Академический Документы
Профессиональный Документы
Культура Документы
Ade Ami
Загружено:
ignasachyntiaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Ade Ami
Загружено:
ignasachyntiaАвторское право:
Доступные форматы
HYPERGLYCEMIA
CRISES
Compiled by:
Choirotussanijjah 0910710048
Feros Rachmi S 0910714072
Geneung Patridina 0910714035
Supervisor:
dr. Ali Haedar, SpEM
Emergency Medicine Department
Medical Faculty
Brawijaya University
2014
CONTENTS
INTRODUCTION
CASE REPORT
DISCUSSION
LESSON LEARNT
INTRODUCTION
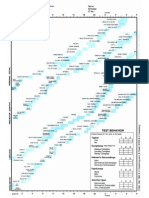
37.4
53.2
+42%
55.2
66.2
+20%
76.7
112.8
+47%
58.7
101.0
+72%
26.5
51.7
+94%
12.1
23.9
+98%
16.0
29.6
+65%
Africa
Middle East and
North Africa
Europe
North America
South and Central America
South-East Asia
Western Pacific
IDF Regions and global
projections for the
number of people with
diabetes (20-79 years),
2010-2030 IDF. Diabetes Atlas 4
th
Edition 2009
Worldwide:
284.6 million people in 2010
438.4 million projected for 2030
54% increase
Diabetes is an increasing healthcare
epidemic throughout the world
Diabetic ketoacidosis (DKA) and hyperosmolar
hyperglycemic state (HHS) are two of the most serious acute
complications of diabetes. These hyperglycemic emergencies
continue to be important causes of morbidity and mortality
among patients with diabetes.
BACKGROUND
Kitabchi et al, 2009
Annual incidence rate DKA 4.6 - 8 episodes per 1,000
(Kitabchi et al, 2006).
Hospitalizations (Kitabchi et al, 2006).
Mortality rate DKA 5%, and HHS still remains high at 11%
(Kitabchi et al, 2009).
Prognosis worsened at the extremes of age and
in the presence of coma and hypotension (Kitabchi
et al, 2009).
BACKGROUND
Similar outcomes of treatment of DKA have been noted in both
community and teaching hospitals, and outcomes have not been
altered by whether the managing physician is a family physician,
general internist, house officer with attending supervision, or
endocrinologist, so long as standard written therapeutic
guidelines are followed (Kitabchi et al, 2009).
BACKGROUND
Standar Kompetensi Dokter Indonesia, 2012
BACKGROUND
PURPOSE
To present practical approach and updated
recommendation to the diagnosis and management
of patients presenting with sign and symptom of DKA
and HHS
Kirabchi et al, 2009
50% were
female,
45% were
nonwhite.
ages of 18-44
years (56%)
45-65 years
(24%)
18% of patients
20 years of age.
2/3 patients type 1 DM
34% type 2 DM
Adult mortality is 1%;
5% reported in elderly and
patients with concomitant
life-threatening illnesses.
AGE SEX
DM
&
MORTALITY
EPIDEMIOLOGY:
DKA
PATHOGENESIS
DIABETES CARE, VOLUME 29, NUMBER 12, DECEMBER 2006
Triad of DKA (hyperglycemia, acidemia, and ketonemia)
and other conditions with which the individual
components are associated.
Kitabchi A E et al. Dia Care 2001;24:131-153
Copyright 2011 American Diabetes Association, Inc.
PRECIPITATING FACTOR:
DKA
Manning et al, 2004
PRECIPITATING FACTOR:
HHS
Kivlehan et al, 2013
Andrew E. Edo . Nigerian Medical Journal | Vol. 53 | Issue 3 |
July-September | 2012
FREQUENCY OF PRESENTING SYMPTOM
IN PATIENTS WITH DKA AND HHS
SYMPTOMS
Manning et al, 2004
DIAGNOSIS CRITERIA
DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009
Tlaleletso. Guidelines update: diabetes mellitus
Emergency Management. 2012
Tlaleletso. Guidelines update: diabetes mellitus
Emergency Management. 2012
Kitabchi AE, Umpierrez GE, Miles JM, et al. Hyperglycemic crises in adult patients with diabetes: a consensus
statement from the American Diabetic Association. Diabetes Care. 2009;32:1335-1343.
