Академический Документы
Профессиональный Документы
Культура Документы
Aulia Rahmatun Nufus Raihanun Nisa Dinur Sri Rizki
Загружено:
Fauzan Jakfar0 оценок0% нашли этот документ полезным (0 голосов)
133 просмотров18 страницMr. R, a 56-year-old man, presented with a rash and itching on his face, back, palms, and soles for two months. Examination found eruptions with scaling, papules, and plaques. Skin scrapings revealed fungal hyphae. He was diagnosed with tinea facialis (ringworm of the face) based on his symptoms and test results. He was prescribed oral ketoconazole and topical antifungal creams to take for 2-4 weeks, with instructions on medication use, hygiene, and preventing secondary infection.
Исходное описание:
Fungal Infection
Оригинальное название
Tinea Facialis
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документMr. R, a 56-year-old man, presented with a rash and itching on his face, back, palms, and soles for two months. Examination found eruptions with scaling, papules, and plaques. Skin scrapings revealed fungal hyphae. He was diagnosed with tinea facialis (ringworm of the face) based on his symptoms and test results. He was prescribed oral ketoconazole and topical antifungal creams to take for 2-4 weeks, with instructions on medication use, hygiene, and preventing secondary infection.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
133 просмотров18 страницAulia Rahmatun Nufus Raihanun Nisa Dinur Sri Rizki
Загружено:
Fauzan JakfarMr. R, a 56-year-old man, presented with a rash and itching on his face, back, palms, and soles for two months. Examination found eruptions with scaling, papules, and plaques. Skin scrapings revealed fungal hyphae. He was diagnosed with tinea facialis (ringworm of the face) based on his symptoms and test results. He was prescribed oral ketoconazole and topical antifungal creams to take for 2-4 weeks, with instructions on medication use, hygiene, and preventing secondary infection.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 18
Aulia Rahmatun Nufus
Raihanun Nisa Dinur
Sri Rizki
Supervisor :
Nanda Earlia
3%-4% of tinea corporis is tinea facialis
Tinea
corporis
Tinea
facialis
Identity of patient
Name : Mr. R
Sex : Male
Age : 56 years old
Weigth : 62 kg
Job : Selling vegetables
Address : Tungkop, Aceh Besar
Phone number : 085277466610
Registration number : 87-06-35
Examination date : December 31
th
2013
History
The Chief Complain:
Rash followed by itching on the face, upper back, palmars and plantars
since two month ago.
History of present illness:
The patient came to the hospital complaint the appearance of rash followed by
itching on the face, upper back, palmars and plantars since two month ago. At first,
the patient found red spots that felt very itchy on the upper back area, the rash was
getting wider and spreaded to the face, palmars and plantars area. Then, about one
month ago the appearance of rash following itching on the upper back was
disappeared. Itching is felt everytime not induced with environment temperature,
but itching is increasing at the time of using pads and when the groin area is moist.
History of previous illness:
The patient had the same complaint before since two month ago.
Patient were also informed having a history of diabetic since
twelve year ago.
History of Family disease:
None of his family had this kind of disease.
History of Treatment:
Since the patient have complaint he was getting treatment from a
doctor and take medication with diagnosis seborrhoic dermatitis
on Descember, 3
th
2013 and tinea manum on September, 13
th
2013 but not healed.
On facial and palmars dextra and
sinistra region, found erithematous
patch and hypopigmentation with
circumpscripta boundary , irreguler
and polycyclic edges. There are
papules and scales on edge of
lesions, multiple lesions, plaque
size, cental healings, disseminated
arrangement and generalized
distribution
Microscopic Examination of skin scrapins with
10% potassium hydroxide (KOH) showed long
septate and branching hyphae
1. Tinea facialis
2. Seborrheic dermatitis
3. Cutaneus candidiasis
4. Granulloma anulare
5. Morbus Hansen
Diagnosis
Tinea facialis
Systemic Medication:
1. Ketokenazole 200 mg tab once daily for 2 to
3 weeks
Topical Medication :
1. Ketokenazole salp once daily at night for 2
to 4 weeks
2. Myconazole cream once daily in the
morning for 2 to 4 weeks.
