Академический Документы
Профессиональный Документы
Культура Документы
Nutrition in Anemia: Dr. Marlina Dewiastuti Mkes
Загружено:
Primarini Riati0 оценок0% нашли этот документ полезным (0 голосов)
16 просмотров37 страницgizi
Оригинальное название
Gizi Anemia
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документgizi
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
16 просмотров37 страницNutrition in Anemia: Dr. Marlina Dewiastuti Mkes
Загружено:
Primarini Riatigizi
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 37
NUTRITION IN ANEMIA
dr. Marlina Dewiastuti MKes
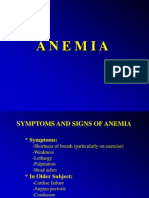
PATHOLOGY, SYMPTOMS, AND SIGNS OF ANEMIA
MORPHOLOGICAL CLASSIFICATION OF ANEMIA
CAUSES OF IRON DEFICIENCY ANEMIA
ANGULAR CHEILITIS AND SMOOTH TONGUE IN IRON
DEFICIENCY
CAUSES OF MEGALOBASTIC ANEMIA
COMPARISON OF FEATURES OF VITAMIN B12 AND FOLIC ACID
DEFICIENCY STATES
Iron
Iron homeostasis is regulated at the level of
intestinal absorption, and it is important that
adequate but not excessive quantities of iron
be absorbed from the diet. Inadequate
absorption can lead to iron-deficiency
disorders such as anemia. On the other hand,
excessive iron is toxic because mammals do
not have a physiologic pathway for its
elimination.
Dietary source
Iron is available from foods of both animal (heme iron) and
plant (non-heme iron) origin. It is better absorbed from
heme iron sources. Absorption of iron is enhanced when
vitamin C foods are eaten with iron rich foods. Iron
cookware also adds to the iron content of cooked foods. The
best sources of iron include liver and other organ meats,
oysters. Good food sources include spinach, beans, and
peas. Fair sources include lean meats, other shellfish, egg
yolks, nuts, dried fruit, other green leafy vegetables, whole
grains, poultry, and fish.
The Recommended Daily Allowance (RDA) of iron for
people who are not iron deficient varies by age group and
other risk factors. (Iron supplements are rarely recommended
in people without evidence of iron deficiency or anemia.)
The RDA recommends these daily amounts of iron:
Children 1 - 3 years old: 10 mg
Teenage boys: 12 mg
Teenage girls and premenopausal women: 15 mg
Pregnant or nursing women: 30 mg
Adult men (up to age 50): 10 mg
Older men and women (over age 50): 10 mg
Ingestion, Absorption, excretion
Ferric iron (Fe+++) in the duodenal lumen
is reduced to its ferrous form through the
action of a brush border ferrireductase. Iron
is the cotransported with a proton into the
enterocyte via the divalent metal transporter
DMT-1. This transporter is not specific for
iron, and also transports many divalent
metal ions.
Once inside the enterocyte, iron follows one
of two major pathways. Which path is taken
depends on a complex programming of the
cell based on both dietary and systemic iron
loads:
Iron abundance states: iron within the
enterocyte is trapped by incorporation into
ferritin and hence, not transported into
blood. When the enterocyte dies and is
shed, this iron is lost.
Iron limiting states: iron is exported out of
the enterocyte via a transporter (ferroportin)
located in the basolateral membrane. It then
binds to the iron-carrier transferrin for
transport throughout the body.
Iron in the form of heme, from ingestion of
hemoglobin or myoglobin, is also readily
absorbed may be transported intact into the
circulation.
Iron Utilization
A model of
hemoglobin at low
resolution. The alpha
chains in this model
are yellow, the beta
chains are blue, and
the heme groups red.
hemoglobins have molecular weights of about 64,500.
Composed of four peptide chains called globins each of
which is bound to a heme. Normal human hemoglobin is
composed of a pair of two identical chains.
