Академический Документы
Профессиональный Документы
Культура Документы
Osteomyelitis
Загружено:
Suci Pramadiani0 оценок0% нашли этот документ полезным (0 голосов)
426 просмотров32 страницыOsteomyelitis
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документOsteomyelitis
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
426 просмотров32 страницыOsteomyelitis
Загружено:
Suci PramadianiOsteomyelitis
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 32
INFECTION
ACUTE, SUBACUTE AND
CHRONIC OSTEOMYELITIS
APLEYS SYSTEM OF ORTHOPAEDICS AND FRACTURES
8
TH
EDITION
TEAM IV : IK, JS, TS, SF
GENERAL ASPECT OF INFECTION
Micro-organisms enter
the bones and joints :
directly : a break in the
skin (a pinprick, a stab
wound, a laceration, an
open fracture or an
operation)
indirectly via the blood
stream from a distant
site:
the nose or mouth, the
respiratory tract, the
bowel or the genito-
urinary tract.
GENERAL ASPECTS OF INFECTION
Acute pyogenic infections are characterized by:
The formation of pus or abscess (Local effect)
a concentrate of defunct leucocytes, dead and dying
bacteria and tissue debris.
Spread further afield via lymphatics or via the
bloodstream (systemic effect)
causing lymphangitis and lymphadenopathy,
bacteraemia and septicaemia, with systemic reaction :
vatigue, mild pyrexia, severe illness, fever, toxaemia
and shock.
GENERAL ASPECT OF INFECTION
Chronic infection
follow on acute infection or start from beginning
The formation of granulation tissue (a combination of
fibroblastic and vascular proliferation) fibrosis.
Host Response:
Age of patient (very young or too old is more
resistance),
state of malnutrition,
immuno-supresan
other disease like diabetes
Local Factors :
damaged muscle and foreign bodies
bone structure itself consist of collection of rigid
compartment make it more susceptible for vascular
damage and cell death..
GENERAL ASPECT OF INFECTION
The principles of treatment are:
(1) to provide analgesia and general supportive
measures;
(2) to rest the affected part;
(3) effective antibiotic or chemotherapy; and
(4) surgical eradication of infected and necrotic tissue.
For acute infections, the timing of surgery is all-important:
in the early stages, antibiotics should be given a chance
and the clinical condition carefully monitored to detect
signs of improvement or deterioration; if there is pus, it
must be let out and the sooner the better.
Acute osteomyelitis is almost invariably a disease
of children.
This predilection for the metaphysis has been
attributed to the peculiar arrangement of the blood
vessels in that area: the non-anastomosing terminal
branches of the nutrient artery twist back in hairpin
loops before entering the large network of
sinusoidal veins; the relative vascular stasis favours
bacterial colonization.
ACUTE HAEMATOGENOUS
OSTEOMYELITIS
In young infants, in
whom there is still a
free anastomosis
between metaphyseal
and epiphyseal blood
vessels, infection can
just as easily lodge in
the epiphysis
In adults,
haematogenous
infection is more
common in the
vertebrae than in the
long bones.
PATHOLOGY OF
ACUTE OSTEMYELITIS
Inflammation
acute inflammatory reaction,
vascular congestion, exudation of
fluid, infiltration of PMN, increase of
intraosseus pressure
Suppuration
Subperiosteal abscess, end plate
and intervertebral disc infection
Necrosis
avascular necrosis of growth
plate in infant. Bacterial toxins
and leucocytic enzymes also
may play their part in the
advancing tissue destruction.
reactive new bone formation
resolution and healing.
NEW BONE FORMATION
New bone forms from the deep layers of the
stripped periosteum.
This is typical of pyogenic infection and is usually
obvious by the end of the second week. With rime
the new bone thickens to form an involucrum
enclosing the infected tissue and sequestra.
If the infection persists, pus and tiny sequestrated
splcules of bone may continue to discharge through
perforations (cloacae) in the involucrum and track
by sinuses to the skin surfaces; the condition is now
established as a chronic osteomyelitis.
