Академический Документы
Профессиональный Документы
Культура Документы
Hepatopulmonary Syndrome (2014)
Загружено:
Robert G. Gish, MD0 оценок0% нашли этот документ полезным (0 голосов)
111 просмотров47 страницHepatopulmonary Syndrome (2014)
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документHepatopulmonary Syndrome (2014)
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
111 просмотров47 страницHepatopulmonary Syndrome (2014)
Загружено:
Robert G. Gish, MDHepatopulmonary Syndrome (2014)
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 47
Hepatopulmonary Syndrome
Hypoxia in a hepatic patient
INTRINSIC LUNG DISEASE
Specific Liver Diseases
Portal Hypertension, Cirrhosis
Pulmonary Vascular Changes
RELATED TO LIVER DISEASE
COPD, Asthma, CHF
INTRINSIC LUNG DISEASE
RELATED TO LIVER DISEASE
Pulmonary vascular disorders 20-30%
Chronic obstructive pulmonary disease 17%
Asictes, hepatic hydrothorax 5%
Congestive heart failure 5%
Specific liver diseases 3%
Deconditioning 2%
Asthma 1%
Fallon et al, Gastro 2008;135:1168-1175
Dilation
60%
Normal
32%
Constriction
8%
THE PULMONARY VASCULATURE IN LIVER
DISEASE
HPS
HPS: Definition
Hypoxemia in cirrhosis
due to
IPVD (saline bubble contrast echo)
Intrinsic Cardiopulmonary disease
MAA scan role
Data needed for MELD exception
HEPATOPULMONARY SYNDROME (HPS)
DEFINITION
HPS is characterized by a defect in arterial oxygenation
Induced by pulmonary vascular dilatation and pulmonary
AV shunting in the setting of liver disease.
HEPATOPULMONARY SYNDROME (HPS)
DEFINITION
Cirrhosis and/or portal hypertension
Arterial p0
2
< 70mmHg or A-aPO
2
> 20 mmHg
Intrapulmonary vasodilatation
Rodriguez-Roisin, Thorax 1992, Eur Respir J 2004
A-aPO
2
: 150- PaCO
2
/0.8 PaO
2
NL age corrected A-aPO
2
: 10 + (age-20) (0.43)
HPS: DIAGNOSIS
Arterial Blood Gas : PaO2 < 70 mmHg
Cardiopulmonary Evaluation
Intrapulmonary vasodilatation
Contrast echocardiography (CE)
Lung perfusion scan (MAA)
Diagnosis of HPS
Chest radiograph and pulmonary function tests are
helpful to exclude other cardiopulmonary abnormalities.
Causes of hypoxemia in a cirrhotic patient include,
ascites, atelectasis, COPD, and hepatic hydrothorax.
The presence of AV shunting establishes the diagnosis
of HPS regardless the presence of cardiopulmonary
disease by radiography.
HPS: SPECTRUM OF DISEASE
Portal vein thrombosis Gupta Gastro 2001
IVC obstruction Binay Gastro 2000
Acute hepatitis Regev AJ Vir Hep 2001, Fuhrmann, Gastro 2006
Chronic hepatitis Teuber Eur J Int Med 2002
HPS: Frequency/Severity
268 OLT evaluations (6 centers)
AaPO2 103/268 38%
IPVD 117/268 44%
HPS 44/268 16%
- AaPO2 40 (22-79)
- PaO2 65 (35-90)
- MELD 13 (7-23)
Mechanism
The exact mechanism is unknown.
Alteration in the production or clearance of chemical
mediators causing intrapulmonary vascular dilatation
and significant AV shunting.
Hypoxia is due to inability of oxygen to diffuse through
the markedly dilated lung capillaries (V/Q mismatch).
Mechanism
Nitric oxide, a potent vasodilator, is exhaled in larger
quantities in patients with HPS and normalizes
following OLT.
Gram negative intestinal endotoxemia in portal HTN
associated with increased NO release can induce
pulmonary vasodilatation.
Mechanism
Capillary vasodilataion is most pronounced at the lung
bases leading to platypnea and orthodeoxia.