1.Taking medicine regularly
2. Do not scratch the rash to prevent the secondary infection
3. Change chlotes when the body is sweating
4. Wearing loose clothing and materials that easily absorb
sweat
5. Dry off after a shower and sweating
Quo ad vitam : dubia ad bonam
Quo ad functionam : dubia ad bonam
Quo ad sanactionam : dubia ad bonam
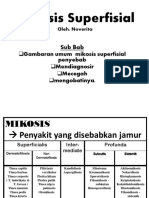
Fungal
infection
Superficial
Subcutaneus
Systemik
Dermatophytosis/
Tinea (Ringworm)
Atacchments
keratin and use as
source of nutriens
to colonize
Stratum corneum
of epidermis,
hair,nails and
horny tissues or
animal
Nonhairy, glabrous
skin
Tinea
Facialis
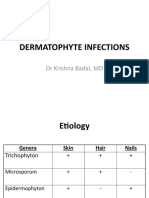
Dermathopytes
Genera
Geophilic
Epidermophyton:
skin,nail
Trichophyton: skin, nail,
hair
Microsporum: skin, hair
Habitat and
pettern of
infection
Anthropophilic
Zoophilic
Skin Disease Location of lesions Clinical Features Fungi Most
Frequently
Responsible
Tinea corporis
(ringworm)
Nonhairy, smooth
skin.
Circular patches with advancing
red, vesiculated border and central
scaling. Pruritic.
T. rubrum,
E.floccosum
Tinea pedis
(athlete`s foot)
Interdigitalis spaces
on feet of persons
wearing shoes.
Acute: itching, red vesicular.
Chroni: itching, scaling, fissures
T. rubrum, T.
mentagrophytes,
E.floccosum
Tinea cruris
(jork itch)
Groin. Eritematous scaling lesion in
intertridiginous area. Pruritic.
T. rubrum, T.
mentagrophytes,
E.floccosum
Tinea capitis Scalp hair.
Endothrix: fungus
inside hair shaft.
Ectothrix: fungus
on surface of hair.
Circular bald patches with short
hair stubs or broken hair within
hair follicles. Kerion rare.
Microsporum-infected hairs
fluoresce.
T.
mentagrophytes,
M.canis
Skin Disease Location of lesions Clinical Features Fungi Most
Frequently
Responsible
Tinea barbae Beard hair. Edematous, erythematous lesion. T.mentagrophyt
es
Tinea
Unguium
(onycho-
mycosis)
Nail. Nails thickened or crumbling
distally;discolored;lusterless.
Usually associated with tinea
pedis.
T. rubrum, T.
mentagrophytes
, E.floccosum
Dermatophytid
(id reaction)
Usually sides and
flexor aspects
fingers. Palm.
Anysite on body.
Pruritic vesicular to bullous
lesions. Most commonly
associated with tinea pedis.
No fungi
present in
lesion. May
become
secondarily
infected with
bacteria.