Iron is coordinated to four pyrrole nitrogens of
protoporphyrin IX, and to an imidazole nitrogen of a
histidine residue from the globin side of the porphyrin. The
sixth coordination position is available for binding with
oxygen and other small molecules.
STRUCTURE OF HEME
Ferrous iron (Fe
2+
)
Protoporphyrin IX:
contains 4 pyrrole
rings linked together
by methenyl bridges
Heme
8
8
Succinyl CoA
Glycine**
HEME SYNTHESIS
** Amino acid (building blocks of protein) synthesized in your body
Disorders of Heme Synthesis
Acquired: Lead poisoning
Congenital: Porphyrias
Deficiency of heme has far-reaching effects
(hemoglobin, cytochromes, etc.)
LEAD TOXICITY
Symptoms
Irritibility Poor appetite
Lethargy Abdominal pain (with or
Sleeplessness without vomiting)
Headaches Constipation
Pathophysoiology
Binds to any compound with a sulfhydryl group
Inhibits multiple enzyme reactions including those
involved in heme biosynthesis (ALA synthase &
ferrochelatase)
One symptom of lead toxicity is increases in 5-ALA
without concomitant increases in PBG
B12 Vitamin
Vitamin B12 is the largest and most complex of all the vitamins. The
name vitamin B12 is generic for a specific group of cobalt-containing
corrinoids with biological activity in humans. Interestingly it is the
only known metabolite to contain cobalt, which gives this water-
soluble vitamin its red colour. This group of corrinoids is also known
as cobalamins. The main cobalamins in humans and animals are
hydroxocobalamin, adenosylcobalamin and methylcobalamin, the last
two being the active coenzyme forms. Cyanocobalamin is a form of
vitamin B12 that is widely used clinically due to its availability and
stability. It is transformed into active factors in the body.
Functions
Essential growth factor
Formation of blood cells and nerve sheaths
Regeneration of folic acid
Coenzyme-function in the intermediary
metabolism, especially in cells of the
nervous tissue, bone marrow and
gastrointestinal tract
Vitamin B12 is necessary for the formation of blood cells, nerve sheaths and
various proteins. It is therefore, essential for the prevention of certain forms
of anaemia and neurological disturbances. It is also involved in fat and
carbohydrate metabolism and is essential for growth. In humans, vitamin B12
functions primarily as a coenzyme in intermediary metabolism. Two
metabolic reactions are dependent on vitamin B12:
The methionine synthase reaction with methylcobalamin
The methylmalonyl CoA mutase reaction with adenosylcobalamin
In its methylcobalamin form vitamin B12 is the direct cofactor for methionine
synthase, the enzyme that recycles homocysteine back to methionine. There is
evidence that vitamin B12 is required in the synthesis of folate
polyglutamates (active coenzymes required in the formation of nerve tissue)
and in the regeneration of folic acid during red blood cell formation.
Methylmalonyl CoA mutase converts 1-methylmalonyl CoA to succinyl CoA
(an important reaction in lipid and carbohydrate metabolism).
Adenosylcobalamin is also the coenzyme in ribonucleotide reduction (which
provides building blocks for DNA synthesis).
Dietary sources
Vitamin B12 is produced exclusively by microbial synthesis
in the digestive tract of animals. Therefore, animal protein
products are the source of vitamin B12 in the human diet, in
particular organ meats (liver, kidney). Other good sources
are fish, eggs and dairy products. In foods, hydroxo-, methyl-
and 5'-deoxyadenosyl-cobalamins are the main cobalamins
present. Foods of plant origin contain no vitamin B12
beyond that derived from microbial contamination. Bacteria
in the intestine synthesise vitamin B12, but under normal
circumstances not in areas where absorption occurs.