Pulmonary vasodilataion leads to increased pulmonary
blood flow and increased COP.
This leads to V/Q mismatch.
PORTAL HYPERTENSION MECHANISMS
VARICES
CARDIAC
Endothelial cell
Stellate cell
Nitric oxide
Constriction
Fibrosis
Nitric oxide
Vasodilation
Angiogenesis
Splanchnic
Systemic Vasodilation
Intrahepatic
Vasoconstriction
Inflammatory cells
ASCITES
HRS
PSE
Pulmonary
HPS, POPH
Portal Hypertension
Cirrhosis
Portosystemic shunting
HPS
Pulmonary
vasodilatation
? Angiogenesis
Normal
Pulmonary
Microvasculature
Abnormal ABGs
40-50% 40-60%
50%
Rodriguez-Roisin et al , Thorax 1992, Eur Respir J 2004
Clinical presentation
Typically, dyspnea, platypnea, and orthodeoxia.
Cyanosis in 90% of cases.
Clubbing
Spider nevi are common and represent a cutaneous
marker of intrapulmonary vascular dilatation.
Clinical Types of HPS
Type I HPS: characterized by vascular dilatation at the
precapillary level, close to the normal gas exchange
units of the lung.
Type II HPS: characterized by focal larger dilatations
amounting to AV shunting distant from gas exchange
units.
100% oxygen inhalation improves type I HPS PaO2 but
not type II.
HPS: Screening
200 OLT evaluations
Pulse oximetry overestimates PaO2
Spo
2
<96% would lead to ABG in ~12% of cohort
Abrams, Liver Transplantation, 2002
4 Chamber View
Contrast Echocardiography
Immediate Post-Contrast
Delayed Post Contrast
HPS: MAA scan
Abrams, Gastroenterology 1998
50
60
70
80
90
100
-20 0 20 40 60 80 100
W
a
k
e
t
i
m
e
P
a
O
2
m
m
H
g
TST-SpO2<90%
Controls (n=10)
HPS (n=10)
Median TST-SpO2 <90%
HPS (25%) vs. Controls (0%)
p = 0.0005
Nocturnal pulse oximetry and HPS
Palma et al. Hepatology 47: 1257-63, 2008
0
20
40
60
80
100
Dyspnea Clubbing Spiders
HPS (30)
non-HPS (181)
HPS: CLINICAL FEATURES
Martinez, 2001, Sood, 1998
93-100%
20-49%
46-64%
8%
73-100%
44-70%
Prognosis of HPS
The median survival time in cirrhotic patients with HPS
is ~ 10.6 months compared to 40.8 months in cirrhotic
patients without HPS.
Survival is worse when PaO2 is low ( 50 mmHg).
The leading cause of death is shock secondary to GI
bleeding.
Portal Hypertension
Chronic Liver Disease
CXR, ABG, PFT, Chest CT
Abnormal gas exchange
No intrinsic
cardiopulmonary disease
Contrast Echocardiogram
Normal
No HPS
Delayed Shunting
(>3 heartbeats)
HPS
Abnormal gas exchange
Intrinsic cardiopulmonary
disease
Contrast Echocardiogram
MAA if hypoxia and delayed
shunting
Swanson, Hepatology 2005
24 months
Schenk, Gastroenterology 2003
HPS: Natural history without OLT
(n=20)
(n=70)
5 mmHg/year
87 months
Survival effect
Progression over time
0
20
40
60
80
100
0 6 12 18 24 30 36 42 48
P
e
r
c
e
n
t
S
u
r
v
i
v
i
n
g
Follow up time in months
HPS: SURVIVAL PRIOR TO LT
Adapted from: Schenk et al Gastroenterology 2003 125:1042-52
HPS (n=27)
Non HPS (n=84)
P = 0.018
0
20
40
60
80
100
0 6 12 18 24 30 36 42 48
P
e
r
c
e
n
t
S
u
r
v
i
v
i
n
g
Follow up time in months
Adapted from: Swanson et al 2005 Hepatology 41: 1122-1129
HPS (n=37)
Non HPS (n=47)
P = 0.0003
HPS: SURVIVAL PRIOR TO LT
0
20
40
60
80
100
0 6 12 18 24 30 36 42 48
P
e
r
c
e
n
t
S
u
r
v
i
v
i
n
g
Follow up time in months
UAB
Columbia
Mayo Clinic
UNC
U. Colorado
Tufts-NEMC
Adapted from: Fallon et al Gastroenterology 2008 135: 1168-75
