Академический Документы
Профессиональный Документы
Культура Документы
Vasovagal Syncope
Загружено:
Emily EresumaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Vasovagal Syncope
Загружено:
Emily EresumaАвторское право:
Доступные форматы
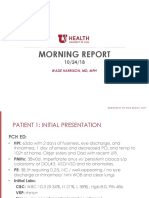
MORNING REPORT
08/06/14
WEI SONG
TRIPLE BOARD YEAR 3
HISTORY
12 year old girl with history of severe depression, PTSD, and 3 prior suicide attempts presents
with 3 week history of feeling lightheaded and passing out.
Over last week had daily episodes of pre-syncope or syncope, especially when standing up
quickly. Improve with continued activity, though she is not an active girl.
Pro-drome of tremulousness, tunnel vision, and dizziness.
Has been tired all month, sleepy, fatigue
Yesterday had syncope at home: fell from toilet in bathroom, hit head on edge of tub
Today went to urgent care when she had symptoms again at grandmothers house.
At urgent care had BP of 80/40, received 500cc NS then transferred to PCH
Initial EKG showed 1
st
degree AV block, no QTc prolongation
MORE HISTORY
PMH:
Severe depression with 3 suicide attempts, 2 inpt hospitalizations, auditory and visual
hallucinations. Denies current SI or intent.
PTSD related to father committing suicide, intense nightmares helped by prazosin
Self-harm (cutting) behaviors when stressed
Transient prolonged QT with trazodone overdose five months ago
Genetic COX-1 disorder that leads to easy bruising
No PCP. Seen by an outpatient psychiatrist.
Surg Hx:
Tonsillectomy and Adenoidectomy
MORE HISTORY
Home Medications:
Prazosin 2mg QHS (Started 5 months ago)
Cymbalta 60mg PO qAM (Started 1 month ago)
Abilify 5mg PO QHS (Started 5 months ago)
Used to take Prozac prior to Cymbalta
Mom locks up all her meds and administers them to her.
Immunizations up to date
Allergies: Amoxicillin (Rash)
Diet: Normal for age. Likes burgers and fries. Eats all meals. Drinks many large cups of water
each day though notes urine is sometimes dark.
MORE HISTORY
FH:
h/o of Asthma
Father committed suicide with a gun (h/o depression)
No h/o arrhythmia, heart failure, SIDS, hearing defects or sudden death
SH:
Lives with mom. Legal guardianship held by mom.
Just started period five days ago, about to end today. Periods regular.
PHYSICAL FINDINGS
VS:
T 36.2, HR 57, RR 18, BP 104/56, SaO2 98% on Room Air
Weight 61.7 kg (91%ile), Height 168.0 cm (95%ile)
Orthostatics:
Supine BP 103/58, HR 68
Sitting BP 98/55, HR 84
Standing BP 100/71, HR 122
PHYSICAL FINDINGS
Gen Lying in bed asleep, appropriately arousable, NAD
HEENT NCAT; PERRL, EOMI, No conjunctival injection; TM normal; No nasal discharge or obstruction; mildly
dry mucus membranes, tonsils symmetric without exudate; no pharyngeal erythema or lesions; No LAD
CV RRR, S1 S2 normal with normal splitting of S2, no murmur rubs or gallops; cap refill < 3 secs; distal pulses
palpable in upper and lower extremities
Lungs: CTAB, good air flow, no wheezing or rales, no retractions
Abd: Soft, NT, ND, NO HSM. No bruits
Extremities: No clubbing cyanosis or edema, warm extremities
Neurological: Sleeping but appropriate arousal to light touch, CN II XII grossly intact, grossly normal strength
and tone. Patellar reflexes normal bilaterally. After fluids was able to get up from sleeping position, to a sitting
position, then stand up walk steadily to the bathroom.
