Академический Документы
Профессиональный Документы
Культура Документы
Syphilis
Загружено:
luisynonАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Syphilis
Загружено:
luisynonАвторское право:
Доступные форматы
Syphilis Curriculum
Syphilis
Renzo Reyes
Patrick Roquel
Syphilis Curriculum
Definition
a chronic bacterial disease that is
contracted chiefly by infection during
sexual intercourse, but also congenitally
by infection of a developing fetus.
a sexually transmitted infection (STI)
caused by a spirochaete bacterium,
Treponema pallidum.
Other modes of infection through direct
contact on open wounds, skin and mouth
Syphilis Curriculum
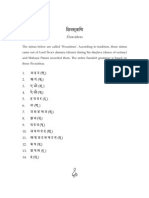
Treponema
pallidum
Spirillum pallidum
Microspironema
pallidum
Spironema
pallidum
Spirochaeta pallida
Gram-negative
bacteria which is
spiral in shape
Syphilis Curriculum
Synonyms
Lues
The great pretender
The pox
syph
Syphilis Curriculum
Pathogenesis
Treponema pallidum
Electron photomicrograph, 36,000 x.
Syphilis Curriculum
Pathogenesis
Treponema pallidum on Darkfield
Microscopy
Source: CDC/NCHSTP/Division of STD Prevention, STD Clinical Slides
Syphilis Curriculum
Pathogenesis
Pathology
Penetration:
T. pallidum enters the body via skin and
mucous membranes through abrasions
during sexual contact
Transmitted transplacentally from mother to
fetus during pregnancy
Dissemination:
Travels via the circulatory system (including
the lymphatic system and regional lymph
nodes) throughout the body
Invasion of the central nervous system (CNS)
can occur during any stage of syphilis.
7
Syphilis Curriculum
Mode of action
migration between endothelial cells
Formation of lesions caused by
Infiltration of sites with CD4+ and
CD8+ T lymphocytes, macrophages,
a few plasma cells
Syphilis Curriculum
Clinical Manifestations
Primary Syphilis
Primary lesion or "chancre" develops at the site
of inoculation.
Chancre
Progresses from macule to papule to ulcer;
Typically painless, indurated, and has a clean base;
Highly infectious;
Heals spontaneously within 3 to 6 weeks; and
Multiple lesions can occur.
Regional lymphadenopathy: classically rubbery,
painless, bilateral
Serologic tests for syphilis may not be positive
during early primary syphilis.
9
Syphilis Curriculum
Clinical Manifestations
Primary SyphilisPenile Chancre
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
10
Syphilis Curriculum
Clinical Manifestations
Primary SyphilisLabial Chancre
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
11
Syphilis Curriculum
Clinical Manifestations
Primary SyphilisPerianal Chancre
12
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
Syphilis Curriculum
Clinical Manifestations
Primary SyphilisChancre of the
Tongue
Source: CDC/ NCHSTP/ Division of STD Prevention /STD Clinical Slides
13
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis
Secondary lesions occur several weeks after the
primary chancre appears; and may persist for
weeks to months.
Primary and secondary stages may overlap
Mucocutaneous lesions most common
Clinical Manifestations:
Rash (75%100%)
Lymphadenopathy (50%86%)
Malaise
Mucous patches (6%30%)
Condylomata lata (10%20%)
Alopecia (5%)
Liver and kidney involvement can occur
Splenomegaly is occasionally present
Serologic tests are usually highest in titer during
this stage.
