Академический Документы
Профессиональный Документы
Культура Документы
Farmakoterapi Terapan Program Pendidikan Profesi Apoteker Medan 2011
Загружено:
Ika Fitri Ramadhana0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров55 страницIdentify ARF earlier and eliminate the cause to avoid the spread of damage Prevention is the key!! in developed ARF, patients should receive therapy to prevent occurrence and reduce its severity avoid nephrotoxins as much as possible. Autoregulation is the maintenance of a near normal intrarenal hemodynamic environment (RBF, RPF, FF and GFR)
Исходное описание:
Оригинальное название
KELOMPOK 4
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документIdentify ARF earlier and eliminate the cause to avoid the spread of damage Prevention is the key!! in developed ARF, patients should receive therapy to prevent occurrence and reduce its severity avoid nephrotoxins as much as possible. Autoregulation is the maintenance of a near normal intrarenal hemodynamic environment (RBF, RPF, FF and GFR)
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров55 страницFarmakoterapi Terapan Program Pendidikan Profesi Apoteker Medan 2011
Загружено:
Ika Fitri RamadhanaIdentify ARF earlier and eliminate the cause to avoid the spread of damage Prevention is the key!! in developed ARF, patients should receive therapy to prevent occurrence and reduce its severity avoid nephrotoxins as much as possible. Autoregulation is the maintenance of a near normal intrarenal hemodynamic environment (RBF, RPF, FF and GFR)
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 55
FARMAKOTERAPI TERAPAN
PROGRAM PENDIDIKAN PROFESI APOTEKER
MEDAN
2011
Dosen Prof. Dr. Urip Harahap, Apt.
21 Oktober 2011
KELOMPOK 4
PSP APOTEKER 2011
Rogabe
Roma Anita
Rosfianita
Santaria
Sri Dewi
Sri Kurniasih
Sri Rahmadani
Sri Dewi Handayani
T. Azma Ulya
Tonny Setiawan
Wahyuni
Widya Akarina
Wilson
Yuliana
Zulkifli
Zulhamidah
Layani Pransiska N
Yustina Samosir
Yensi Zahara
Tamba T. Pasaribu
Identify ARF earlier and eliminate the cause to
avoid the spread of damage
Prevention is the key!!
In developed ARF, patients should receive
therapy to prevent occurrence and reduce its
severity
Avoid nephrotoxins as much as possible
Once the cause of ARF is identified and
eliminated, supportive therapy is the only
remaining option, as we can hasten the
recovery of developed ARF
RENAL BLOOD FLOW
Effective Circulating Volume
Normal
RBF/RPF
Intrarenal Autoregulation
GFR, FF
Renal
Perfusion
Pressure
Cardiac
out put
Mean
Arterial
Pressure
Autoregulation is the maintenance
of a near normal intrarenal
hemodynamic environment (RBF,
RPF, FF and GFR) despite large
changes in the systemic blood
pressure
RBF - blood perfusing the kidneys each minute
(1200 ml/min)
Renal Plasma Flow (RPF) - plasma flowing to
kidneys each minute (670 ml/min or 55-60% of
RBF)
GFR - amount of plasma filtered each minute
by the glomeruli. (Normal GFR -125 ml /min for
men and 100 ml/min for women)
Filtration Fraction (FF) - the ratio of GFR to
RPF (Normal - .18 - .22)
F = P
R
RAP
RBF
R
aff
+ R
eff
~
F = Flow
P = Pressure Changes
R = Resistance
RBF = Renal blood flow
Raff = Afferent arteriolar resistance
RAP = Renal arterial pressure
Reff = Efferent arteriolar resistance
Major sites of renal vascular
resistance -> Glomerular afferent
(R
aff
)
and efferent (R
eff
) arterioles
Changes in R
aff
and R
eff
affect RBF
Vasoconstrictors
Renin
Angiotensin II
Endothelin
ADH
Vasodilators
PGs
Kinins
NO
ANP
RBF
GFR
Figure : RBF / GFR is maintained by a balance between vasodilators and
vasoconstrictors of Afferent and Efferent arterioles
Afferent
Arteriole
PGC
GFR.