(A) INFECTION IN THE METAPHYSIS MAY SPREAD COWARDS THE SURFACE, TO FORM A
SUBPERIOSTEAL ABSCESS (B). SOME OF THE BONE MAY DIE, AND IS ENCASED IN PERIO STEAL
NEW BONE AS A SEQUESTRUM (C).THE ENCASING INVOLUCRUM IS SOMETIMES PERFORATED BY
SINUSES.
RESOLUTION
Once common, chronic osteomyelitis following on
acute is nowadays seldom seen. If infection is
controlled and intraosseous pressure released at
an early stage, this dire progress can be aborted.
The bone around the zone of infection is at first
osteoporotic (probably due to hypcraemia).
CLINICAL FEATURES
The patient, usually a child,
presents with severe pain,
malaise and a fever; in
neglected cases, toxaemia
may be marked.
X-RAYS NORMAL DURING
FIRST 10 DAYS
Ultrasound may detect a
subperiosteal collection of fluid
in the early stages of
osteomyelitis, but it cannot
distinguish between a
haematoma and pus.
Radioscintigrapby with
99m
Tc-HDP reveals
increased activity in both the perfusion phase and
the bone phase.. It has relatively low specificity and
other inflammatory lesions can show similar
changes.
In doubtful cases, scanning with Ga-citrate or In
labelled leucocytes may be more revealing.
MRI is extremely sensitive, even in the early phase
of bone infection, and can help to differentiate
between soft-tissue infection and osteomyelitis.
The most typical feature is a reduced intensity
signal in T1-weighted images.
INVESTIGATIONS
The most certain way to confirm the clinical
diagnosis is to aspirate pus from the metaphyseal
subperiosteal abscess or the adjacent joint.
The white cell count and C-reactive protein values
are usually high and the haemoglobin concentration
diminished; the ESR also rises but it may take
several days to do so and it often remains elevated
even after the infection subsides.
Blood culture is positive in only about half the cases
of proven infection.
DIFFERENTIAL DIAGNOSIS
Cellulitis
Streptococcal necrotizing myositis
Acute suppurative arthritis
Acute rheumatism
Sickle-cell crisis
Gaucher's disease
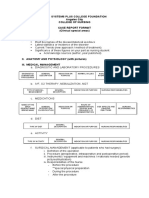
TREATMENT
Supportive treatment for pain and dehydration;
Splintage of the affected part;
Antibiotic therapy 3 6 weeks; and
Surgical drainage
ANTIBIOTIK TREATMENT
Older children and fit adult : Staphylococcus group
Flucloxacillin and fusidic acid i.v 1 2 weeks
Orally antibiotics 3 6 weeks
Children < 4 years ; Haemophilus group and gram
negatife organisms
Cephalosporins (cefuroxime or cefotaxime) i.v or orally
Amoxicillin-clavulanic acid combination (co-amoxiclav, a
-lactamase inhibitor)
SUBACUTE OSTEOMYELITIS
Relative mildness
The organism being less
virulent (Staphylococcus
aureusor ) and the patient
more resistance (or both);
More variable in skeletal
distribution than acute
osteomyelitis
The Distal femur and the
proximal and distal tibia
are favorite sites.
PATHOLOGY
Well defined cavity in cancellous bone glairy
seropurulent fluid (rare pus)
Cavity is lined by granulation tissue of mixture of
acute and chronic inflammatory cells.
The surrounding bone trabeculae are often
thickened
CLINICAL FEATURES
The patient : child or adolescent
Pain near one of the larger joints for several weeks
or even months
A limp or slight swelling, muscle wasting and local
tenderness
Normal temperature to slight higher
White cell count may be normal but ESR is raised
IMAGING
Plain X-Ray
A circumscribed, oval or round cavity 1 2 cm in
diameter on tibia or femoral metaphysis or in epiphysis
or in cuboidal bone (calcaneus)
Cavity surrounded by halo of sclerosis (the classic
Brodies abscess)
Metaphysis lesion little or no periosteal reaction
Diaphysial lesion periosteal new bone formation and
cortical thickening
Radioisotope scan
DIAGNOSIS
Differential diagnosis : Osteoid osteoma with
appearance as malignant bone tumour
Certain examination by Biopsy for bacteriological
culture.