14
Syphilis Curriculum
Clinical Manifestations
Secondary
Syphilis
Papulosquamo
us Rash
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
15
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis
Palmar/Plantar Rash
Source: Seattle STD/HIV Prevention
Training Center at the University of
Washington, UW HSCER Slide Bank
Source: CDC/NCHSTP/Division of STD
Prevention, STD Clinical Slides
16
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis Generalized
Body Rash
Source: Cincinnati STD/HIV Prevention
Training Center
Source: CDC/NCHSTP/Division of STD Prevention, STD
Clinical Slides
17
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis
Papulo-pustular Rash
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
18
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis Condylomata
lata
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
19
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis Nickel/Dime
Lesions
Syphilis Curriculum
Clinical Manifestations
Secondary Syphilis
Alopecia
21
Syphilis Curriculum
Clinical Manifestations
Latent Syphilis
Host suppresses infection, but no
lesions are clinically apparent
Only evidence is a positive serologic
test
May occur between primary and
secondary stages, between secondary
relapses, and after secondary stage
Categories:
Early latent: <1 year duration
Late latent: 1 year duration
22
Syphilis Curriculum
Clinical Manifestations
Neurosyphilis
Occurs when T. pallidum invades the central
nervous system (CNS)
May occur at any stage of syphilis
Can be asymptomatic
Early neurosyphilis occurs a few months to a few
years after infection
Clinical manifestations can include acute syphilitic
meningitis, meningovascular syphilis, and ocular
involvement
Neurologic involvement can occur decades after
infection and is rarely seen
Clinical manifestations can include general paresis, tabes
dorsalis, and ocular involvement
Ocular involvement can occur in early or late
23
neurosyphilis.
Syphilis Curriculum
Clinical Manifestations
NeurosyphilisSpirochetes in
Neural Tissue
Silver stain, 950x
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
24
Syphilis Curriculum
Clinical Manifestations
Tertiary (Late) Syphilis
Approximately 30% of untreated patients
progress to the tertiary stage within 1 to
20 years.
Rare because of the widespread
availability and use of antibiotics
Manifestations
Gummatous lesions
Cardiovascular syphilis
25
Syphilis Curriculum
Clinical Manifestations
Late SyphilisSerpiginous
Gummata of Forearm
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
26
Syphilis Curriculum
Clinical Manifestations
Late Syphilis - Ulcerating Gumma
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
27
Syphilis Curriculum
Clinical Manifestations
Late Syphilis
Cardiovascular
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
28
Syphilis Curriculum
Clinical Manifestations
Congenital Syphilis
Occurs when T. pallidum is transmitted from a
pregnant woman to her fetus
May lead to stillbirth, neonatal death, and infant
disorders such as deafness, neurologic
impairment, and bone deformities
Transmission can occur during any stage of
syphilis; risk is much higher during primary and
secondary syphilis
Fetal infection can occur during any trimester of
pregnancy
Wide spectrum of severity exists; only severe
cases are clinically apparent at birth
Early lesions (most common): Infants <2 years old;
usually inflammatory
Late lesions: Children >2 years old; tend to be
immunologic and destructive
29
Syphilis Curriculum
Clinical Manifestations
Congenital SyphilisMucous
Patches
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
30
Syphilis Curriculum
Clinical Manifestations
Congenital Syphilis Hutchinsons
Teeth
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
31
Syphilis Curriculum
Clinical Manifestations
Congenital Syphilis Perforation of
Palate
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
32
Syphilis Curriculum
Diagnosis
Laboratory Diagnosis
Identification of Treponema pallidum
in lesion exudate or tissue
Darkfield microscopy
Tests to detect T. pallidum
Serologic tests to allow a
presumptive diagnosis
Nontreponemal tests
Treponemal tests
33
Syphilis Curriculum
Diagnosis
Darkfield Microscopy
What to look for
T. pallidum morphology and motility
Advantage
Definitive immediate diagnosis
Rapid results
Disadvantages
Requires specialized equipment and an
experienced microscopist
Possible confusion with other pathogenic and
nonpathogenic spirochetes
Must be performed immediately
Generally not recommended on oral lesions
Possibility of false-negatives
34
Syphilis Curriculum
Diagnosis
Serologic Tests for Syphilis
Two types
Treponemal (qualitative)
Nontreponemal (qualitative and
quantitative)
The use of only one type of serologic
test is insufficient for diagnosis
35
Syphilis Curriculum
Diagnosis
Nontreponemal Serologic Tests
Principles
Measure antibody directed against a cardiolipinlecithin-cholesterol antigen
Not specific for T. pallidum
Titers usually correlate with disease activity and
results are reported quantitatively
May be reactive for life, referred to as serofast
Nontreponemal tests include VDRL, RPR,
TRUST, USR
36
Syphilis Curriculum
Diagnosis
Treponemal Serologic Tests
Principles
Measure antibody directed against T.
