Академический Документы
Профессиональный Документы
Культура Документы
Diabetic Nephropathy DR Rahul
Загружено:
parahulОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Diabetic Nephropathy DR Rahul
Загружено:
parahulАвторское право:
Доступные форматы
DIABETIC NEPHROPATHY
Dr. P. Rahul
Nephrologist
INTRODUCTION
Microvascular complication
Occurs in upto 40% of diabetes patients
Emerging as a leading cause of ESRD in India
Mortality of ESRD patients with Diabetes Mellitus is higher
than in ESRD patients without Diabetes
However all diabetic patients with ESRD do not have DN as
underlying cause of ESRD.
EPIDEMIOLOGY - DIABETES
Number of diabetics world wide: 171 million.
By 2030 - 334 million.
USA - 8%
Europe - 7%
India - 12-15% (Urban)
Type I ~ 10%
Type II > 90%
EPIDEMIOLOGY
General incidence of Diabetic Nephropathy:
30-40 % of patients with Type I DM
25-40 % of patients with Type II DM
20 - 30 % of Type I DM Progress to ESRD
10 20 % of Type II DM Progress to ESRD
> 30 % of all chronic renal failure patients have Diabetic
Nephropathy
Diabetic Kidney 2007
EPIDEMIOLOGY
In Type 1 DM with Microalbuminuria:
30 80 % develop albuminuria in 10-15 yrs
50-78% develop ESRD in 10-18 yrs
In Type 2 DM :
8-10% have microalbuminuria at diagnosis
20-40% develop albuminuria in 10-15 yrs
20% progress to ESRD in 10-18 yrs
Diabetic Kidney 2007
Genetic Susceptibility
Likelihood of developing DN is markedly increased in patients
with a diabetic sibling or parent who has diabetic nephropathy.
RISK FACTORS FOR DN
Age
Increasing age, along with increasing duration of diabetes,
was associated with increased risk for developing
albuminuria.
RISK FACTORS FOR DN
Blood Pressure
Association between the subsequent development of
nephropathy and higher systemic pressures.
RISK FACTORS FOR DN
Glycemic Control
Diabetic nephropathy is more likely to develop in patients with
worse glycemic control (higher HbA1c levels).
RISK FACTORS FOR DN
Race
Increased incidence in African-Americans, Pima Indians,
Asians
RISK FACTORS FOR DN
Obesity
Associated with an increased risk of chronic kidney disease
among patients with diabetes.
RISK FACTORS FOR DN
Smoking
Associated with increases in albuminuria and the risk of end-
stage renal disease and of decreased survival once dialysis is
begun.
RISK FACTORS FOR DN
NATURAL HISTORY
DN develops after a well defined time period and is usually
associated with retinopathy
DN is characterised by certain well defined stages and presents with
proteinuria , hypertension and renal failure.
All renal disease in a diabetic is not Diabetic Nephropathy
TIME TO ONSET
20 to 30 percent will have microalbuminuria in 15 years
Less than half of these patients will progress to overt
nephropathy.
Onset of overt nephropathy is typically between 10 and 15
years after the onset of the disease.
Those patients who have no proteinuria after 20 to 25 years
have a risk of developing overt renal disease of only about 1
percent per year.
RELATION BETWEEN DIABETIC
NEPHROPATHY AND RETINOPATHY
Patients with nephropathy and type 1 diabetes almost always
have other signs of diabetic microvascular disease, such as
retinopathy and neuropathy
Relationship between diabetic nephropathy and retinopathy is
less predictable in type 2 diabetes
Type 2 diabetics with marked proteinuria and retinopathy most
likely have diabetic nephropathy, while those without
retinopathy have a high frequency of non-diabetic glomerular
disease
30 percent of type 2 diabetics with renal insufficiency have non-
diabetic renal disease
RELATION BETWEEN DIABETIC
NEPHROPATHY AND RETINOPATHY
2007 K/DOQI Guidelines for diabetes and chronic kidney
disease suggest that chronic kidney disease should be
attributed to diabetes in most patients with diabetes if
microalbuminuria and diabetic retinopathy are both present.
By comparison, other causes of CKD should be entertained if
diabetic retinopathy is absent
RELATION BETWEEN DIABETIC
NEPHROPATHY AND RETINOPATHY
Non Diabetic renal disease
suspected when.
No retinopathy
Absence of albuminuria
Rapid increase in serum creatinine.
Presence of active urinary sediment.
