Академический Документы
Профессиональный Документы
Культура Документы
Abscesses Maxillo: Vittorio Carlino MGE VI
Загружено:
Vittorio Carlino0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров31 страницаAbcesses maxillofacciale
Оригинальное название
Abscesses maxillo
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документAbcesses maxillofacciale
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров31 страницаAbscesses Maxillo: Vittorio Carlino MGE VI
Загружено:
Vittorio CarlinoAbcesses maxillofacciale
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 31
Abscesses maxillo
Vittorio Carlino MGE VI
Inflammation may spread
in three ways:
1.
By passing through tissue
spaces and planes.
2.
By way of the lymphatic
system.
3. By way of blood circulation.
Most Common Teeth and Associated
Periodontium Involved in Clinical Presentations
of Abscesses and Fistulae.
Maxillary vestibule
Maxillary central or lateral incisor, all surfaces, and roots.
Maxillary canine, all surfaces, and roots (short roots below levator anguli
oris).
Maxillary premolars, buccal surfaces, and roots.
Maxillary molars, buccal surfaces, or buccal roots (short roots below
buccinator).
Penetration of nasal floor
Maxillary central incisor, roots.
Maxillary canine, all surfaces, and root (long root above levator anguli oris).
Palate
Maxillary lateral incisor, lingual surfaces, and roots. Maxillary premolars,
lingual surfaces, and roots. Maxillary molars, lingual surfaces, or palatal
roots.
Perforation Into maxillary sinus
Maxillary molars, buccal surfaces, and buccal roots (long roots). Maxillary
molars, buccal surfaces, and buccal roots (long roots above buccinator).
Mandibular first and second molars, buccal surfaces, and buccal roots (long
roots below buccinator).
Mandibular vestibule
Mandibular incisors, all surfaces, and roots (short roots above mentalis).
Mandibular canine and premolars, all surfaces, and roots (all roots above
depressors).
Mandibular first and second molars, buccal surfaces, and roots (short roots
above buccinator).
Buccal space infection
Submandibular space
Most Common Teeth and Associated
Periodontium Involved in Clinical
Presentations of Abscesses and Fistulae.
Submental skin region
Mandibular incisors, roots (long roots below mentalis).
Sublingual region
Mandibular first molar, lingual surfaces, and roots (all roots
above mylohyoid). Mandibular second molar, lingual
surfaces, and roots (short roots above mylohyoid).
Submandibular skin region
Mandibular second molar, lingual surfaces, and roots (long
roots below mylohyoid). Mandibular third molars, all
surfaces, and roots (all roots below mylohyoid).
Surgical treatment of facial
space infection
Possible Space. Teeth, and Periodontium Involved With a Clinical
Presentation of Phlegmon from the Spread of Dental Infection.
SPREAD BY SPACES
The spaces of the head and neck can allow
the spread of infection from the teeth and
associated oral tissues because the
pathogens can travel within the fascial
planes, from one space near the infected
site to another distant space, by the
spread of the related inflammatory
exudate. When involved in infections, the
space can undergo phlegmon or abscess,
which can cause a change in the normal
proportions of the face.
Frontal section of the head and neck highlighting the
submandibular and sublingual spaces.
SPREAD BY LYMPHATICS
The lymphatics of the head and neck can
allow the spread of infection from the
teeth and associated oral tissues. This
occurs because the pathogens can travel
in the lymph through the lymphatics that
connect the series of nodes from the oral
cavity to other tissues or organs. Thus,
these pathogens can move from a primary
node near the infected site to a secondary
node at a distant site .
Superficial cervical lymph nodes
and associated structures.
Deep cervical lymph nodes and
associated structures.
SPREAD BY THE BLOOD
SYSTEM
The blood system of the head and
neck can allow the spread of
infection from the teeth and
associated oral tissues, because
pathogens can travel in the veins
and drain the infected oral site into
other tissues or organs. The spread
of dental infection by way of the
blood system can occur from
bacteremia or an infected thrombus.
Pathways of the internal jugular vein and facial
vein, as well as the location of the cavernous
venous sinus.
SPREAD TO THE PARANASAL
SINUSES
The paranasal sinuses of the skull can
become infected through the direct spread
of infection from the teeth and associated
oral tissues, resulting in a secondary
sinusitis. A perforation in the wall of the
sinus can also be caused by an infection.
