Академический Документы
Профессиональный Документы
Культура Документы
633666227389668750
Загружено:
TotaAl-mutairi0 оценок0% нашли этот документ полезным (0 голосов)
15 просмотров33 страницыAbnormal implantation of placenta in the lower uterine segment, partially or completely covering the internal cervical os. Age (35-40) Gender Race (nonwhite ethnicity) Heredofamilial Predisposing Factors: Previous abortion Previous placental previa Multiple births Endometritis VBAC (vaginal birth after cesarean delivery) Lifestyle (smoking, etc.)
Исходное описание:
Оригинальное название
131285_633666227389668750
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документAbnormal implantation of placenta in the lower uterine segment, partially or completely covering the internal cervical os. Age (35-40) Gender Race (nonwhite ethnicity) Heredofamilial Predisposing Factors: Previous abortion Previous placental previa Multiple births Endometritis VBAC (vaginal birth after cesarean delivery) Lifestyle (smoking, etc.)
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
15 просмотров33 страницы633666227389668750
Загружено:
TotaAl-mutairiAbnormal implantation of placenta in the lower uterine segment, partially or completely covering the internal cervical os. Age (35-40) Gender Race (nonwhite ethnicity) Heredofamilial Predisposing Factors: Previous abortion Previous placental previa Multiple births Endometritis VBAC (vaginal birth after cesarean delivery) Lifestyle (smoking, etc.)
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 33
The abnormal implantation of placenta
in the lower uterine segment, partially or
completely covering the internal cervical os.
Top Placenta Previa
(Complete)
The placenta
completely covers the
cervix
Partial
Placenta Previa
The placenta is
partially over the cervix
Marginal
Placenta Previa
The placenta is near
the edge of the cervix
Predisposing Factors:
Age (35-40)
Gender
Race (nonwhite ethnicity)
Heredofamilial
Predisposing Factors:
Previous abortion
Previous placenta previa
Multiple births
Endometritis
VBAC (vaginal birth after
cesarean delivery)
Lifestyle (smoking, etc.)
Previous abortion
Previous placenta previa
Multiple births
Endometritis
VBAC (vaginal birth after cesarean delivery)
Lifestyle (smoking, etc.)
Damage to
endometrium
Defective decidual vascularization exists (2 to inflammatory or atrophic
changes)
Incomplete development of the fibrinoid layer
IMPLANTATION
Adherence of embryo (embryonic plate) in the lower uterus
Attachment of placenta to
lower uterine segment
Accreta
Covers cervical opening as
placenta Inc. in size
Total P. Previa
Partial P. Previa
Marginal P. Previa
ONSET OF LABOR
Thinning of the area (implantation site)
Disruption of placental attachment
Uterus unable to contract
Unable to stop flow of blood from the open vessels
Bleeding at the implantation site
Release of Thrombin from the bleeding sites
Promote contraction
Promote contraction
FOLLOWS A VICIOUS CYCLE:
Bleeding Contractions Placental
separation - Bleeding
Altered Tissue Perfusion related to excessive
bleeding causing fetal compromise
Frequently monitor mother and fetus
Administer IV fluids as prescribed
Position on side to promote placental perfusion
Administer oxygen as facemask as indicated (8-10 per minute)
Fluid volume deficit related to excessive
bleeding
Establish and maintain a large-bore IV line, as prescribed and draw blood for
type and screen for blood replacement
Position in a sitting position to allow weight of fetus to compress the placenta
and decrease bleeding
Maintain strict bed rest during any bleeding episode
Prepare woman for a cesarean delivery
Administer blood or blood products protocol per institutional policy
Risk for infection related to excessive
blood loss
Use aseptic technique when providing care
Evaluate temperature q4h unless elevated; then evaluate q2h
Evaluate WBC and differential count
Teach perineal care and hand washing techniques
Assess odor of all vaginal bleeding or lochia
Anxiety related to excessive bleeding
Explain all treatments and procedure
Encourage verbalization of feelings by patient and family
Provide information on a CS delivery
Discuss the effects of long-term hospitalization or prolonged bed rest
Fear related to outcome of pregnancy after
episodes of bleeding
Explain all treatments and procedure
Encourage verbalization of feelings by patient and family
Provide information on a CS delivery
Determine the amount and type of bleeding
Inquire as to presence or absence of pain in association with the bleeding
Record maternal and fetal VS
Palpate for the presence of uterine contractions
Evaluate laboratory data on Hct and Hgb
Assess fetal status with continuous fetal monitoring
Never perform a vaginal examination when pt is bleeding
Placenta accreta
Immediate hemorrhage, with possible shock and maternal death
Increased risk for anemia secondary to increased blood loss and infection
secondary to invasive procedures to resolve bleeding
Intrauterine growth restriction (IUGR)
Congenital anomalies
Fetal mortality resulting from hypoxia in utero and prematurity
Nursing intervention
- Monitor amount of blood loss, pain level, and uterine contractility.