Glomerulus
Efferent
Arteriole
Tubule
Figure - shows normal conditions normal renal perfusion
pressure and a normal GFR.
RBF
Reff / Raff ratio
=N
N Engl J Med 357;8 August 23, 2007
RBF
Afferent
Arteriole
PGC
GFR.
Efferent
Arteriole
PGE
Ang II
Figure: shows reduced perfusion pressure within the autoregulatory range.
Normal glomerular capillary pressure is maintained by afferent
vasodilatation and efferent vasoconstriction.
MAP
Reff / Raff ratio =
N Engl J Med 357;8 August 23, 2007
Reff / Raff ratio
Figure: Loss of vasodilatory PGs increases afferent resistance causing drop in the
glomerular capillary pressure below normal values and the fall in GFR
RBF
PGC
GFR.
Ang II
Afferent
Arteriole
Efferent
Arteriole
PGE
NSAID
Reduced perfusion pressure with a NSAID.
N Engl J Med 357;8 August 23, 2007
PGC
GFR.
Ang II
Afferent
Arteriole
Efferent
Arteriole
PGE
ACEIs /ARB
Figure: Loss of angiotensin II action reduces efferent resistance;
this causes the glomerular capillary pressure to drop below normal values
and the GFR to decrease.
Reff / Raff ratio
RBF
N Engl J Med 357;8 August 23, 2007
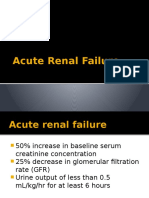
Sudden and sustained decrease in GFR which
is occuring over hours to days, sometimes
over weeks, that associated with an
accumulation of waste products, including
urea and creatinine (Cr).
Acute renal failure is an acute loss of kidney
function that occurs over days to weeks and
results in an inability to appropriately excrete
nitrogenous wastes and creatinine.
ARF is a common condition in the general
population, with an annual incidence of
approximately 200 cases per million
population per year.
The incidence rate is higher in hospitalized
patients (1-5%).
The highest incidence of ARF is in
hospitalized patients in the intensive care
unit (15-20%), reported mortality rates range
from 50-70%.
Am Fam Physician 2005;72:1739-46. Copyright 2005
American Academy of Family Physicians
Infection and cardiorespiratory complications
are the most common causes of death in
patients with acute renal failure.
Am Fam Physician 2005;72:1739-46. Copyright 2005
American Academy of Family Physicians
Based on Severity (RIFLE classification).
RIFLE : Risk, Injury, Failure, Loss, and
End-stage Kidney Disease
STAGE I
RISK
(R)
STAGE II
INJURY
(I)
STAGE V
ESRD
(E)
STAGE III
FAILURE
(F)
STAGE IV
LOSS
(L)
Severity
Outcome
increasing in the serum creatinine level of 0.5 mg
per dL (44.2 mol per L) or a 50 percent increase
in the creatinine level above the baseline value,
a 50 percent decrease in the baseline-calculated
glomerular filtration rate (GFR), or the need for
acute kidney replacement therapy.
Oliguria : a urine output of less than 400 mL in
24 hours.
Anuria : a urine output of less than 100 mL in 24
hours.
Catt : Nilai Normal GFR = 120-125 ml/menit
Am Fam Physician 2005;72:1739-46. Copyright 2005
American Academy of Family Physicians
CAUSES OF ARF
Generalized or localized
reduction in RBF
Hypovolaemia
Haemorrhage
Volume depletion
( vomiting,
diarrhoea,
inappropriate
diuresis, burns)
Hypotension
Cardiogenicshock
Distributive shock
(sepsis,
anaphylaxis)
Oedema
states
Cardiac failure
Hepatic cirrhosis
Nephrotic syndrome
Renal
Hypoperfusion
NSAIDs
ACEI / ARBs
AAA
RAS /occlusion
Hepatorenal
syndrome
Reduced GFR
PRE-RENAL (Hemodynamic)
PRERENAL
RENAL
TUBULAR
Ischemia, Nefrotoxins (Table 2)
tubular cells begin to die ATN (Acute
Tubular Necrosis)
GLOMERULAR
Glomerulonefritis : fever, rash, and
arthritis, urine findings include red
blood cell casts, hematuria, and
proteinuria.