Once the Patient Stabilized
Tlaleletso. Guidelines update: diabetes
mellitus Emergency Management. 2012
Hemphill, 2012
deep coma at
the time of
diagnosis
Hypothermia
Oliguria
Overall MR: 2%
POOR,
If:
Older age
presence of
concurrent illnesses
severity of the
metabolic
derangements
Overall MR: 10-20%
DKA HHS
Name : Mr. J
Gender : male
Age : 75 years old
Address : Jl. Bumirejo RT 3/5 Dampit Malang
Occupation : Unemployment
Reg. number : 140606xxxx
Body weight : 55 kg
Patient came to the emergency department on June 6th, 2014
at 2.10 pm.
PATIENTS IDENTITY
Patient came to the emergency department due to
chest pain and burning sensation suddenly lasted for
more than 30 minutes that happened 4 hours ago
before admission while patient working in the field.
Chest pain worse when he breathing, chest pain is not
spread, shortness of breath, cold sweat, cough (-),
fever (-), nausea (-), vomit (-)
History of past illness : patient have experienced
similar pain since 1 years ago. Chest pain when patient
walking away (2 kilometers), relief with rest.
SUMMARY OF CASE
Family history : there is no family relatives with chest
pain or the same complain.
Social history : patient is married and has 2 children.
He works at the field as foreman. He smoked 6 bar
per day and has stopped for 35 years ago.
Upon the arrival at the emergency department, the patient
had chest pain with GCS 456, increasing respiratory rate (26
times per minute), increasing pulse rate (108 times per
minute).
The patient then placed at P1 and got O2 10 lpm via NRBM, IV
lines with IVFD NaCl 0,9% 30 tpm. Patient got Aspirin 320 mg,
Clopidogrel 300 mg via oral, and also ranitidin 25 mg IV.
From physical examination, it was found that the
patient looked unstable, increase breath sounds in
both lung fields.
Then we did further diagnostic evaluation: laboratory
(complete blood count, ureum/creatinine,
SGOT/SGPT, RBS, serum electrolyte, cardiac marker),
radiology (chest x-ray) and ECG.
After performed the primary survey and gave initial treatment
for the patient, we did secondary survey wich include
anamnesis, physical examination and also further diagnostic
evaluation.
From the summary of te case that have already read before,
we suspected that the cause of the typical chest pain due to
miocard infarct.
So we did further diagnostic evaluation.
DISCUSSION
Patient came to the emergency department with chief complain chest pain
and primary survey as mentioned below :
A : patent
B : respiratory rate 26 times per minute with O2 NRBM 10 lpm, increase sound breat
in both lung fields.
C : blood pressure 150/70 mmHg, pulse rate 108 times per minute, weak and
regular, warm acral, CRT <2 seconds
D : GCS 456
E : axillary temperature 37
0
C
Patient then placed at P1
A : -
B : O2 10 lpm via NRBM
C :IV lines with IVFD NaCl 0,9% 30 time per minutes
D : -
INITIAL TREATMENT
What we did is according to the theory that
patient with acute miocard infarct should be managed
initially in the critical care area (P1).
The initial priorities of the patient with acute
miocard infarct include evaluation and management of
A, B, C and patient must be managed in a monitored
area.
MANAGEMENT OF
HYPERGLYCEMIA CRISES
MANAGEMENT OF
HYPERGLYCEMIA CRISES
At first, we can distinguish whether the condition is DKA or HHS.
So we can suspect the patient to certain diagnosis with:
1. Presenting symptom of patient: polydipsi, polyuria,
hyperventilation (Kusmaul breathing), and ketone breath odor.