HPS (n=72)
Non HPS (n=146)
P = 0.013 (adjusted for age, gender, BMI, MELD, LT, PaO2)
HPS: SURVIVAL PRIOR TO LT
HPS: Markov model
CP-A
No-HPS
CP-B/C
No-HPS
CP-A
HPS
Death
CP-B/C
HPS
OLT
HPS: Modeling
Discounted Analysis (3%) Cost
Incremental
Cost
Life
Expectancy
Incremental
Life
Expectancy ICER
Pulse-oximetry $284,710 ------ 11.310 --------
Dyspnea-fatigue index $285,200 $490 11.313 0.003 years $163,333
No screening $291,898 $6,690 11.131 - 0.182 years Dominated
Discounted Analysis (3%) Cost
Incremental
Cost
Life
Expectancy
Incremental
Life
expectancy ICER
No screening $289,495 ------ 12.04 --------
Pulse Oximetry $299,719 $10,224 12.27 0.23 years $45,452
Dyspnea-Fatigue Index $300,278 $559 12.28 0.01 years $55,900
All Patients with HPS Eligible for OLT
Patients with HPS and PaO2 > 50mmHg Eligible for OLT
1) Uniform diagnostic data for exception
- RA ABG, bubble echo, CXR, PFTs IPVD, A-a gradient common
- MAA only if CXR/PFTs abnormal
2) Eligibility at PaO2 < 60mmHg Natural hx data, ABG decline
3) Prospective data to assess policy
- Screen listed pts (pulse oximetry q 12 months) ? Incidence, ? Influence of PaO2
- ABG q 3- 6 months with HPS exception pre and post OLT
- Track mortality, LOS, cause of death
RECOMMENDATION RATIONALE
HEPATOPULMONARY SYNDROME (HPS)
MELD EXCEPTION
Definition/Diagnosis
Frequency/Severity
Natural History
Impact of OLT
Modeling of screening
Recommendations
46% (14)
36% (12)
18% (5)
PaO
2
in HPS patients at LT evaluation
(31% of patients had HPS)
UAB
Columbia
Mayo Clinic
UNC
U. Colorado
Tufts-NEMC
LT EVALUATION
Pulse
Oximetry
96%
TTE
95%
CTTE
Shunt No shunt
ABGs
CXR, PFTs, Chest CT
Other causes
PaO2 60 PaO2>60
MELD
ABG 3-6m
Monitor
Treat
Low PO2 HPS
Abrams, Liver Transpl. 2002:8;391-6
Roberts, Liver Transpl. 2007:13:206-14
Arguedas, Clin Gastro Hepatol. 2007:5;749-54
Kochar, Dig Dis Sci. 2011:56;1862-8
HPS: Outcome with OLT
Type # Post-op Mortality Pre-op PaO2
Taile R 23 30% 51.4 (33-64)
Arguedas P 24 29% 43 (35-51)
Swanson R 24 21% 40.6 (33-51)
Schenk P 7 42% 66 (60-79)
Collison R 6 50% 57.2 (40-84)
Schiffer P 9 33% 60 (52-70)
93 34%
HPS: Outcome with OLT
Type # Post-op Mortality Pre-op PaO2
Taile R 23 30% 51.4 (33-64)
Arguedas P 24 29% 43 (35-51)
Swanson R 24 21% 40.6 (33-51)
Schenk P 7 42% 66 (60-79)
Collison R 6 50% 57.2 (40-84)
84 34%
PaO2 and MELD appear to
Influence outcome
Study Study design Sample
Size
Mean
PaO
2
mmHg
Length of
follow-up
(months)
Survival
Arguedas (2003) Prospective 24 54 12 71%
Taille (2003) Retrospective 23 51 17 69%
Schenk (2003) Prospective 7 68 58%
Swanson (2005) Retrospective 24 57 60 79%
Schiffer (2006) Prospective 9 60 6 67%
Deberaldini (2008) Retrospective 25 77 49 60%
Gupta (2009) Retrospective 21 50 20 95%
HPS: OUTCOME AFTER OLT
(2003)
(2008)
(2006)
(2003)
(2003)
(2005)
(2009)
40
50
60
70
80
50 60 70 80 90 100
P
a
O
2
(
m
m
H
g
)
1 Year Survival (%)
HPS: OUTCOME AFTER OLT
0
20
40
60
80
100
0 3 6 9 12
S
u
r
v
i
v
a
l
(
%
)
Follow up (months)
0
10
20
30
40
50
60
50
9
59
18
53
9
43
41
Alive
Expired
*
*
HPS FEATURES AND LT OUTCOME
Arguedas Hepatol. 2003:37;192-197
Treatment of HPS
Oxygen
Liver transplant
No effective medical treatment is available.
