Академический Документы
Профессиональный Документы
Культура Документы
Fever
Загружено:
Tashii TsheringАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Fever
Загружено:
Tashii TsheringАвторское право:
Доступные форматы
PRE SCHOOL CHILD
PRESENTING WITH FEVER AND
COUGH
BY
SUCHINTHA TILAKARATNE
HARSHA WIMALARATHNA
History
Miss Radha Gimhani
5 years old (Date of Birth: 28
nd
April
1999)
No 73, Sri Nanda Mawatha, Madinnagoda,
Rajagiriya.
Date of admission: 10
th
November 2004
8:30 am
PLAN
History
Examination
Summary
Problems Identified
Management & Discussion
History
Presenting complaint
Fever for 9 days
Cough for 6 days
Difficulty of breathing for one day
History of presenting complaint
Apparently well on 30 /10/2004
Day 1 ( 31/10/2004)
Fever
Not documented
No chills and rigors
Intermittent fever responding to paracetamol
Measures taken
Tepid sponging
Paracetamol tablet (250mg) 6 hourly
Fever temporarily subsided
History
Day 2 ( 01/11/2004)
intermittent fever responding to paracetamol
History
Day 3 ( 02/11/2004)
Intermittent fever responding to paracetamol
Cough
Dry/non productive
Worst at night
sleep not disturbed
Treatment LRH OPD.
Amoxycillin 1 capsule (250mg) tds 3 days
Paracetamol tablet (250mg) qds 3 days
Vitamin C tablet
British Thoracic Society
Indicators for admission to hospital in older children:
oxygen saturation <92%, cyanosis;
respiratory rate >50 breaths/min;
difficulty in breathing;
grunting;
signs of dehydration;
family not able to provide appropriate observation or supervision.
History
Day 4,5
Fever and cough continued despite
treatment
Day 6 (05/11/2004)
Treatment LRH OPD - full blood count done
Sent home with medication
Amoxycillin 1 capsule (250mg) tds 3 days
Paracetamol tablet (250mg) qds 3 days
Vitamin c tablet
Full blood count
WBC 5400 /L (6000- 15000)
DC Neutrophils 73% (3942/ L)
Lymphocytes 25% (1350 / L)
Monocytes 2% (108 / L)
PCV 32%
Platelet count 152000/ L)
History
Day 7 & 8
Fever and cough continued despite
treatment
On day 8 evening she developed difficulty
of breathing
Day 9 (10/11/2004 8.30 am)
Increase in cough and fever
Admitted to Ward 1
On admission fever 102 F
Difficulty of breathing present
No sputum
No chest pain
History
History
No history of sore throat
No chest pain
No wheezing
No urinary symptoms
Bowel habits normal
No vomiting
Loss of appetite present through out the
illness
History
No skin rashes or bleeding manifestations
No recent contact history of fever
No visits to malarial areas
No neck pain or fits
No headache
No earache
History
D9 (at ward)
Paracetamol given
Tepid sponging done
Blood taken for investigations
X ray taken
Drugs given by needle
Cough,fever persistant
History
D10
Chest exercises started
D11
Nebulization started
D13
X ray taken
History
D14
Blood taken for a test
Chest exercises stopped
Scan done
D16
Blood sent for an out side investigation
History
D18(morning)
Scan done
D18(evening)
Child active
Improved appetite
Cough and fever present
Well between fever episodes
Past medical history
No significant past medical history
No history of recurrent chest infections
or wheezing
Birth history
unplanned pregnancy, Uncomplicated
Normal vaginal delivery
Birth weight 2. 75 kg
No post natal complications
Exclusive breast feeding up to 4 months
Immunization
Development age appropriate
Immunization up to date
All EPI vaccines given at appropriate ages
JE 3 doses given
Hib not given
CHDR
CHDR
Feeding history
On adult diet
Early morning full cream milk (2 tea spoons) with 2 biscuits
Mid morning Samaposha, noodles, rice 1-2 cups
Lunch rice, fish,vegetables
Evening tea with 2 biscuits
Night rice with fish and vegetables
Before sleep - full cream milk (2 tea spoons) with Sustegen
Family history
Non consanguinous marrriage
No family history of asthma, chronic
cough
37yr
38yr