2. Urgent investigation : CBC, urinalysis (ketones and leucocytes),
blood glucose, renal function test, BGA, electrolytes, Ca, Mg, P.
3. Labs: later show diagnosis criteria meet the criteria DKA or HHS
4. Other investigation, chest x-ray, ECG
5. Monitoring: ECG, Pulse oximetry, VS every 15-30 min, RBS,
potassium and acid base balance every 2 hours.
Immediate management hyperglycemia crises in emergency :
1. IV access
2. Start IV fluids (NaCl 0,9% 1 lt/hours), kalium and insulin
(rapid acting insulin 0,1 unit/kg IV, continuous (IV) infusion
of insulin with syringe pumps), monitor blood pressure, ECG
and give O2.
What we did is fit with the theory:
1. We checked the cardiac marker, the result was normal.
2. We checked electrocardiogram, the result ..
3. We checked the serum electrolyte, for further diagnostic
evaluation.
4. For the management we give oksigen 10 lpm via NRBM, IV
fluids (NaCl 0,9% 30 times per minutes), Aspirin 320 mg,
clopidogrel 300 mg oral, also ranitidin 25 mg IV.
After performed the primary survey and gave initial treatment
for the patient, we did SECONDARY SURVEY which
include anamnesis, physical examination and also further
diagnostic evaluation.
From the summary of the case that patient have experienced
similar pain since 1 years ago. Chest pain when patient walking
away (2 kilometers), relief with rest.
So, we did further diagnostic evaluation such as laboratory,
radiology, and ECG.
Laboratory Findings
Lab Value Lab Value
Leukocyte 11830 4700-11300/uL SGOT
SGPT
4
5
0-32 U/L
0-33 U/L
Hemoglobine 13,00 11,4-15,1 g/dL Troponin I 0,10 < 1,0
Trombocyte 228000 142000-424000 CK-NAC
CK-MB
66
17
39 308
7 - 25
Hematocrit 40% 38-42 RBS 109 <200 g/dL
Natrium
Kalium
Cloride
134
3,80
111
136-145 mmol/L
3,5-5 mmol/L
98-100 mmol/L
Ureum
creatinin
66,1
1,61
16,6-48,52
<1,2
LABS FINDING
Serum osmolarity = 352, 78 mOsm/kg > 320 mOsm/kg
Mix KAD HHS
ECG Result
Sinus rhythm, with heart rate 110 bpm
Frontal axis : Normal
Horizontal axis : slightly CCW rotation
PR interval : 0, 12
QRS complex : 0, 08
QT interval : 0,16
Conclusion : sinus tachycardia with HR 110 bpm
ECG Results
Chest X-Ray
AP position, symetric,
enough KV
Soft tissue & bone normal
Left & right phrenicostalis
angle sharp
Left & right hemidiapragm
dome-shaped
Trachea in the middle
Pulmo : infiltrate in the R/L
pulmo
Aorta: Normal
Cardiac : enlargement to
the left side
Chest X-Ray
Pedis X-Ray
Position AP lateral
aligment : normal
Bone : periosteal reaction (-),
litik (-), fracture (-), blastik (-)
Cartilage : normal
Soft tissue : normal
Conclusion: periostium intact,
perioteal reaction (-)
Pedis X-Ray
Cruris X-Ray
position AP lateral
aligment : normal
Bone : litik (-), fracture (-), blastik (-)
Cartilage : normal
Soft tissue : normal
Cruris X-Ray
AMS dt Hyperglycemia crises
DISPOSITION Internal Medicine Department
WORKING DIAGNOSIS
LESSON LEARNT
Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic
state (HHS) are two of the most serious acute complications of
diabetes.
Both disorders are associated with absolute or relative insulin
deficiency, volume depletion, and acid-base abnormalities.
Management of hyperglycemia crises requires correction of
dehydration, hyperglycemia, and electrolyte imbalances,
identification of comorbid precipitating events, and close
monitoring.
