Академический Документы
Профессиональный Документы
Культура Документы
Peripheral Nerve Disorders
Загружено:
Eddie Wyatt0 оценок0% нашли этот документ полезным (0 голосов)
32 просмотров34 страницыThis document discusses peripheral nerve disorders, focusing on radial nerve, ulnar nerve, peroneal nerve, and tibial nerve disorders. It describes the etiology and clinical features of injuries at different levels for each nerve. Assessment involves determining the degree and type of injury through history, exam, and EMG testing. Treatment may include exploration, nerve repair/grafting, tendon transfers, splinting, and surgery depending on the specific nerve and severity of injury. The goal is to address motor and sensory deficits while preventing deformities.
Исходное описание:
sew
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThis document discusses peripheral nerve disorders, focusing on radial nerve, ulnar nerve, peroneal nerve, and tibial nerve disorders. It describes the etiology and clinical features of injuries at different levels for each nerve. Assessment involves determining the degree and type of injury through history, exam, and EMG testing. Treatment may include exploration, nerve repair/grafting, tendon transfers, splinting, and surgery depending on the specific nerve and severity of injury. The goal is to address motor and sensory deficits while preventing deformities.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
32 просмотров34 страницыPeripheral Nerve Disorders
Загружено:
Eddie WyattThis document discusses peripheral nerve disorders, focusing on radial nerve, ulnar nerve, peroneal nerve, and tibial nerve disorders. It describes the etiology and clinical features of injuries at different levels for each nerve. Assessment involves determining the degree and type of injury through history, exam, and EMG testing. Treatment may include exploration, nerve repair/grafting, tendon transfers, splinting, and surgery depending on the specific nerve and severity of injury. The goal is to address motor and sensory deficits while preventing deformities.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 34
PERIPHERAL NERVE DISORDERS
By :
HANANTO WILDAN HABIBI
G0014111
Sebelas Maret of Medical Faculty
Radial Nerve Disorders
Etiology
Injured in the elbow, in the upper arm, or in the
axilla
The Types of Clinical Features
1. Low Lessions
2. High Lessions
3. Very High Lessions
Radial Nerve Disorders
1. Low Lessions
. Etiology: fracture or dislocation at the
elbow, a local wound, Iatrogenic lessions
of the posterior interosseus nerve.
. Clinical Features: Clumsiness, cannot
extend the metacarpophalangeal joint of
the hand, weakness extension and
retroposition of the thumb, wrist extension
is preserved.
Radial Nerve Disorders
2. High Lessions
Etiology: Fracture of the humerus,
prolonged torniquet pressure.
Clinical Features: an obvious wrist
drop, sensory loss is limited to a
small patch on the dorsum around
the anatomical snuffbox.
Radial Nerve Disorders
Radial Nerve Disorders
3. Very High Lessions
Etiology: Trauma or operations around
the shoulder, chronic compression in the
axilla.
Clinical Features: Weakness of the wrist
and hand, the triceps is paralyzed, and
the triceps reflex is absent.
Radial Nerve Disorders
ASSESSMENT
1. The degree of Injury
. The history of the injury, Physical
examination, Electromyography (EMG)
2. Nerve Function
. Sensory and motor function
Radial Nerve Disorders
TREATMENT
1. Open injury
The nerve should be explored
and repaired or grafted as soon as
possible
Radial Nerve Disorders
TREATMENT
2. Closed injury
a. Exploration for a radial nerve injury on
admission before treatment and again after
manipulation or internal fixation.
b. Surgery (Nerve Grafting, Tendon transfer).
c. While recovery is awaited, the small joint of the
hand must be put through a full range of
passive movement. (with splintage)
Radial Nerve Disorders
d. If recovery doesnt occur the disability
can be largely overcome by tendon
transfer: Pronator teres to the short
radial extensor of the wrist; flexor carpi
radialis to the long finger extensor and
palmaris longus to the long thumb
abductor.
Ulnar Nerve Disorders
Etiology
Injuries of the ulnar nerve usually near the
wrist or near the elbow.
The Types of Clinical features
1. Low Lessions
2. High Lessions
Ulnar Nerve Disorders
1. Low Lessions
. Etiology: often caused by cut on shattered
glass, entrapment of the ulnar nerve in the
pisohamate tunnel (guyons canal) by a
deep carpal ganglion or ulnar artery
aneurism.