Ingestion & Absorption
Vitamin B12 from food sources is bound to proteins and is only released
by an adequate concentration of hydrochloric acid in the stomach. Free
vitamin B12 is then immediately bound to glycoproteins originating from
the stomach and salivary glands. This glycoprotein complex protects
vitamin B12 from chemical denaturation. Gastrointestinal absorption of
vitamin B12 occurs in the small intestine by an active process requiring the
presence of intrinsic factor, another glycoprotein, which the gastric parietal
cells secrete after being stimulated by food. The absorption of
physiological doses of vitamin B12 is limited to approximately 10g/dose.
The vitamin B12 intrinsic factor complex is then absorbed through
phagocytosis by specific ileal receptors. Once absorbed, the vitamin is
transferred to a plasma-transport protein which delivers the vitamin to
target cells. A lack of intrinsic factor results in malabsorption of
cobalamin. If this is untreated, potentially irreversible neurological damage
and life-threatening anaemia develops (see deficiency).
Regardless of dose, approximately 1% of vitamin B12 is
absorbed by passive diffusion, so this process becomes
quantitatively important at pharmacological levels of
exposure. Once absorbed, vitamin B12 is stored principally
(60%) in the liver. The average B12 content is
approximately 1.0 mg in healthy adults, with 20-30 g
found in the kidneys, heart, spleen and brain. Estimates of
total vitamin B12 body content for adults range from 0.6 to
3.9 mg with mean values of 2-3 mg. The normal range of
vitamin B12 plasma concentrations is 150-750 pg/ml, with
peak levels achieved 8-12 hours after ingestion.
Excretion
Excretion of vitamin B12 is proportional to stores and
occurs mainly by urinary and faecal routes. Vitamin B12 is
very efficiently conserved by the body, with 65-75% re-
absorption in the ileum of the 0.5-5 g excreted into the
alimentary tract per day (mainly into the bile). This helps
to explain the slow development (over several years) of
deficiency states in subjects with negligible vitamin B12
intake, such as vegans. Subjects with a reduced ability to
absorb cobalamin via the intestine (lack of intrinsic factor)
develop a deficiency state more rapidly.
Deficiency
Clinical cobalamin deficiency due to dietary insufficiency is rare in
younger people, but occurs more frequently in older people. Vitamin
B12 deficiency affects 10-15% of individuals over the age of 60.
Deficiency of vitamin B12 leads to defective DNA synthesis in cells,
which affects the growth and repair of all cells. Tissues most affected are
those with the greatest rate of cell turnover, e.g. those of the
haematopoietic system. This can lead to megaloblastic anaemia
(characterised by large and immature red blood cells) and neuropathy,
with numerous symptoms including: glossitis, weakness, loss of appetite,
loss of taste and smell, impotence, irritability, memory impairment, mild
depression, hallucination, breathlessness (dyspnea) on exertion, tingling
and numbness (paraesthesia).
Pernicious anaemia:
Pernicious anaemia is the classical symptom of B12 deficiency, but it
is actually the end-stage of an autoimmune inflammation of the
stomach, resulting in destruction of stomach cells by the bodys own
antibodies. Anaemia is a condition in which red blood cells do not
provide adequate oxygen to body tissues. Pernicious anaemia is a type
of megaloblastic anaemia.
Gastric atrophy:
Gastric atrophy is a chronic inflammation of the stomach resulting in
decreased stomach acid production. Because this is necessary for the
release of vitamin B12 from the proteins in food, vitamin B12
absorption is reduced.
Recommended Dietary Allowance (RDA
RDA intakes for vitamin B12 range from 0.3 to 5.0 g/day in 25
countries. An increase to 2.2 g/day is recommended during pregnancy
and to 2.6 g/day for lactation to cover the additional requirements of
the foetus/infant. The Committee on Nutrition of the American
Academy of Paediatrics recommends a daily vitamin B12 intake of 0.15
g/100 kcal energy intake for infants and preadolescent children. Other
authorities have suggested intakes of 0.3-0.5 g (0-1 year of age), 0.7-
1.5 g (1-10 years of age) and 2 g (> 10 years). The average western
diet probably supplies 3-15 g/day, but can range from 1-100 g/day.