DIFFERENTIAL
Long QT syndrome
Brugada syndrome
Catecolaminergic polymorphic ventricular tachycardia
Preexcitation syndrome (e.g. WPW)
Congenital short QT syndrome
Hypertrophic Cardiomyopathy
Coronary Artery anomalies
Valvar aortic stenosis
Pulmonary hypertension
Dilated cardiomyopathy
Acute myocarditis
Heat illness
Anaphylaxis
Vasovagal syncope
Breath holding spells
Orhtostatic hypotension
Toxic exposure / Medication
Hypoglycemia
SVT
Bradycardia
Seizures
Migraines
Conversion
Hyperventilation
Intentional strangulation
Narcolepsy
Intentional ingestion of meds
VASOVAGAL SYNCOPE
SYNCOPE
Approximately 15% of children experience a syncopal episode prior to end of adolescence
Some evaluating questions:
Exercise During exertion is concerning for cardiac etiology; after is more like vasovagal
Acute arousal or startle Some pt with long QT syndrome can be triggered this way
Postural changes upright prolonged or had just changed positions vasovagal
Pain, or emotional stress vasovagal or certain inherited arrhythmias
Palpitations or chest pain may be concerning for cardiac etiology or vasovagal
Motor activity If it starts at beginning of event, followed by prolonged recovery, think
seizures
SYNCOPE
Past histories:
Congential Heart Disease
Acquired Heart Disease (Kawasaki, rheumatic heart disease, myocarditis)
Arrhythmias
Previous syncopal events
DM or other conditions associated with hypoglycemia
Access to medications or illicit drugs and/or previous history of SA via overdose
Family histories of early cardiac death (<50 years of age), unexplained sudden deaths,
known arrhythmias, familial cardiomyopathies, or vasovagal syncope
VASOVAGAL SYNCOPE
Also known as neurocardiogenic, reflex, or situational syncope.
Most common cause of fainting among children, >50% of cases presenting to ED
Thoughts of causes:
Cardioinhibitory response enhanced parasympathetic tone, drop in heart rate and
contractility, leading to decreasein cardiac output
Vasodepressor response decreased sympathetic tone, drop in blood pressure without
much change in heart rate, most likely due to vasodilation
Clinical features:
Standing or physical or emotional stress, swallowing, hair grooming, micturition
Prodrome of lightheadedness, blurry vision, tunnel vision, double vision, nausea, pallor,
diaphoresis
VASOVAGAL SYNCOPE
Increase oral intake of water to approximately 30-50ml/kg per day
Add salty snacks (e.g. pretzels, pickles, or crackers); may need to add NaCl supplementation if
refractory
Avoid caffeinated beverages
Perform techniques to prevent venous pooling, including keeping knees slightly bent when
standing for a long time; contracting extremity muscles, toe raises, folding of the arms, and
crossing of the legs
A large percentage of patients may improve with non-pharmacologic treatment with oral
fluids and salt intake alone.
Вам также может понравиться
- Syncope, A Simple Guide to the Condition, Treatment and Related DiseasesОт EverandSyncope, A Simple Guide to the Condition, Treatment and Related DiseasesОценок пока нет
- EpilepsyДокумент73 страницыEpilepsyabenezer g/kirstosОценок пока нет
- BEC Module 5 Part 1Документ32 страницыBEC Module 5 Part 1colorred818Оценок пока нет
- Shock in Children TutorialДокумент37 страницShock in Children TutorialSsenyonga DominicОценок пока нет
- Behavioral Disorder by Dr. Mohammed AlneamiДокумент49 страницBehavioral Disorder by Dr. Mohammed AlneamimaithamОценок пока нет