. Clinical Features: numbness of the ulnar
one and a half finger, Claw hand deformity,
finger abduction is weak, loss of thumb
adduction.
Ulnar Nerve Disorders
2. High Lessions
Etilologi: elbow fracture or dislocation, ulnar
neuritis that caused by compression of the
nerve in the medial epicondylar tunnel.
Clinical features: the hand isnt markedly
deformed, the fingers are therfore less
clawed, motor and sensory are the same
as the low lession
Ulnar Nerve Disorders
Ulnar Nerve Disorders
ASSESSMENT
1. The degree of Injury
. The history of the injury,
examination (e.g.: froments
Electromyography (EMG)
2. Nerve Function
. Sensory and motor function
Physical
sign) ,
Ulnar Nerve Disorders
TREATMENT
a. Exploration for a Ulnar nerve injury on
admission before treatment and again after
manipulation or internal fixation.
b. Surgery (such as nerve repairing, nerve
Grafting, Tendon transfer).
c. Hand physioterapy keeps the hand supple
and useful
Ulnar Nerve Disorders
TREATMENT
Brand Procedure
Tendon transfer from M. Extensor Carpi radialis
longus to Intrinsic Muscle can improve
Metacarpophalangeal flexion.
Zancolli Procedure
Looping a slip of M. Flexor digitorum
superficialis around the opening of the flexor
sheath can also improve Metacarpophalangeal
flexion.
Peroneal Nerve Disorders
Injuries may affect eithe the common
peroneal nerve (lateral popliteal) or one of its
branches the deep or supercial peroneal
nerves.
Clinical Features:
1. The common peroneal nerve
2. The deep peroneal nerve
3. The superficial peroneal nerve
Peroneal Nerve Disorders
1. The common peroneal nerve
. Etiology: damage at the level of the fibular
neck (by severe traction, splintage, and
plaster cast or a ganglion from superior
tibio-fibular joint).
. Clinical features: drop foot, walking with a
high-stepping gait, sensation is lost over the
front and outer half of the leg and the
dorsum of the food. Pain may be significant.
Peroneal Nerve Disorders
2. The deep peroneal nerve
Etiology: anterior compartment syndrome
Clinical features: pain and weakness of
dorsoflexion, sensory loss in small area
of skin between the first and second toes,
paraesthesia and numbness on the
dorsum around first web space if the
distal portion is cut during operation on
the ankle.
Peroneal Nerve Disorders
3. Superficial Peroneal Nerve
Etiology: Lateral compartment syndrome
Clinical features: pain in the lateral part of
the leg and numbness or paraesthesia of
the foot, may be weakness of eversion and
sensory loss on the dorsum of the foot.
The cutaneus branches maybe trapped and
stretched by a severe injury, causing pain
and sensory symptoms without muscle
weakness.
Peroneal Nerve Disorders
ASSESSMENT
1. The degree of Injury
. The history of the injury, Physical
examination, Electromyography (EMG)
2. Nerve Function
. Sensory and motor function
Peroneal Nerve Disorders
TREATMENT
a. Exploration for a peroneal nerve injury on
admission before treatment and again
after manipulation or internal fixation.
b. Surgery (such as Nerve repairing, Nerve
Grafting, Tendon transfer) followed by
splintage to control ankle weakness
c. Tibialis posterior, Permanent Splintage,
or hind foot stabilization if there is no
recovery.
Tibial Nerve Disorders
Etiology:
The tibial (medial popliteal) nerve is rarely injured
except in open wounds. The distal part (posterior
tibial nerve) is sometimes involved in injuries around
the ankle. (can be fracture or dislocation)
Clinical Features:
Unable to plantarflex the ankle or flex the toes,
sensation is absent over the sole and part of the calf,
not much clawing (both intrinsic muscle and long
flexors are involved).
Tibial Nerve Disorders
The posterior tibial nerve gives off a small
calcaneal branch and then divides into
medial and lateral plantar nerve.
The posterior tibial nerve lessions cause
wide sensory loss and clawing of the toes
(intrinsic muscle paralysis, but long
flexors is active)
Injury to one of the smaller branches
causes only limited sensory loss and less
noticable motor weakness.