TREATMENT
Conservative
Immobilization and antibiotics (flucloxacillin and
fusidic acid) for 6 weeks than thereafter for 6 12
months
Curretage; indicate for lesion after biopsy and also
for the case with no healing with conservative
treatment. Antibiotics
CHRONIC OSTEOMYELITIS
The usual organisms (and with time there is always
a mixed infection) are Staph. aureus, E. coti, S.
pyogenes, Proteus and Pseudomonas;
In the presence of foreign implants Staph.
cpidermidis, which is normally non-pathogenic, is
the commonest of all.
PATHOLOGY
Bone is destroyed or devitalized in a discrete area
at the focus of infection or more diffusely along the
surface of a foreign implant.
Cavities containing pus and pieces of dead bone
(sequestra) are surrounded by vascular tissue, and
beyond that by areas of sclerosis -the result of
chronic reactive new bone formation. The
sequestra act as substrates
The histological picture is one of chronic
inflammatory cell infiltration around areas of
acellular bone or microscopic sequestra.
CHRONIC OSTEOMYELITIS CHRONIC BONE INFECTION, WITH A PERSISTENT
SEQUESTRUM, MAY BE A SEQUEL TO ACUTE OSTEOMYELITIS (A). MORE
OFTEN IT FOLLOWS AN OPEN FRACTURE OR OPERATION (B). OCCASIONALLY
IT PRESENTS AS A BRODIE'S ABSCESS (C).
CLINICAL FEATURES
The patient presents because pain, pyrexia,
redness and tenderness have recurred (a 'flare'), or
with a discharging sinus.
In long-standing cases the tissues are thickened
and often puckered or folded in where a scar or
sinus is attached to the underlying bone.
There may be a sero-purulent discharge and
excoriation of the surrounding skin.
In post-traumatic osteomyelitis the bone may be
deformed or non-united.
IMAGING
X-ray examination
Bone resorption with thickening and sclerosis of surrounding
bone, loss of trabeculation, area osteoporosis, periosteal
thickening, sequestra, or the bone crudely thickened and
misshapen
Radioisotope scintigraphy
Sensitive but not specific. Using
99m
Tc-HDP for showing
increased activity of perfusion and bone phase and
67
Ga-
Citrate or In-labelled leucocytes for showing hidden foci of
infection
CT and MRI
Show the extent of bone destruction and reactive edema,
hidden abscess and sequestra
INVESTIGATIONS
ESR and blood white cell count
may be increased; are
helpful in assessing the
progress of bone infection but
they are not for diagnostic.
Organisms cultured from
discharging sinuses should be
tested repeatedly for antibiotic
sensitivity; with time, they often
change their characteristics
and become resistant to
treatment.