Allyfamines
Imidazoles
Tolnaffate
Butenafine
Ciclopirox
Topical
treatment
Adults:
Fluconazol 150 mg/week
Itraconazole 100 mg/day
Terbinafin 250 mg/day
Griseovulvin 500 mg/day
Children:
Griseovulvin 10-20 mg/kg/day
Itraconazole 5 mg/kg/day
Terbinafrin 3-6 mg/kg/day
Systemic
treatment
Вам также может понравиться
- Tinea Capitis Favus-Like Appearance: Problem of Diagnosis: Dwi Ratna Adisty, Linda AstariДокумент7 страницTinea Capitis Favus-Like Appearance: Problem of Diagnosis: Dwi Ratna Adisty, Linda AstarihaningpradyОценок пока нет
- Fungal Skin Infections-1Документ27 страницFungal Skin Infections-1Fabb Nelson100% (1)
- Detector Vol 1 No 3 Agustus 2023 Hal 223-234Документ12 страницDetector Vol 1 No 3 Agustus 2023 Hal 223-234Shimie Shimie KokobopОценок пока нет
- DERMATOMYCOSISДокумент114 страницDERMATOMYCOSISQonita Qurrota AyunОценок пока нет
- Dermatomycosis Periode 2 Maret - 5 JuniДокумент128 страницDermatomycosis Periode 2 Maret - 5 JuniDevy KurniawatiОценок пока нет
- Tinea Capitis Kerion Type: A Case Report: Laporan KasusДокумент7 страницTinea Capitis Kerion Type: A Case Report: Laporan Kasuswahyu purnamaОценок пока нет
- Fungal InfectionДокумент114 страницFungal InfectionAini Shofa Haniah100% (2)
- Classification and Epidemiology of Communicable DiseasesДокумент40 страницClassification and Epidemiology of Communicable DiseasesRwapembe StephenОценок пока нет
- (JURNAL) Update Terapy MycosesДокумент51 страница(JURNAL) Update Terapy MycosesHabibah Nurla LumiereОценок пока нет
- DR Pankaj Final Paper UploadДокумент5 страницDR Pankaj Final Paper Uploadaman babuОценок пока нет
- Dermatophyte InfectionsДокумент41 страницаDermatophyte Infectionsshoaib khanОценок пока нет
- MycologyДокумент55 страницMycologyAlpana Laisom100% (2)
- Eczema: Pathogenesis. Atopic Dermatitis Depends On A Complex Interaction BetweenДокумент5 страницEczema: Pathogenesis. Atopic Dermatitis Depends On A Complex Interaction BetweenSuhas IngaleОценок пока нет
- Dermatophytosis, Chromomycosis and Majocchi's Granuloma: A Review.Документ24 страницыDermatophytosis, Chromomycosis and Majocchi's Granuloma: A Review.Deba P SarmaОценок пока нет
- MycosesДокумент2 страницыMycosesMadabout MusicОценок пока нет
- Role of Homoeopathic Medicines in Tinea Corporis: A Case StudyДокумент4 страницыRole of Homoeopathic Medicines in Tinea Corporis: A Case StudySandip VaghelaОценок пока нет
- Fungal Skin Infections ملزمةДокумент6 страницFungal Skin Infections ملزمةعبدالرحمن طارق عبدالله صالحОценок пока нет
- Fungi of Medical ImportanceДокумент11 страницFungi of Medical ImportanceRi FitrianaОценок пока нет
- Superficial MycosisДокумент30 страницSuperficial MycosisLakshayraj SinghОценок пока нет
- A Clinico-Epidemiological Study On Palmoplantar DermatosesДокумент8 страницA Clinico-Epidemiological Study On Palmoplantar DermatosesIJAR JOURNALОценок пока нет
- Fungal InfectionsДокумент42 страницыFungal InfectionsleenaloveuОценок пока нет
- REFERAT Napkin EzcemaДокумент20 страницREFERAT Napkin Ezcemaade nusrayaОценок пока нет
- CHN Fungal InfectionДокумент14 страницCHN Fungal InfectionChrysteline FabrezОценок пока нет
- Superficial Fungal InfectionДокумент24 страницыSuperficial Fungal InfectionzakiОценок пока нет
- Refer atДокумент4 страницыRefer atArieZta Kautsar RahmanОценок пока нет
- Medical MycologyДокумент14 страницMedical Mycologyhawkar omerОценок пока нет