Red blood cell cast
MARKER OF GLOMERULAR INJURY
Granular cast
Am Fam Physician 2005;72:1739-46. Copyright
2005 American Academy of Family Physicians
INTERSTITIAL
Acute Interstitial Nephritis
results from an allergic reaction to a drug
(Table 3)
Sign : fever, rash, serum and urine eosinophil
counts may be elevated.
VASCULAR
microvascular
macrovascular
Am Fam Physician 2005;72:1739-46. Copyright 2005
American Academy of Family Physicians
MARKER OF ACUTE INTERSTITIAL NEPHRITIS
POST RENAL
Obstruction of the outflow tracts of the
kidneys
Prostatic hypertrophy,
Catheters,
Tumors, Strictures, Crystals
Neurogenic bladder obstruction
The following symptoms may occur with acute Renal
failure. Some people have no symptoms, at least in
the early stages. The symptoms may be very subtle.
Hyperkalemia
Nausea/Vomiting
Pulmonary edema
Oliguria or non oliguria
Swelling, especially of the legs and feet
Ascites
Asterixis
Encephalopathy
Decrease urine output
Mental changes
Heart failure
Pruritus
Anemia
Tachypenic
Pale and moist skin
Identify and correct pre-renal, renal and post-
renal factors
Optimise cardiac output and RBF
Review drugs:
Stop ACEIs, NSAIDs
Adjust doses / monitor drug concentrations
Avoid aminoglicoside
Maintaining adequate intravascular volume and
mean arterial pressure
Discontinuing all nephrotoxic drugs
Eliminating exposure to any other nephrotoxins
Accurately monitor fluid balance and daily body
weight
Identify and treat acute complications
Hyperkalaemia
Acidosis
Oedema
Optimise nutritional support
Prinsip Terapi
Pengetahuan dan perjalanan klinik dari tahap-
tahap GGA, dengan cairan:
1. Terapi Konservatif
a. Preventif
b. Suportif
c. Substitusi
2. Terapi ginjal pengganti/dialisa
Dilakukan apabila terapi konservatif gagal
Mencegah faktor risiko yg ada baik akibat
tindakan di dalam Rumah sakit maupun yang
memang sudah ada sebelumnya
Memperingan keadaan GGA dan mengusahakan
agar perfusi renal seoptimal mungkin (oliguri
menjadi non-oliguri).
Volume efektif tubuh diusahakan normal, bila
hipovolemi ditambah, bila hipervolemi harus
dikurangi.
Catt : Volume urine normal = 600-1800 mL
1. Perdarahan, diberi transfusi
2. Plasma expander bila ada luka peritonitis
3. Air dan elektrolit yang sesuai
a. Muntah-muntah : NaCl 0,45% + Kalium 10-20
mmol/l
b. Kehilangan cairan/gangguan pankreatitis : NaCl
0,9 % + HCO3
c. Diare : D5% ditambah HCO3 + Kalium
4. Bila masih terjadi oliguri, diberi diuresis
osmotik berupa:
a. Mannitol 12,5 g iv/5 menit diulang 30 menit
kemudian bila produksi urin <20cc/jam. Bila
produksi urin >20cc/jam teruskan Mannitol 100
grdalam D5% liter/24 jam.
b. Furosemid 40-80 mg iv. Bila dalam 1-2jam
diuresis tidak timbul, dilakukan diuresis paksa
dengan dosis 250-500 mg drip dalam 150cc
D5%/jam.
5. Bila tetap oliguri, berikan vasoaktif untuk
memperbaiki perfusi ginjal yaitu: dopamin
dosis rendah 2-5mg per kg/menit dalam 12
jam.