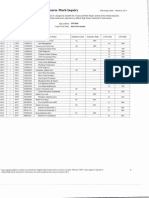
Stage Duration Features
I Hypertrophy < 2 yrs Nephromegaly, No laboratory
abnormalities, RPF
II Histological
abnormalities
> 2 yrs Initial morphological lesions :
GBM thickness,
Mesangium
III Incipient
nephropathy
10-20
yrs
Microalbuminuia, GFR - N
Hypertension (50%)
IV Overt
nephropathy
15-20
yrs
Persistent proteinuria, HTN
(70%), RPF & GFR
V End stage
renal disease
20-40
yrs
GFR < 10%
Hypertension (90%)
MOGENSENS STAGING
Staging well defined in Type 1 DM
In Type 2
15-30% patients can have Microalbuminuria at diagnosis
(Stage 3)
2-8 % can have Overt proteinuria at diagnosis (Stage 4)
SCREENING
When ?
Type 1 DM
Young patients from puberty
Adults - 5 yrs after diagnosis
Type 2 DM
At diagnosis
Yearly thereafter in both
How ?
Spot Urine albumin-creatinine ratio
24 hour urine gold standard
Dipstick/Micral
ALBUMINTO-CREATININE RATIO
Calculation of albumin-to- creatinine ratio in an untimed urine
specimen.
A value above 30mg/g or 0.03mg/mg suggests that albumin
excretion is above 30mg/d and hence microalbuminuria is
probably present.
Almost 100% sensitivity for detection of microalbuminuria.
Preferred screening strategy for all diabetic patients.
MICROALBUMINURIA
Persistent albumin excretion between 30 and 300 mg/day (20
to 200 g/min) is called microalbuminuria
At least 2/3 samples positive for microalbuminuria in 6
months.
No e/o infection, hyperglycemia, no prior exertion.
Significance:
Type I DM:
Predicts overt nephropathy
Type II DM:
Predicts CV mortality
Predicts nephropathy
MICROALBUMINURIA
MICROALBUMINURIA AND GFR
Loss of renal function - defined as an estimated decrease in
GFR of more than 3.3 percent per year occurred in
9% of patients with normoalbuminuria
16% - regression of microalbuminuria.
32% - Stable microalbuminuria
68% - Progressive microalbuminuria
PROGRESSION TO
MACROALBUMINURIA
Albumin excretion above 300 mg/day (200 g/min) is
considered to represent macroalbuminuria
Rate of progression from microalbuminuria to
macroalbuminuria was 2.8 percent per year
Mean rate of loss of GFR in patients with macroalbuminuria
was 0.93 mL/min per month
MANAGEMENT OF DN
Primary
prevention
Secondary
prevention
Tertiary
prevention
ESRD
MA DM
Overt
nephropathy
Ref. Tobe SW et al. CMAJ 2002; 167(5): 499-503
LIFE STYLE MODIFICATION
Ideal body weight
Abstinence from alcohol
Cessation of smoking
Regular exercise
PRIMARY PREVENTION
Glycemic control
Strict glycemic control is recommended in all patients
because of its beneficial effects on microvascular
complications
LANDMARK TRIALS
Type I DM - DCCT
Type II DM - UKPDS
Tight glycemic control leads to significant decrease in retinopathy,
neuropathy and nephropathy and macrovascular complications
Adapted from Diabetes Care ,Jan 2007
Key concepts in setting glycemic goals:
A1C is the primary target for glycemic control
Ideal HbA1C < 7%
More stringent glycemic goals (i.e., a normal A1C, <6%)
may further reduce complications at the cost of increased
risk of hypoglycemia and cardiovascular events.
Glycemic Control
Diet
Exercise
Insulin
Oral hypoglycemic agents
OHAs in CKD
OHA s in CKD
ACE INHIBITORS OR ARBS
Three randomized, placebo-controlled trials of 256 to 3326
patients with diabetes and normoalbuminuria (RASS,
EUCLID, DIRECT) showed no benefit from angiotensin
inhibition
There is no evidence that ACE inhibitors or ARBs are
effective for the primary prevention of microalbuminuria in
patients with diabetes who are normoalbuminuric and
normotensive.
SECONDARY PREVENTION
How to control proteinuria?
Dietary Management
0.6-0.8 g/kg protein day, normal (1-1.2 gm/kg) if on dialysis
High Biological value proteins
Vegetable protein better
Essential amino acids
Ketoanalogues of essential amino acids
Salt intake and proteinuria
high salt intake has been shown to blunt the antiproteinuric
effects of angiotensin inhibitors in patients with non-diabetic
kidney disease.