Somatostatin analogues, cyclooxygenase inhibitors, and immunosuppressive agents
have poor results.
Almitrine bismesylate (a selective pulmonary vasoconstrictor) shows promising
results.
Garlic (Allium sativum) powder has a modest effect.
TIPS.
Thank you to:
Mike Fallon for his slide sharing generosity
Вам также может понравиться
- MediastinumДокумент27 страницMediastinumAndrei PanaОценок пока нет
- Atrial Septal DefekДокумент29 страницAtrial Septal DefekChe Ainil ZainodinОценок пока нет
- Pneumothorax, Tension and TraumaticДокумент29 страницPneumothorax, Tension and TraumaticicaОценок пока нет
- PneumothoraxДокумент14 страницPneumothoraxAsterlita WenasОценок пока нет
- Radiologi ILO Terbaru (PIPKRA 2011)Документ47 страницRadiologi ILO Terbaru (PIPKRA 2011)elsaОценок пока нет
- Ventilator Associated Pneumonia (Vap)Документ11 страницVentilator Associated Pneumonia (Vap)Suresh KumarОценок пока нет
- Diagnosis of PneumoconiosisДокумент55 страницDiagnosis of PneumoconiosiselsaОценок пока нет
- Kuliah 16 Cor PulmonaleДокумент41 страницаKuliah 16 Cor PulmonalecaturwiraОценок пока нет
- The Immune Reconstitution Inflammatory SyndromeДокумент7 страницThe Immune Reconstitution Inflammatory SyndromeAlexandra PaunОценок пока нет
- Asthma + COPD - 2022 LectureДокумент85 страницAsthma + COPD - 2022 Lecturedesti purnama sariОценок пока нет
- Understanding Pulmonary MycosesДокумент33 страницыUnderstanding Pulmonary MycosesselviaОценок пока нет
- Adult Questionnaire Self-CompletionДокумент39 страницAdult Questionnaire Self-CompletionAnnisa Ratna DОценок пока нет
- Gagal Napas: Pembimbing Dr. Ngakan Putu Parsama Putra, SPP (K) Presenter Dr. Muli YamanДокумент20 страницGagal Napas: Pembimbing Dr. Ngakan Putu Parsama Putra, SPP (K) Presenter Dr. Muli YamanAdlan BinharyantoОценок пока нет
- Ards 2Документ7 страницArds 2LUCIBELLOT1Оценок пока нет
- Gold 2019Документ43 страницыGold 2019Hayatillah Natasya100% (1)
- Interpreting ABG ResultsДокумент28 страницInterpreting ABG Resultsmafoel39Оценок пока нет
- AdrenalineДокумент20 страницAdrenalinecreatativeОценок пока нет
- Modern View of AsthmaДокумент27 страницModern View of AsthmaraisaОценок пока нет
- Adenosine Deaminase: The Test SampleДокумент1 страницаAdenosine Deaminase: The Test Sampleja_sam_radivoje3093Оценок пока нет
- Therapeutically Administered Ribonucleoside Analogue Mk-4482/Eidd-2801 Blocks Sars-Cov-2 Transmission in FerretsДокумент15 страницTherapeutically Administered Ribonucleoside Analogue Mk-4482/Eidd-2801 Blocks Sars-Cov-2 Transmission in FerretsCarlosgustavo SaavedrarubioОценок пока нет
- HP Diagnosis ChallengesДокумент51 страницаHP Diagnosis ChallengesskchhabraОценок пока нет
- CVP Guided Deresuscitation in Managing Overload in Icu PDFДокумент57 страницCVP Guided Deresuscitation in Managing Overload in Icu PDFJonathan Hamm100% (1)
- DR Syed Aqeel Gilani Department of Pulmonology Ayub Teaching Hospital AbbottabadДокумент49 страницDR Syed Aqeel Gilani Department of Pulmonology Ayub Teaching Hospital AbbottabadAnka EremiaОценок пока нет