6. Bila semua tindakan 1-5 gagal, diperlukan
terapi aktif/dialisa agar tidak terjadi oliguri
menetap.
Fase gawat dalam GGA
Biasanya disertai komplikasi : Hiperkalemia,
infeksi/sepsis, koma, kardiovaskuler,
gastrointestinal, respirasi, dan asidosis
metabolik.
Tujuan : untuk menjaga agar pasien tetap dpt
bertahan hidup sehingga ada kesempatan ginjal
pulih.
Terapi suportif adalah dengan mengatasi
gangguan keseimbangan.
1. Cairan
a. Bila ada overhidrasi, berikan furosemid 40-80 mg/iv.
Dapat dilakukan diuresis paksa dosis 250 mg dalam
600cc D5%. Bila gagal lakukan dialisa.
b. Pemberian cairan dibatasi 500 cc
c. Bila penderita panas dpt ditambah 10cc/jam tiap
kenaikan 1derajat C.
Catt : pedoman kebutuhan cairan dipantau dari kadar
Na, bila turun, berarti terjadi overhidrasi, sehingga
asupan cairan lebih dibatasi.
2. Elektrolit Asam Basa
a. Hiperkalemi
Penyebab kematian yang paling sering
pada GGA.
Bila <6 mg/L, hiperkalemi ringan, berikan
resin exchange 25-50 gr/3-4 hari
Bila >6mg/L, hiperkalemi sedang + berat,
dapat dilakukan pilihan pengobatan
hiperkalemia sbb :
2. Hiponatremia
Sering terjadi karena hidrasi berlebihan akibat
pemberian cairan yg sangat banyak
Terapi : pembatasan cairan atau pemberian 2g NaCl
0,9% atau 34 mEq.
3. Hipokalsemia
Akibat kegagalan absorbsi di GI, asidosis, dan
rhabdomiolisis
Terapi : pemberian Ca Gkukonat 10-30 cc/hari
4. Hipermagnesia
Sering berupa gejala paralisis otot, depresi
pernapasan, hipotensi bahkan koma
Terapi : preparat Kalsium, insulin + D5%.
5. Asidosis metabolik
Terjadi pernapasan Kussmaul, kadar bikarbobat
sering 15mg/l
Jumlah bikarbonat = 0,5 x BB x 15 serum HCO3
6. Nutrisi
1. Kalori : diberikan kalori 35-50 kal/kg BB
2. Protein : ditentukan oleh hiperkatabolisme pasien,
sebaiknya 0,5 gr/kgBB/hari
3. Lemak : jumlah kecil (maksimal 1/3 jumlah kalori)
7. Pemakaian obat-obatan
Hindari pemakaian obat-obatan yang nefrotoksik
Jika memang sangat dibutuhkan, atur lama dan
interval dosis
Perlu diperhatikan adanya poliuri (4000-5000
cc/hari) yang mungkin berakibat dehidrasi,
asidosis, bahkan hipokalemi.
Terapi substitusi cairan, garam, bikarbonat,
kalium, dicoba per oral, bila tidak mungkin
dapat secara parenteral 3-5 hari.
Indikasi dilakukan dialisa pada GGA :
1. Secara Klinis
overload cairan, perdarahan hebat, sindrom
ureum, asidosis metabolik, koma yang tidak
teratasi dengan terapi konservatif
2. Secara Laboratoris
HCO3 < 12 mEq , K > 6,0 mEq , Na < 120 mEq
, BUN > 100 mg/dl
ARF is common worldwide
Occurs in all clinical & community settings
It carries a high morbidity and mortality risks,
involves high cost of management.
ARF is increasingly common, particularly among
hospital inpatients, elderly people, and critically ill
patients.
It carries a high mortality
Patients at risk are - elderly people; patients with
diabetes, hypertension, or vascular disease; and
those with pre -existing renal impairment
ARF is often preventable.