- Assess maternal vital signs
- Monitor the lab results.
- Emotional support
- Bed rest
- Kick count
- Prevent vaginal examination
- FHS monitoring
- Administer Rh immunoglobulin if the client Rh negative at 28
weeks
- Prepare for CS
- Monitor tocolytic agents
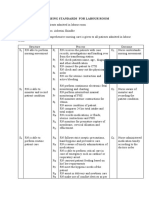
CHARACTERISTIC PLACENTA PREVIA ABRUPTIO PLACENTA
ONSET
Third trimester commonly @32-
36wks
Third trimester
BLEEDING
Mostly external, small to
profuse in amount, bright red
May be concealed, external
dark hemorrhage or bloody
amniotic fluid
PAIN AND UTERINE TENDERNESS
Usually absent; uterus soft
Usually present; irritable
uterus, progresses to board
like consistency
FETAL HEART TONE
Usually normal Maybe irregular or absent
PRESENTING PART
Usually not engaged May be engaged
SHOCK
Usually not present unless
bleeding is excessive
Moderate to severe depending
on extent of concealed and
external hemorrhage
DELIVERY
Delivery may be delayed
depending on size of fetus and
amount of bleeding
Immediate delivery, usually by
CS section
Is premature separation of the
implanted placenta before the birth of
the fetus
Hemorrhage can be either occult or apparent. With an occult hemorrhage, the
placenta usually separates centrally, and a large amount of blood is accumulated
under the placenta. When the apparent hemorrhage is present, the separation is
along the placental margin, and blood flows under the membranes and through
the cervix.
If the placenta begins to detach during pregnancy, there is bleeding from these vessels. The larger the area that
detaches, the greater the amount of bleeding
Predisposing Factors:
Age (> 35y.o)
Gender
Heredofamilial
Predisposing Factors:
Previous abruptio placenta
PIH
Abdominal trauma
Smoking
Cocaine use
Chorioamnionitis
Damage in small arterial
vessels in the basal layer of
decidua
Bleeding
Splits decidua, leaving a thin layer
attached to the placenta
Destruction of the placental tissues
OCCULT APPARENT
Hematoma formation
Compression of the basal
layer
Obliteration of the
intervillous space
Destruction of the placental tissues
Impaired exchange of
respiratory gases and
nutrients
Visible Bleeding Concealed Bleeding
Blood reaches the edge of
the placenta
Blood passes through the
membranes of amniotic sac
Blood passes through the
membranes of amniotic sac
Port wine discoloration
of discharges
( PATHOGNOMONIC SIGN)
NOTE:
Small amount of blood goes out to the vagina (not an indication of the severity of condition)
Ineffective tissue perfusion (placental) related to excessive
bleeding, hypotension, and decreased cardiac output, causing
fetal compromise
Evaluate amount of bleeding by weighing all pads. Monitor CBC results and VS
Position in the left lateral position, with the head elevated to enhance placental
perfusion
Administer oxygen through a snug face mask at 8-12L per minute
Evaluate fetal status with continuous external fetal monitoring
Prepare for possible CS delivery if maternal or fetal compromise is evident
Instruct patient on the cause of pain to decrease anxiety
Instruct and encourage the use of relaxation technique to augment analgesics
Administer pain medications as needed and as prescribed
Acute Pain related to increase uterine
activity
Establish and maintain a large-bore IV line, as prescribed and draw blood for
type and screen for blood replacement
Evaluate coagulation studies
Monitor maternal VS and contractions
Monitor vaginal bleeding and evaluate fundal height to detect an increase in
bleeding
Fluid volume deficit related to excessive
bleeding
Use aseptic technique when providing care
Evaluate temperature q4h unless elevated; then evaluate q2h
Evaluate WBC and differential count
Teach perineal care and hand washing techniques
Assess odor of all vaginal bleeding or lochia
Risk for infection related to excessive blood
loss
Inform the woman and her family about the status of herself and the fetus
Explain all procedures in advance when possible or as they are performed
Answer questions in a calm manner, using simple terms
Encourage the presence of a support person
Fear related excessive bleeding procedures
and unknown outcome
Determine the amount and type of bleeding and the presence or absence of
pain.
