Академический Документы
Профессиональный Документы
Культура Документы
Ointments, Creams, and Gels (4) Legit
Загружено:
Thea Valdez-VitalОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Ointments, Creams, and Gels (4) Legit
Загружено:
Thea Valdez-VitalАвторское право:
Доступные форматы
OINTMENTS, CREAMS,
AND GELS
Ointments, creams
and gels
- Semisolid dosage
forms intended for
topical application
Types of Preparations according to effects
Medicated
Unmedicated
used for the therapeutic agents
they contain
used as protectants or lubricants
Types according to dermatologic applications
Topical dermatological product
Transdermal product
Deliver drug into the skin in treating
dermal disorders
Skin as the target organ
Deliver drugs though the skin
(percutaneous absorption) the
general circulation for systemic
effects
The skin is not a target organ
OINTMENTS
Ointments are semisolid preparations intended for external
application to the skin or mucous membranes
Either medicated or unmedicated
Ointment bases used for their physical effects or as
vehicles for medicated ointments
Ointment Bases
Generally classified by the USP into four groups
1. oleaginous bases
2. absorption bases
3. water-removable bases
4. water soluble bases
Oleaginous bases
a.k.a hydrocarbon bases
Emollient effect
Protect against the escape of moisture
Occlusive dressing
Remain on the skin for long periods
Difficult to wash off
Mineral oil levigating agent when powdered
substances are incorporated
4 TYPES OF OLEAGINOUS BASES
Petrolatum, USP
Purified mixture of
semisolid hydrocarbons
obtained from petroleum
Also known as yellow
petrolatum and
petroleum jelly
Commercial product:
Vaseline
White Petrolatum, USP
Purified mixture of semisolid
hydrocarbons from petroleum
that has been wholly or nearly
decolorized
Same purpose as petrolatum
but esthetically pleasing
Also known as white petroleum
jelly
White Vaseline
Yellow Ointment, USP
This ointment has the
following formula for the
preparation of 1000 g:
Yellow wax 50 g
Petrolatum 950 g
Puried wax obtained from
the honeycomb of the bee
Apis mellifera.
White Ointment, USP
This ointment differs from
yellow ointment by
substitution of white wax
and white petrolatum in the
formula
Absorption Bases
TWO TYPES:
(a)those that permit the incorporation of aqueous solutions
resulting in the formation of water-in-oil (W/O) emulsions
e.g., hydrophilic petrolatum
(b) those that are W/O emulsions (syn: emulsion bases)
that permit the incorporation of additional quantities of
aqueous solutions
e.g., lanolin
TWO TYPES OF ABSORPTION BASES
Hydrophilic Petrolatum,
USP
Has the following formula for the
preparation of 1000 g:
Cholesterol 30 g
Stearyl alcohol 30 g
White wax 80 g
White petrolatum 860 g
Aquaphor (commercial product)
- has the capacity to absorb up to
three times its weight in water and
useful to help incorporate a water-
soluble drug into an oleaginous
ointment base
e.g. tobramycin sulfate
Lanolin, USP (Anhydrous lanolin)
obtained from the wool of sheep
(Ovis aries), is a puri ed waxlike
substance that has been cleaned,
deodor- ized, and decolorized.
o Modified Lanolin, USP - is lanolin
processed to reduce the contents of
free lanolin alcohols and any
detergent and pesticide residues
Water-Removable Bases
are oil-in-water emulsions
resembling creams
easily washed from skin
often called water-
washable bases
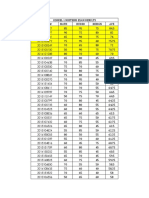
Example: Hydrophilic Ointment, USP
has the ff. formula for the preparation of
about 1000 g:
Ingredient Amount (grams)
Methylparaben 0.25
Propylparaben 0.15
Sodium lauryl sulfate 10.00
Propylene glycol 120.00
Stearyl alcohol 250.00
White petrolatum 250.00
Puried water 370.00
Water-Soluble Bases
do not contain oleaginous
components
water washable
greaseless
Example: Polyethylene Glycol
Ointment, NF
- a polymer of ethylene oxide
and water represented by the
formula H(OCH2CH2)nOH
oThe general formula for
preparation of 1,000 g of PEG
ointment:
PEG 3350 400 g
PEG 400 600 g
PEG 3350 (solid) + PEG 400
(liquid) = very pliable semisolid
ointment
(pic pls)
Preparation of Ointments
Incorporation and Fusion
Incorporation
components are mixed until a uniform preparation is
attained
Small scale using a mortar and pestle
Others use Unguator electronic mortar and pestle (pic)
Two types of Incorporation
1. Incorporation of Solids
2. Incorporation of Liquids
Incorporation of Solids
the pharmacist works the
ointment with a stainless
steel spatula having a long,
broad blade and removes
the accumulation of ointment
on the large spatula with a
smaller one
Hard rubber spatulas used
when ointments react with
metal
Incorporation of Liquids
Liquid sub- stances or
solutions of drugs, as
described above, are added
to an ointment only after due
consid- eration of an
ointment bases capacity to
accept the volume required.