Secondary sinusitis of dental origin occurs
mainly with the maxillary sinuses, since
the maxillary posterior teeth and
associated tissues are in close proximity to
these sinuses.
Lateral view of the skull and the
paranasal sinuses.
Dental abscess
An abscess is an accumulation of
pus. Pus is a thick fluid that
usually contains white blood
cells, dead tissue and bacteria
(germs). The usual cause of an
abscess is an infection with
bacteria. A dental abscess is an
infection in the centre of a tooth
which spreads through the tooth
to infect supporting bone and
other nearby tissues.
Dental abscess
Dental abscess is common. It may
develop as a complication of tooth
decay (caries), or from an infection
in the gums.
CAUSES
The cause of these infections is direct growth of the
bacteria from an existing cavity into the soft tissues
and bones of the face and neck.
An infected tooth that has not received
appropriate dental care can cause a dental
abscess to form. Poor oral hygiene, (such
as not brushing and flossing properly or
often enough) can cause cavities to form
in your teeth. The infection then may
spread to the gums and adjacent areas
and become a painful dental abscess.
Classification abscesses and
phlegmons of maxillofacial area:
1.Abscesses and phlegmons of the
maxilla region.
2.Abscesses and phlegmons of the
mandible region.
3.Abscesses and phlegmons of the
bottom oral cavity.
4.Abscesses and phlegmons of the
tongue and of the neck.
Symptoms of a dental abscess
include:
Pain (toothache) which can quickly become
worse. It can be severe and throbbing.
Swelling of the gum which can be tender.
Swelling of the face. The skin over an abscess
may become red and inflamed.
The affected tooth may become tender to touch,
and may even become loose.
High temperature and feeling generally unwell.
In severe cases there may be spasm of the jaw
muscles with difficulty swallowing and/or
breathing.
PHYSICIAN DIAGNOSIS
A doctor or dentist can determine by
physical examination if you have a
drainable abscess. X-rays of the
teeth may be necessary to show
small abscesses that are at the
deepest part of the tooth. Signs
observed by the doctor, including
nausea, vomiting, fever, chills, or
diarrhea, may indicate that the
infection has progressed to the point
where it is making your whole body
sick.
PHYSICIAN TREATMENT
The doctor may decide to cut open the
abscess and allow the pus to drain. Unless
the abscess ruptures on its own, this is
the only way that the infection can be
cured. People with dental abscesses are
typically prescribed pain relievers and, at
the discretion of the doctor, antibiotics to
fight the infection. An abscess that has
extended to the floor of the mouth or to
the neck may need to be drained in the
operating room under anesthesia.
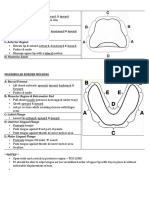
Directions of cuts during treatment of
purulent processes in maxillofacial area.
Directions of cuts during treatment of
purulent processes in maxillofacial area.
Prognosis
If treated, the outlook is good. The pus
can usually be drained and the tooth can be
saved if it is not badly broken down.
If left untreated, complications may
develop which can include:
Spread of infection
The abscess may 'burst' onto the skin of the face,
or into the mouth. This may leave a sinus tract (a
channel) between a persistent focus of infection
and the skin or mouth which can discharge pus
from time to time.
Cavernous sinus thrombosis - a serious infection
and clotting of a blood vessel in the brain.
Sinusitis - spread of infection to the nearby sinus
in the face bone.
A dental cyst (fluid filled cavity) may develop.