Salt restriction and/or diuretics enhance the effect of renin-
angiotensin blockade on proteinuria
Salt restriction to 70 meq/day has been found to enhance
the antiproteinuric effects of ARB in patients with type 2
diabetes
ACEI & ARBS
Beyond BP Control
Proteinuria
RAS
Growth factors
Free oxygen radicals
Antifibrotic role
Sodium absorption
ACE inhibitor plus ARB
The superiority of combination therapy with an ACE inhibitor
and an ARB compared to either therapy alone in decreasing
proteinuria has been established in both type 1 and type 2
diabetes
combination therapy with an ACE inhibitor and ARB is
associated with a higher incidence of adverse effects
ARB plus aliskiren
The first effective oral direct renin inhibitor
Aliskiren lowers blood pressure to a degree comparable to
most other agents
In the AVOID trial, aliskiren plus losartan was associated with
a significant 20 percent greater reduction in proteinuria
compared to losartan alone
Aldosterone antagonism
Aldosterone antagonists appear to reduce proteinuria when
used alone, and to have an additive effect on proteinuria
when used in combination with an ACE inhibitor or an ARB in
both type 1 and type 2 diabetes
Spironolactone, Eplerenone
Other antihypertensive drugs
Diltiazem and verapamil appear to be as consistently effective
as an ACE inhibitor or ARB in lowering protein excretion in
diabetic patients
Other agents
Pentoxifylline lowers proteinuria
Weight reduction
Marked decreases in proteinuria may be observed in obese
diabetics who lose weight.
HYPERTENSION AND
PROGRESSION
Transmission to glomerulus initiation of sclerosis
DBP > 90 mm hg progression twice as fast
MAP of 90 almost normalizes rate of decline (2
ml/min/year)
In proteinuric hypertensives effects more marked
HYPERTENSION
1. Diet
2. Exercise
3. Drugsicsers
calcium antagonists
* Lowering BP by any drug beneficial
ACEI
ARBs
Ca channel blockers
Blockers
Diuretics
HYPERLIPIDEMIA AND
PROGRESSION
Dyslipidemia implicated in the pathogenesis of progression
lipids nephrotoxic.
Increase glomerular capillary pressure.
Mesangial changes structural and functional (lipid peroxidation
of LDL foam cells )
Lipoprotein thrombi in the glomerular capillaries
HYPERLIPIDEMIA TREATMENT
Diet
Exercise
Drugs
Statins
Fibrates
ANEMIA AND PROGRESSION
Enhances renal hypoxia
Stimulates release of profibrotic cytokines
Target Hb 12 g/dL
Erythropoietin therapy and correction of anemia may slow CKD progression
RENAL REPLACEMENT THERAPY
Dialysis
Hemodialysis
Peritoneal Dialysis
Transplant
NEWER THERAPIES
Inhibition of TGF-beta (Monoclonal Antibodies to TGF-beta)
appears to ameliorate diabetic nephropathy in experimental
models of diabetes and in preliminary human studies.