Rapid recognition of incipient ARF and early
treatment of established ARF may prevent
irreversible loss of nephrons.
No drug treatment has been shown to limit the
progression of, or speed up recovery from, ARF.
Advice from a nephrologist should be sought for all
cases of ARF.
Вам также может понравиться
- Acute Renal FailureДокумент33 страницыAcute Renal FailureAqsa Akbar AliОценок пока нет
- 6.19.07 Nephrology Board Review ShahДокумент57 страниц6.19.07 Nephrology Board Review Shahactidwell0% (1)
- MKSAP 13-Endocrinology and MetabolismДокумент77 страницMKSAP 13-Endocrinology and Metabolismatul_desai_3100% (2)
- Osce RevisionДокумент38 страницOsce RevisionVivek PatelОценок пока нет
- 404 Veterinary Referral Hospital - BrochureДокумент11 страниц404 Veterinary Referral Hospital - BrochureJoanne FagnouОценок пока нет
- Health Assessment Handout MayannДокумент9 страницHealth Assessment Handout MayannDENNIS N. MUÑOZОценок пока нет
- Acute Renal Failure BДокумент60 страницAcute Renal Failure BEzekiel moraraОценок пока нет
- Acute Renal Failure Lecture 1 Critical Care NursingДокумент52 страницыAcute Renal Failure Lecture 1 Critical Care NursingDina Rasmita100% (2)
- Acute Renal FailureДокумент33 страницыAcute Renal Failureimranqazi11Оценок пока нет
- Acute Renal Failure Lecture 1 Critical Care Nursing NewДокумент41 страницаAcute Renal Failure Lecture 1 Critical Care Nursing NewEdwin Jose SОценок пока нет
- Acute Renal FailureДокумент6 страницAcute Renal Failurearif kurnia timurОценок пока нет
- Acute Liver Failure 2012Документ47 страницAcute Liver Failure 2012nancy voraОценок пока нет
- Perioperative Acute Kidney Injury: DR Mukul Kapoor Director Anesthesia, Max Smart Super Specialty Hospital, Saket, DelhiДокумент46 страницPerioperative Acute Kidney Injury: DR Mukul Kapoor Director Anesthesia, Max Smart Super Specialty Hospital, Saket, DelhiChiragОценок пока нет
- Acute Kidney Injury: DR Hodan Ahmed Dept of Pediatrics and Child Health Amoud Medical School, AUДокумент32 страницыAcute Kidney Injury: DR Hodan Ahmed Dept of Pediatrics and Child Health Amoud Medical School, AUMohamoud MohamedОценок пока нет
- Acute Renal Failure and TreatmentДокумент103 страницыAcute Renal Failure and TreatmentNathan AsinasОценок пока нет
- Acute Renal FailureДокумент47 страницAcute Renal FailureBarryKuppОценок пока нет
- Renal Failure 1 - 095851Документ36 страницRenal Failure 1 - 095851gaynuwanketengОценок пока нет
- Guidelines For The Management of HyponatraemiaДокумент8 страницGuidelines For The Management of HyponatraemiaMuhammad Amiro RasheeqОценок пока нет
- Akd & CKDДокумент44 страницыAkd & CKDﻣﻠﻚ عيسىОценок пока нет
- Anaesthesia For Renal TransplantationДокумент46 страницAnaesthesia For Renal TransplantationShehan WijayasiriwardanaОценок пока нет
- TMJ - Fluid Management in Heart FailureДокумент5 страницTMJ - Fluid Management in Heart FailureSamir SarkarОценок пока нет
- Nephrologi NotesДокумент43 страницыNephrologi NotesSigit Harya HutamaОценок пока нет
- Acute Renal Failure in The Hospital: Diagnosis and ManagementДокумент8 страницAcute Renal Failure in The Hospital: Diagnosis and ManagementJulio César Valdivieso AguirreОценок пока нет
