Академический Документы
Профессиональный Документы
Культура Документы
(Fix) Topic List Placenta Previa
Загружено:
Sam Hendratno0 оценок0% нашли этот документ полезным (0 голосов)
19 просмотров14 страницd
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документd
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
19 просмотров14 страниц(Fix) Topic List Placenta Previa
Загружено:
Sam Hendratnod
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 14
PLACENTA PREVIA
Supervised by: dr. Pim Gonta, Sp.OG
Created by:
Kevin Kristian (2012-061-144)
Melissa Judi Koesyanto (2012-061-145)
Revy Aditya (2012-061-148)
Dominicus Dimitri (2013-061-132)
Roswita Yohana Manek (2013-061-139)
Maria Novilina Basso (2013-061-141)
Definition
Placenta previa is a condition in pregnancy which
placenta is implanted over or very near the
internall cervical ostium.
Classification
Total placenta previa: The placenta covers the
internal cervical ostium completely.
Partial placenta previa: The placenta covers
the internal cervical ostium partially.
Marginal placenta previa: The edge of the
placenta is located at the marginal of the
internal cervical ostium.
Low lying placenta: The placenta is implanted
in the lower uterine segment, but the edge of
it doesnt reach the internal cervical ostium.
Risk Factor
Advancing maternal age
Multiparity
Multiple gestation (gemelli)
Prior cesarean section delivery
Maternal smoker
Unexplained elevated screening levels of
alpha-fetoprotein
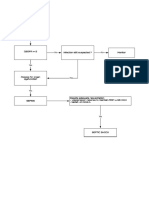
Pathophysiology
The bleeding in placenta previa is caused by
the laceration of the placenta which resulted
from the disengagement of the basal
descidua to the uterine lining that caused by
dilatation and effacement of the cervix.
The blood comes from the intervillus spaces
of the placenta and it is ease by the
uncontractable lower segment of the uterus.
Pathophysiology
The bleeding eventually will stop, but if the
laceration is located in the bigger sinus, the
bleeding be longer.
Since the formation of lower uterine segment is
progressive, the laceration will re-occur, so do
the bleeding.
The blood will flow freely from the cervical
ostium since there are no tampon on the cervical
ostium and retroplacental hematoma is not
formatted.
This also the reason why coagulopathy is rarely
happens on patients with placenta previa
Pathophysiology
The lower uterine segment is thin and
relatively weak and this cause the
trophoblastic villus invade stronger to the
uterine wall, thats why placenta accreta and
increta could happen.
Clinical Finding
Spontaneous and painless bleeding, usually
appear on the end of second trimester or
later.
Recurrent bleeding.
Diagnosis
Clinical findings.
Bleeding after vaginal touchier.
Ultrasonography
Transabdominal
Trans perineal
MRI: for the detection of placenta accreta,
increta or percetta.
Complication
Bleeding complication: shock.
Placenta accreta, incretta and percetta
Placental retention.
Uterus Rupture.
Premature birth.
Placental abruption.
Management
Preterm fetus
Hospitalization and close observation.
Blood group testing and sensitization in Rh(-)
patients.
Discharge after the fetus is judged to be healthy
and the bleeding stops.
In massive bleeding, MgSO
4
is given to stop
uterine contraction and steroid is given to
maturate fetals lung, blood transfusion also
considered.
Avoiding sexual intercourse.
Management and Prognosis
Management
Delivery
Caesarian section with general anaesthesia.
Prognosis
47% premature birth.
2.5-fold fetal anomalies in placenta previa.
Вам также может понравиться
- Blank Diagram PDFДокумент1 страницаBlank Diagram PDFSam HendratnoОценок пока нет
- 30C SectioncostsДокумент32 страницы30C SectioncostsZaqila AtkОценок пока нет
- Sepsis: Update On Surviving Sepsis Campaign 2018 RSUD Kefamenanu 2019Документ5 страницSepsis: Update On Surviving Sepsis Campaign 2018 RSUD Kefamenanu 2019Sam HendratnoОценок пока нет
- Morpot 18817Документ3 страницыMorpot 18817Sam HendratnoОценок пока нет
- AvoidДокумент1 страницаAvoidSam HendratnoОценок пока нет
- Tubal Evaluation Is Essential in Subfertile PatientsДокумент2 страницыTubal Evaluation Is Essential in Subfertile PatientsSam HendratnoОценок пока нет
- Morning Report Rabu Pagi 30-8-2017: Dr. Samuel & Dr. ScovaniДокумент3 страницыMorning Report Rabu Pagi 30-8-2017: Dr. Samuel & Dr. ScovaniSam HendratnoОценок пока нет
- Morpot 14-9Документ7 страницMorpot 14-9Sam HendratnoОценок пока нет
- Historical Characterization of Trigeminal.20aДокумент5 страницHistorical Characterization of Trigeminal.20aSam HendratnoОценок пока нет
- AvoidДокумент1 страницаAvoidSam HendratnoОценок пока нет
- Respiratory Distress Syndrome (RDS) : American Lung AssociationДокумент3 страницыRespiratory Distress Syndrome (RDS) : American Lung AssociationMirza RisqaОценок пока нет