- Case Summary For EmfДокумент19 страницCase Summary For EmfStella CooKeyОценок пока нет
- CPC EncephalitisДокумент42 страницыCPC EncephalitisANSAR AliОценок пока нет
- Atrial FibrillationДокумент13 страницAtrial FibrillationChristianneMikeОценок пока нет
- SyncopeДокумент28 страницSyncopeDurgesh PushkarОценок пока нет
- Hypertension: Colegio de San Juan de LetranДокумент13 страницHypertension: Colegio de San Juan de LetranJenna AbuanОценок пока нет
- High Yield Psychiatry Shelf Exam ReviewДокумент43 страницыHigh Yield Psychiatry Shelf Exam ReviewEdgar SotoОценок пока нет
- Basic Overview of NeurologyДокумент45 страницBasic Overview of NeurologyDith Rivelta CallahanthОценок пока нет
- DeliriumДокумент53 страницыDeliriumakinpe1Оценок пока нет
- The Child With A Neurologic DisorderДокумент42 страницыThe Child With A Neurologic DisorderLeilani FullerОценок пока нет
- Neonatal Seizures: Causes, Treatment and PrognosisДокумент34 страницыNeonatal Seizures: Causes, Treatment and PrognosisClaudiaNathaliaОценок пока нет
- NeuroДокумент87 страницNeuroSHANIA FUNDALОценок пока нет
- High Yield PsychiatryДокумент44 страницыHigh Yield PsychiatryAntony Awad100% (2)
- Fever With HemiplegiaДокумент65 страницFever With HemiplegiaMohit JainОценок пока нет
- NeurologyДокумент58 страницNeurologyDanielle GroupfiveОценок пока нет
- Coma-Causes, Diagnosis, Treatment and ManagementДокумент19 страницComa-Causes, Diagnosis, Treatment and ManagementHabtamu AdimasuОценок пока нет
- Understanding Syncope: Evaluation and Risk StratificationДокумент18 страницUnderstanding Syncope: Evaluation and Risk StratificationMiftahThariqОценок пока нет
- Bipolar Disorder Shelf Exam ReviewДокумент43 страницыBipolar Disorder Shelf Exam Reviewgreg100% (1)
- Approach To SeizuresДокумент60 страницApproach To SeizuresHerrera MiguelОценок пока нет
- Syncope: Ed Da Veiga, M.D. August 20, 2008Документ36 страницSyncope: Ed Da Veiga, M.D. August 20, 2008Abdul SattarОценок пока нет
- Management of Unconscious PatientДокумент51 страницаManagement of Unconscious PatientHylman Mahendra100% (1)
- NP Manages Case of PalpitationsДокумент31 страницаNP Manages Case of PalpitationsoikhileОценок пока нет
- Academic Group OF Internal Medicine - Revision Note of CVA-2010Документ88 страницAcademic Group OF Internal Medicine - Revision Note of CVA-2010abdallhОценок пока нет
- Case Presentation Ob MaternityДокумент44 страницыCase Presentation Ob MaternityRodean Andrew NonatoОценок пока нет
- Management of Severe HypertensionДокумент58 страницManagement of Severe Hypertensioneyobhabtamu3Оценок пока нет
- History of Syncope: A Guide to DiagnosisДокумент6 страницHistory of Syncope: A Guide to DiagnosisIsmail Ali إسماعيل عليОценок пока нет
- High Yield Psychiatry: Shelf Exam Review Emma Holliday RamahiДокумент71 страницаHigh Yield Psychiatry: Shelf Exam Review Emma Holliday RamahisamОценок пока нет
- Media 221736 enДокумент58 страницMedia 221736 ensamОценок пока нет
- Multiple SclerosisДокумент3 страницыMultiple Sclerosisapi-3822433Оценок пока нет
- Atrial Fibrillation CASE STUDYДокумент2 страницыAtrial Fibrillation CASE STUDYChristianneMikeОценок пока нет
- Epilepsy in Adults A Basic IntroductionДокумент40 страницEpilepsy in Adults A Basic IntroductionDrGasnasОценок пока нет
- Neurological Exam LectureДокумент114 страницNeurological Exam LectureLolla SinwarОценок пока нет