- Chronic Kidney Disease: DR - SarmisthaДокумент19 страницChronic Kidney Disease: DR - SarmisthaGebby MamuayaОценок пока нет
- Hepatorenal Syndrome 1Документ4 страницыHepatorenal Syndrome 1astrealove.5Оценок пока нет
- AkiДокумент38 страницAkiPhillip MartinezОценок пока нет
- Perioperative Oliguria and ATNДокумент22 страницыPerioperative Oliguria and ATNmhelmykhafagaОценок пока нет
- Noel A. Villanueva, MD, FPCP, FPSNДокумент62 страницыNoel A. Villanueva, MD, FPCP, FPSNagilОценок пока нет
- EdemaДокумент45 страницEdemaEdwin GabrielОценок пока нет
- Dr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalДокумент81 страницаDr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalvaishnaviОценок пока нет
- Materi 7 - Gagal Ginjal AkutДокумент30 страницMateri 7 - Gagal Ginjal AkutTegar Muhamad RifkiОценок пока нет
- Congestive Heart FailureДокумент25 страницCongestive Heart Failureemman122392Оценок пока нет
- Management of Anesthesia in Chronic Renal Failure Patients: (Brief Practical Review)Документ23 страницыManagement of Anesthesia in Chronic Renal Failure Patients: (Brief Practical Review)Gebby MamuayaОценок пока нет
- Acute Chronic Renal FailureДокумент41 страницаAcute Chronic Renal FailuresgolbariОценок пока нет
- Prescribing Safely - Analgesia, Antimicrobials and Fluids During Cardiac Failure, Renal Failure and Hepatic Failure States by Oliver Ki Kek YeeДокумент27 страницPrescribing Safely - Analgesia, Antimicrobials and Fluids During Cardiac Failure, Renal Failure and Hepatic Failure States by Oliver Ki Kek YeeoliverkisteamОценок пока нет
- 2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)Документ7 страниц2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)elleinas100% (1)
- Gagal Jantung "Manajemen Iskemik Vs Non Iskemik: DR - Tengku M Budiansyah, SP - JP Siloam Hospitals BogorДокумент76 страницGagal Jantung "Manajemen Iskemik Vs Non Iskemik: DR - Tengku M Budiansyah, SP - JP Siloam Hospitals BogorIndahnvkОценок пока нет
- Dr. Vineet ChaturvediДокумент69 страницDr. Vineet ChaturvediVinay PatilОценок пока нет
- ADHF Wecoc FinalДокумент27 страницADHF Wecoc FinalNovrian Ali YlberОценок пока нет
- Chronic Renal Failure Chapter 261 Pp. 1653-1663Документ6 страницChronic Renal Failure Chapter 261 Pp. 1653-1663Emil GulmaticoОценок пока нет
- Self-Assessment QuestionsДокумент14 страницSelf-Assessment QuestionsFransiska DewiОценок пока нет
- Acute Chronic Renal FailureДокумент43 страницыAcute Chronic Renal FailureHigh Education100% (1)
- Hipertensi Pada Gagal Jantung Kronik: Apa Obat Pilihan Dan Tujuan PengobatanДокумент33 страницыHipertensi Pada Gagal Jantung Kronik: Apa Obat Pilihan Dan Tujuan PengobatanAfraDewitaОценок пока нет
- Acute Kidney InjuryДокумент43 страницыAcute Kidney InjuryIwan ToniroОценок пока нет
- Sample Book: Vasodilator DrugsДокумент4 страницыSample Book: Vasodilator DrugsManangioma ManОценок пока нет
- Acute Liver FailureДокумент78 страницAcute Liver FailurePankaj IngleОценок пока нет
- Admission To The ICU and Monitoring Technique Early Postoperative CareДокумент7 страницAdmission To The ICU and Monitoring Technique Early Postoperative CareWidiartha WahyudiОценок пока нет