Monitor maternal and fetal vital signs, especially maternal BP, pulse, FHR, and
FHR variability.
Palpate the abdomen
oNote the presence of contractions and relaxations between contractions
(if contractions are present)
oIf contractions are not present assess the abdomen for firmness
Measure and record fundal height to evaluate the presence of concealed
bleeding.
Prepare for possible delivery.
Maternal shock
Anaphylactoid syndrome of pregnancy
Postpartum hemorrhage
Acute respiratory distress syndrome
Sheehans syndrome
Renal tubular necrosis
Rapid labor and delivery
Maternal and fetal death
Prematurity
Nursing intervention
- Hourly I&O.
- V/S
- Observe bleeding( dark or bright red)
- IV line
- Avoid VE
- Pain medication
- Evaluate fundal height
- Observe signs of DIC
- Observe fetal distress
- Assess oxygen sat. by pulse oxymetry
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Placental Abruption Causes, Symptoms, DiagnosisДокумент15 страницPlacental Abruption Causes, Symptoms, DiagnosisTotaAl-mutairiОценок пока нет
- Abortion 2Документ47 страницAbortion 2Irfandy Chairi Sulaiman LubisОценок пока нет
- 3-Critical Thinking in NursingДокумент17 страниц3-Critical Thinking in NursingTotaAl-mutairiОценок пока нет
- 2-Health Care Delivery SystemsrabiaДокумент21 страница2-Health Care Delivery SystemsrabiaTotaAl-mutairiОценок пока нет
- Disorders of The Immune SystemДокумент39 страницDisorders of The Immune SystemTotaAl-mutairiОценок пока нет
- Dietary For DiabeticДокумент24 страницыDietary For DiabeticTotaAl-mutairiОценок пока нет
- 1-The Growth of A ProffessionДокумент15 страниц1-The Growth of A ProffessionTotaAl-mutairiОценок пока нет
- 3-Critical Thinking in NursingДокумент17 страниц3-Critical Thinking in NursingTotaAl-mutairiОценок пока нет
- Theories & Models of NursingДокумент15 страницTheories & Models of NursingTotaAl-mutairiОценок пока нет
- Dietary For DiabeticДокумент24 страницыDietary For DiabeticTotaAl-mutairiОценок пока нет
- 1-Develomental Theories Part OneДокумент33 страницы1-Develomental Theories Part OneTotaAl-mutairiОценок пока нет
- 2 - Lecture Developmental Part TwoДокумент25 страниц2 - Lecture Developmental Part TwoTotaAl-mutairiОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Guía OxigenoterapiaДокумент39 страницGuía OxigenoterapiaSMIBA MedicinaОценок пока нет
- College DetailsДокумент48 страницCollege Detailsvivek chauhanОценок пока нет
- Malnutrition in Critical Illness and Beyond A Narrative Review PDFДокумент9 страницMalnutrition in Critical Illness and Beyond A Narrative Review PDFEsteban DavidОценок пока нет
- Apollo Hospitals: Porters Generic FrameworkДокумент6 страницApollo Hospitals: Porters Generic FrameworkVaibhav AroraОценок пока нет
- BiopharmaceuticsДокумент52 страницыBiopharmaceuticsDharma ShantiniОценок пока нет
- Surgical Site InfectionДокумент7 страницSurgical Site InfectionCaxton ThumbiОценок пока нет
- History, Diagnosis and Treatment Planning in Removable Partial DenturesДокумент96 страницHistory, Diagnosis and Treatment Planning in Removable Partial DenturesPriya BagalОценок пока нет