- Tinea Corporis Pedia-1Документ11 страницTinea Corporis Pedia-1Denso Antonius LimОценок пока нет
- Fungal InfectionsДокумент9 страницFungal InfectionsCoral Srinivasa RamaluОценок пока нет
- Scabies and PediculosisДокумент22 страницыScabies and PediculosisEvady IllusionОценок пока нет
- Case ReportДокумент12 страницCase ReportRimueng GhuenОценок пока нет
- Abstrak RokiДокумент16 страницAbstrak Rokirocky salamaОценок пока нет
- Ringworm (Dermatophytosis)Документ20 страницRingworm (Dermatophytosis)Santosh BhandariОценок пока нет
- Tinea - The DermatophytesДокумент67 страницTinea - The Dermatophytesmansoor aliОценок пока нет
- Novia CASE REPORT KulitДокумент6 страницNovia CASE REPORT KulitNovia ShawolОценок пока нет
- Mycology: Clinical FindingsДокумент5 страницMycology: Clinical FindingsLuqman Al-Bashir FauziОценок пока нет
- Mikosis SuperfisialДокумент46 страницMikosis SuperfisialAdipuraAtmadjaEgokОценок пока нет
- Superficial Fungal Disorders of The SkinДокумент121 страницаSuperficial Fungal Disorders of The SkinhaniОценок пока нет
- Classification of Fungal InfectionsДокумент26 страницClassification of Fungal Infectionstev26100% (1)
- Mycology Lecture FinalДокумент258 страницMycology Lecture FinalBahaa Shaaban100% (1)
- Modul #3 - Student Activity Sheet - CUTANEOUS MYCOSESДокумент7 страницModul #3 - Student Activity Sheet - CUTANEOUS MYCOSESYlia MastarsОценок пока нет
- Fungal InfectionДокумент5 страницFungal InfectionFiras HamidehОценок пока нет
- D.K.M.M. Homoeopathic Medical College & Hospital, AurangabadДокумент14 страницD.K.M.M. Homoeopathic Medical College & Hospital, AurangabadShreyance Parakh100% (1)
- ImpetigoДокумент21 страницаImpetigoHanif GandohОценок пока нет
- Ankur Vashishtha S Ubharti University MeerutДокумент34 страницыAnkur Vashishtha S Ubharti University MeerutKana FajarОценок пока нет
- Superficial Fungal Infections of The Skin VoiceoverДокумент67 страницSuperficial Fungal Infections of The Skin VoiceoverMedo JT100% (1)
- Ourd 20122 26Документ2 страницыOurd 20122 26Armin AbasОценок пока нет
- Tinea CorporisДокумент19 страницTinea CorporisDenny AndreaОценок пока нет
- 6-1 Slideshow MOOC MEMYS GUEGANДокумент14 страниц6-1 Slideshow MOOC MEMYS GUEGANamalОценок пока нет
- The Kerion An Angry Tinea Capitis PBДокумент7 страницThe Kerion An Angry Tinea Capitis PBprajnamitaОценок пока нет
- Kata PengantarДокумент21 страницаKata PengantarKartika RosyahОценок пока нет
- RingwormДокумент7 страницRingwormSAMSON, MAXZENE ANICKAОценок пока нет
- Dermatomycosis 18th July 2021Документ120 страницDermatomycosis 18th July 2021Sekar OktaviaОценок пока нет
- E Tra: Diagnosis and Management of Cutaneous Tinea InfectionsДокумент8 страницE Tra: Diagnosis and Management of Cutaneous Tinea InfectionsFuad hadyanОценок пока нет
- Scabies Guideline Sept 07 PDFДокумент10 страницScabies Guideline Sept 07 PDFMira ApriliaОценок пока нет
- Tinea CapitisДокумент7 страницTinea CapitisNadya LiemОценок пока нет
- SCABIES by DR Pavan PatilДокумент5 страницSCABIES by DR Pavan PatilDr. Pavan PatilОценок пока нет
- Dermatofitosis 2011 1Документ35 страницDermatofitosis 2011 1Carmen Cajina Doña MamiОценок пока нет
- Dermatophytosis: LectureДокумент35 страницDermatophytosis: LectureGideon MukalaziОценок пока нет
- K7 Jamur Superficial 2020Документ51 страницаK7 Jamur Superficial 2020Jimmy Fran IIОценок пока нет