- Invasive Pulmonary Aspergi Llosis: Seminars in Respiratory and Critical Care MedicineДокумент24 страницыInvasive Pulmonary Aspergi Llosis: Seminars in Respiratory and Critical Care MedicineChengShiun ShiueОценок пока нет
- Asmiua UrologyДокумент2 страницыAsmiua UrologylewandowskyОценок пока нет
- 1.2. PneumothoraxДокумент42 страницы1.2. PneumothoraxFarahRullyta100% (1)
- 2nd Announcement JakNews 2024Документ19 страниц2nd Announcement JakNews 2024Nando EllaОценок пока нет
- COPD SlidesДокумент27 страницCOPD SlidesMelito Vergara IIОценок пока нет
- ARDS (Dr. Edi Nurtjahja - SP.P)Документ23 страницыARDS (Dr. Edi Nurtjahja - SP.P)Mirna Ayu Permata SariОценок пока нет
- Pneumonia AlgorithmДокумент3 страницыPneumonia AlgorithmBien ChuОценок пока нет
- Kul Sem 4 Heat Stroke N Fever UHT 2016Документ63 страницыKul Sem 4 Heat Stroke N Fever UHT 2016NandaSuryaWijayaОценок пока нет
- Gap Co2 Cocc 2018Документ9 страницGap Co2 Cocc 2018Cesar Rivas CamposОценок пока нет
- NSTEMI Refarat Cardio 2016Документ48 страницNSTEMI Refarat Cardio 2016Anonymous IOkNvM8VbtОценок пока нет
- Copd PDFДокумент28 страницCopd PDFDarawan MirzaОценок пока нет
- Treatment of ARDS: Ventilation, Fluids, NutritionДокумент15 страницTreatment of ARDS: Ventilation, Fluids, Nutritionf3wlОценок пока нет
- Acute Lung Injury/Acute Respiratory Distress Syndrome: Deepak Mulajker, Vasu Vardhan, AK NagpalДокумент6 страницAcute Lung Injury/Acute Respiratory Distress Syndrome: Deepak Mulajker, Vasu Vardhan, AK NagpalDeepak MulajkerОценок пока нет
- Kurva Disosiasi HB OksigenДокумент6 страницKurva Disosiasi HB Oksigenhendra_darmawan_4Оценок пока нет
- Respiratory Diseases Commonly FoundДокумент29 страницRespiratory Diseases Commonly FoundyudhaОценок пока нет
- COPD - Update Diagnosis and Management of Stable COPDДокумент29 страницCOPD - Update Diagnosis and Management of Stable COPDIwanОценок пока нет
- Kuliah Kanker Paru 1 Oleh Prof BenДокумент77 страницKuliah Kanker Paru 1 Oleh Prof Benmemphis3Оценок пока нет
- Update in Diagnosis and Management of Interstitial Lung DiseaseДокумент8 страницUpdate in Diagnosis and Management of Interstitial Lung DiseaseTimothy23 SiregarОценок пока нет
- Bab I Pendahuluan 1.1. Latar BelakangДокумент18 страницBab I Pendahuluan 1.1. Latar BelakangAntasiaSiregarОценок пока нет
- PDF Heart FailureДокумент30 страницPDF Heart FailureNitya Manggala JayaОценок пока нет
- GLomerulus DiseaseДокумент5 страницGLomerulus DiseaseMEDS easyОценок пока нет
- Bronchitis Acute and ChronicДокумент3 страницыBronchitis Acute and Chronicdwi rina putriОценок пока нет
- Kuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)Документ17 страницKuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)DillaОценок пока нет
- Types of FeverДокумент16 страницTypes of Fevercute_ildz0% (1)
- Toxic GasesДокумент21 страницаToxic GasesBestariNugrahiniОценок пока нет
- Lutembacher's Syndrome at KolonodaleДокумент7 страницLutembacher's Syndrome at KolonodaleWayan GunawanОценок пока нет
- Adrenal DisordersДокумент32 страницыAdrenal DisordersJyoti ChadhaОценок пока нет
- Pneumocystis Carinii PneumoniaДокумент16 страницPneumocystis Carinii PneumoniaHera HeraОценок пока нет
