMonica EmeraldaОценок пока нет
- Problems Faced by KFCДокумент5 страницProblems Faced by KFCManisha Sharma100% (4)
- City Limits Magazine, September/October 2005 IssueДокумент36 страницCity Limits Magazine, September/October 2005 IssueCity Limits (New York)Оценок пока нет
- Elderly PrimiДокумент7 страницElderly PrimiAnnapurna Dangeti67% (3)
- Abdominal OSCE Exam ChecklistДокумент3 страницыAbdominal OSCE Exam ChecklistqmajidОценок пока нет
- Chicken Nutrition - A Guide For Nutritionists and Poultry ProfessionalsДокумент23 страницыChicken Nutrition - A Guide For Nutritionists and Poultry ProfessionalsJamshid63% (8)
- Feeds and FeedingДокумент47 страницFeeds and FeedingDylan Warmfuzzies SalesОценок пока нет
- Fermenting Course Lesson1)Документ29 страницFermenting Course Lesson1)Ninela Cristel100% (1)
- LMSC Vitamin D3 PresentationДокумент19 страницLMSC Vitamin D3 PresentationWidiyantoОценок пока нет
- Final DraftДокумент7 страницFinal DraftMattUrbanОценок пока нет
- Everest AyurvedaДокумент29 страницEverest AyurvedaSamhitha Ayurvedic ChennaiОценок пока нет
- LP Modeling Applications With Computer Analyses in Excel and QM For WindowsДокумент10 страницLP Modeling Applications With Computer Analyses in Excel and QM For WindowsMohammad Saleh AlrantisiОценок пока нет
- Organic Radio ScriptДокумент8 страницOrganic Radio Scriptapi-35127666275% (4)
- Effect of Food Azo Dyes Tartrazine and Carmoisine On Biochemical ParametersДокумент6 страницEffect of Food Azo Dyes Tartrazine and Carmoisine On Biochemical ParametersAbdou CherifiОценок пока нет
- Basic Introduction To Complementary and Alternative Medicine (CAM) SyllabusДокумент7 страницBasic Introduction To Complementary and Alternative Medicine (CAM) Syllabusapi-309695111Оценок пока нет
- Organoleptic Evaluation and Profitability Analysis of "Yoghurt Like Product" Manufactured Using Tiger NutДокумент4 страницыOrganoleptic Evaluation and Profitability Analysis of "Yoghurt Like Product" Manufactured Using Tiger NutEditor IJTSRDОценок пока нет
- 100 đề và 16 17Документ89 страниц100 đề và 16 17Thúy PhạmОценок пока нет
- Alzheimer's Disease (Stages of A.D)Документ5 страницAlzheimer's Disease (Stages of A.D)Elena Karen HermonoОценок пока нет
- Ascorbic Acid: An Enhancing Factor in Iron AbsorptionДокумент11 страницAscorbic Acid: An Enhancing Factor in Iron AbsorptionТатьяна СаенкоОценок пока нет