6yr 6yr
5yr
Social history
Father
Electrician
39 years old
Education A/L
Working in Dubai for past 3 years
Income Rs. 25000 per month
Occasional alcoholic
Smokes 2 3 cigarettes per day
Mother
Housewife
37 years old
Education O/L
Contraceptives OCP
Social history
Elder brothers
6 years old
Schooling grade one
Grand parents
Healthy
Capable of looking after children
Gimhani
Attending nursery school km from home
Social history
Housing
Fully completed single story house
Toilet water sealed squatting type, attach to the
house
Pipe borne water
Water boiled before drinking
Bed room
Good ventilation, neatly maintained
Social history
Pre school
Around 20 children in the class
Well ventilated
No recent outbreak of fever or cough in the class
Pre school
Examination (On admission)
General examination
Weight 15.5kg ( Between 3
rd
10
th
centiles)
Height 112cm ( Between 50
th
75
th
centiles)
Ill looking
Dyspneic at rest
Hydration adequate
Temperature 102 F
No pallor
Good oral hygiene,throat not inflamed
No dental caries
Bilateral cervical lymphadenopathy present
Discrete,mobile,non tender lymphnodes
no skin rashes
BCG scar present
Examination
Respiratory system
RR 38/min (normal 30/min)
Nasal flaring present
No chest wall deformities
Intercostal recession present
Trachea central
Apex beat not shifted
Dullness on right lower zone
Bronchial breathing on right lower zone
Air entry decreased on right lower zone
No pleural rub
Examination
Cardiovascular system
Pulse rate 92 beats /min (80 -120)
Regular good volume
Blood Pressure 90/60 mmHg
Dual rhythm. No murmurs
Examination
Abdomen
Not distended
Soft
Non tender
No hepatomegaly
Examination
Nervous system
No neck stiffness
Kernigs sign negative
Summary
5yrs old Gimhani presenting with
fever for 9 days, dry cough for 6 days
and difficulty of breathing for one day
On examination fever 102 F, mild
dyspnea and cervical lymphadenopathy
Dullness on right lower zone with
bronchial breathing and decreased air
entry
Problems identified
Lower respiratory tract infection
Loss of preschool activities
Anxiety of the mother
Absence of father
Lack of proper spacing between
children
Diagnosis Pneumonia
Cough and fever
Difficulty of breathing
Increased respiratory
rate
Nasal flaring
Intercostal recessions
Dull to percussion
Decreased air entry
Bronchial breathing
MANAGEMENT AND DISCUSSUON
day 9 (D
1
)
ACUTE MANAGEMENT
TEPID SPONGING
Paracetamol 250mg 6 hourly
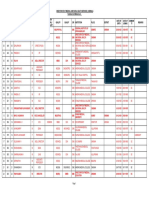
DAY1 DAY2 DAY3 DAY4 DAY5 DAY7 DAY8
98
99
100
101
102
103
104
0 5 10 15 20 25 30 35
FEVER PATTERN
D
1
D
2
D
3
D
4
D
5
D
6
D
7
D
8
D
9
IV penicillin
IV Gentamicin
IV Cefotaxime
IV Clarithromycin
MANAGEMENT AND DISCUSSION
Subsequent management (D
1
)
bed in the acute side
QHT
Paracetamol 250mg (10 15 mg/kg) 6 hourly
Salbutamol 2mg 8 hourly
Chart RR 2 hourly
MANAGEMENT AND DISCUSSION
INVESTIGATIONS (D
1
)
WBC/DC
ESR
CXR (URGENT)
Mycoplasma antibodies
Sputum culture & ABST
Blood culture
Viral studies
MANAGEMENT AND DISCUSSION
WBC/DC
WBC 6700/L (6000- 15000)
DC Neutrophils 72%
Lymphocytes 20%
Monocytes 6%
PCV 40%
Platelet count 200000/ L)
Hb 10.1 g/dL (10.5 14 g/dL)
ESR 68mm 1
st
hour
CXR(D
1
)
MANAGEMENT AND DISCUSSION
D
1 afternoon
C. Penicillin 1.5 million units 6 hourly after ST
ST negative
D
1 5 pm
Fever and dry cough present
No vomiting
MANAGEMENT AND DISCUSSION
D
2 (11/11/2004)
Fever spikes present Ex- RR - 40/min
Dry cough present signs of consolidation
Hydration adequate No signs of effusion
Mx Chest physiotherapy
MANAGEMENT AND DISCUSSION
D
3 (12/11/2004)
Fever spikes Ex-RR- 48/min
Dry cough signs of consolidation
SOB & intercostal recession
no effusion
Hydration adequate
No chest pain
Mx IV Gentamicin 37 mg 8 hourly 3-5 mg/kg/day
MANAGEMENT AND DISCUSSION
Ototoxicity
Peak / trough blood levels
MRI
Why not done?