pallidum antigens
Qualitative
Usually reactive for life
Titers should not be used to assess
treatment response
Treponemal tests include TP-PA, FTAABS, EIA, and CIA
37
Syphilis Curriculum
Diagnosis
Causes of False-Positive Reactions in
Serologic Tests for Syphilis
Disease
RPR/VDRL
Age
Autoimmune Diseases
FTA-ABS
Yes
Yes
Cardiovascular Disease
Yes
Yes
Yes
--
Dermatologic Diseases
Yes
Yes
Drug Abuse
Yes
Yes
Febrile Illness
Yes
Glucosamine/chondroitin sulfate
Leprosy
TP-PA
Possibly
Yes
Lyme disease
No
--
Yes
Malaria
Yes
No
Pinta, Yaws
Yes
Yes
Yes
Recent Immunizations
Yes
--
--
STD other
than Syphilis
Source:
Syphilis
Reference Guide, CDC/National Yes
Center
38
for Infectious Diseases, 2002
Syphilis Curriculum
Diagnosis of Latent
Syphilis
Diagnosis
Criteria for early latent syphilis, if within
the year preceding the evaluation
Documented seroconversion or 4-fold increase
in comparison with a serologic titer
Unequivocal symptoms of primary or
secondary syphilis reported by patient
Contact to an infectious case of syphilis
Only possible exposure occurred within past 12
months
Patients with latent syphilis of unknown
duration should be managed clinically as if
they have late latent syphilis.
Public health laws require that all cases of
syphilis be reported to the state/local
39
health department.
Syphilis Curriculum
Diagnosis
CNS Disease Diagnostic Issues
CNS disease can occur during any
stage of syphilis.
Conventional therapy is effective for
the vast majority of immunocompetent patients with
asymptomatic CNS involvement in
primary and secondary syphilis.
40
Syphilis Curriculum
Diagnosis
Indications for CSF Examination
Patients with syphilis who demonstrate any
of the following criteria should have a
prompt CSF evaluation:
Neurologic or ophthalmic signs or symptoms
Evidence of active tertiary syphilis (e.g.,
gummatous lesions)
Treatment failure
HIV infection with a CD4 count 350 and/or a
nontreponemal serologic test titer of 1:32
41
Syphilis Curriculum
Diagnosis
Diagnosis of CNS Disease
No test can be used alone to diagnose
neurosyphilis.
VDRL-CSF: highly specific, but insensitive
Diagnosis usually depends on the following factors:
Reactive serologic test results
Abnormalities of CSF cell count or protein
A reactive VDRL-CSF with or without clinical
manifestations
CSF leukocyte count usually is elevated (>5
WBCs/mm3) in patients with neurosyphilis.
The VDRL-CSF is the standard serologic test for CSF,
and when reactive in the absence of contamination
of the CSF with blood, it is considered diagnostic of
42 it can be
neurosyphilis. However, in early syphilis
Syphilis Curriculum
Management
Therapy for Primary, Secondary, and
Early Latent Syphilis
Benzathine penicillin G 2.4 million units
intramuscularly in a single dose (Bicillin
L-A)
If penicillin allergic
Doxycycline 100 mg orally twice daily for 14
days, or
Tetracycline 500 mg orally 4 times daily for
14 days
Syphilis Curriculum
Management
Therapy for Late Latent Syphilis
Benzathine penicillin G 7.2 million units
total, administered as 3 doses of 2.4
million units intramuscularly each at 1week intervals
If penicillin allergic
Doxycycline 100 mg orally twice daily for 28
days or
Tetracycline 500 mg orally 4 times daily for
28 days
Syphilis Curriculum
Management
Therapy for Tertiary
Syphilis
Benzathine penicillin G 7.2 million units
total, administered as 3 doses of 2.4
million units intramuscularly each at 1week intervals
If penicillin allergic
Doxycycline 100 mg orally twice daily for 28
days or
Tetracycline 500 mg orally 4 times daily for
28 days
Syphilis Curriculum
Management
Therapy for Neurosyphilis
Aqueous crystalline penicillin G 1824 million
units per day, administered as 34 million
units intravenously every 4 hours or
continuous infusion for 10 to14 days
intravenously
Alternative regimen (if compliance can be
ensured)
Procaine penicillin 2.4 million units
intramuscularly once daily PLUS Probenecid 500
mg orally 4 times a day, both for 10 to14 days
Syphilis Curriculum
Management
Therapy for Syphilis in
Pregnancy
Treat with penicillin according to stage of
infection.