Pic
Fusion Method
all or some of the components
of an ointment are combined by
being melted together and
cooled with constant stirring
until congealed
Examples:
Medicated ointments and
ointment bases containing
components such as beeswax,
parafn, stearyl alcohol, and
high-molecular-weight PEG
pic
Compendial Requirements for Ointments
MICROBIAL CONTENT
preparations prone to microbial growth must contain
antimicrobial preservatives
Preparations that contain water tend to support
microbial growth to a greater extent than water-free
preparations.
o Example: Betamethasone Valerate Ointment, USP,
meet the requirements of the tests for absence of
Staphylococcus aureus and Pseudomonas aeruginosa.
PACKAGING, STORAGE, AND
LABELING
Ointments and other semisolid preparations - large-
mouth ointment jars or in metal or plastic tubes.
Semisolid preparation - well-closed containers to
protect against contamination and in a cool place to
protect against product separation in heat.
Light-sensitive preparations - opaque or light-resistant
containers.
MINIMUM FILL
The USPs minimum ll test is determination of the net
weight or volume of the contents of lled containers to
ensure proper contents compared with the labeled
amount
ADDITIONAL STANDARDS
examine semisolid preparations for viscosity and for in
vitro drug release to ensure within-lot and lot-to-lot
uniformity
CREAMS
semisolid preparations containing one or
more medicinal agents dissolved or dispersed
in either a W/O emulsion or an oil-in-water
emulsion or in another type of water-washable
base.
easier to spread and remove than ointments
Vanishing creams - oil-in-water emulsions
containing large percentages of water and
stearic acid or other oleaginous components.
(pic sa left)
GELS
semisolid systems consisting of dispersions of small
or large molecules in an aqueous liquid vehicle
rendered jellylike by the addition of a gelling agents
Also called jellies
May thicken on standing, forming a thixotrope
Examples of gelling agents:
synthetic macromolecules - carbomer 934
cellulose derivatives - carboxymethylcellulose or
hydroxypropyl methylcellulose
natural gums tragacanth (pic sa left)
Single-phase gels
gel mass consisting of occules of small distinct
particles
Ex. Milk of magnesia consists of a gelati- nous
precipitate of magnesium hydroxide
(pics for the two please)
Magma (two-phase
system)
are gels in which the macro- molecules
are uniformly distributed throughout a
liquid with no apparent boundaries
between the dispersed macromolecules
and the liquid.
MISCELLANEOUS SEMISOLID
PREPARATIONS
PASTES, PLASTERS, AND GLYCEROGELATINS
PASTES
are semisolid preparations intended for application to the
skin. They generally contain a larger proportion of solid
material (such as 25%) than ointments and therefore are
stiffer.
Example:
Lassars Plain Zinc Paste zinc oxide paste
PLASTERS
o are solid or semisolid adhesive masses spread on a backing of
paper, fabric, moleskin, or plastic.
o adhesive material is a rubber base or a synthetic resin
o provide prolonged contact at the site
o provide protection or mechanical support at the site of application
o provide effects at the site of application.
Example: Salicylic acid plaster removal of corns
GLYCEROGELATINS
plastic masses containing gelatin (15%), glycerin
(40%), water (35%), and an added medicinal
substance (10%)
applied to the skin for the long term
melted before applica- tion, cooled to slightly above
body temperature
Example:
Zinc gelatin - treatment of varicose ulcers
PACKAGING SEMISOLID
PREPARATIONS
Topical dermatologic products
jars, tubes, or syringes (pics)
Ophthalmic, nasal, vaginal, and
rectal semisolid products
tubes or syringes (pics)
Ointment jars
clear or opaque glass or plastic
colored green, amber, or blue
Opaque jars
Used for light-sensitive products
Porcelain white, dark green, or
amber
0.5 oz to 1 lb.