Folic acid
Vitamine B9
Function :
Biochemistry of DNA base and amino acid
production
DNA and cell division
Folate is needed to carry one-carbon groups for
methylation reactions and nucleic acid synthesis
(the most notable one being thymine, but also
purine bases)
Absorpsed in jejenum, actively transport,
excretion 90% urine
Sources
Certain foods are very high in folate:
Leafy vegetables such as spinach, asparagus, turnip greens
Legumes such as dried or fresh beans, peas and lentils
Egg yolks.
[70]
Baker's yeast
Fortified grain products (pasta, cereal, bread); some
breakfast cereals (ready-to-eat and others) are fortified with
25% to 100% of the recommended dietary allowance (RDA)
for folic acid
Sunflower seeds
Liver and liver products contain high amounts of folate
RDA: 400 mcg
Optimal Level: 400 mcg
Maximum: 2 mg
Function
Biochemistry of DNA base and amino
acid production
DNA and cell division
Folate is needed to carry one-carbon groups for
methylation reactions and nucleic acid
synthesis (the most notable one being thymine,
but also purine bases)
Вам также может понравиться
- VitaminДокумент32 страницыVitaminmohammed aliОценок пока нет
- Agents Used Anemias: John Hommer E. Dy, MDДокумент48 страницAgents Used Anemias: John Hommer E. Dy, MDhommercuteОценок пока нет
- VitaminДокумент32 страницыVitaminmohammed aliОценок пока нет
- Haematinics & ErythropoietinДокумент30 страницHaematinics & ErythropoietinManikanta GupthaОценок пока нет
- Drugs Acting On The Blood or Blood-Forming OrgansДокумент4 страницыDrugs Acting On The Blood or Blood-Forming OrgansJenОценок пока нет
- Vitamin 21 JulyДокумент35 страницVitamin 21 JulySafura IjazОценок пока нет
- Lec. B12Документ94 страницыLec. B12Arshad Mehmood MinhasОценок пока нет
- Vitamin B12 and FolateДокумент12 страницVitamin B12 and FolateAllessandria DimaggioОценок пока нет
- 2.FST 511 - Blood Formation Micronutrient and Iron Deficiency AnaemiaДокумент45 страниц2.FST 511 - Blood Formation Micronutrient and Iron Deficiency AnaemianajwaОценок пока нет
- Hematinic AgentsДокумент89 страницHematinic AgentsHussain Rizvi50% (2)
- Drugs For Blood PDFДокумент12 страницDrugs For Blood PDFRaya LuОценок пока нет
- Vitamin B12 and Folic AcidДокумент43 страницыVitamin B12 and Folic AcidErin HillОценок пока нет
- Vitamin B12:: A Water Soluble Hematopoietic VitaminДокумент25 страницVitamin B12:: A Water Soluble Hematopoietic Vitamindr. SheryarOrakzaiОценок пока нет
- Agents Used in Anemias 2Документ25 страницAgents Used in Anemias 2Raboha TawilОценок пока нет
- 6.megaloblastic AnaemiasДокумент34 страницы6.megaloblastic AnaemiasWissam AlwazaniОценок пока нет
- GM SirДокумент23 страницыGM SirAyesha AhmedОценок пока нет
- Hematinics: Madan Sigdel Lecturer Department of Pharmacology Gandaki Medical CollegeДокумент44 страницыHematinics: Madan Sigdel Lecturer Department of Pharmacology Gandaki Medical Collegemadan sigdelОценок пока нет
- Kuliah Macrocytic Anemia 2017Документ40 страницKuliah Macrocytic Anemia 2017igus696Оценок пока нет