TREATMENT
Antibiotics ; Fucidic acid,
clindamycin and
cephalosporins
Local treatment : incision and
drainage
Operation
THANK
YOU
Вам также может понравиться
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsРейтинг: 4 из 5 звезд4/5 (2)
- OMCДокумент37 страницOMCyurie_ameliaОценок пока нет
- Ranula Cyst, (Salivary Cyst) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandRanula Cyst, (Salivary Cyst) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Open FractureДокумент9 страницOpen FractureAnnyl LaurelОценок пока нет
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОт EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОценок пока нет
- PYOMYOSITISДокумент12 страницPYOMYOSITISJeg B. Israel Jr.Оценок пока нет
- Glasgow Coma ScaleДокумент3 страницыGlasgow Coma Scaletoto11885Оценок пока нет
- Film Analysis: in Health Care Ethics (NR-NUR127)Документ5 страницFilm Analysis: in Health Care Ethics (NR-NUR127)John MagtibayОценок пока нет
- Pat 2 Medsurg1Документ20 страницPat 2 Medsurg1api-300849832Оценок пока нет
- LCPDДокумент7 страницLCPDakoismeОценок пока нет
- Septic ArthritisДокумент8 страницSeptic ArthritisLorebell100% (2)
- HNP Case Scenario For Case StudyДокумент2 страницыHNP Case Scenario For Case StudyDeinielle Magdangal RomeroОценок пока нет
- Belles Palsy Case Study Group 1Документ36 страницBelles Palsy Case Study Group 1JOEY MEAD ARUGAY100% (1)
- What is Paget's Disease: Causes, Symptoms, Diagnosis and TreatmentДокумент17 страницWhat is Paget's Disease: Causes, Symptoms, Diagnosis and Treatmentraghunandhakumar100% (1)
- Infectious Myositis Causes and SymptomsДокумент7 страницInfectious Myositis Causes and SymptomsJens OcampoОценок пока нет
- Spinal Cord Injury: Andi IhwanДокумент31 страницаSpinal Cord Injury: Andi IhwanAndi Muliana SultaniОценок пока нет
- Paget's Disease of The BoneДокумент9 страницPaget's Disease of The BonePam RomeroОценок пока нет
- MS 1ST & 2ND Term ExamДокумент114 страницMS 1ST & 2ND Term ExamKathleen Dela CruzОценок пока нет
- Chronic Osteomyelitis Nursing Care PlanДокумент18 страницChronic Osteomyelitis Nursing Care PlanMar OrdanzaОценок пока нет
- Colles FractureДокумент89 страницColles Fracturenur syafiqah kamaruzaman100% (1)
- A Case Study Presentation On Subarachnoid Hemorrhage: Presented byДокумент78 страницA Case Study Presentation On Subarachnoid Hemorrhage: Presented byNinaОценок пока нет
- Case Analysis - FractureДокумент7 страницCase Analysis - FractureMichelle TeodoroОценок пока нет
- Case Presentation OsteomylitisДокумент64 страницыCase Presentation OsteomylitisDemi Rose Bolivar100% (1)
- CAP Pneumonia CaseДокумент46 страницCAP Pneumonia CaseMatty FelОценок пока нет
- Multiple Organ Dysfunction SyndromeДокумент2 страницыMultiple Organ Dysfunction SyndromeMaryjoy Gabriellee De La CruzОценок пока нет
- Bell - S PalsyДокумент17 страницBell - S PalsyRickzen Hawkins NikecholantОценок пока нет
- Eric OsteomyelitisДокумент22 страницыEric OsteomyelitisJonathan Delos ReyesОценок пока нет
- Pathophysiology of OsteomyelitisДокумент2 страницыPathophysiology of Osteomyelitissorryandreosayanisalreadytaken100% (1)
- Case Study For Pleural-EffusionДокумент10 страницCase Study For Pleural-EffusionGabbii CincoОценок пока нет
- Intracranial (Inside The Skull) Hemorrhage (Bleeding)Документ41 страницаIntracranial (Inside The Skull) Hemorrhage (Bleeding)MASIIОценок пока нет
- Management and Prevention of Upper GI BleedingДокумент0 страницManagement and Prevention of Upper GI Bleedingbasinang_jangil100% (1)