Tibial Nerve Disorders
ASSESSMENT
1. The degree of Injury
. The history of the injury, Physical
examination, Electromyography (EMG)
2. Nerve Function
. Sensory and motor function
Tibial Nerve Disorders
TREATMENT
a. Exploration for a Tibial nerve injury on admission
before treatment and again after manipulation or
internal fixation.
b. Surgery (such as Nerve repairing, Nerve
Grafting, Tendon transfer) followed by orthosis (to
prevent excessive plantar flexion) and the sole is
protected pressure ulceration.
c. Weakness of plantar flexion can be treated by
hind-foot fusion or transfer of the tibialis anterior
to the back of the foot.
Terima Kasih...
Вам также может понравиться
- Sciatic Nerve - IipptДокумент21 страницаSciatic Nerve - IipptPraneetha NouduriОценок пока нет
- An Update On Peroneal Nerve Entrapment and NeuropathyДокумент9 страницAn Update On Peroneal Nerve Entrapment and NeuropathyClara ViMiОценок пока нет
- Spinal Cord Deseases: Na ShaoДокумент38 страницSpinal Cord Deseases: Na ShaoArvindhanОценок пока нет
- Avascular Necrosis of The HipДокумент22 страницыAvascular Necrosis of The Hipbjpalmer100% (2)
- Choosehealth BrochureДокумент18 страницChoosehealth Brochureapi-487757844Оценок пока нет
- Co-Ordination: Prepared by Ahmed Shawky AliДокумент59 страницCo-Ordination: Prepared by Ahmed Shawky Alivenkata ramakrishnaiahОценок пока нет
- Coordination AssessmentДокумент30 страницCoordination AssessmentBhawna PalОценок пока нет
- Human Anatomy & PhysiologyДокумент72 страницыHuman Anatomy & PhysiologyJoie UrsalОценок пока нет
- Leg UlcerДокумент28 страницLeg UlcerRanindya PutriОценок пока нет
- Wrist FracturesДокумент3 страницыWrist FracturesFarah AzizahОценок пока нет
- Cervical SpondylosisДокумент9 страницCervical SpondylosisNurHidayah Borhanudin100% (1)
- Anxiety and Anxiety Disorders1Документ41 страницаAnxiety and Anxiety Disorders1Anne de VeraОценок пока нет
- Lecture 19 - Vessels and CirculationДокумент67 страницLecture 19 - Vessels and CirculationSasikala MohanОценок пока нет
- Claw HandДокумент23 страницыClaw HandAditya Pratama Saanin100% (1)
- Articular Neurophysiology: Presented by - Yogesh VyasДокумент15 страницArticular Neurophysiology: Presented by - Yogesh VyasvictoryvelavaОценок пока нет
- Soft Tissue InjuryДокумент2 страницыSoft Tissue InjuryThiruОценок пока нет
- Motor Functions of Spinal CordДокумент51 страницаMotor Functions of Spinal CordZoafshan Ashfaque100% (1)
- Seizure Disorder, Spinal Injury Neural TumorДокумент52 страницыSeizure Disorder, Spinal Injury Neural TumornipoОценок пока нет
- Anatomy Reviewer 2.0Документ7 страницAnatomy Reviewer 2.0Angeline VegaОценок пока нет
- MusclesДокумент66 страницMusclesusernameОценок пока нет
- Neurology - Saif.wesmosis.2013 104907Документ68 страницNeurology - Saif.wesmosis.2013 104907Helene AlawamiОценок пока нет
- Shoulder InjuryДокумент79 страницShoulder InjurySudipta BhowmickОценок пока нет
- Peripheral CirculationДокумент27 страницPeripheral CirculationRachel ThomsonОценок пока нет
- A Patient's Guide To Radial Tunnel SyndromeДокумент4 страницыA Patient's Guide To Radial Tunnel SyndromeKarunya Vk100% (1)
- Recognising and Classifying Injuries 9c Injuries Recognising ClassifyingДокумент4 страницыRecognising and Classifying Injuries 9c Injuries Recognising ClassifyingJake GarciaОценок пока нет