- Acute Kidney Injury: Cedera Ginjal Akut (?)Документ36 страницAcute Kidney Injury: Cedera Ginjal Akut (?)Mahfira AmaliaОценок пока нет
- Drugs Uses For Heart FailureДокумент45 страницDrugs Uses For Heart FailureJoshua ObrienОценок пока нет
- Uia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREДокумент4 страницыUia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREfadhiliОценок пока нет
- NCP and DSДокумент6 страницNCP and DSfranzcatchie100% (1)
- Grand Round Case Presentation: by DR Sanjay Khare MD MedicineДокумент19 страницGrand Round Case Presentation: by DR Sanjay Khare MD MedicineHrishikeshОценок пока нет
- Hepato and Cardiorenal SyndromeДокумент31 страницаHepato and Cardiorenal SyndromeanandababuОценок пока нет
- Case Presentation CKDДокумент17 страницCase Presentation CKDPrabal bhuniaОценок пока нет
- Acute Renal Failure in The ICU PulmCritДокумент27 страницAcute Renal Failure in The ICU PulmCritchadchimaОценок пока нет
- Coursematerial 136Документ13 страницCoursematerial 136Nyj QuiñoОценок пока нет
- AcuterenalfailureДокумент3 страницыAcuterenalfailureJessica JacksonОценок пока нет
- The Hepatorenal SyndromeДокумент26 страницThe Hepatorenal SyndromeWaraBawanaОценок пока нет
- Chronic Kidney Disease: A Case Presentation OnДокумент16 страницChronic Kidney Disease: A Case Presentation OnSafoora RafeeqОценок пока нет
- Renal Replacement TherapyДокумент23 страницыRenal Replacement TherapyShelly Dwi SilvitaОценок пока нет
- Acute Renal FailureДокумент17 страницAcute Renal FailureAnitha SuprionoОценок пока нет
- Multiple Organ Dysfunction Syndrome (MODS) : Inayatur Rosyidah., S.Kep - NsДокумент62 страницыMultiple Organ Dysfunction Syndrome (MODS) : Inayatur Rosyidah., S.Kep - Nsmahendra-kurniahОценок пока нет
- Med-Surg LEWIS 47 Final Foofed UpДокумент10 страницMed-Surg LEWIS 47 Final Foofed Uphariniliaankhen100% (1)
- ISPD Peritonitis Guideline Recommendations: 2022 Update On Prevention and TreatmentДокумент44 страницыISPD Peritonitis Guideline Recommendations: 2022 Update On Prevention and TreatmentMisael JimenezОценок пока нет
- Global Guidelines For The Prevention of Surgical Site InfectionДокумент186 страницGlobal Guidelines For The Prevention of Surgical Site InfectionLe Ngoc Quynh GiaoОценок пока нет
- Abces Hati 2 PDFДокумент2 страницыAbces Hati 2 PDFIka Fitri RamadhanaОценок пока нет
- DM PDFДокумент5 страницDM PDFIka Fitri RamadhanaОценок пока нет
- Castor Oil Book PDFДокумент128 страницCastor Oil Book PDFIka Fitri Ramadhana100% (5)
- AntibioticProphylaxis OrtopedyДокумент72 страницыAntibioticProphylaxis OrtopedyIka Fitri RamadhanaОценок пока нет
- Jenis Tumbuhan Sebagai Pewarna AlamДокумент7 страницJenis Tumbuhan Sebagai Pewarna AlamMaulida Part II100% (1)
- Hipnotik PDFДокумент8 страницHipnotik PDFIka Fitri RamadhanaОценок пока нет
- Synthesis, Antispasmodic and Antidiarrheal Activities of Some 1-Substituted Imidazole DerivativesДокумент10 страницSynthesis, Antispasmodic and Antidiarrheal Activities of Some 1-Substituted Imidazole DerivativesIka Fitri RamadhanaОценок пока нет
- Antidiare Again 3 ML orДокумент6 страницAntidiare Again 3 ML orIka Fitri RamadhanaОценок пока нет
- Diarrhea: What I Need To Know AboutДокумент24 страницыDiarrhea: What I Need To Know AboutIka Fitri RamadhanaОценок пока нет