Thank you for
attention
Вам также может понравиться
- Muscle Evolution Posing HandbookДокумент17 страницMuscle Evolution Posing HandbookKels100% (1)
- Dance Terms and Ballet Blah Blah BlahДокумент11 страницDance Terms and Ballet Blah Blah BlahColton CarrigoОценок пока нет
- Tooth Form & Function - IДокумент32 страницыTooth Form & Function - IMasayi K MackatianiОценок пока нет
- Inferior Alveolar Nerve BlockДокумент7 страницInferior Alveolar Nerve BlockSyedMuhammadJunaidОценок пока нет
- Impacted Wisdom Tooth, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandImpacted Wisdom Tooth, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Delayed Eruption PDFДокумент6 страницDelayed Eruption PDFIsharajini Prasadika Subhashni GamageОценок пока нет
- 1.GIT All DisordersДокумент240 страниц1.GIT All DisordersCabdisacid yasinОценок пока нет
- Development of Occlusion 1 PDFДокумент5 страницDevelopment of Occlusion 1 PDFFadiShihabОценок пока нет
- HyperpituitarismДокумент3 страницыHyperpituitarismGerardLumОценок пока нет
- Advanced Tooth Morphology, Tooth Identification and Enamel COH Senior StudentsДокумент10 страницAdvanced Tooth Morphology, Tooth Identification and Enamel COH Senior StudentsshuankayОценок пока нет
- D-Dentin-Lec 1Документ45 страницD-Dentin-Lec 1api-3710331100% (7)
- Periodical Test in Science 6Документ4 страницыPeriodical Test in Science 6jocelynberlin100% (2)
- Mouth Preparation and Master Cast in Removable PartialДокумент45 страницMouth Preparation and Master Cast in Removable PartialSrishti SrivastavaОценок пока нет
- 5-Aetiology of MalocclusionДокумент7 страниц5-Aetiology of MalocclusionKhalid Mortaja100% (1)
- Diagnosis and Management of Odontogenic InfectionsДокумент52 страницыDiagnosis and Management of Odontogenic InfectionsAhmed EmadОценок пока нет
- 3rd Molars ExtractionДокумент48 страниц3rd Molars ExtractionJessica Wu100% (1)
- Space AnalysisДокумент43 страницыSpace AnalysismarieОценок пока нет
- Management of Class II Div IДокумент13 страницManagement of Class II Div Iapi-19840404Оценок пока нет
- Flap Surgery 2Документ38 страницFlap Surgery 2Fah100% (1)
- Oral Anatomy ReviewerДокумент57 страницOral Anatomy ReviewerJEVELYN D. TUMBAGAОценок пока нет
- Anat 5.2 Pelvis and Perineum - ElevazoДокумент14 страницAnat 5.2 Pelvis and Perineum - Elevazolovelots1234Оценок пока нет
- Teeth Eruption WordДокумент24 страницыTeeth Eruption WordAhmed hegazyОценок пока нет
- Fixed Orthodontic ApplianceДокумент45 страницFixed Orthodontic ApplianceBudi AthAnza SuhartonoОценок пока нет
- Patología Bucal - Bruch (Ingles)Документ176 страницPatología Bucal - Bruch (Ingles)MarielEsmeraldaОценок пока нет
- All Dental AnatomyДокумент114 страницAll Dental AnatomyKhanh NguyễnОценок пока нет
- Nuclear MedicineДокумент7 страницNuclear MedicineMarco Mendoza67% (3)
- Tooth Carving Exercise As A Foundation For Future Dental Career - A ReviewДокумент3 страницыTooth Carving Exercise As A Foundation For Future Dental Career - A ReviewRik ChatterjeeОценок пока нет
- MFL Women BeginnerДокумент13 страницMFL Women Beginneramey patkarОценок пока нет
- Oral Surgery FlapДокумент14 страницOral Surgery Flapdiaz2050Оценок пока нет
- Selection and Arrangement of Teeth For Complete Dentures: By: Dr. Rohan BhoilДокумент84 страницыSelection and Arrangement of Teeth For Complete Dentures: By: Dr. Rohan BhoilMaqbul AlamОценок пока нет
- Oral Surgery Volume 4, Extraction and Impacted TeethДокумент32 страницыOral Surgery Volume 4, Extraction and Impacted TeethskyangkorОценок пока нет