Erythromycin is no longer an acceptable
alternative drug in penicillin-allergic patients.
Patients who are skin-test-reactive to
penicillin should be desensitized in the
hospital and treated with penicillin.
Some evidence suggests that additional
therapy can be beneficial for pregnant
women in some settings.
47
Syphilis Curriculum
Jarisch-Herxheimer
Reaction
Management
Self-limited reaction to antitreponemal therapy
Fever, malaise, nausea/vomiting; may be associated with chills
and exacerbation of secondary rash
Occurs within 24 hours after therapy
Not an allergic reaction to penicillin
More frequent after treatment with penicillin and
treatment of early syphilis
Antipyretics can be used to manage symptoms, but they
have not been proven to prevent this reaction.
Pregnant women should be informed of this possible
reaction, that it may precipitate early labor, and to call
obstetrician if problems develop.
Вам также может понравиться
- 12.contamination and Infection ControlДокумент21 страница12.contamination and Infection ControlluisynonОценок пока нет
- Anatomy of The HeartДокумент31 страницаAnatomy of The HeartYuNa YoshinoyaОценок пока нет
- Syphilis SsДокумент4 страницыSyphilis SsluisynonОценок пока нет
- Recombinant Dna Technology: EcoriДокумент2 страницыRecombinant Dna Technology: EcoriluisynonОценок пока нет
- Iinternship 13Документ35 страницIinternship 13Darwin MangabatОценок пока нет
- Stereo ChemistryДокумент1 страницаStereo ChemistryluisynonОценок пока нет
- 04b.bacteriology - BiofilmsДокумент97 страниц04b.bacteriology - Biofilmsluisynon100% (1)
- Anatomy of The EarДокумент20 страницAnatomy of The EarluisynonОценок пока нет
- Unit Dose SystemДокумент38 страницUnit Dose SystemluisynonОценок пока нет
- Trigonometric Ratios of Special AnglesДокумент28 страницTrigonometric Ratios of Special AnglesluisynonОценок пока нет
- Anatomy of The Digestive SystemДокумент71 страницаAnatomy of The Digestive SystemluisynonОценок пока нет
- Endocrine SystemДокумент32 страницыEndocrine Systemluisynon100% (2)
- Chapter 11 Transdermal Drug Delivery SystemДокумент3 страницыChapter 11 Transdermal Drug Delivery SystemluisynonОценок пока нет
- 10 Translational Equilibrium HandoutДокумент18 страниц10 Translational Equilibrium HandoutluisynonОценок пока нет
- Gymnosperms 2013Документ57 страницGymnosperms 2013luisynonОценок пока нет
- Why MARRYДокумент1 страницаWhy MARRYmeerocks_12Оценок пока нет
- Locating Center of Gravity ObjectsДокумент18 страницLocating Center of Gravity ObjectsluisynonОценок пока нет
- Preparation of Sodium Bicarbonate Ear Drops StudentsДокумент2 страницыPreparation of Sodium Bicarbonate Ear Drops Studentsluisynon67% (3)
- Cost Benefit AnalysisДокумент46 страницCost Benefit AnalysisluisynonОценок пока нет
- Transdermal Drug DeliveryДокумент4 страницыTransdermal Drug DeliveryluisynonОценок пока нет
- Knowledge Management of Hypertension in All Ages in UrbanДокумент3 страницыKnowledge Management of Hypertension in All Ages in UrbanluisynonОценок пока нет
- (Yaranaika) MS EXCEL 2010Документ3 страницы(Yaranaika) MS EXCEL 2010Kenrick EvanderОценок пока нет
- CapsulesДокумент2 страницыCapsulesluisynonОценок пока нет
- Ms Word 2010Документ3 страницыMs Word 2010BillQueОценок пока нет
- Bacteriology Culture Media Day 2Документ3 страницыBacteriology Culture Media Day 2luisynonОценок пока нет
- Naming Alcohols GuideДокумент1 страницаNaming Alcohols GuideluisynonОценок пока нет