- Nursing Interventions CHFДокумент3 страницыNursing Interventions CHFbanyenye25100% (1)
- Case Report - Juliet - Closed Fracture Middle of The Left FemurДокумент28 страницCase Report - Juliet - Closed Fracture Middle of The Left FemurGupiesОценок пока нет
- PYOMYOSITISДокумент6 страницPYOMYOSITISChristine CoridoОценок пока нет
- BSN Iii-A Unit Ii Skills Lab ActivityДокумент2 страницыBSN Iii-A Unit Ii Skills Lab ActivityDimple Castañeto CalloОценок пока нет
- Case Presentation Meyke Liechandra C11109130 Fracture ClavicleДокумент24 страницыCase Presentation Meyke Liechandra C11109130 Fracture ClavicleWahyunita IlhamОценок пока нет
- Fracture CaseДокумент15 страницFracture CaseAnna Theresa Cruz100% (2)
- HNPДокумент7 страницHNPLyka Mae Imbat - Pacnis100% (1)
- Intestinal Obstruction: Methas Arunnart MDДокумент42 страницыIntestinal Obstruction: Methas Arunnart MDJhe-sie AngelinaОценок пока нет
- PATHOPHYSIOLOGY OF CORONARY ARTERY DISEASEДокумент2 страницыPATHOPHYSIOLOGY OF CORONARY ARTERY DISEASEPamela DomingoОценок пока нет
- Casestudy OsteomyelitisДокумент52 страницыCasestudy OsteomyelitisJoshua Caacbay PaningbatanОценок пока нет
- ChickenpoxДокумент16 страницChickenpoxJeet ThuraiОценок пока нет
- Palatoplasty Case StudyДокумент26 страницPalatoplasty Case StudySometwo C. Hangal100% (1)
- NCP OsteosarcomaДокумент6 страницNCP OsteosarcomaNiksОценок пока нет
- Case 2 and 3 Q1Документ3 страницыCase 2 and 3 Q1Jeffrey Ramos0% (1)
- Fractured femur nursing careДокумент41 страницаFractured femur nursing careLovella FuentesОценок пока нет
- USC Case 04 - SinusitisДокумент9 страницUSC Case 04 - SinusitisDisti Damelia SebayangОценок пока нет
- Acute TonsillopharyngitisДокумент39 страницAcute TonsillopharyngitisCin AtianzarОценок пока нет
- MS 3 Case Analysis DownloadableДокумент1 страницаMS 3 Case Analysis DownloadableCharissa Magistrado De LeonОценок пока нет
- Congenital hip dysplasia diagnosis in under 40Документ6 страницCongenital hip dysplasia diagnosis in under 40Bek DiazОценок пока нет
- Brief Description of The Disease/statistical IncidenceДокумент2 страницыBrief Description of The Disease/statistical IncidenceLeanne Princess Gamboa100% (1)
- Patient ChartДокумент2 страницыPatient ChartHydieОценок пока нет
- Acute TonsillopharyngitisДокумент17 страницAcute TonsillopharyngitisRachel Haide NaravalОценок пока нет
- Annotated Group 2 Impetigo Concept Mapping 1Документ30 страницAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANOОценок пока нет
- Case Study OsteomyelitisДокумент3 страницыCase Study OsteomyelitisFirsandiPrasastyaFikryGozaliОценок пока нет
- Abdominal Case Study CompiledДокумент392 страницыAbdominal Case Study CompiledIshak IzharОценок пока нет
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodДокумент5 страницTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellОценок пока нет
- BPH Case HistoryДокумент4 страницыBPH Case HistoryChino Dela CruzОценок пока нет
- ASSESSMENTДокумент2 страницыASSESSMENTColeen PequitОценок пока нет
- Managing Anesthesia for Obese PatientsДокумент21 страницаManaging Anesthesia for Obese PatientsAndi Wija Indrawan PangerangОценок пока нет
- 2015 AHA CPR Guidelines Update Focuses on High-Quality Chest CompressionsДокумент4 страницы2015 AHA CPR Guidelines Update Focuses on High-Quality Chest CompressionsAndi Wija Indrawan PangerangОценок пока нет
- OsteomyelitisДокумент32 страницыOsteomyelitisAndi Wija Indrawan PangerangОценок пока нет
- BrochiectasisДокумент34 страницыBrochiectasisAndi Wija Indrawan PangerangОценок пока нет