- Development of OcclusionДокумент9 страницDevelopment of OcclusionЕленаОценок пока нет
- Anterior Open BiteДокумент34 страницыAnterior Open BiteAbdullah100% (1)
- ParaplegiaДокумент56 страницParaplegiarashid38Оценок пока нет
- Chapter 1 - Practical Notions Concerning Dental Occlusion: Personal InformationДокумент61 страницаChapter 1 - Practical Notions Concerning Dental Occlusion: Personal InformationEmil Costruț100% (1)
- Chronology of Tooth DevelopmentДокумент20 страницChronology of Tooth DevelopmentPrince Ahmed100% (1)
- Chapter 17 Maxillary Sinus - SlidesДокумент40 страницChapter 17 Maxillary Sinus - SlidesRajat GuptaОценок пока нет
- Tarrson Family Endowed Chair in PeriodonticsДокумент54 страницыTarrson Family Endowed Chair in PeriodonticsAchyutSinhaОценок пока нет
- Understanding Masticatory Function in Unilateral CrossbitesОт EverandUnderstanding Masticatory Function in Unilateral CrossbitesОценок пока нет
- 3D-CT Evaluation of Facial Asymmetry in Patients With Maxillofacial DeformitiesДокумент9 страниц3D-CT Evaluation of Facial Asymmetry in Patients With Maxillofacial DeformitiesR KОценок пока нет
- Clasificare Carii Dentare Otr Cariologie An IIIДокумент79 страницClasificare Carii Dentare Otr Cariologie An IIIStefana NanuОценок пока нет
- Border Molding PDFДокумент1 страницаBorder Molding PDFNajeeb UllahОценок пока нет
- Anatomi Radiologi Tulang Dan Sendi: Oleh: Yeti Kartikasari, ST, M.KesДокумент51 страницаAnatomi Radiologi Tulang Dan Sendi: Oleh: Yeti Kartikasari, ST, M.KesHilmi NovrianОценок пока нет
- 3D Teeth ReconstructionДокумент0 страниц3D Teeth ReconstructionSamir Alberita KeljmendiОценок пока нет
- Tooth DevelopmentДокумент36 страницTooth DevelopmentDaffa YudhistiraОценок пока нет
- Andrews 6 Keys of Normal OcclusionДокумент2 страницыAndrews 6 Keys of Normal OcclusionKaren AlfredОценок пока нет
- Dental Anatomy - Lecture 4Документ17 страницDental Anatomy - Lecture 4Mohamed Harun B. SanohОценок пока нет
- 1 Introduction and Ideal OcclusionДокумент33 страницы1 Introduction and Ideal OcclusionJASPREETKAUR0410100% (1)
- Lec 5 P 4Документ5 страницLec 5 P 4brshlwnytwaftkhr956Оценок пока нет
- Morphology of Permanent CaninesДокумент15 страницMorphology of Permanent Caninesamanita238Оценок пока нет
- Dental Anatomy - Lecture 2Документ9 страницDental Anatomy - Lecture 2Mohamed Harun B. SanohОценок пока нет
- Pulp and Periapical: - Also Notes From Biopsy TechniquesДокумент31 страницаPulp and Periapical: - Also Notes From Biopsy TechniquesmythaiuОценок пока нет
- Individual Tooth MalpositionsДокумент9 страницIndividual Tooth MalpositionsWiet Sidharta0% (1)
- Mandibular NerveДокумент8 страницMandibular NerveSridevi KОценок пока нет
- Characterization Art of CamouflageДокумент33 страницыCharacterization Art of CamouflageVikas Aggarwal100% (1)
- Anatomy For Complete DentureДокумент45 страницAnatomy For Complete Dentureisraa0dentist100% (5)
- Esthetic Considerations in Interdental Papilla PDFДокумент11 страницEsthetic Considerations in Interdental Papilla PDFXavier AltamiranoОценок пока нет
- Endodontic Treatment of Dens InvaginatusДокумент7 страницEndodontic Treatment of Dens InvaginatusParidhi GargОценок пока нет
- Tooth DevelopmentДокумент20 страницTooth DevelopmentArslan Jokhio0% (1)
- 4.2 Scaling and Root Planning Lec2 PDFДокумент49 страниц4.2 Scaling and Root Planning Lec2 PDFAbdulrahman Al-MukhtarОценок пока нет
- Extraction of Primary TeethДокумент6 страницExtraction of Primary TeethmirfanulhaqОценок пока нет
- Serial ExtractionДокумент21 страницаSerial Extractionabhay_narayane34560% (1)