TUBES
o light in weight
o inexpensive
o convenient for use
o compatible with most formulative components
o provide greater protec- tion against external
contamination and environ- mental conditions than jars
Ointment tubes
made of aluminum or plastic (PIC)
special applicator tips
Tubes of aluminum
coated with an epoxy resin, vinyl,
or lacquer to elimi- nate any
interactions between the contents
and the tube (PIC)
Plastic tubes
made of high- or low-density polyethylene (HDPE or
LDPE) or a blend of each, polypropylene (PP),
polyethylene terephthalate (PET), and various plastic,
foil, and/or paper laminates, sometimes 10 layers thick
(PIC ON THE RIGHT PLS)
Special Features and Advantages of
Plastics
LDPE (Low Density Polyethylene) - soft and resilient,
and it provides a good moisture barrier
HDPE (High Density Polyethylene) - provides a
superior moisture barrier but is less resilient
PP (Polypropylene) - has a high level of heat
resistance
PET (Polyethylene Terephthalate) - offers transparency
and a high degree of product chemical compatibility
Laminates - provide an excellent moisture barrier
because of the foil content, high durability, and product
compatibility
Multiple-dose tubes
have conventional, continuous
thread closures (pic)
Single-dose tubes
prepared with a tearaway tip (pic)
Filling Ointment Jars
SMALL SCALE
- carefully transferring the weighed amount of ointment
into the jar with a spatula
Ointments prepared by fusion - poured directly into the
ointment jar to congeal in it.
LARGE-SCALE
- pressure llers force the specied amount of ointment
into the jars
Filling Ointment Tubes
oTubes are lled from the open back end of the tube, opposite from the cap
end
o Plastic and laminate tubes - closed and sealed by heat and crimping
o Metal tubes - sealed by folding and crimping with or without a vinyl, latex, or
lacquer sealant
Ointments prepared by fusion - poured while still soft but viscous directly
into the tubes with caution to prevent stratication of the components
SMALL SCALE - tube may be lled manually or with a small-scale lling
machine
Caulking-gun system - semisolid is lled into the chamber and the product is
delivered into the tube
LARGE-SCALE - automatic lling, closing, crimping, and labeling machines
Filling syringes
o by drawing the semisolid into the barrel using the plunger
(it may be necessary to soften the preparation by gentle
heating first)
by removing the plunger and filling through the back end of
the syringe.
o The plunger can then be reinserted
placing a straightened paper clip down the inside of the
barrel and inserting the plunger. The paper clip allows the
escape of air until the plunger contacts the ointment. The
paper clip can then be removed and the seal formed by the
plunger is reestablished.
FEATURES AND USE OF
DERMATOLOGIC PREPARATIONS
in treating skin diseases, the drug in a medicated application
should penetrate and be retained in the skin for a while.
the stratum corneum functions as a semi permeable artificial
membrane and drug penetration is only possible through passive
diffusion.
the rate of drug movement from this skin layer depends on the drug
concentration on the vehicle, aqueous solubility and oil-water
partition coefficient.
if the drug reaches the vascularized dermal layer, it becomes
available for absorption in the general circulation.
Oleaginous bases provide greater occlussion and emollient effects than do hydrophilic and water-
washable bases.
Pastes offer greater occlusion and are more effective than ointments.
Creams usually o/w emulsions spread more easily than ointments and are easier to remove.
Water soluble bases are non greasy and easy to remove unless directed not to.
1-3 mg of ointment or cream is applied per square cm of the skin.