- Seizure Disorders in Children: (Febrile Convulsion)Документ16 страницSeizure Disorders in Children: (Febrile Convulsion)Alokh Saha RajОценок пока нет
- Syncope: UCI Internal Medicine Core Curriculum - Mini LectureДокумент15 страницSyncope: UCI Internal Medicine Core Curriculum - Mini LecturechandanОценок пока нет
- Sudden Unexpected Death in EpilepsyДокумент22 страницыSudden Unexpected Death in EpilepsyYu Xiang LinОценок пока нет
- Ems Endocrine and Heme LectureДокумент27 страницEms Endocrine and Heme LectureAhmed NisarОценок пока нет
- BEC Altered Mental Status 2018aДокумент76 страницBEC Altered Mental Status 2018aMaria Hernita SigiroОценок пока нет
- Seizures in Children: Rashmi Kumar Prof & Head, Pediatrics King George Medical University LucknowДокумент47 страницSeizures in Children: Rashmi Kumar Prof & Head, Pediatrics King George Medical University LucknowSonam SonamОценок пока нет
- Evaluating A Patient With Seizure Disorders 2Документ47 страницEvaluating A Patient With Seizure Disorders 2Yvonne Sorviel SiiloОценок пока нет
- SyncopeДокумент83 страницыSyncopeReza SatriaОценок пока нет
- Child Hood Seizuer ManagmantДокумент78 страницChild Hood Seizuer Managmantsentayehu siyumОценок пока нет
- Pernicious AnemiaДокумент75 страницPernicious AnemiaEncee Mian50% (2)
- Movement Disorder in ChildrenДокумент35 страницMovement Disorder in Childrenstandar 1 neuroОценок пока нет
- Case ReportДокумент24 страницыCase Report張仁豪Оценок пока нет
- Alzheimer, ParkinsonДокумент63 страницыAlzheimer, ParkinsonnurulchoriahОценок пока нет
- Approach To The Patient With Headache and Facial PainДокумент25 страницApproach To The Patient With Headache and Facial Painfaza ghaniОценок пока нет
- Alcoholism and substance abuse treatment guideДокумент37 страницAlcoholism and substance abuse treatment guideStephanie RiveraОценок пока нет
- University of Medicine (1) Yangon Community Medicine ProgramДокумент31 страницаUniversity of Medicine (1) Yangon Community Medicine ProgramThuta128Оценок пока нет
- SeizuresДокумент50 страницSeizuresPoonam AggarwalОценок пока нет
- Case Study On CVAДокумент54 страницыCase Study On CVAmolukas10186% (7)
- Systemic Lupus Erithematosus & Marfan's SyndromeДокумент74 страницыSystemic Lupus Erithematosus & Marfan's SyndromeFitriYani SimangunsoNgОценок пока нет
- Catatonia: Kristen Shirey, M.D. Duke University Hospital Internal Medicine and PsychiatryДокумент26 страницCatatonia: Kristen Shirey, M.D. Duke University Hospital Internal Medicine and PsychiatryarunvangiliОценок пока нет
- Delirium and Its ManagmentДокумент64 страницыDelirium and Its ManagmentViren Solanki100% (1)
- Epilepsy 34Документ102 страницыEpilepsy 34Dian zaini PutraОценок пока нет
- Critical Care and ER Lower Back EmergenciesДокумент57 страницCritical Care and ER Lower Back EmergencieschadchimaОценок пока нет
- LECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)Документ57 страницLECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)CristinaGheorgheОценок пока нет
- Investing 101 For Residents: RJ Nemeyer MDДокумент12 страницInvesting 101 For Residents: RJ Nemeyer MDEmily EresumaОценок пока нет
- Kidney Disorders 03.27.2019Документ33 страницыKidney Disorders 03.27.2019Emily EresumaОценок пока нет
- Pediatric Hypertension Noon Conference 03.20.2019Документ44 страницыPediatric Hypertension Noon Conference 03.20.2019Emily EresumaОценок пока нет