- TX of Endodontic EmergenciesДокумент7 страницTX of Endodontic EmergenciesNovia SetyowatiОценок пока нет
- Examination, Diagnosis and Treatment Planning For Edentulous or Partially Edentulous PatientsДокумент73 страницыExamination, Diagnosis and Treatment Planning For Edentulous or Partially Edentulous PatientsMohamedОценок пока нет
- Avulsion: DEFINITION: - Tooth Avulsion (Exarticulation) Implies Total Displacement of The ToothДокумент39 страницAvulsion: DEFINITION: - Tooth Avulsion (Exarticulation) Implies Total Displacement of The Toothshailesh_shenoyОценок пока нет
- MAXILLAДокумент21 страницаMAXILLACamille MagdirilaОценок пока нет
- Tooth Morphology Basics: Howard Chi, D.M.DДокумент79 страницTooth Morphology Basics: Howard Chi, D.M.DMihaela Vasiliu0% (1)
- Development of The Maxilla: Dr. Samson NegussieДокумент38 страницDevelopment of The Maxilla: Dr. Samson NegussieLintoОценок пока нет
- Dental Anatomy and PhysiologyДокумент36 страницDental Anatomy and PhysiologyCpt.WnchstrОценок пока нет
- A Beginners Guide To Lateral Cephalometric RadiographsДокумент4 страницыA Beginners Guide To Lateral Cephalometric RadiographsClaudiaОценок пока нет
- Logbook Spring 2023Документ79 страницLogbook Spring 2023Horn DudeОценок пока нет
- Library of Teachings - Preparatory Exercises For Lungs Magnetic Field and Deep Meditation - ©the-Teachings-Of-Yogi-BhajanДокумент7 страницLibrary of Teachings - Preparatory Exercises For Lungs Magnetic Field and Deep Meditation - ©the-Teachings-Of-Yogi-BhajanValentinaZoccaОценок пока нет
- PDF]Jan-Febc 2010 - Jaypee Brothers Medical Publishers jaypeebrothers.com/pdf/cataloginmonths/jan-feb2010.pdf by S Bhat - 2010 A unique book on clinical methods in surgery along with interactive DVD-ROM ... and clinical approach to each and individual surgical cases .... including a brief outline on prognosis. • Provides in-depth ..... Susmita Bhattacharya. Epidemiology. mbbs books - Scribd https://www.scribd.com/doc/239765747/mbbs-books Sep 15, 2014 - mbbs books - Download as Word Doc (.doc / .docx), PDF File (.pdf), Text ... BHATTACHARYA SHORT CASES IN SURGERY 5TH 2002 200.00 BOOKS1 - Scribd https://www.scribd.com/doc/99385577/BOOKS1 Jul 7, 2012 - BOOKS1 - Ebook download as PDF File (.pdf), Text file (.txt) or read book ... LAWRENCE W. SHORT CASES IN SURGERY / BHATTACHARYA, ... Medical Books - mbbs exam questions for second third and ... hafeesh.blogspot.com/2009/12/medical-books.html Dec 25, 2009 - GUPTE SHORT TEXTBOOK OF MEDICAL MICROBIOLOGY 8TH 2002 .... BHATTACHARYA SHORT CASESДокумент3 страницыPDF]Jan-Febc 2010 - Jaypee Brothers Medical Publishers jaypeebrothers.com/pdf/cataloginmonths/jan-feb2010.pdf by S Bhat - 2010 A unique book on clinical methods in surgery along with interactive DVD-ROM ... and clinical approach to each and individual surgical cases .... including a brief outline on prognosis. • Provides in-depth ..... Susmita Bhattacharya. Epidemiology. mbbs books - Scribd https://www.scribd.com/doc/239765747/mbbs-books Sep 15, 2014 - mbbs books - Download as Word Doc (.doc / .docx), PDF File (.pdf), Text ... BHATTACHARYA SHORT CASES IN SURGERY 5TH 2002 200.00 BOOKS1 - Scribd https://www.scribd.com/doc/99385577/BOOKS1 Jul 7, 2012 - BOOKS1 - Ebook download as PDF File (.pdf), Text file (.txt) or read book ... LAWRENCE W. SHORT CASES IN SURGERY / BHATTACHARYA, ... Medical Books - mbbs exam questions for second third and ... hafeesh.blogspot.com/2009/12/medical-books.html Dec 25, 2009 - GUPTE SHORT TEXTBOOK OF MEDICAL MICROBIOLOGY 8TH 2002 .... BHATTACHARYA SHORT CASESSaiSuryaTeja0% (1)