Unless there is a specified need for an occlusive dressing to protect the area from excessive contact or
contaminants, a bandage should not be used.
the major route by which drugs enter the eye is simple diffusion through the cornea.
for drugs that are poorly absorbed by the cornea, the conjunctiva and sclera provide an
alternate route.
compared with ophthalmic solutions, ophthalmic ointments and gels provide extended
residence time on the surface of the eye, increasing the duration of their surface effects and
bioavailability for absorption to the ocular tissues.
the ointment base must not cause irritation to the eye and permit the diffusion of medicinal
substances throughout the secretion of the eye
FEATURES AND USE OF
Ophthalmic Ointments and Gels
Ophthalmic ointments must meet the USP sterility tests and the test for metal particles
in ophthalmic ointments requirement.
steam sterilization or ethylene oxide methods are ineffective because neither is capable
of penetrating the ointment base.
dry heat sterilization can penetrate the ointment base but the high heat might pose a threat to
the stability of the drug substance
because of this, sterilization generally is not under taken but strict method of asceptic
processing are employed.
antimicrobial preservative methylparaben & proplylparaben combinations, phenylmercuric
acetate, chlorobutanol and benzalkonium chloride.
USP directs that ophthalmic ointments must be packaged in collapsible ointment tubes - these
tube shave elongated narrow tip to facilitate a narrow band of ointment to the eye.
drugs introduced into the nasal passage are primarily
for local effects on the mucous membrane and
underlying tissues.
drug absorption can occur through the blood supply in
the nasal lining.
nasal route holds great promise for the administration
of insulin, vaccines, polypeptides and proteins.
FEATURES AND USE OF
Nasal Ointments and Gels
FEATURES AND USE OF
Rectal Preparations
Dosage forms used in the topical treatment of anorectal conditions
ointments gels
creams
cream-like aerosol
foams
solutions (for enema or irrigation)
suppositories
10/22/2014
Ointments, creams, and gels are:
used for topical application to the perianal area and for insertion within the anal canal
used to treat local conditions of anorectal pruritus, inflammation, and the pain associated with
hemorrhoids
The drugs includes (ointments):
astringents (e.g., zinc oxide)
protectants and lubricants (e.g., cocoa butter, lanolin)
Local anesthetics (e.g., pramoxine HCl)
antipruritics, anti- infl ammatory agents (e.g.,hydrocortisone), and antiepileptics (diazepam).
The bases used in anorectal ointments and creams include:
combinations of PEG 300 and 3350
emulsion cream bases using cetyl alcohol and cetyl esters wax
white petrolatum and mineral oil.
10/22/2014
When antimicrobial preservatives are required, methylparaben, propylparaben,
benzyl alcohol, and butylated hydroxyanisole are frequently used.
Administration of rectal ointments and creams:
1. With the patient lying down on the back or side or in an otherwise comfortable
position, rectal tip is slowly and carefully inserted into the anus.
2. Tube is squeezed to force medication through the perforations in the rectal tip and
releases it to the inner lining of the anus.
3. Tip is slowly removed from the anus and any excess ointment or cream removed
from the perianal area
4. Rectal tip should be cleaned thoroughly, the closure cap replaced on the tube, and
the hands washed
o Rectal aerosol foam products (e.g., Proctofoam-HC, Schwarz) also are
accompanied by applicators to facilitate administration.
10/22/2014
Administration if rectal aerosol foam products:
1. Applicator is attached attached to the aerosol
container and filled with a measured dose of product.
2. Applicator is then inserted into the anus and the
product delivered by pushing the plunger of the
applicator
3. After removal, the applicator should be thoroughly
washed
10/22/2014
10/22/2014
FEATURES AND USE OF
Vaginal Preparations
Dosage forms used in the topical treatment of conditions and diseases of the
vulvovaginal area:
ointments
creams
creamlike foams
gels
suppositories
vaginal inserts
transdermal drug delivery systems
oral forms
10/22/2014
Topical products are used to treat vulvovaginal infections, vaginitis, conditions of endometrial atrophy,
and for contraception with spermatocidal agents.
The usual pathogenic organisms of vulvovaginal infections and vaginitis are: Trichomonas vaginalis,
Candida (Monilia) albicans, and Haemophilus vaginalis.
Anti-infective agents:
nystanin, clotrimazole, miconazole, clindamycin and sulfonamides
Endometrial atrophy may be treated locally by:
dienestrol and progesterone (which are used to restore the vaginal mucosa to its normal state).
Contraceptive preparations containing spermicidal agents such as nonoxynol-9 and octoxynol are used
alone or in combination with a cervical diaphragm
10/22/2014
Ointments, creams, and gels for vaginal use are packaged in tubes
Vaginal foams, in aerosol canisters
Preparations are applied externally to the vulva: Mycelex-7 Vaginal Cream, Bayer
Treating external vulvar conditions:
The patient squeezes a small amount of product onto the fingers or tissue and gently
spreads it
For intravaginal treatment:
patient uses a plastic applicator, some of which are prefilled and disposable and others
reusable and filled by the patient immediately prior to use.