- Intravenous TherapyДокумент48 страницIntravenous TherapyFrancr ToledanoОценок пока нет
- Postural Assessment (Mia)Документ9 страницPostural Assessment (Mia)im. EliasОценок пока нет
- Bones and Joints TBДокумент19 страницBones and Joints TBmichaelcylОценок пока нет
- Lumbar Disc HerniationДокумент19 страницLumbar Disc HerniationRabie'ahBahananОценок пока нет
- Peripheral Nerve Injury and Repair: Adam Osbourne, 5th Year MedicineДокумент5 страницPeripheral Nerve Injury and Repair: Adam Osbourne, 5th Year Medicineayrahma29Оценок пока нет
- Male GU ExamДокумент5 страницMale GU ExamOmar Farid ElgebalyОценок пока нет
- Anatomy and Pathoanatomic of Lumbosacral PlexusДокумент33 страницыAnatomy and Pathoanatomic of Lumbosacral PlexusRachmad FaisalОценок пока нет
- Nerve Pain and Nerve Damage 2Документ17 страницNerve Pain and Nerve Damage 2Ryan BediОценок пока нет
- Ataxias Neuro Condition DetailedДокумент80 страницAtaxias Neuro Condition DetailedMikail AtiyehОценок пока нет
- Cerebellar StrokeДокумент17 страницCerebellar StrokeAna CotomanОценок пока нет
- Acute Spinal Cord InjuryДокумент3 страницыAcute Spinal Cord InjuryMarisol Dellera ValmoriaОценок пока нет
- DD ScrotumДокумент4 страницыDD ScrotumAy HaanОценок пока нет
- Sequelae of Trumatic Brain InjuryДокумент19 страницSequelae of Trumatic Brain InjuryAnurag SuryawanshiОценок пока нет
- Foot and AnkleДокумент21 страницаFoot and AnkleAli MullaОценок пока нет
- Introduction To Intervertebral Disc Anatomy, Pivd (Lumbar) and Its ManagementДокумент104 страницыIntroduction To Intervertebral Disc Anatomy, Pivd (Lumbar) and Its ManagementVivek SaxenaОценок пока нет
- Neuro-Coordination Umair PTДокумент20 страницNeuro-Coordination Umair PTFatima SeharОценок пока нет
- Joint, Connective Tissue, and Bone Disorders and ManagementДокумент47 страницJoint, Connective Tissue, and Bone Disorders and ManagementAmbreen TariqОценок пока нет
- Neurogenic Bladder: When Nerve Damage Causes Bladder ProblemsДокумент3 страницыNeurogenic Bladder: When Nerve Damage Causes Bladder ProblemsmarselamgeОценок пока нет
- Herniated Disc orДокумент10 страницHerniated Disc orChristine Marie BationОценок пока нет
- What Is PolymyositisДокумент24 страницыWhat Is PolymyositisAshraf MobyОценок пока нет
- Hamstring InjuriesДокумент6 страницHamstring InjuriesIlian GeorgievОценок пока нет
- Budgeting Workshop PowerPointДокумент13 страницBudgeting Workshop PowerPointCj SmithОценок пока нет
- Motor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)Документ2 страницыMotor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)james cordenОценок пока нет
- Body Coordination (Mohd Fahim Mohd Farid 4ukm)Документ17 страницBody Coordination (Mohd Fahim Mohd Farid 4ukm)Tham SuperОценок пока нет
- Reflex ExamДокумент4 страницыReflex ExamDan Ali100% (1)
- Check Unit 557 Jan-Feb Genetics v3 PDFДокумент36 страницCheck Unit 557 Jan-Feb Genetics v3 PDFdragon66Оценок пока нет
- Week 1 and 2 PCP Workbook QuestionsДокумент4 страницыWeek 1 and 2 PCP Workbook Questionsapi-479717740100% (1)
- Scapulohumeral PeriarthritisДокумент29 страницScapulohumeral PeriarthritisMárcia PatríciaОценок пока нет
- Ankle Sprain - UpToDateДокумент48 страницAnkle Sprain - UpToDateDavid RyanОценок пока нет
- Week 3 - PCPДокумент3 страницыWeek 3 - PCPapi-479754549100% (1)