- Cytotoxins Pose Risks for Healthcare WorkersДокумент2 страницыCytotoxins Pose Risks for Healthcare WorkersMaria Nesen NuezОценок пока нет
- Community Pharmacy Management CH 3 Prescription and Prescription Handlind NotesДокумент9 страницCommunity Pharmacy Management CH 3 Prescription and Prescription Handlind Notesi.bhoomi12Оценок пока нет
- Prasugrel and RosuvastatinДокумент7 страницPrasugrel and RosuvastatinMohammad Shahbaz AlamОценок пока нет
- NCM 103 Aliasas AtelectasisДокумент3 страницыNCM 103 Aliasas AtelectasisDARREN EDMARKОценок пока нет
- Led Astray: Clinical Problem-SolvingДокумент6 страницLed Astray: Clinical Problem-SolvingmeganОценок пока нет
- A History of Prostate Cancer Cancer, Men and Medicine First Edition PDFДокумент248 страницA History of Prostate Cancer Cancer, Men and Medicine First Edition PDFMarcela Osorio DugandОценок пока нет
- SBI Insurance Violating PMJAY NormsДокумент4 страницыSBI Insurance Violating PMJAY NormsAntar SinghОценок пока нет
- Dolan 1996Документ7 страницDolan 1996Ainia TaufiqaОценок пока нет
- Atrial Fibrillation - Diagnosis and Treatment - AAFP PDFДокумент8 страницAtrial Fibrillation - Diagnosis and Treatment - AAFP PDFNaufal AmanullahОценок пока нет
- Rheumatological History Taking OSCE GuideДокумент11 страницRheumatological History Taking OSCE GuideChen BrionesОценок пока нет
- Cervical Cancer: Causes, Symptoms, Prevention & TreatmentДокумент21 страницаCervical Cancer: Causes, Symptoms, Prevention & TreatmentKen Edward ZataОценок пока нет
- Infusion Pumps, Large-Volume - 040719081048Документ59 страницInfusion Pumps, Large-Volume - 040719081048Freddy Cruz BeltranОценок пока нет
- ATT Induced Hepatotoxicity: Dr. K. K. SharmaДокумент36 страницATT Induced Hepatotoxicity: Dr. K. K. SharmaSucharita Ray100% (1)
- Practices of Self-Medication Among Tribal Population North Maharashtra (Khandesh)Документ5 страницPractices of Self-Medication Among Tribal Population North Maharashtra (Khandesh)Latasha WilderОценок пока нет
- Designed To Enhance From The Inside Out: Apd TherapyДокумент7 страницDesigned To Enhance From The Inside Out: Apd TherapyNumael Alfonso Serrato AlvaradoОценок пока нет
- Approach To Neurologic Infections.4 PDFДокумент18 страницApproach To Neurologic Infections.4 PDFosmarfalboreshotmail.comОценок пока нет
- Medical Design BriefsДокумент62 страницыMedical Design Briefsneto512Оценок пока нет
- Nursing Standards for Labour RoomДокумент3 страницыNursing Standards for Labour RoomRenita ChrisОценок пока нет
- Unknown PDFДокумент3 страницыUnknown PDFSandy CastellanoОценок пока нет
- Machine Learning Medical Imaging Market to Top $2 BillionДокумент13 страницMachine Learning Medical Imaging Market to Top $2 BillionFrado SibaraniОценок пока нет
- Prescribing Information: 1. Name of The Medicinal ProductДокумент5 страницPrescribing Information: 1. Name of The Medicinal Productddandan_20% (1)
- National Mental Health ProgrammeДокумент9 страницNational Mental Health ProgrammeSharika sasi0% (1)
- Implementasi PMKP di Rumah SakitДокумент29 страницImplementasi PMKP di Rumah SakitikaoktaviasaktiОценок пока нет