10/22/2014
To fill the applicator:
1. the closure cap is removed from the tube, the applicator screwed on in its place,
the tube gently squeezed until the applicator is filled and the plunger rises to its
marked stopping point.
2. The filled applicator is unscrewed from the tube and replaced by the cap.
o Inserting intravaginal products:
is best accomplished with the patient lying on her back or in an otherwise
comfortable position.
The applicator barrel is firmly grasped and inserted into the vagina as far as
possible without causing discomfort.
The plunger is depressed until it stops, releasing the medication in the vagina.
The applicator is carefully withdrawn for washing and ultimately discarding.
The patient should be instructed to wash her hands thoroughly after use.
10/22/2014
Aerosol foams are used intravaginally in the same general
manner.
1. The aerosol package contains an inserter device which when
attached to the canister, may be filled with foam.
2. The filled inserter is placed in the vagina and the product
delivered by pushing the plunger.
3. Vaginal foams are oil-in-water emulsions resembling light
creams. They are water miscible and nongreasy.
4. The patient should be instructed to wash her hands
thoroughly after use
10/22/2014
When once-a-day administration is prescribed, it is best done at bedtime for reasons of
medication retention, avoidance of daytime leakage, and lessened soiling of clothing.
Creams with water washable bases are preferred to oleaginous ointments.
Patients who are pregnant must not use intravaginal products except with their doctors
approval and supervision.
Tampons are not to be used during intravaginal treatment.
Unmedicated lubricant jellies are used by physicians in rectal, urethral, and vaginal
examinations.
All products should be tightly closed when not in use to prevent contamination. If left
unsealed, gels and jellies are particularly prone to dry out.
10/22/2014
Вам также может понравиться
- Topical Drug Delivery Systems: DR Khalid Sheikh Department of Pharmaceutics Room 419 EmailДокумент36 страницTopical Drug Delivery Systems: DR Khalid Sheikh Department of Pharmaceutics Room 419 Emailchegu BusinessОценок пока нет
- Semisolid Dosage Forms: Industrial ProcessingДокумент35 страницSemisolid Dosage Forms: Industrial ProcessingSharon Fredric SinghОценок пока нет
- Phardose Report (Solutions)Документ59 страницPhardose Report (Solutions)Anne Marion PerezОценок пока нет
- OintmentsДокумент74 страницыOintmentsJezreel JavierОценок пока нет
- Semi-Solid Dosage Forms: Ointments, Creams, Pastes & GelsДокумент35 страницSemi-Solid Dosage Forms: Ointments, Creams, Pastes & GelsAnaliza Kitongan LantayanОценок пока нет
- Ointment Cream and GelsДокумент79 страницOintment Cream and GelsGwyneth Cartalla100% (2)
- Chapter 7 Semi-SolidДокумент13 страницChapter 7 Semi-SolidAnaliza Kitongan Lantayan0% (1)
- Liquid Orals DeepsДокумент58 страницLiquid Orals Deepsjalsadeeps1100% (1)
- Semi-Solid Dosage Forms: Ointments, Creams, Pastes & GelsДокумент38 страницSemi-Solid Dosage Forms: Ointments, Creams, Pastes & GelsNanthicha Mkpl100% (1)
- Herbal Cosmetics 1Документ19 страницHerbal Cosmetics 1Mas Nuri100% (1)
- Topical and Transdermal Drug Delivery: Principles and PracticeОт EverandTopical and Transdermal Drug Delivery: Principles and PracticeHeather A. E. BensonРейтинг: 5 из 5 звезд5/5 (1)
- SUPPOSITORIESДокумент38 страницSUPPOSITORIESRahul LakhaniОценок пока нет
- Standardisation of Herbal DrugsДокумент15 страницStandardisation of Herbal Drugsharishkumar kakraniОценок пока нет