- Surgery Topic List: Nama Mahasiswa: NIM: PeriodeДокумент2 страницыSurgery Topic List: Nama Mahasiswa: NIM: PeriodeSam HendratnoОценок пока нет
- Hernia Examination SchemeДокумент4 страницыHernia Examination Schemeatribecalledquest20Оценок пока нет
- Benchmark ResultsДокумент1 страницаBenchmark ResultsSam HendratnoОценок пока нет
- Op ENko REДокумент13 страницOp ENko REhanz1234zОценок пока нет
- Hernia Examination SchemeДокумент4 страницыHernia Examination Schemeatribecalledquest20Оценок пока нет
- Maurice Nicoll The Mark PDFДокумент4 страницыMaurice Nicoll The Mark PDFErwin KroonОценок пока нет
- Surgery Topic List: Nama Mahasiswa: NIM: PeriodeДокумент2 страницыSurgery Topic List: Nama Mahasiswa: NIM: PeriodeSam HendratnoОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- NRP (Neonatal Resuscitation Program) 6th Edition 2 of 5Документ88 страницNRP (Neonatal Resuscitation Program) 6th Edition 2 of 5iamlucil100% (4)
- "Combining Medical Excellence With Luxury Travel": Marketing Strategies of Medical TourismДокумент18 страниц"Combining Medical Excellence With Luxury Travel": Marketing Strategies of Medical TourismRajesh SainiОценок пока нет
- Reproductive Female System: by Dr.H.Gusbakti, MSC, PKK, Aifm Professor of PhysiologyДокумент44 страницыReproductive Female System: by Dr.H.Gusbakti, MSC, PKK, Aifm Professor of PhysiologyRizki YulianaОценок пока нет
- English For NursesДокумент63 страницыEnglish For NursesDyah Elvi Meiedietik88% (17)
- Going Under Chapter SamplerДокумент28 страницGoing Under Chapter SamplerAllen & UnwinОценок пока нет
- OB Midterm ReviewerДокумент15 страницOB Midterm ReviewerCarlos Miguel AndalОценок пока нет
- The Influence of Finger Hold Relaxation Technique On Pain Reduction of Post Sectio Caesare A PatientsДокумент10 страницThe Influence of Finger Hold Relaxation Technique On Pain Reduction of Post Sectio Caesare A PatientsIntan Dwi AriniОценок пока нет
- Resume - CrnaДокумент3 страницыResume - Crnaapi-267840443Оценок пока нет
- Partogram CORRECTEDДокумент45 страницPartogram CORRECTEDjayasankariОценок пока нет
- Unit VI-progressive Patient CareДокумент34 страницыUnit VI-progressive Patient CareAnand gowda100% (1)
- Slides 3 - Internal AnatomyДокумент45 страницSlides 3 - Internal AnatomyCWT2010100% (1)
- Guidelines For Obstetric Epidural Blood Patch NPS 5.4.06Документ2 страницыGuidelines For Obstetric Epidural Blood Patch NPS 5.4.06grigmihОценок пока нет
- Hangat Campuran Kencur Terhadap Edema Kaki Ibu Hamil Trimester Iii Di Wilayah Kerja Puskesmas I Wangon, BanyumasДокумент13 страницHangat Campuran Kencur Terhadap Edema Kaki Ibu Hamil Trimester Iii Di Wilayah Kerja Puskesmas I Wangon, BanyumasTri YaniОценок пока нет
- Mcvary 2011 Update On AUA Guideline BPHДокумент11 страницMcvary 2011 Update On AUA Guideline BPHFoxglove83Оценок пока нет
- Total Experience 12 Years: Academic QualificationsДокумент3 страницыTotal Experience 12 Years: Academic QualificationsNHNОценок пока нет
- Wayfinding and Architectural Design in Eye HospitalsДокумент3 страницыWayfinding and Architectural Design in Eye HospitalsIqRa JaVedОценок пока нет
- Scurt Istoric FracturiДокумент5 страницScurt Istoric FracturiMusgociu NelaОценок пока нет
- Fertilization, Pregnancy, and Fetal Development: Paul F. Terranova, PH.DДокумент23 страницыFertilization, Pregnancy, and Fetal Development: Paul F. Terranova, PH.DChairul Nurdin AzaliОценок пока нет
- MCN Lect Multiple Pregnancy Hydramnios PosttermДокумент5 страницMCN Lect Multiple Pregnancy Hydramnios PosttermAmethystОценок пока нет
- ReportsДокумент2 страницыReportssawtulhassanОценок пока нет
- Ac Resume 1Документ1 страницаAc Resume 1api-438312001Оценок пока нет
- Dr Jayasree's CV for HospitalityДокумент3 страницыDr Jayasree's CV for HospitalitySathish KumarОценок пока нет
- Osteosintesis Ortognatica MandibulaДокумент41 страницаOsteosintesis Ortognatica MandibulaMaria Mercedes Rosales NuñezОценок пока нет
- Antenatal Care: Routine Care For The Healthy Pregnant WomanДокумент304 страницыAntenatal Care: Routine Care For The Healthy Pregnant WomanNadia Gina AnggrainiОценок пока нет
- UG Assessment Form AIIДокумент39 страницUG Assessment Form AIIdrpklalОценок пока нет
- Cardinal Santos Profile 2Документ4 страницыCardinal Santos Profile 2Nina Fatima AllamОценок пока нет
- Pi Care of Third and Fourth Degree Tears OasiДокумент6 страницPi Care of Third and Fourth Degree Tears OasiPetros Akin-NibosunОценок пока нет
- Svvfuip Brochure VersionДокумент16 страницSvvfuip Brochure VersionViswasukthamОценок пока нет
- Achilles Tendon Rupture: What Is The Achilles Tendon? Signs and SymptomsДокумент2 страницыAchilles Tendon Rupture: What Is The Achilles Tendon? Signs and SymptomsChristian RezaОценок пока нет
- Final Report - Development of Patient-Centered Infrastructure Master Plans For VSS Medical PDFДокумент207 страницFinal Report - Development of Patient-Centered Infrastructure Master Plans For VSS Medical PDFamar jeetОценок пока нет