MANAGEMENT AND DISCUSSION
D
3 7.30pm
Fever spikes PR 150/min(80- 120)
Increased cough BP 90/70 mmHg
SOB O2 saturation 95%
Intercostal recessions
Mx
Nebulize- salbutamol 5mg with normal saline 4
hourly
MANAGEMENT AND DISCUSSION
D
4 (13/11/2004)
Fever spikes Ex-RR- 44/min
Dry cough signs of consolidation
SOB & intercostal recession
no effusion
Hydration adequate
No chest pain
MANAGEMENT AND DISCUSSION
D
5 (14/11/2004)
Fever spikes
Dry cough
Signs of consolidation
Mx- CXR
IV cefotaxime 250 mg 8 hourly
MANAGEMENT AND DISCUSSION
D
6 (15/11/2004)
No improvement in the clinical state
Mx
Blood culture
Stop physiotherapy
USS (right lower lobe consolidation with a small pleural effusion)
MANAGEMENT AND DISCUSSION
D
7 (16/11/2004)
No improvement in the clinical state
Mx
Blood for mycoplasma antibodies (private sector)
Inward cold agglutination test positive
IV Clarithromycin125mg/5% dextrose 100cc/12 hr
(125mg/12hr)
Omit Gentamicin and C. Penicillin
Hb- 9.5 g/dL
MANAGEMENT AND DISCUSSION
Inward cold agglutination test
o 1ml of blood
o Anticoagulated bottle
o Cooling 4
0
C
o 3-4 minutes
o Check for agglutination of RBC
nonspecific test
MANAGEMENT AND DISCUSSION
Serum bilirubin- total \direct\ indirect
Blood picture
Blood for cold agglutinin titres (1:32)
Coombs test
MANAGEMENT AND DISCUSSION
D
8(17/11/2004)
No significant clinical improvement
signs of consolidation
Blood culture negative
Mx
Start chest physiotherapy
MANAGEMENT AND DISCUSSION
D
9(18/11/2004)
Fever spikes present
Appetite improving
No sleep disturbances
Signs of consolidation present
USS (right lower lobe consolidation with a small pleural effusion,
no evidence of empyema)
MANAGEMENT AND DISCUSSION
D
9(18/11/2004)
Traced the mycoplasma antibody test in
MRI
Report - Significant titer suggestive of recent
mycoplasma infection
Mycoplasma
Further management
IV clarithromicin
CXR
Problems identified
Lower respiratory tract infection
Loss of preschool activities
Anxiety of the mother
Absence of father
Lack of proper spacing between
children
THANK YOU
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Learn Different Ways in Which Such Mental Health Problems Will Interfere With The Management of The Physical ProblemДокумент5 страницLearn Different Ways in Which Such Mental Health Problems Will Interfere With The Management of The Physical ProblemTashii TsheringОценок пока нет
- Group BДокумент6 страницGroup BTashii TsheringОценок пока нет
- A Patient With Haemoptysis: Professorial Group B Iwc 3 MFC 864 - 873Документ31 страницаA Patient With Haemoptysis: Professorial Group B Iwc 3 MFC 864 - 873Tashii TsheringОценок пока нет
- Management of Cardiac FailureДокумент21 страницаManagement of Cardiac FailureTashii Tshering100% (1)
- Drug Route Dose FrequencyДокумент2 страницыDrug Route Dose FrequencyTashii TsheringОценок пока нет
- Drug ChartДокумент2 страницыDrug ChartTashii TsheringОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Citation WorksheetДокумент5 страницCitation WorksheetZafar Ibn Kader 2013819030Оценок пока нет
- Jonas, Waine B. - Manual de Terapias AlternativasДокумент348 страницJonas, Waine B. - Manual de Terapias AlternativaspauloadrianoОценок пока нет
- Letter of Support Template - 0 PDFДокумент2 страницыLetter of Support Template - 0 PDFselamitspОценок пока нет
- Case Study - Mariveles - BataanДокумент22 страницыCase Study - Mariveles - Bataankoko BunchОценок пока нет
- Implementing Telemedicine Services During COVID-19: Guiding Principles and Considerations For A Stepwise ApproachДокумент25 страницImplementing Telemedicine Services During COVID-19: Guiding Principles and Considerations For A Stepwise ApproachlauОценок пока нет