- Journal of GelДокумент25 страницJournal of GelRiskilla Fauziyanda PОценок пока нет
- Formulation of DoxyclineДокумент92 страницыFormulation of Doxyclinealexpharm0% (1)
- Microencapsulationgss 160227005508 PDFДокумент70 страницMicroencapsulationgss 160227005508 PDFSelva RathinamОценок пока нет
- Topical GelДокумент4 страницыTopical GelBINDUОценок пока нет
- Phardose - Transdermal Drug Delivery SystemДокумент25 страницPhardose - Transdermal Drug Delivery SystemEdrick RamoranОценок пока нет
- Unit 5, Biostatistics and Research Methodology, B Pharmacy 8th Sem, Carewell PharmaДокумент8 страницUnit 5, Biostatistics and Research Methodology, B Pharmacy 8th Sem, Carewell Pharma60 Shriniwas RaipatwarОценок пока нет
- Effervescent PharmaceuticalsДокумент37 страницEffervescent Pharmaceuticalsatikah febrianiОценок пока нет
- EMULSIONS: Understanding Types, Applications, Stabilization and FormulationДокумент85 страницEMULSIONS: Understanding Types, Applications, Stabilization and FormulationNadia RodasОценок пока нет
- Bioprocessing in The Pharmaceutical Industry: (An Engineering and Technological Overview)Документ39 страницBioprocessing in The Pharmaceutical Industry: (An Engineering and Technological Overview)ManchowОценок пока нет
- New Drug Delivery Systems: A Global OpportunityДокумент24 страницыNew Drug Delivery Systems: A Global OpportunityRugun Clara SamosirОценок пока нет
- Chapter 27 Suspensions and EmulsionsДокумент49 страницChapter 27 Suspensions and EmulsionsKate Montenegro67% (3)
- Archive of SID: Riginal RticleДокумент4 страницыArchive of SID: Riginal RticleDyah Putri Ayu DinastyarОценок пока нет
- Pharmaceutical FormulationДокумент60 страницPharmaceutical FormulationDeepakОценок пока нет
- Oral FormulationsДокумент10 страницOral FormulationsSiddhartha MuppallaОценок пока нет
- Kapitel 6Документ125 страницKapitel 6Jai Murugesh100% (1)
- Cosmetics ReportДокумент13 страницCosmetics ReportSantosh MysoreОценок пока нет
- Lec 10 Drugs Containing Saponin GlycosidesДокумент51 страницаLec 10 Drugs Containing Saponin GlycosidesSandhya Parameswaran100% (2)
- Cosmetic Product Development: Key Definitions and RegulationsДокумент12 страницCosmetic Product Development: Key Definitions and RegulationsHeyward TangilanОценок пока нет
- Modern Pharmaceutics Preformulation ConceptsДокумент35 страницModern Pharmaceutics Preformulation ConceptsTarun ChauhanОценок пока нет
- Preformulation Studies For Development of A Generic Capsule Formulation of Celecoxib Comparable To The Branded (Reference) ProductДокумент14 страницPreformulation Studies For Development of A Generic Capsule Formulation of Celecoxib Comparable To The Branded (Reference) Productsskkale100% (2)
- S02 Dispensing CalculationДокумент15 страницS02 Dispensing CalculationJoe BlackОценок пока нет
- Bio Pharmaceutical An IntroductionДокумент4 страницыBio Pharmaceutical An IntroductionNarendrakumarОценок пока нет
- Manufacturing Phenyl DisinfectantДокумент13 страницManufacturing Phenyl DisinfectantKrishnan NamboothiriОценок пока нет
- Extraction and Isolation TechniquesДокумент58 страницExtraction and Isolation TechniquesLetin Shrivastav100% (1)
- Introduction To Phytochemistry and Tannins-1Документ35 страницIntroduction To Phytochemistry and Tannins-1Boas WayneОценок пока нет
- Dosage Form Manual PharmacyДокумент70 страницDosage Form Manual PharmacySyed Sibtain Hussain ShahОценок пока нет
- Eye Drops PreparationДокумент1 страницаEye Drops PreparationJai MurugeshОценок пока нет
- Phytochemistry PDFДокумент68 страницPhytochemistry PDFTrixia Marix BunglayОценок пока нет