- Md. Riazuddin (MS - 210931) DocsДокумент10 страницMd. Riazuddin (MS - 210931) DocsMohona Rahman KhanОценок пока нет
- Vitamin B12Документ10 страницVitamin B12api-388948078Оценок пока нет
- Megaloblastic AnemiaДокумент36 страницMegaloblastic AnemiaMandyam Monica SaiОценок пока нет
- NewДокумент93 страницыNewNarayan TiwariОценок пока нет
- Nutrients: Vitamin B in Health and DiseaseДокумент18 страницNutrients: Vitamin B in Health and DiseaseSrinivas RajanalaОценок пока нет
- HaematinicsДокумент20 страницHaematinicsGeetika Mehta100% (1)
- Vitamin B12 in Vegetarian DietsДокумент4 страницыVitamin B12 in Vegetarian DietsJesica DiazОценок пока нет
- Clinical Nutrition: Jardine Jade Albert C. Valdez, RMT, MSMT (C)Документ53 страницыClinical Nutrition: Jardine Jade Albert C. Valdez, RMT, MSMT (C)Yna EstandarteОценок пока нет
- Vitamins: Basem Battah, Pharm, MSC, PHDДокумент47 страницVitamins: Basem Battah, Pharm, MSC, PHDNaya AbdullahОценок пока нет
- Vitamin B12 ReviewДокумент12 страницVitamin B12 ReviewMunyaradzi Nhambure100% (1)
- 3 - Metabolisme Vitamin B12 B9 CДокумент49 страниц3 - Metabolisme Vitamin B12 B9 CPaulinОценок пока нет
- Drugs With Action On BloodДокумент11 страницDrugs With Action On BloodVaishali PrasharОценок пока нет
- Obat AntianemiaДокумент49 страницObat AntianemiadilaОценок пока нет
- HematinicsДокумент27 страницHematinicsDeepankar SutradharОценок пока нет
- Pernicious Anemia - ECEДокумент46 страницPernicious Anemia - ECEaparna reddyОценок пока нет
- Presentation of Vitamin B12Документ10 страницPresentation of Vitamin B12Dipak YogiОценок пока нет
- Vitamin B12Документ18 страницVitamin B12Kimberly A. S. SmithОценок пока нет
- Vitamin B12 Deficiency, A Simple Guide To The Condition, Treatment And Related DiseasesОт EverandVitamin B12 Deficiency, A Simple Guide To The Condition, Treatment And Related DiseasesРейтинг: 5 из 5 звезд5/5 (2)
- Nutritional AnemiaДокумент78 страницNutritional AnemiaJoUng DjelauОценок пока нет
- Lec 15Документ23 страницыLec 15jayОценок пока нет
- Haematopoietic Agents & Erythropoeitin: Dr. Rishi Pal Assistant Professor Department of PharmacologyДокумент43 страницыHaematopoietic Agents & Erythropoeitin: Dr. Rishi Pal Assistant Professor Department of PharmacologyDERRICK AAGYEREYIR SAANUMEОценок пока нет
- Anti Anemia DrugsДокумент36 страницAnti Anemia DrugsArabelle GOОценок пока нет
- Blood PharmacologyДокумент71 страницаBlood PharmacologyNo NameОценок пока нет
- R.G. VermaДокумент16 страницR.G. VermaMohit ShrivastavaОценок пока нет
- Vitamins BUC PDFДокумент40 страницVitamins BUC PDFThe Egy NerdОценок пока нет
- Vitamin B12Документ24 страницыVitamin B12pranshutiwari820Оценок пока нет
- Overview of VitaminsДокумент30 страницOverview of Vitaminsdavis ombuiОценок пока нет
- Drugs Used in The Treatment of Anemia: Prepared By: Dr. Ghazi BamagousДокумент42 страницыDrugs Used in The Treatment of Anemia: Prepared By: Dr. Ghazi BamagousAyman B-DadyОценок пока нет
- Cobalt MetabolismДокумент14 страницCobalt MetabolismShofwatunnisaОценок пока нет
- Anemia inДокумент15 страницAnemia inronaldocenaОценок пока нет