- Methamphetamine Increases Locomotion and Dopamine Transporter Activity in Dopamine D5 ReceptorДокумент1 страницаMethamphetamine Increases Locomotion and Dopamine Transporter Activity in Dopamine D5 ReceptorluisynonОценок пока нет
- Ointments Cream and GelsДокумент3 страницыOintments Cream and GelsluisynonОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- CV 20150412Документ2 страницыCV 20150412api-286316633Оценок пока нет
- Strong As An Ox Olympic Weightlifting Program Manual PDFДокумент32 страницыStrong As An Ox Olympic Weightlifting Program Manual PDFJonathan Schroeder80% (5)
- Animal Production (Poultry-Chicken) NC IIДокумент10 страницAnimal Production (Poultry-Chicken) NC IIAljon BalanagОценок пока нет
- Seaweed Feasibility Final ReportДокумент115 страницSeaweed Feasibility Final Reportg4nz0100% (3)
- What Happened in Jay and Sniffer: The Bike Race? Answer The QuestionsДокумент8 страницWhat Happened in Jay and Sniffer: The Bike Race? Answer The QuestionsEssential English CenterОценок пока нет
- 9 Categorical SyllogismДокумент48 страниц9 Categorical SyllogismMK KMОценок пока нет
- 0528Документ5 страниц0528dokter muda obgynОценок пока нет
- İngilizce Testindeki Boşluklara Uygun Kelime BulmaДокумент15 страницİngilizce Testindeki Boşluklara Uygun Kelime Bulmamehmet100% (1)
- Intermediate Reading Comprehension Test 02Документ3 страницыIntermediate Reading Comprehension Test 02Diosmari Santos100% (1)
- Master Tung's Four Horses Combination - Master Tung's Magic PointsДокумент12 страницMaster Tung's Four Horses Combination - Master Tung's Magic PointsAWEDIOHEAD93% (14)
- Rabbit Health LogДокумент9 страницRabbit Health LogEriu NobletОценок пока нет
- Nursing Case Study CellulitisДокумент26 страницNursing Case Study CellulitisjoselaureanoОценок пока нет
- The Death of SiegfriedДокумент6 страницThe Death of SiegfriedStephen Ashley SalvadorОценок пока нет
- Sanskrit TextbookДокумент113 страницSanskrit TextbookGokul Bhandari100% (4)
- Đề KT Unit 2 - Tiếng Anh 2 Smart Start - Ma TrậnДокумент2 страницыĐề KT Unit 2 - Tiếng Anh 2 Smart Start - Ma TrậnThuỳ LinhОценок пока нет
- Fish Integument FunctionsДокумент67 страницFish Integument Functionslow luffecussОценок пока нет
- Bearing Torches A Devotional Anthology For Hekate PDFДокумент287 страницBearing Torches A Devotional Anthology For Hekate PDFCyndi Brannen100% (5)
- External Parts of Fish and Their FunctionsДокумент2 страницыExternal Parts of Fish and Their FunctionsElYah100% (1)
- Google-digitized Library Book on Ila Language HandbookДокумент511 страницGoogle-digitized Library Book on Ila Language HandbookGarvey Lives0% (1)
- Seafood/Fish AllergyДокумент4 страницыSeafood/Fish Allergymelissascheichl416Оценок пока нет
- ULTRASOUND Abdomen Normal MeasurementsДокумент20 страницULTRASOUND Abdomen Normal Measurementsadinatop100% (2)
- Oriental MonstersДокумент21 страницаOriental MonstersCaleb Thomas Gutshall100% (2)
- Mijbil The Otter - PPT (2023)Документ9 страницMijbil The Otter - PPT (2023)Ash NagОценок пока нет
- Jurnal Vaksin HPVДокумент9 страницJurnal Vaksin HPVlitaayuningdyahОценок пока нет
- SemanticsДокумент50 страницSemanticsHazirah MustapaОценок пока нет
- Cardio Lesson PlanДокумент4 страницыCardio Lesson PlanAmiel Francisco Reyes100% (1)
- Shakepeare MonolouguesДокумент3 страницыShakepeare MonolouguesLamont Walker IIОценок пока нет
- D&D Adventurers League FAQ v7.1 SummaryДокумент17 страницD&D Adventurers League FAQ v7.1 SummaryFernando LuizОценок пока нет
- Ultrasound Report for 33 Week PregnancyДокумент1 страницаUltrasound Report for 33 Week PregnancyAUSTRIAN DIAGNOSTIC CENTERОценок пока нет