- Nerve Compression Syndromes: (Sindroma Jebakan)Документ51 страницаNerve Compression Syndromes: (Sindroma Jebakan)Astri Kartika SariОценок пока нет
- Types of Synovial JointsДокумент7 страницTypes of Synovial Jointsaulia nurfadillahОценок пока нет
- Tuberculosis of Hip JointДокумент25 страницTuberculosis of Hip JointYousra ShaikhОценок пока нет
- PNF FullДокумент46 страницPNF FullHUZAIFA YAMAAN100% (1)
- Clinical Practice GuidelinesДокумент2 страницыClinical Practice GuidelinesEddie WyattОценок пока нет
- Pi Is 0091674906013704Документ2 страницыPi Is 0091674906013704Eddie WyattОценок пока нет
- Pi Is 0091674906013704Документ2 страницыPi Is 0091674906013704Eddie WyattОценок пока нет
- EngДокумент48 страницEngnina nurhayatiОценок пока нет
- Analisis Penetapan Kriteria Kawasan HutanДокумент14 страницAnalisis Penetapan Kriteria Kawasan HutanHarunHasibОценок пока нет
- Jurnal Terapi FaringitisДокумент7 страницJurnal Terapi Faringitisarstantyar0% (1)
- Prophylactic Antipyretics For Prevention of Febrile Seizures Following VaccinationДокумент3 страницыProphylactic Antipyretics For Prevention of Febrile Seizures Following VaccinationEddie WyattОценок пока нет
- Baca Sebelum Instal GameДокумент1 страницаBaca Sebelum Instal GameEddie WyattОценок пока нет
- 59 15-68Документ7 страниц59 15-68Eddie WyattОценок пока нет
- Normal-Pressure Hydrocephalus: Roger SalloumДокумент2 страницыNormal-Pressure Hydrocephalus: Roger SalloumEddie WyattОценок пока нет
- Osteoporosis NOGG Guideline 2017Документ36 страницOsteoporosis NOGG Guideline 2017Claudia Micu100% (1)
- Baca Sebelum Instal GameДокумент1 страницаBaca Sebelum Instal GameEddie WyattОценок пока нет
- Guidline TetanusДокумент363 страницыGuidline TetanusferianaОценок пока нет
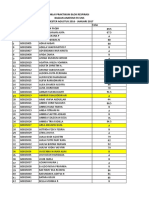
- Absensi PraktikumДокумент18 страницAbsensi PraktikumEddie WyattОценок пока нет
- Absensi PraktikumДокумент18 страницAbsensi PraktikumEddie WyattОценок пока нет
- Daftar PustakaДокумент5 страницDaftar PustakaEddie WyattОценок пока нет
- Kumpulan Osce Ukmppd - BimaДокумент2 страницыKumpulan Osce Ukmppd - BimaEddie Wyatt0% (1)
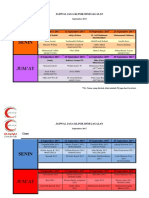
- Jadwal Jaga Klinik Bsmi Jagalan September 2017Документ8 страницJadwal Jaga Klinik Bsmi Jagalan September 2017Eddie WyattОценок пока нет
- Infant Feeding PracticeДокумент46 страницInfant Feeding PracticeEddie WyattОценок пока нет
- Obat BaksosДокумент1 страницаObat BaksosEddie WyattОценок пока нет
- NIlai 2016Документ31 страницаNIlai 2016Eddie WyattОценок пока нет
- Obat BaksosДокумент1 страницаObat BaksosEddie WyattОценок пока нет
- Zam 7116Документ6 страницZam 7116DdCasadoLasterosОценок пока нет
- Pembahasan Soal UB10 Muskulo 2010Документ10 страницPembahasan Soal UB10 Muskulo 2010Eddie WyattОценок пока нет
- DMS 2014 - B - Basic of Bone & Joint InfectionДокумент28 страницDMS 2014 - B - Basic of Bone & Joint InfectionEddie WyattОценок пока нет
- Jadwal Pembelajaran Laboratorium Anatomi Fakultas Kedokteran UNS IMO 2017Документ1 страницаJadwal Pembelajaran Laboratorium Anatomi Fakultas Kedokteran UNS IMO 2017Eddie WyattОценок пока нет
- Nail Loss: Oleh: Hananto Wildan Habibi (G0014111)Документ11 страницNail Loss: Oleh: Hananto Wildan Habibi (G0014111)Eddie WyattОценок пока нет