- ASMAДокумент61 страницаASMAdinimusman100% (1)
- Pleural Effusion Diagnosis and TreatmentДокумент35 страницPleural Effusion Diagnosis and TreatmentAlfina Aulia RizkiОценок пока нет
- Sars Vs CovidДокумент11 страницSars Vs CovidYu Theng ChumОценок пока нет
- Final 2nd Announcement Konas Perdatin Perdici 2019 - WebsiteДокумент65 страницFinal 2nd Announcement Konas Perdatin Perdici 2019 - Websitetia_drОценок пока нет
- 2016-1014 ARDS Update v3.0Документ75 страниц2016-1014 ARDS Update v3.0Edwin CvОценок пока нет
- Jurnal AMS PDFДокумент8 страницJurnal AMS PDFputriseptinaОценок пока нет
- Timebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisОт EverandTimebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesОт EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodОценок пока нет
- CBD DR SaugiДокумент36 страницCBD DR SaugiQisthy Kurrota AiniОценок пока нет
- Cost of Curing HCVДокумент36 страницCost of Curing HCVRobert G. Gish, MDОценок пока нет
- Hepatitis C Virus As A Systemic Disease: Reaching Beyong The LiverДокумент9 страницHepatitis C Virus As A Systemic Disease: Reaching Beyong The LiverRobert G. Gish, MDОценок пока нет
- Letter To MHPA Jeff MyersДокумент4 страницыLetter To MHPA Jeff MyersRobert G. Gish, MDОценок пока нет
- CDC Lab 2016 - Hepatitis Testing A-EДокумент8 страницCDC Lab 2016 - Hepatitis Testing A-ERobert G. Gish, MDОценок пока нет
- Hepatitis C Rallies in San FranciscoДокумент1 страницаHepatitis C Rallies in San FranciscoRobert G. Gish, MDОценок пока нет
- CME Conference: Hepatitis C From A To ZДокумент2 страницыCME Conference: Hepatitis C From A To ZRobert G. Gish, MDОценок пока нет
- Hepatitis C Policy California MedicaidДокумент4 страницыHepatitis C Policy California MedicaidRobert G. Gish, MDОценок пока нет
- Centers For Medicare & Medicaid Services Letter To StatesДокумент4 страницыCenters For Medicare & Medicaid Services Letter To StatesRobert G. Gish, MDОценок пока нет
- Presentation at The 2015 Liver SummitДокумент211 страницPresentation at The 2015 Liver SummitRobert G. Gish, MDОценок пока нет
- Cost Effectiveness and Budget Impact of Treating HCVДокумент12 страницCost Effectiveness and Budget Impact of Treating HCVRobert G. Gish, MDОценок пока нет
- Stanford Clinic in San FranciscoДокумент1 страницаStanford Clinic in San FranciscoRobert G. Gish, MDОценок пока нет
- Stanford Clinic in SacramentoДокумент1 страницаStanford Clinic in SacramentoRobert G. Gish, MDОценок пока нет
- Presentation: SOTA 2015Документ140 страницPresentation: SOTA 2015Robert G. Gish, MDОценок пока нет
- Article in The Journal of Medical Practice ManagementДокумент5 страницArticle in The Journal of Medical Practice ManagementRobert G. Gish, MDОценок пока нет
- Article: Hepatology - Prevalence of Chronic HBV and HCVДокумент3 страницыArticle: Hepatology - Prevalence of Chronic HBV and HCVRobert G. Gish, MDОценок пока нет
- Conference: Focus On The Hepatitis B VirusДокумент52 страницыConference: Focus On The Hepatitis B VirusRobert G. Gish, MDОценок пока нет
- Dr. Gish LectureДокумент1 страницаDr. Gish LectureRobert G. Gish, MDОценок пока нет