Thank you
Вам также может понравиться
- (KASUS-ENDOKRIN) (2023-10-24) A HYPEROSMOLAR HYPERGLYCEMIC STATE (HHS) PATIENT WITH NEUROLOGICAL MANIFESTATION INVOLUNTARY MOVEMENT (Biyan Maulana)Документ11 страниц(KASUS-ENDOKRIN) (2023-10-24) A HYPEROSMOLAR HYPERGLYCEMIC STATE (HHS) PATIENT WITH NEUROLOGICAL MANIFESTATION INVOLUNTARY MOVEMENT (Biyan Maulana)AОценок пока нет
- Complementary and Alternative Medical Lab Testing Part 8: UrologyОт EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyРейтинг: 3 из 5 звезд3/5 (1)
- Fluid Management in HFДокумент47 страницFluid Management in HFPandu AnggoroОценок пока нет
- NIICU Clinical Database #1Документ10 страницNIICU Clinical Database #1angela0289Оценок пока нет
- Lapsus Cardio v3Документ31 страницаLapsus Cardio v3Nurfitrianti ArfahОценок пока нет
- Clinical case in the emergency room of a patient with an ischemic strokeОт EverandClinical case in the emergency room of a patient with an ischemic strokeОценок пока нет
- Laki-Laki, 21 Tahun Dengan Ketoasidosis DiabetikumДокумент66 страницLaki-Laki, 21 Tahun Dengan Ketoasidosis DiabetikumAnonymous gudRSKОценок пока нет
- COPD Case PresentationДокумент66 страницCOPD Case PresentationAzima Abdelrhaman100% (5)
- Room 307Документ2 страницыRoom 307Macy AbellaОценок пока нет
- Ward Duty Report 12-2-14 (English)Документ25 страницWard Duty Report 12-2-14 (English)gilnifОценок пока нет
- Ajmcr 10 9 10Документ4 страницыAjmcr 10 9 10saОценок пока нет
- SAQand MCQДокумент21 страницаSAQand MCQSanjeev Harry BudhooramОценок пока нет
- Karapitiya OSCE 2017 With AnswersДокумент34 страницыKarapitiya OSCE 2017 With Answersweerawarna fernandoОценок пока нет
- June 2014 Questions Returned From Candidates - Thank You: Long Case 1Документ14 страницJune 2014 Questions Returned From Candidates - Thank You: Long Case 1karan270Оценок пока нет
- Vulnus Ictum: Dr. Jeremia SamosirДокумент64 страницыVulnus Ictum: Dr. Jeremia SamosirjerryОценок пока нет
- Kematian Janin Dalam KandunganДокумент30 страницKematian Janin Dalam KandunganpriscaharahapОценок пока нет
- Diabetic Emergencies Case StudiesДокумент32 страницыDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Nyeri DadaДокумент27 страницNyeri DadaAji Setia UtamaОценок пока нет
- Assessment:: ABG Which Shows A Potassium of 9.0, PH of 7.23 and A BloodДокумент3 страницыAssessment:: ABG Which Shows A Potassium of 9.0, PH of 7.23 and A BloodYamete KudasaiОценок пока нет
- Materials and MethodsДокумент5 страницMaterials and Methodsike ikeОценок пока нет
- Instruction: The Following Continuous Assessment Sheets Contain Two CategoriesДокумент6 страницInstruction: The Following Continuous Assessment Sheets Contain Two CategoriesfekaduОценок пока нет
- Community-Acquired PneumoniaДокумент10 страницCommunity-Acquired PneumoniaHajir AldahhanОценок пока нет
- Hashimotos ThyroiditisДокумент9 страницHashimotos ThyroiditisKristiannlae DanoОценок пока нет
- Flail Chest MP Shah - CcuДокумент29 страницFlail Chest MP Shah - CcuMARTINОценок пока нет