- Data Diagnosa P-CareДокумент458 страницData Diagnosa P-CarerinaОценок пока нет
- Covid19 Reading Comprehension ExercisesДокумент2 страницыCovid19 Reading Comprehension ExercisesMariela SeijasОценок пока нет
- DermatomycosesДокумент34 страницыDermatomycosesRomMy WiEn MicKhoОценок пока нет
- Mtap - Virology NotesДокумент7 страницMtap - Virology NotesMoira Pauline LibroraniaОценок пока нет
- TuberculosisДокумент2 страницыTuberculosisapi-300978388Оценок пока нет
- Basic Facts ON HIV: By: Ms. May Jacklyn C. Radoc-Samson, RN, LPT, MancДокумент20 страницBasic Facts ON HIV: By: Ms. May Jacklyn C. Radoc-Samson, RN, LPT, MancMay Jacklyn RadocОценок пока нет
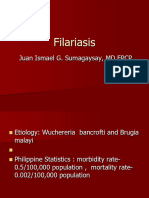
- FilariaДокумент65 страницFilarialunaghilvin2026Оценок пока нет
- TB - SeminarДокумент12 страницTB - SeminarLaith DmourОценок пока нет
- PoliomyelitisДокумент4 страницыPoliomyelitisapi-3710926100% (2)
- Activity No. 11 Apicomplexan Protozoans I-ObjectivesДокумент2 страницыActivity No. 11 Apicomplexan Protozoans I-ObjectivesCindy NonaОценок пока нет
- Feature ArticleДокумент2 страницыFeature ArticleChantelle BlakeleyОценок пока нет
- Rubella On 22-2-2018Документ48 страницRubella On 22-2-2018farigОценок пока нет
- Hiv/Aids and Stis: ChlamydiaДокумент5 страницHiv/Aids and Stis: Chlamydiaapi-283317714Оценок пока нет
- Faktor-Faktor Predisposisi Yang Berhubungan DenganДокумент13 страницFaktor-Faktor Predisposisi Yang Berhubungan DenganBobozОценок пока нет
- WIFA Recording FormsДокумент96 страницWIFA Recording FormsClaude Ryker TalinioОценок пока нет
- TORCH Infection-2073Документ38 страницTORCH Infection-2073NancyОценок пока нет
- The Black PlagueДокумент3 страницыThe Black PlagueKevin MoralesОценок пока нет
- 01 Diseases - Guess What It IsДокумент11 страниц01 Diseases - Guess What It IsRahmania PamungkasОценок пока нет
- ICD 10 English Indonesia Lengkap 2Документ836 страницICD 10 English Indonesia Lengkap 2DINY NOORKHAYATIОценок пока нет
- Malaria Identification It Is Easier Than You Think!: Susan Flaker Johnson, MT (ASCP), MEPDДокумент30 страницMalaria Identification It Is Easier Than You Think!: Susan Flaker Johnson, MT (ASCP), MEPDasclswisconsinОценок пока нет
- Zika Virus FactsheetДокумент2 страницыZika Virus Factsheetfriska_arianiОценок пока нет
- Communicable Disease ChartДокумент4 страницыCommunicable Disease ChartSanjeev Kumar0% (1)
- Mapeh 8Документ4 страницыMapeh 8Hannah Loth ExceliseОценок пока нет
- CasestudyvaccinesДокумент5 страницCasestudyvaccinesapi-323720899Оценок пока нет
- What Is HIV LBL FДокумент1 страницаWhat Is HIV LBL FKevinОценок пока нет
- Centro Escolar University Makati Campus Department of Nursing 2 SEM 2019-2020 BSN 2asДокумент2 страницыCentro Escolar University Makati Campus Department of Nursing 2 SEM 2019-2020 BSN 2asmyeonnieОценок пока нет
- "Hiv and Aids Awareness of Junior and Senior High School Students" Part I: Profile of RespondentsДокумент1 страница"Hiv and Aids Awareness of Junior and Senior High School Students" Part I: Profile of RespondentsDahl xxОценок пока нет
- Final Exam 2013 Sample Epidemiology of Infectious DiseasesДокумент7 страницFinal Exam 2013 Sample Epidemiology of Infectious DiseasesIsha Bhatt100% (1)
- Powerpoint TaeniasisДокумент23 страницыPowerpoint TaeniasisAyshaShariff0% (1)
- HIVAIDS Crossword Puzzle Answer Key PDFДокумент1 страницаHIVAIDS Crossword Puzzle Answer Key PDFjackie pascualОценок пока нет