- Summary - Ocular Manifestations of HIVДокумент1 страницаSummary - Ocular Manifestations of HIVRyan HumeОценок пока нет
- (Urinary System, Digestive System and Nervous System) : My Lost HopesДокумент3 страницы(Urinary System, Digestive System and Nervous System) : My Lost HopesCesar Dave PresentacionОценок пока нет
- Surgical Techniques: Plication of The DiaphragmДокумент14 страницSurgical Techniques: Plication of The DiaphragmFranciscoJ.ReynaSepúlvedaОценок пока нет
- Brave New World of Communication: Dr. Cindy RussellДокумент4 страницыBrave New World of Communication: Dr. Cindy Russelltemp001bunnОценок пока нет
- Rough Mcqs For MCQ BankДокумент6 страницRough Mcqs For MCQ BankAvinash KawaleОценок пока нет
- PHE Prevention Diseases Infographic enДокумент5 страницPHE Prevention Diseases Infographic enangel_deeaОценок пока нет
- Autopeep Paul Pepe Jhon MariniДокумент5 страницAutopeep Paul Pepe Jhon MariniRenatoОценок пока нет
- Breast CancerДокумент42 страницыBreast CancerLester Paul SivilaОценок пока нет
- Management of CRAOДокумент3 страницыManagement of CRAOvennieОценок пока нет
- APE QuestionsДокумент6 страницAPE QuestionsJahg WongОценок пока нет
- ThrombophiliasДокумент9 страницThrombophiliasSeraj Abed ElmoatiОценок пока нет
- Demonstration On Chest Physiotherapy DefinitionДокумент3 страницыDemonstration On Chest Physiotherapy Definitiondileep0% (1)
- Guide: DR Srinath Rao Presenter:Dr SR Soumya (Materia Medica MD Part-1) 15/12/14Документ50 страницGuide: DR Srinath Rao Presenter:Dr SR Soumya (Materia Medica MD Part-1) 15/12/14Krishna Veni100% (2)
- FCC Cell Phone CaseДокумент167 страницFCC Cell Phone CaseLaw&Crime50% (2)
- Xerostomia - Understanding The Diagnosis and The Treatment of Dry MouthДокумент5 страницXerostomia - Understanding The Diagnosis and The Treatment of Dry MouthferifhransОценок пока нет
- Choroidal and Retinal Thickening in Severe Preeclampsia: RetinaДокумент7 страницChoroidal and Retinal Thickening in Severe Preeclampsia: RetinaAssifa RidzkiОценок пока нет
- Social Legislation Case DigestsДокумент10 страницSocial Legislation Case DigestsLogia LegisОценок пока нет
- Cancer NotesДокумент9 страницCancer NotesEmily CarlsonОценок пока нет
- Ñ-û-Ç-â-Ç - Û-Ç-+-+ - +-Ç-+-Ä-Û-+-ÎДокумент34 страницыÑ-û-Ç-â-Ç - Û-Ç-+-+ - +-Ç-+-Ä-Û-+-ÎVidhyanand RamachandranОценок пока нет
- Nitrosaminas em Preservativos e BalõesДокумент4 страницыNitrosaminas em Preservativos e BalõeseveltoncОценок пока нет
- Calorie Restriction Highly Anti-CancerДокумент17 страницCalorie Restriction Highly Anti-CancerSpore FluxОценок пока нет
- Pharmacology MCQsДокумент88 страницPharmacology MCQsDr.Tawheed86% (7)
- Melanoma: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Документ154 страницыMelanoma: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Ilham PermanaОценок пока нет
- Chapter 28 Lung CancerДокумент8 страницChapter 28 Lung CancerShanin SalapuddinОценок пока нет
- E Learning Multimodular Treatment in Head and Neck Squamous Cell Carcinoma HNSCCДокумент96 страницE Learning Multimodular Treatment in Head and Neck Squamous Cell Carcinoma HNSCChsfbjbfsОценок пока нет
- Apple BenifitsДокумент8 страницApple Benifitsnara4allОценок пока нет