- Treatment of Adrenalectomy Intraoperative Complications in A Patient With Adrenal Tumor Accompanied by Hypercortisol ManifestationДокумент13 страницTreatment of Adrenalectomy Intraoperative Complications in A Patient With Adrenal Tumor Accompanied by Hypercortisol ManifestationRainbow DashieОценок пока нет
- Emergency Red Flags: DR - Magdy Khames AlyДокумент58 страницEmergency Red Flags: DR - Magdy Khames AlyJerry AbleОценок пока нет
- Case ReportДокумент10 страницCase ReportFika Wilda AnggraeniОценок пока нет
- Clinical Nutrition - Compiled CasesДокумент3 страницыClinical Nutrition - Compiled CasesCzara DyОценок пока нет
- Emergency Room: Case Scenario (Group 1)Документ40 страницEmergency Room: Case Scenario (Group 1)Victoria Castillo TamayoОценок пока нет
- Case Studies On Lipids and Cardiac EnzymesДокумент11 страницCase Studies On Lipids and Cardiac EnzymesIdrissa John Sebeh ContehОценок пока нет
- Simulation Acute Coronary Syndrome (Learner)Документ2 страницыSimulation Acute Coronary Syndrome (Learner)Wanda Nowell0% (1)
- Acute Pancreatitis Case PresДокумент29 страницAcute Pancreatitis Case Preskristine keen buanОценок пока нет
- Nursing Care Plan Sample For BeginnersДокумент15 страницNursing Care Plan Sample For BeginnersMoe KhanОценок пока нет
- Suspecting Pulmonary Hypertension in The Dyspneic Patient: Who, When, and HowДокумент92 страницыSuspecting Pulmonary Hypertension in The Dyspneic Patient: Who, When, and HowJonathan LongОценок пока нет
- Diabetic KetoacidosisДокумент26 страницDiabetic Ketoacidosissalma.nasr003Оценок пока нет
- Current Clinical Strategies, Critical Care and Cardiac Medicine (2005) BM OCR 7.0-2Документ79 страницCurrent Clinical Strategies, Critical Care and Cardiac Medicine (2005) BM OCR 7.0-2api-3709022100% (2)
- n451 Baradi - Case StudyДокумент18 страницn451 Baradi - Case Studyapi-272878167Оценок пока нет
- Duty Report 01 MARCH, 2015: GP On Duty: Dr. Ruben Coass On Duty: Aris ZikrilДокумент24 страницыDuty Report 01 MARCH, 2015: GP On Duty: Dr. Ruben Coass On Duty: Aris ZikrilKarina Pratiwi SoetomoОценок пока нет
- Cardiogenic Shock 11Документ2 страницыCardiogenic Shock 11Kemal TaufikОценок пока нет
- Protocol pES PDFДокумент4 страницыProtocol pES PDFPaola Gracielle CabreraОценок пока нет
- Tuberculous Lymphadenitis Coexists With Non-Hodgkin LymphomaДокумент5 страницTuberculous Lymphadenitis Coexists With Non-Hodgkin LymphomaThania WazintaОценок пока нет
- CVD Ekdum FinalДокумент59 страницCVD Ekdum FinalGanesh RasalОценок пока нет
- Case Study 2Документ27 страницCase Study 2Hal00mОценок пока нет
- DF Case ReportДокумент26 страницDF Case ReportMuhamad IrsyadОценок пока нет
- Congestive Heart Failure Case PressДокумент33 страницыCongestive Heart Failure Case PressNikki M. ArapolОценок пока нет
- Ojsadmin, 1034Документ5 страницOjsadmin, 1034杨嘉宜Оценок пока нет
- Week 5 Respiratory EmergencyДокумент61 страницаWeek 5 Respiratory EmergencyArmand Bong SantiagoОценок пока нет
- DR Fiona Dignan - Acute Haematological EmergenciesДокумент37 страницDR Fiona Dignan - Acute Haematological EmergenciesAndreKrisleeОценок пока нет
- Duty Report MARCH 22ND 2017: Anemia On CKDДокумент18 страницDuty Report MARCH 22ND 2017: Anemia On CKDsarahОценок пока нет