- Message From CEVHAPДокумент2 страницыMessage From CEVHAPRobert G. Gish, MDОценок пока нет
- CEVHAP PamphletДокумент2 страницыCEVHAP PamphletRobert G. Gish, MDОценок пока нет
- Event: BEYOND THE WALLS OF THE CLINICДокумент1 страницаEvent: BEYOND THE WALLS OF THE CLINICRobert G. Gish, MDОценок пока нет
- Changing Nomenclature For PBC: From Cirrhosis' To Cholangitis'Документ3 страницыChanging Nomenclature For PBC: From Cirrhosis' To Cholangitis'Robert G. Gish, MDОценок пока нет
- The Hepatitis C Education and Support Group Assistance ProgramДокумент1 страницаThe Hepatitis C Education and Support Group Assistance ProgramRobert G. Gish, MDОценок пока нет
- Press ReleaseДокумент3 страницыPress ReleaseRobert G. Gish, MDОценок пока нет
- CEVHAP Membership Application FormДокумент1 страницаCEVHAP Membership Application FormRobert G. Gish, MDОценок пока нет
- Gish - Et - Al-2015-Hepatology HBV HCV New EstimatesДокумент8 страницGish - Et - Al-2015-Hepatology HBV HCV New EstimatesRobert G. Gish, MDОценок пока нет
- HCV Policy Presentation 2015Документ18 страницHCV Policy Presentation 2015Robert G. Gish, MDОценок пока нет
- Abnormal Liver Tests PresentationДокумент63 страницыAbnormal Liver Tests PresentationRobert G. Gish, MD100% (1)
- Advisory Letter 2015Документ1 страницаAdvisory Letter 2015Robert G. Gish, MDОценок пока нет
- Final Comments On Medicaid MCO Proposed RuleДокумент8 страницFinal Comments On Medicaid MCO Proposed RuleRobert G. Gish, MDОценок пока нет
- Gish - Et - Al-2015-Hepatology HBV HCV New EstimatesДокумент8 страницGish - Et - Al-2015-Hepatology HBV HCV New EstimatesRobert G. Gish, MDОценок пока нет
- DiazepamДокумент7 страницDiazepamنمر نصارОценок пока нет
- Tetralogy of FallotДокумент5 страницTetralogy of FallotNoor FadhilaОценок пока нет
- Dr. T. Perungo - Arinaa Obesity Bariatric CoEДокумент11 страницDr. T. Perungo - Arinaa Obesity Bariatric CoEbhagavathi.muruganpillai6851Оценок пока нет
- FAQs for Vaccination Site Staff on COVID-19 Vaccines in ChildrenДокумент11 страницFAQs for Vaccination Site Staff on COVID-19 Vaccines in ChildrenzzОценок пока нет
- A Read-Along Coloring Book About Surgey at Children SДокумент24 страницыA Read-Along Coloring Book About Surgey at Children SMiguel Ángel Palacio RodríguezОценок пока нет
- Principles of Tendon Transfer in The Hand and ForearmДокумент9 страницPrinciples of Tendon Transfer in The Hand and Forearm'Ema Surya PertiwiОценок пока нет
- CPDProgram Medicine 122719 PDFДокумент1 137 страницCPDProgram Medicine 122719 PDFhotknifeОценок пока нет
- Adolescent Health Guidelines FOGSIДокумент28 страницAdolescent Health Guidelines FOGSISandip PatilОценок пока нет
- Trip Report Technical WritingДокумент3 страницыTrip Report Technical Writingapi-550629785Оценок пока нет
- Radial Styloid (Chauffeur) FractureДокумент9 страницRadial Styloid (Chauffeur) Fractureanon_612448249Оценок пока нет
- DMSCO Log Book Vol.39 3-12/1961Документ41 страницаDMSCO Log Book Vol.39 3-12/1961Des Moines University Archives and Rare Book RoomОценок пока нет
- Immunology PDFДокумент1 страницаImmunology PDFTanushree PalОценок пока нет