- Parentral Injections PDFДокумент184 страницыParentral Injections PDFMuhammad NadeemОценок пока нет
- List APOTIKДокумент17 страницList APOTIKAtuq MudhaОценок пока нет
- Stability Considerations in Liquid Dosage Forms Extemporaneously ...Документ29 страницStability Considerations in Liquid Dosage Forms Extemporaneously ...herryapt100% (1)
- Pharmaceutical ExcipientsДокумент11 страницPharmaceutical ExcipientsRusyda Humaira ArumaishaОценок пока нет
- United States PharmacopeiaДокумент4 страницыUnited States Pharmacopeiagabriel Rosell0% (1)
- Ridwan Olawale: Dr. 'WaleДокумент6 страницRidwan Olawale: Dr. 'WaleRidwan OlawaleОценок пока нет
- Techniques of SolubilizationДокумент33 страницыTechniques of SolubilizationSreekanth NamaОценок пока нет
- From-philosophy-To-practice Certificate of Achievement PifneqkДокумент2 страницыFrom-philosophy-To-practice Certificate of Achievement PifneqkRidwan OlawaleОценок пока нет
- 02.tablets (-II-)Документ42 страницы02.tablets (-II-)Subha ShankareeОценок пока нет
- Mac Peds FormularyДокумент45 страницMac Peds FormularyLUIS MIGUEL CASTILLA MORANОценок пока нет
- Pharmaceutical SolutionsДокумент29 страницPharmaceutical SolutionsAhmed Imran KabirОценок пока нет
- Evaluation of Crude Drugs PDFДокумент2 страницыEvaluation of Crude Drugs PDFCharles0% (1)
- Pharmaceutical Suppositories & PessariesДокумент34 страницыPharmaceutical Suppositories & PessariesAh Boon100% (1)
- Ointments, Creams and Gels. PhardoseДокумент8 страницOintments, Creams and Gels. PhardoseKim Manlangit100% (1)
- Dosage - Chapter 10Документ9 страницDosage - Chapter 10kaukau4everОценок пока нет
- Reflection 2Документ1 страницаReflection 2Thea Valdez-VitalОценок пока нет
- Group 9 (Higad-Higaran)Документ2 страницыGroup 9 (Higad-Higaran)Thea Valdez-VitalОценок пока нет
- Reflection 3Документ1 страницаReflection 3Thea Valdez-VitalОценок пока нет
- Double Burden of NutritionДокумент1 страницаDouble Burden of NutritionThea Valdez-VitalОценок пока нет
- Anti-Cancer Drugs: Anti-Metabolites ExplainedДокумент4 страницыAnti-Cancer Drugs: Anti-Metabolites ExplainedThea Valdez-VitalОценок пока нет
- InternДокумент23 страницыInternThea Valdez-VitalОценок пока нет
- Hyaline Cartilage Patella - Google SearchДокумент1 страницаHyaline Cartilage Patella - Google SearchThea Valdez-VitalОценок пока нет
- The Role of Age, Gender, Mood States and Exercise Frequency On Exercise Dependence PDFДокумент1 страницаThe Role of Age, Gender, Mood States and Exercise Frequency On Exercise Dependence PDFThea Valdez-VitalОценок пока нет
- Notes Ko Sa Phar12Документ4 страницыNotes Ko Sa Phar12Thea Valdez-VitalОценок пока нет
- Label 114Документ1 страницаLabel 114Thea Valdez-VitalОценок пока нет
- Group 34CДокумент7 страницGroup 34CThea Valdez-VitalОценок пока нет
- OrgChem Formal Report - CaffeineДокумент3 страницыOrgChem Formal Report - CaffeineThea Valdez-VitalОценок пока нет
- Homework in PhilosophyДокумент2 страницыHomework in PhilosophyThea Valdez-VitalОценок пока нет
- Formal Report in Physics (UST)Документ2 страницыFormal Report in Physics (UST)Thea Valdez-VitalОценок пока нет
- Biochemistry Lab Table of ReactionsДокумент1 страницаBiochemistry Lab Table of ReactionsThea Valdez-VitalОценок пока нет
- SCL 3Документ60 страницSCL 3Thea Valdez-VitalОценок пока нет
- Hetar Chapter 22 Outline (Mankiw's)Документ3 страницыHetar Chapter 22 Outline (Mankiw's)Thea Valdez-VitalОценок пока нет
- Classification Tests For Organic Halides Formal ReportДокумент4 страницыClassification Tests For Organic Halides Formal ReportThea Valdez-VitalОценок пока нет