- Morning Report Case Presentation: APRIL 1, 2019Документ14 страницMorning Report Case Presentation: APRIL 1, 2019Emily EresumaОценок пока нет
- Food Challenge 03.20.2019Документ17 страницFood Challenge 03.20.2019Emily EresumaОценок пока нет
- Tachycardia How To Keep Your Patient Alive in The Middle of The NightДокумент30 страницTachycardia How To Keep Your Patient Alive in The Middle of The NightEmily Eresuma100% (1)
- Ophtho Pearls 03.13.2019Документ17 страницOphtho Pearls 03.13.2019Emily EresumaОценок пока нет
- Board Prep Metabolics Feb 2019Документ23 страницыBoard Prep Metabolics Feb 2019Emily EresumaОценок пока нет
- Dangers of Vaping 03.15.2019Документ23 страницыDangers of Vaping 03.15.2019Emily EresumaОценок пока нет
- Anemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentДокумент16 страницAnemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentEmily EresumaОценок пока нет
- Bells Palsy or Stroke 02.06.2019Документ19 страницBells Palsy or Stroke 02.06.2019Emily EresumaОценок пока нет
- Case Presentation: Tad MiyaДокумент41 страницаCase Presentation: Tad MiyaEmily EresumaОценок пока нет
- Somatization 01.28.2019Документ28 страницSomatization 01.28.2019Emily EresumaОценок пока нет
- Board Prep Genetics Dec 2018Документ62 страницыBoard Prep Genetics Dec 2018Emily EresumaОценок пока нет
- Board Prep GI Jan 2019Документ32 страницыBoard Prep GI Jan 2019Emily EresumaОценок пока нет
- Chronic Granulomatous Disease 01.23.2019Документ10 страницChronic Granulomatous Disease 01.23.2019Emily EresumaОценок пока нет
- Pertussis 01.14.2019Документ29 страницPertussis 01.14.2019Emily EresumaОценок пока нет
- MysteryCase 10.22.18Документ10 страницMysteryCase 10.22.18Emily EresumaОценок пока нет
- Morning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Документ24 страницыMorning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Emily EresumaОценок пока нет
- Board Prep Emergency Ingestions Dec.2018Документ46 страницBoard Prep Emergency Ingestions Dec.2018Emily EresumaОценок пока нет
- Limping 12.10.2018Документ32 страницыLimping 12.10.2018Emily Eresuma100% (1)
- Morning Report: Melanie Nelson, PGY-2Документ25 страницMorning Report: Melanie Nelson, PGY-2Emily EresumaОценок пока нет
- Ventilators 11.07.2018Документ38 страницVentilators 11.07.2018Emily EresumaОценок пока нет
- Wilderness Medicine 11.20.2018Документ12 страницWilderness Medicine 11.20.2018Emily EresumaОценок пока нет
- Pediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Документ35 страницPediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Emily EresumaОценок пока нет
- Morning Report: Lindsey Gakenheimer-Smith MD PGY3Документ20 страницMorning Report: Lindsey Gakenheimer-Smith MD PGY3Emily EresumaОценок пока нет
- Jaundice 11.28.2018Документ13 страницJaundice 11.28.2018Emily EresumaОценок пока нет
- Halloween Safety: Dominique ChevalierДокумент21 страницаHalloween Safety: Dominique ChevalierEmily EresumaОценок пока нет
- Morning Report: Wade Harrison, MD, MPHДокумент13 страницMorning Report: Wade Harrison, MD, MPHEmily EresumaОценок пока нет
- Foster Care in Utah: Marlayna DespresДокумент11 страницFoster Care in Utah: Marlayna DespresEmily EresumaОценок пока нет
- Grade 12 - General Biology2 - Q4 - Module - 3 - Transport and Circulation. For PrintingДокумент9 страницGrade 12 - General Biology2 - Q4 - Module - 3 - Transport and Circulation. For Printingairamaymalicdem052Оценок пока нет