- Atropine Sulfate for Bradycardia and PoisoningДокумент4 страницыAtropine Sulfate for Bradycardia and PoisoningSuraya_Mohamed_3281Оценок пока нет
- List of Accredited CPD Providers As of March 2022Документ6 страницList of Accredited CPD Providers As of March 2022Tariku GelesheОценок пока нет
- Bio Emulation Edinburgh EventsДокумент8 страницBio Emulation Edinburgh EventsAing MaungОценок пока нет
- The Hebrew and The Arabic Version of The LittlEARS® Auditory Questionnaire For The Assessment of Auditory Development - Results in Normal Hearing Children and Children With Cochlear ImplantsДокумент6 страницThe Hebrew and The Arabic Version of The LittlEARS® Auditory Questionnaire For The Assessment of Auditory Development - Results in Normal Hearing Children and Children With Cochlear ImplantsRonald Ivan WijayaОценок пока нет
- Molecular Mechanism of Cancer MetastasisДокумент43 страницыMolecular Mechanism of Cancer MetastasisDipesh Ludhwani100% (1)
- Canine Idiopathic Linear Pustular Acantholytic Dermatosis - A Second CaseДокумент1 страницаCanine Idiopathic Linear Pustular Acantholytic Dermatosis - A Second CasejenОценок пока нет
- Wholesale Botox Supplier UKДокумент1 страницаWholesale Botox Supplier UKreliablemedicareОценок пока нет
- Reliability and Accuracy of The Lower Incisor Mandibular Plane Angle - Proposed Correction FactorДокумент5 страницReliability and Accuracy of The Lower Incisor Mandibular Plane Angle - Proposed Correction FactorAmeliaDiansariОценок пока нет
- OrthoNeuro Neurologist Dr. Martin Taylor Enrolls First Patient in The United States and Australia For New Parkinson's Phase 3 Research TrialДокумент2 страницыOrthoNeuro Neurologist Dr. Martin Taylor Enrolls First Patient in The United States and Australia For New Parkinson's Phase 3 Research TrialPR.comОценок пока нет
- Boost Your Practice With Brain Health CoachingДокумент4 страницыBoost Your Practice With Brain Health CoachingClint RumboltОценок пока нет
- Diagnosis and Management of Ulnar Nerve PalsyДокумент20 страницDiagnosis and Management of Ulnar Nerve PalsyamaliafarahОценок пока нет
- Effect of Conditioned Fear Stress On Serotonin Metabolism in The Rat BrainДокумент4 страницыEffect of Conditioned Fear Stress On Serotonin Metabolism in The Rat BrainJef_8Оценок пока нет
- PALICC - Pediatric - ARDS Consensus PDFДокумент12 страницPALICC - Pediatric - ARDS Consensus PDFCarkos MorenoОценок пока нет
- Management TOF in AdultДокумент103 страницыManagement TOF in AdultBagus Budi SantosoОценок пока нет
- Adding An "R" in The "DOPE" Mnemonic For Ventilator TroubleshootingДокумент1 страницаAdding An "R" in The "DOPE" Mnemonic For Ventilator TroubleshootingkelvinaОценок пока нет
- 2016-17 Match Book Final Final Sep 2, 2016Документ41 страница2016-17 Match Book Final Final Sep 2, 2016TommyОценок пока нет
- Couden - Community Health Promotion PaperДокумент11 страницCouden - Community Health Promotion Paperapi-449016836Оценок пока нет
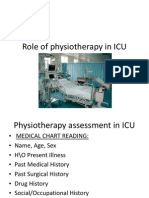
- Role of Physiotherapy in ICUДокумент68 страницRole of Physiotherapy in ICUprasanna3k100% (2)