- CRITIQUE PAPER - Pharmaceutical DosageДокумент3 страницыCRITIQUE PAPER - Pharmaceutical DosageThea Valdez-VitalОценок пока нет
- Lab Manual MCSE 101Документ35 страницLab Manual MCSE 101Juan JacksonОценок пока нет
- Chapter 11 revision notes on budgeting and planningДокумент5 страницChapter 11 revision notes on budgeting and planningRoli YonoОценок пока нет
- MTech Information Security FINAL 10052018Документ20 страницMTech Information Security FINAL 10052018sirisha vОценок пока нет
- Goniophotometer T1: OxytechДокумент6 страницGoniophotometer T1: OxytechGustavo CeccopieriОценок пока нет
- Introducing WESAD, A Multimodal Dataset For Wearable Stress and Affect DetectionДокумент9 страницIntroducing WESAD, A Multimodal Dataset For Wearable Stress and Affect DetectionJhónatan CarranzaОценок пока нет
- Max Born, Albert Einstein-The Born-Einstein Letters-Macmillan (1971)Документ132 страницыMax Born, Albert Einstein-The Born-Einstein Letters-Macmillan (1971)Brian O'SullivanОценок пока нет
- Tradesman Electronics PDFДокумент13 страницTradesman Electronics PDFsandeepxrОценок пока нет
- Determination of Voltage DropДокумент6 страницDetermination of Voltage DropFahmi CumiОценок пока нет
- Advu en PDFДокумент65 страницAdvu en PDFGustavo Rodrigues de SouzaОценок пока нет
- Pub - The Physics of The Standard Model and Beyond PDFДокумент314 страницPub - The Physics of The Standard Model and Beyond PDFEduardo Gareca100% (2)
- Smart Dustbin using ArduinoДокумент22 страницыSmart Dustbin using ArduinoEr Dinesh TambeОценок пока нет
- Astm D5501Документ3 страницыAstm D5501mhmdgalalОценок пока нет
- Nādatanumanisham Shankaram Namami Me Manasa ShirasaДокумент12 страницNādatanumanisham Shankaram Namami Me Manasa Shirasaveena murthyОценок пока нет
- Visualizing Interstellar WormholesДокумент14 страницVisualizing Interstellar WormholesFranciscoОценок пока нет
- Facilities Assignment 1-2-2015Документ2 страницыFacilities Assignment 1-2-2015Xnort G. Xwest0% (1)
- Xenomai 3 DocumentationДокумент673 страницыXenomai 3 DocumentationGuile BonafiniОценок пока нет
- Delta VFD E Series User ManualДокумент399 страницDelta VFD E Series User ManualTendai AlfaceОценок пока нет
- PF-CIS-Fall 2022 LABДокумент4 страницыPF-CIS-Fall 2022 LABMuhammad FaisalОценок пока нет
- Tutorial CorelDRAW-X8Документ10 страницTutorial CorelDRAW-X8Ajay BhargavaОценок пока нет
- Example 3 - S-Beam CrashДокумент13 страницExample 3 - S-Beam CrashSanthosh LingappaОценок пока нет
- Metacentric Height: From Wikipedia, The Free EncyclopediaДокумент6 страницMetacentric Height: From Wikipedia, The Free EncyclopediaВладимир ШевченкоОценок пока нет
- Bottazzini RiemannДокумент36 страницBottazzini RiemanncedillaОценок пока нет
- Cross Belt Magnetic Separator (CBMS)Документ2 страницыCross Belt Magnetic Separator (CBMS)mkbhat17kОценок пока нет
- 12 Animation Q1 AnswerДокумент38 страниц12 Animation Q1 AnswerBilly Joe TanОценок пока нет
- CI SetДокумент18 страницCI Setতন্ময় ঢালি Tanmay DhaliОценок пока нет
- Notifier Battery Calculations-ReadmeДокумент11 страницNotifier Battery Calculations-ReadmeJeanCarlosRiveroОценок пока нет
- RelativedensityipgДокумент2 страницыRelativedensityipgapi-310625232Оценок пока нет
- SIEMENS-7SA522 Setting CalculationДокумент20 страницSIEMENS-7SA522 Setting Calculationnaran19794735Оценок пока нет
- SPPID QuestionsДокумент2 страницыSPPID Questionsvivek83% (12)
- Midterm Exam Result Ce199-1l 2Q1920Документ3 страницыMidterm Exam Result Ce199-1l 2Q1920RA CarpioОценок пока нет