- The Fractured Femur: Directed Readings in The ClassroomДокумент68 страницThe Fractured Femur: Directed Readings in The ClassroomEddie Wyatt100% (1)
- TriageДокумент14 страницTriageNiko AndreanОценок пока нет
- Tara Liska ResumeДокумент4 страницыTara Liska Resumeapi-384128955Оценок пока нет
- Rehabilitation Rcpsych Report 2009Документ46 страницRehabilitation Rcpsych Report 2009psychforall100% (2)
- Dental Plans and Rates: Bay AreaДокумент6 страницDental Plans and Rates: Bay AreaJDanaОценок пока нет
- Baclofen KemstroДокумент2 страницыBaclofen KemstroKristi WrayОценок пока нет
- Plugged Milk Ducts and Nipple Blebs: What Are The Symptoms of A Plugged Milk Duct?Документ4 страницыPlugged Milk Ducts and Nipple Blebs: What Are The Symptoms of A Plugged Milk Duct?MuhammadRajifОценок пока нет
- 00 Statistical Report 2016Документ248 страниц00 Statistical Report 2016wudthipanОценок пока нет
- Blood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical CareДокумент48 страницBlood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical Carehagir alhajОценок пока нет
- Adverse Reaction Blood BankДокумент10 страницAdverse Reaction Blood BankyourfamilydoctorОценок пока нет
- Copd and Cor PulmonalДокумент14 страницCopd and Cor PulmonalAldi RafaelОценок пока нет
- Merchant Shipping (Medicines, Medical Stores and Appliances) Rules, 1994Документ18 страницMerchant Shipping (Medicines, Medical Stores and Appliances) Rules, 1994pravenОценок пока нет
- FUNDA NotesДокумент63 страницыFUNDA NotesNina Anne Paracad0% (1)
- EC2021-Medical Electronics Notes For All Five UnitsДокумент147 страницEC2021-Medical Electronics Notes For All Five UnitsJason Jackson100% (1)
- The Wick: The Magazine of Hartwick College - Summer 2011Документ56 страницThe Wick: The Magazine of Hartwick College - Summer 2011Stephanie BrunettaОценок пока нет
- Hypo ReviewДокумент5 страницHypo ReviewShreyans DamadeОценок пока нет
- ADHDДокумент2 страницыADHDMerijn MattheijssenОценок пока нет
- Trait Theory of PersonalityДокумент5 страницTrait Theory of PersonalityBenitez GheroldОценок пока нет
- GONIOMETRYДокумент6 страницGONIOMETRYchloegmndzОценок пока нет
- PredictiveДокумент7 страницPredictiveAlbert VijayОценок пока нет
- Entire Pharm ClassДокумент173 страницыEntire Pharm ClassnancyОценок пока нет
- CBT OutlineДокумент2 страницыCBT OutlineRoss Laurenne FortunadoОценок пока нет
- Assessing Dehydration in ChildrenДокумент40 страницAssessing Dehydration in ChildrenDr. Jayesh PatidarОценок пока нет
- Fractures of Radius and Ulnar Shaft: Dima HabanjarДокумент56 страницFractures of Radius and Ulnar Shaft: Dima HabanjarDima HabanjarОценок пока нет
- Pediatric Osteomyelitis: Annisa Nur ArifinДокумент18 страницPediatric Osteomyelitis: Annisa Nur ArifinWahyu Adhitya PrawirasatraОценок пока нет
- Metabolic Bone Diseases: Dr. R.C.JindalДокумент73 страницыMetabolic Bone Diseases: Dr. R.C.JindalpriyankОценок пока нет
- Dana Ullman HomeopathyДокумент4 страницыDana Ullman Homeopathydavid_moloneyОценок пока нет
- Bronchodilators and Other Respiratory DrugsДокумент44 страницыBronchodilators and Other Respiratory DrugsastriedamaliaamanatОценок пока нет
- Autism DyslexiaДокумент2 страницыAutism DyslexiaAutismDyslexiaОценок пока нет
- Traumatic Brain Injury PresentationДокумент14 страницTraumatic Brain Injury Presentationapi-413607178Оценок пока нет