- Introduction To Emergency Nursing Concepts FinalДокумент128 страницIntroduction To Emergency Nursing Concepts FinalKarren FernandezОценок пока нет
- Basic Life SupportДокумент2 страницыBasic Life SupportDaphne SanchaОценок пока нет
- CSMLS Exam Guide Notes (Referrence Range)Документ4 страницыCSMLS Exam Guide Notes (Referrence Range)software4us.2023Оценок пока нет
- Dyslipidemia: Darmono SSДокумент35 страницDyslipidemia: Darmono SSLa Ode Rinaldi0% (1)
- Should Torsemide Be The Loop Diuretic of Choice in Systolic Heart Failure?Документ37 страницShould Torsemide Be The Loop Diuretic of Choice in Systolic Heart Failure?Mohammad ElghazalyОценок пока нет
- (Physiology) Endocrine MCQ 1Документ21 страница(Physiology) Endocrine MCQ 1Eslam HamadaОценок пока нет
- Final Internalmed2Документ1 788 страницFinal Internalmed2Sharayu DhobleОценок пока нет
- ACUTE RESPIRATORY FAILURE GUIDEДокумент10 страницACUTE RESPIRATORY FAILURE GUIDEGabbii CincoОценок пока нет
- Nursing Care The Mechanical VentilatedДокумент11 страницNursing Care The Mechanical VentilatedIchal faisОценок пока нет
- Kidney in Liver Failure 2024Документ16 страницKidney in Liver Failure 2024Srinivas PingaliОценок пока нет
- Emergency Drugs Drug StudyДокумент15 страницEmergency Drugs Drug StudyCathrine Sandile Tangwara100% (1)
- I RECOVER Post Vaccine ProtocolДокумент58 страницI RECOVER Post Vaccine ProtocolJohnny SmithОценок пока нет
- Breathe In: Write Your Answer On These Activity SheetДокумент4 страницыBreathe In: Write Your Answer On These Activity Sheetirah jane valentinoОценок пока нет
- CHF Case StudyДокумент20 страницCHF Case StudyDelia Soriano AlingayaoОценок пока нет
- Pathophysiology of Hypovolemic ShockДокумент8 страницPathophysiology of Hypovolemic ShockKAYCEEОценок пока нет
- Fatty LiverДокумент4 страницыFatty LiverVincent MwirigiОценок пока нет
- 84 Questions - With Answer - Gloucestershire HospitalsДокумент171 страница84 Questions - With Answer - Gloucestershire HospitalsŞahin EmerОценок пока нет
- Kelainan Hemodinamik, Thromboemboli Dan SyokДокумент82 страницыKelainan Hemodinamik, Thromboemboli Dan SyokwulanОценок пока нет
- Medical Diagnosis PDFДокумент30 страницMedical Diagnosis PDF99nonameОценок пока нет
- Dysrhythmias ChartДокумент6 страницDysrhythmias Chartjkrix100% (1)
- Jurnal Tentang MriДокумент3 страницыJurnal Tentang MriParjoe PanbesОценок пока нет
- Acute Coronary Syndromes - M. Brizzio (Intech, 2012) WW PDFДокумент224 страницыAcute Coronary Syndromes - M. Brizzio (Intech, 2012) WW PDFMihaela NițulescuОценок пока нет
- Hypoplastic Left Heart SyndromeДокумент26 страницHypoplastic Left Heart SyndromeKhaled S. HarbОценок пока нет
- Drug Study AzathioprineДокумент3 страницыDrug Study AzathioprineBunnie AlphaОценок пока нет
- VELARDE-Pharmacology Notes Unit B-Cardiovascular System-2019Документ19 страницVELARDE-Pharmacology Notes Unit B-Cardiovascular System-2019j blОценок пока нет
- Diseases of The ThyroidДокумент65 страницDiseases of The ThyroidEdil M JamaОценок пока нет
- ABG Analysis - NCMB 312 Skills LaboratoryДокумент22 страницыABG Analysis - NCMB 312 Skills LaboratoryANGELICA JOY GATDULAОценок пока нет
- Medicine COC Exam Questions and Answers PDF: Main NavigationДокумент45 страницMedicine COC Exam Questions and Answers PDF: Main NavigationTadesse Muhammed50% (2)
- Full download book Case Files Surgery Pdf pdfДокумент27 страницFull download book Case Files Surgery Pdf pdfsang.green395100% (13)