- Anatomical Landmarks of Denture Bearing Areas - Mandible PresentationДокумент19 страницAnatomical Landmarks of Denture Bearing Areas - Mandible PresentationAdil Kaukab100% (1)
- Beginner & Advanced Rotator Cuff Exercises For Shoulder Pain - MyodetoxДокумент18 страницBeginner & Advanced Rotator Cuff Exercises For Shoulder Pain - MyodetoxJustin Wigon100% (1)
- Bhoyar 2011Документ6 страницBhoyar 2011Ahmad zakОценок пока нет
- Assistive Devices For WalkingДокумент4 страницыAssistive Devices For Walkingthomasfinley44Оценок пока нет
- Autonomic Innervation of Abdomen and PelvisДокумент6 страницAutonomic Innervation of Abdomen and PelvisTahir MahmoodОценок пока нет
- Shivanshu Gangwar M. Pharma (Pharmaceutics)Документ16 страницShivanshu Gangwar M. Pharma (Pharmaceutics)Shibbu GangwarОценок пока нет
- Cardiac - Anatomy of The HeartДокумент9 страницCardiac - Anatomy of The HeartRiya ThoratОценок пока нет
- Integumentary, Anatomy, FunctionДокумент1 страницаIntegumentary, Anatomy, Functionviandi diniОценок пока нет
- Mosbys Essentials For Nursing Assistants 5Th Edition Sorrentino Test Bank Full Chapter PDFДокумент38 страницMosbys Essentials For Nursing Assistants 5Th Edition Sorrentino Test Bank Full Chapter PDFShawnHessbody100% (10)
- Comparison Between Antegrade Nailing and Retrograde Nailing in Humeral Diaphyseal FracturesДокумент5 страницComparison Between Antegrade Nailing and Retrograde Nailing in Humeral Diaphyseal FracturesPrabhakaran NarayanasamyОценок пока нет
- 7 Structural Organisation in Animals PPT - Part 5Документ22 страницы7 Structural Organisation in Animals PPT - Part 5Jeevan RaajОценок пока нет
- Spinal Manual 20 August 2004Документ235 страницSpinal Manual 20 August 2004Forum PompieriiОценок пока нет
- PID L4-L5 (Case Study)Документ67 страницPID L4-L5 (Case Study)NannieОценок пока нет
- 01.05.2018 To 12.05.2018Документ22 страницы01.05.2018 To 12.05.2018SunilОценок пока нет
- Ankle-Foot Orthoses and Footwear For Children With Cerebral PalsyДокумент10 страницAnkle-Foot Orthoses and Footwear For Children With Cerebral Palsypt.mahmoudОценок пока нет
- Epithelial Tissue (Finale)Документ2 страницыEpithelial Tissue (Finale)Adz Na HarОценок пока нет
- NIH Public Access: Clinical Examination of The Rotator CuffДокумент26 страницNIH Public Access: Clinical Examination of The Rotator CuffCasian TripacОценок пока нет






































































![PDF]Jan-Febc 2010 - Jaypee Brothers Medical Publishers jaypeebrothers.com/pdf/cataloginmonths/jan-feb2010.pdf by S Bhat - 2010 A unique book on clinical methods in surgery along with interactive DVD-ROM ... and clinical approach to each and individual surgical cases .... including a brief outline on prognosis. • Provides in-depth ..... Susmita Bhattacharya. Epidemiology. mbbs books - Scribd https://www.scribd.com/doc/239765747/mbbs-books Sep 15, 2014 - mbbs books - Download as Word Doc (.doc / .docx), PDF File (.pdf), Text ... BHATTACHARYA SHORT CASES IN SURGERY 5TH 2002 200.00 BOOKS1 - Scribd https://www.scribd.com/doc/99385577/BOOKS1 Jul 7, 2012 - BOOKS1 - Ebook download as PDF File (.pdf), Text file (.txt) or read book ... LAWRENCE W. SHORT CASES IN SURGERY / BHATTACHARYA, ... Medical Books - mbbs exam questions for second third and ... hafeesh.blogspot.com/2009/12/medical-books.html Dec 25, 2009 - GUPTE SHORT TEXTBOOK OF MEDICAL MICROBIOLOGY 8TH 2002 .... BHATTACHARYA SHORT CASES](https://imgv2-2-f.scribdassets.com/img/document/270707806/149x198/154b6610c1/1605034206?v=1)
