Protein Kinase C Inhibitors: Ruboxistaurine
Antifibrotic agents: Tranilast
Endothelin antagonist: Bosentan
NEWER THERAPIES
PPAR-gamma agonists
thiazolidinediones (eg, pioglitazone and rosiglitazone) -
variety of beneficial effects in animal models of diabetic
nephropathy, such as reductions in fibrosis, mesangial cell
proliferation, and inflammation
reduce urinary albumin excretion at various stages of
nephropathy and reduce blood pressure
NEWER THERAPIES
Reduction of Advanced Glycation end products:
ACE I & ARB
Metformin
Aminoguanidine (Pinagedine)
Pyridoxamine
Lipoic acid
Vitamin E
Benfotiamine
Monoclonal Ab to Amadori glycated albumin
SUMMARY
Diabetic renal disease reaching epidemic proportions
All renal disease in a diabetic not diabetic nephropathy
Early detection important Spot urine test/MICRAL
Multi-pronged approach
Diet, Glycemic control, Blood pressure control, ACEI/ARBs
Renal replacement therapies are available but a poor substitute
for prevention
THANK YOU
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Registration ListДокумент5 страницRegistration ListGnanesh Shetty BharathipuraОценок пока нет
- Chapter 5 Constructing An Agile Implementation PlanДокумент4 страницыChapter 5 Constructing An Agile Implementation PlanAHMADОценок пока нет
- Evidence Prove DiscriminationДокумент5 страницEvidence Prove DiscriminationRenzo JimenezОценок пока нет
- SDSSSSDДокумент1 страницаSDSSSSDmirfanjpcgmailcomОценок пока нет
- (20836104 - Artificial Satellites) Investigation of The Accuracy of Google Earth Elevation DataДокумент9 страниц(20836104 - Artificial Satellites) Investigation of The Accuracy of Google Earth Elevation DataSunidhi VermaОценок пока нет
- Culture 2007 2013 Projects Overview 2018-03-18Документ133 страницыCulture 2007 2013 Projects Overview 2018-03-18PontesDeboraОценок пока нет
- 11.3.1 Some Special CasesДокумент10 страниц11.3.1 Some Special CasesSiddharth KishanОценок пока нет
- Ultra ConductorsДокумент28 страницUltra ConductorsAnu Kp50% (8)
- Tangerine - Breakfast Set Menu Wef 16 Dec UpdatedДокумент3 страницыTangerine - Breakfast Set Menu Wef 16 Dec Updateddeveloper louОценок пока нет
- Nikos MIDI Pack - Chord Progression GuideДокумент5 страницNikos MIDI Pack - Chord Progression GuideSamuel ThompsonОценок пока нет
- 4th Sept - Marathon Series Lecture 8 - General AwarenessДокумент208 страниц4th Sept - Marathon Series Lecture 8 - General AwarenessManbir ArinОценок пока нет
- Iguard® LM SeriesДокумент82 страницыIguard® LM SeriesImran ShahidОценок пока нет
- Ej. 1 Fin CorpДокумент3 страницыEj. 1 Fin CorpChantal AvilesОценок пока нет
- Immunity Question Paper For A Level BiologyДокумент2 страницыImmunity Question Paper For A Level BiologyJansi Angel100% (1)
- DJ Crypto ResumeДокумент1 страницаDJ Crypto ResumeNitin MahawarОценок пока нет
- DIR-819 A1 Manual v1.02WW PDFДокумент172 страницыDIR-819 A1 Manual v1.02WW PDFSerginho Jaafa ReggaeОценок пока нет
- Hare and Hyena: Mutugi KamundiДокумент18 страницHare and Hyena: Mutugi KamundiAndresileОценок пока нет
- AIIMS 2015 Solved PaperДокумент436 страницAIIMS 2015 Solved PaperSurya TejaОценок пока нет
- Generation III Sonic Feeder Control System Manual 20576Документ32 страницыGeneration III Sonic Feeder Control System Manual 20576julianmataОценок пока нет
- JCP4 XDOBursting EngineДокумент13 страницJCP4 XDOBursting Enginesubhash221103Оценок пока нет
- Safety Data Sheet SDS For CB-G PG Precision Grout and CB-G MG Multipurpose Grout Documentation ASSET DOC APPROVAL 0536Документ4 страницыSafety Data Sheet SDS For CB-G PG Precision Grout and CB-G MG Multipurpose Grout Documentation ASSET DOC APPROVAL 0536BanyuОценок пока нет
- European Asphalt Standards DatasheetДокумент1 страницаEuropean Asphalt Standards DatasheetmandraktreceОценок пока нет
- Lesson 1 3 Transes in Reading in Philippine HistoryДокумент17 страницLesson 1 3 Transes in Reading in Philippine HistoryNAPHTALI WILLIAMS GOОценок пока нет
- Shri Naina Devi Aarti English 167Документ5 страницShri Naina Devi Aarti English 167ratt182Оценок пока нет
- Active Hospital Network List For Vidal Health Insurance Tpa PVT LTD As On 01 Feb 2023Документ119 страницActive Hospital Network List For Vidal Health Insurance Tpa PVT LTD As On 01 Feb 2023jagdeepchkОценок пока нет
- Sample CVFormat 1Документ2 страницыSample CVFormat 1subham.sharmaОценок пока нет
- Acting White 2011 SohnДокумент18 страницActing White 2011 SohnrceglieОценок пока нет
- SilmaДокумент12 страницSilmanobleconsultantsОценок пока нет
- Simran's ResumeДокумент1 страницаSimran's ResumesimranОценок пока нет
- Img 20150510 0001Документ2 страницыImg 20150510 0001api-284663984Оценок пока нет