- Case Presentation ETD (COPD)Документ45 страницCase Presentation ETD (COPD)Dzachary13Оценок пока нет
- Hashim Major LogДокумент26 страницHashim Major LogHashim AlsammawiОценок пока нет
- Jurnal KDMДокумент8 страницJurnal KDMFhietry Idrus ScaftweeОценок пока нет
- Roll No - BR (On) - 2, Kaung Htike San, PresentationДокумент22 страницыRoll No - BR (On) - 2, Kaung Htike San, PresentationHnin Thiri SoeОценок пока нет
- Research Article: Prevalence and Risk Factors of Prolonged QTC Interval Among Chinese Patients With Type 2 DiabetesДокумент6 страницResearch Article: Prevalence and Risk Factors of Prolonged QTC Interval Among Chinese Patients With Type 2 DiabetesHesbon MomanyiОценок пока нет
- Cardiovascular Case: Presented By: Dr. SyahrianiДокумент30 страницCardiovascular Case: Presented By: Dr. SyahrianiAkbar IskandarОценок пока нет
- Suggested Discharge SummaryДокумент2 страницыSuggested Discharge SummaryJohnОценок пока нет
- Explain The Mechanism of Action of Group of DrugsДокумент2 страницыExplain The Mechanism of Action of Group of DrugsignasachyntiaОценок пока нет
- Ucm 319628Документ46 страницUcm 319628ignasachyntiaОценок пока нет
- Needle Thoracocentesis AnastesiДокумент5 страницNeedle Thoracocentesis AnastesiignasachyntiaОценок пока нет
- 120-Review of Internal Hernias. Radiographic and Clinical FindingsДокумент20 страниц120-Review of Internal Hernias. Radiographic and Clinical FindingsbobbylaksanaОценок пока нет
- Dr. Ery Olivianto, Sp.A: Division of Gastrohepatology, Child Health DepartmentДокумент15 страницDr. Ery Olivianto, Sp.A: Division of Gastrohepatology, Child Health DepartmentignasachyntiaОценок пока нет
- Dka and HonkДокумент30 страницDka and HonkignasachyntiaОценок пока нет
- Ich Magistris, 2013Документ8 страницIch Magistris, 2013ignasachyntiaОценок пока нет
- Formato Denver IIДокумент1 страницаFormato Denver IIMelly AnidaОценок пока нет
- PPS - Revised Dengue Guidelines Fluid Management Oct 2012Документ22 страницыPPS - Revised Dengue Guidelines Fluid Management Oct 2012lovelots1234100% (3)
- Bells PalsyДокумент15 страницBells PalsyDavid SugiartoОценок пока нет
- Intro To CHDДокумент91 страницаIntro To CHDignasachyntiaОценок пока нет
- Study Design Epidemology-HoliДокумент49 страницStudy Design Epidemology-HoliignasachyntiaОценок пока нет
- PC's & Laptop Accessories PDFДокумент4 страницыPC's & Laptop Accessories PDFsundar chapagainОценок пока нет
- 5070 s17 QP 22 PDFДокумент20 страниц5070 s17 QP 22 PDFMustafa WaqarОценок пока нет
- Harley Davidson U S Reportedly Uses Risk Sharing Agreements With Its Foreign SubsidiariesДокумент1 страницаHarley Davidson U S Reportedly Uses Risk Sharing Agreements With Its Foreign Subsidiariestrilocksp SinghОценок пока нет
- Material Safety Data Sheet: - AdsealДокумент12 страницMaterial Safety Data Sheet: - Adsealwuhan lalalaОценок пока нет
- GT I9100g Service SchematicsДокумент8 страницGT I9100g Service SchematicsMassolo RoyОценок пока нет
- Forensic My Cology Mcgraw HillДокумент8 страницForensic My Cology Mcgraw HillJayanti RaufОценок пока нет
- Daily Plankton Agrabinta CianjurДокумент141 страницаDaily Plankton Agrabinta CianjurPutra Cahya GemilangОценок пока нет