- Megaloblastic AnemiasДокумент37 страницMegaloblastic AnemiasL3mi DОценок пока нет
- Nutritional AnemiaДокумент90 страницNutritional AnemiaIrham KhairiОценок пока нет
- Pathophysiology of Blood and Circulatory Sys: Physiology DepartmentДокумент73 страницыPathophysiology of Blood and Circulatory Sys: Physiology DepartmentISRAELОценок пока нет
- Nutrients: Vitamin B in Health and DiseaseДокумент18 страницNutrients: Vitamin B in Health and DiseaseMuhammad FaqihОценок пока нет
- Vitamin B12 (Cobalamin) Deficiency in Elderly PatientsДокумент9 страницVitamin B12 (Cobalamin) Deficiency in Elderly PatientsGrady ChristianОценок пока нет
- Nutritional Anemia: Dr. Mardiana, M.Kes, SP - GK Department of Clinical Nutrition Hasanuddin University MakassarДокумент77 страницNutritional Anemia: Dr. Mardiana, M.Kes, SP - GK Department of Clinical Nutrition Hasanuddin University MakassarDianaОценок пока нет
- Vitamin and HormoneДокумент26 страницVitamin and HormoneMohammad JewelОценок пока нет
- Elgar, 2022Документ17 страницElgar, 2022Caoimhe O'BrienОценок пока нет
- 8 - Basics in Deficiency AnaemiasДокумент59 страниц8 - Basics in Deficiency AnaemiasWasana MendisОценок пока нет
- VitaminsДокумент48 страницVitaminsBhumika ghimireОценок пока нет
- Megaloblastic Anemias: Dept of Medicine AcmsДокумент71 страницаMegaloblastic Anemias: Dept of Medicine Acmskunal ghosh100% (1)
- Iron Deficiency Anaemia (IDA) Diagnosis: Dr. Saifeldein M. A. ElimamДокумент33 страницыIron Deficiency Anaemia (IDA) Diagnosis: Dr. Saifeldein M. A. ElimamSaifeldein ElimamОценок пока нет
- Anemia (Syptoms and Signs)Документ17 страницAnemia (Syptoms and Signs)Primarini RiatiОценок пока нет
- Autoimmune DiseaseДокумент38 страницAutoimmune DiseaseGustiandari FidhyaОценок пока нет
- Neoplasm AДокумент14 страницNeoplasm ASiti Nurwulan FebryanОценок пока нет
- Anemia (Syptoms and Signs)Документ17 страницAnemia (Syptoms and Signs)Primarini RiatiОценок пока нет
- Anemia (Syptoms and Signs)Документ17 страницAnemia (Syptoms and Signs)Primarini RiatiОценок пока нет
- Dengan Metoda Pendekatan Johnson SieglerДокумент2 страницыDengan Metoda Pendekatan Johnson SieglerPrimarini RiatiОценок пока нет
- Aplikasi Dengan Spss Anova 2 FaktorДокумент13 страницAplikasi Dengan Spss Anova 2 FaktorPrimarini RiatiОценок пока нет
- Anemia (Syptoms and Signs)Документ17 страницAnemia (Syptoms and Signs)Primarini RiatiОценок пока нет
- Evidence-Based Medicine: Tools, Techniques, ResultsДокумент42 страницыEvidence-Based Medicine: Tools, Techniques, ResultsPrimarini RiatiОценок пока нет
- Tda12110h1 N300Документ1 страницаTda12110h1 N300rolandseОценок пока нет
- Continuous Microbiological Environmental Monitoring For Process Understanding and Reduced Interventions in Aseptic ManufacturingДокумент44 страницыContinuous Microbiological Environmental Monitoring For Process Understanding and Reduced Interventions in Aseptic ManufacturingTorres Xia100% (1)
- Keith UrbanДокумент2 страницыKeith UrbanAsh EnterinaОценок пока нет
- Electronic Fetal MonitoringДокумент4 страницыElectronic Fetal MonitoringMauZungОценок пока нет