- Full Psych DB InterviewДокумент30 страницFull Psych DB InterviewAdam GОценок пока нет
- NRSG367-202160 AT2 - Case Study-Written Assignment V2Документ3 страницыNRSG367-202160 AT2 - Case Study-Written Assignment V2sirjaxx motivation and rootsОценок пока нет
- Understanding Osteoarthritis and Its ManagementДокумент160 страницUnderstanding Osteoarthritis and Its ManagementPedro GouveiaОценок пока нет
- Part-IДокумент507 страницPart-INaan SivananthamОценок пока нет
- UN Declaration of The Rights of The Child (1959)Документ2 страницыUN Declaration of The Rights of The Child (1959)bonalawОценок пока нет
- Sleeping Habits Classroom Behaviour andДокумент10 страницSleeping Habits Classroom Behaviour andSamir SolimanОценок пока нет
- 3390 3396 PDFДокумент7 страниц3390 3396 PDFXavier Alexandro Ríos SalinasОценок пока нет
- EO-GA-32 Continued Response To COVID-19 IMAGE 10-07-2020Документ7 страницEO-GA-32 Continued Response To COVID-19 IMAGE 10-07-2020Jakob RodriguezОценок пока нет
- Puskesmas Wanggudu Raya: Dinas Kesehatan Kabupaten Konawe UtaraДокумент6 страницPuskesmas Wanggudu Raya: Dinas Kesehatan Kabupaten Konawe UtaraicaОценок пока нет
- The Original Prevention of Sickness PamphletДокумент88 страницThe Original Prevention of Sickness PamphletGeorge Singleton100% (4)
- Ethical & Legal Issues in Canadian NursingДокумент950 страницEthical & Legal Issues in Canadian NursingKarl Chelchowski100% (1)
- Asynchronous Activities IE 533Документ34 страницыAsynchronous Activities IE 533Ryanne TeñosoОценок пока нет
- Beneficence and NonДокумент4 страницыBeneficence and NonRoselle Farolan LopezОценок пока нет
- Understanding COVID - 19 PandemicДокумент10 страницUnderstanding COVID - 19 PandemicShyam KantОценок пока нет
- Nooriya Prabhakaran Visualcv Resume 2017Документ2 страницыNooriya Prabhakaran Visualcv Resume 2017api-372799602Оценок пока нет
- Ncezid FRM Pass Attest Eng 508Документ5 страницNcezid FRM Pass Attest Eng 508GO STUDY ABROAD OFFICIALОценок пока нет
- Science: Quarter 1, WK 2 - Module 2Документ29 страницScience: Quarter 1, WK 2 - Module 2Raniey Mayol100% (1)
- Irene Gee Regidor BSED-English Conditions of Developmental Delay 1. Mental RetardationДокумент3 страницыIrene Gee Regidor BSED-English Conditions of Developmental Delay 1. Mental RetardationAliana CabalunaОценок пока нет
- Low Back Pain - Mechanism, Diagnosis and Treatment 6th Ed - J. Cox (Williams and Wilkinson, 1999) WW PDFДокумент752 страницыLow Back Pain - Mechanism, Diagnosis and Treatment 6th Ed - J. Cox (Williams and Wilkinson, 1999) WW PDFMatei Teodorescu100% (5)
- NANDA Nursing Diagnosis Domain 1Документ8 страницNANDA Nursing Diagnosis Domain 1krystaliciousОценок пока нет
- Queenie Rose Domingo - Drug Study (Silver Sulfadiazine)Документ1 страницаQueenie Rose Domingo - Drug Study (Silver Sulfadiazine)Sheryl Ann Barit PedinesОценок пока нет
- Approach To The History and Evaluation of Vertigo and DizzinessДокумент24 страницыApproach To The History and Evaluation of Vertigo and DizzinessPAULA GABRIELA ABAD POLOОценок пока нет
- Mitchell H. Katz-Evaluating Clinical and Public Health Interventions - A Practical Guide To Study Design and Statistics (2010)Документ176 страницMitchell H. Katz-Evaluating Clinical and Public Health Interventions - A Practical Guide To Study Design and Statistics (2010)Lakshmi SethОценок пока нет
- Hearing Loss in Adults Assessment and Management PDF 1837761878725 PDFДокумент20 страницHearing Loss in Adults Assessment and Management PDF 1837761878725 PDFxtineОценок пока нет
- Assessment Test Descriptions PyДокумент19 страницAssessment Test Descriptions PyDewa Ayu VeronicaОценок пока нет