- Corregidor Title DefenseДокумент16 страницCorregidor Title DefenseJaydee ColadillaОценок пока нет
- Regulated and Non Regulated BodiesДокумент28 страницRegulated and Non Regulated Bodiesnivea rajОценок пока нет
- Sco 8th Class Paper - B Jee-Main Wtm-15 Key&Solutions Exam DT 17-12-2022Документ4 страницыSco 8th Class Paper - B Jee-Main Wtm-15 Key&Solutions Exam DT 17-12-2022Udaya PrathimaОценок пока нет
- Haymne Uka@yahoo - Co.ukДокумент1 страницаHaymne Uka@yahoo - Co.ukhaymne ukaОценок пока нет
- Propp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeДокумент10 страницPropp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeRohith KumarОценок пока нет
- PDF Synopsis PDFДокумент9 страницPDF Synopsis PDFAllan D GrtОценок пока нет
- De On Tap So 4-6Документ8 страницDe On Tap So 4-6Quy DoОценок пока нет
- Estill Voice Training and Voice Quality Control in Contemporary Commercial Singing: An Exploratory StudyДокумент8 страницEstill Voice Training and Voice Quality Control in Contemporary Commercial Singing: An Exploratory StudyVisal SasidharanОценок пока нет
- Capital Structure and Leverage: Multiple Choice: ConceptualДокумент53 страницыCapital Structure and Leverage: Multiple Choice: ConceptualArya StarkОценок пока нет
- Catalogue Laboratory Products - Heraeus KulzerДокумент288 страницCatalogue Laboratory Products - Heraeus KulzerDentaDentОценок пока нет
- British Birds 10 LondДокумент376 страницBritish Birds 10 Londcassy98Оценок пока нет
- Amine Processing Unit DEAДокумент9 страницAmine Processing Unit DEAFlorin Daniel AnghelОценок пока нет
- 30 de Thi Hoc Ky 2 Mon Tieng Anh Lop 9 Co Dap An 2023Документ64 страницы30 de Thi Hoc Ky 2 Mon Tieng Anh Lop 9 Co Dap An 2023Trần MaiОценок пока нет
- Enzyme Immobilization - Advances in Industry, Agriculture, Medicine, and The Environment-Springer International Publishing (2016)Документ141 страницаEnzyme Immobilization - Advances in Industry, Agriculture, Medicine, and The Environment-Springer International Publishing (2016)Komagatae XylinusОценок пока нет
- Story 1Документ3 страницыStory 1api-296631749Оценок пока нет
- 762id - Development of Cluster-7 Marginal Field Paper To PetrotechДокумент2 страницы762id - Development of Cluster-7 Marginal Field Paper To PetrotechSATRIOОценок пока нет
- O Repensar Da Fonoaudiologia Na Epistemologia CienДокумент5 страницO Repensar Da Fonoaudiologia Na Epistemologia CienClaudilla L.Оценок пока нет
- Activity Sheet Housekeeping Week - 8 - Grades 9-10Документ5 страницActivity Sheet Housekeeping Week - 8 - Grades 9-10Anne AlejandrinoОценок пока нет
- Chapter 15: Religion in The Modern World: World Religions: A Voyage of DiscoveryДокумент11 страницChapter 15: Religion in The Modern World: World Religions: A Voyage of DiscoverysaintmaryspressОценок пока нет
- HUAWEI PowerCube 500Документ41 страницаHUAWEI PowerCube 500soumen95Оценок пока нет
- License Fee PaidДокумент1 страницаLicense Fee Paidmy nОценок пока нет
- Snowflake ScarfДокумент2 страницыSnowflake ScarfAmalia BratuОценок пока нет
- Business Plan - A TeahouseДокумент6 страницBusiness Plan - A TeahouseJoe DОценок пока нет