- 9 - 1 H Wood Cabinet Spec Options NelДокумент8 страниц9 - 1 H Wood Cabinet Spec Options NelinformalitybyusОценок пока нет
- Ideal Discharge Elderly PatientДокумент3 страницыIdeal Discharge Elderly PatientFelicia Risca RyandiniОценок пока нет
- Case Study of Flixborough UK DisasterДокумент52 страницыCase Study of Flixborough UK Disasteraman shaikhОценок пока нет
- Expressions of QuantityДокумент5 страницExpressions of Quantitybenilde bastidaОценок пока нет
- Bleeding in A NeonateДокумент36 страницBleeding in A NeonateDrBibek AgarwalОценок пока нет
- C50SCR PLC Complete ManualДокумент286 страницC50SCR PLC Complete ManualthuanОценок пока нет
- Section-A: Terrace Ramp To Basement BalconiesДокумент4 страницыSection-A: Terrace Ramp To Basement BalconiesRitikaОценок пока нет
- Lpalmer ResumeДокумент4 страницыLpalmer Resumeapi-216019096Оценок пока нет
- Mental Health & TravelДокумент18 страницMental Health & TravelReyza HasnyОценок пока нет
- Design and Fabrication of Floor Cleaning Machine - A ReviewДокумент4 страницыDesign and Fabrication of Floor Cleaning Machine - A ReviewIJIERT-International Journal of Innovations in Engineering Research and Technology100% (1)
- Texas Steering and Insurance DirectionДокумент2 страницыTexas Steering and Insurance DirectionDonnie WeltyОценок пока нет
- Synopsis of Involex TurbineДокумент3 страницыSynopsis of Involex TurbineTanviОценок пока нет
- Work Environment Act (1977:1160) : Chapter 1 Purpose and Scope of The ActДокумент26 страницWork Environment Act (1977:1160) : Chapter 1 Purpose and Scope of The ActNatalie BlackmoreОценок пока нет
- Consolidation of ClayДокумент17 страницConsolidation of ClayMD Anan MorshedОценок пока нет
- Big Elephants Are Useful Mnemonics & IdiomsДокумент144 страницыBig Elephants Are Useful Mnemonics & IdiomsNachoAndrésLlorente100% (1)
- Bio1 11 - 12 Q1 0501 FDДокумент23 страницыBio1 11 - 12 Q1 0501 FDIsabelle SchollardОценок пока нет
- Piaget Stages of Cognitive DevelopmentДокумент2 страницыPiaget Stages of Cognitive DevelopmentSeph TorresОценок пока нет
- Open Courses Myanmar Strategic English Week 4: U Yan Naing Se NyuntДокумент24 страницыOpen Courses Myanmar Strategic English Week 4: U Yan Naing Se NyuntYan Naing Soe NyuntОценок пока нет
- 2009 HSC Exam Chemistry PDFДокумент38 страниц2009 HSC Exam Chemistry PDFlillianaОценок пока нет
- Amino AcidsДокумент17 страницAmino AcidsSiddharth Rohilla100% (2)
- Ott OTT Ecolog 1000 Water Level LoggerДокумент3 страницыOtt OTT Ecolog 1000 Water Level LoggerNedimZ1Оценок пока нет
- Prestress 3.0Документ10 страницPrestress 3.0Jonel CorbiОценок пока нет
- Director's Update Our StudentsДокумент23 страницыDirector's Update Our StudentsAdrian MojicaОценок пока нет
- Deductions From Gross IncomeДокумент2 страницыDeductions From Gross Incomericamae saladagaОценок пока нет
- Chemsheets AS 006 (Electron Arrangement)Документ27 страницChemsheets AS 006 (Electron Arrangement)moiz427Оценок пока нет
- Canfield FairДокумент3 страницыCanfield Fairapi-546463844Оценок пока нет