Академический Документы
Профессиональный Документы
Культура Документы
Poliomyelitis
Загружено:
adericky84100%(1)100% нашли этот документ полезным (1 голос)
97 просмотров14 страницPoliomyelitis, commonly known as polio, is caused by infection with the poliovirus. There are three serotypes of the poliovirus. The virus typically enters the body through the mouth and replicates in the throat and gastrointestinal tract before spreading to the nervous system where it can cause paralysis. Most polio infections are asymptomatic, but it can cause a range of symptoms from minor illness to paralysis. There is no cure for polio, so treatment focuses on rehabilitation and prevention through vaccination.
Исходное описание:
slide kuliah poliomyelitis
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документPoliomyelitis, commonly known as polio, is caused by infection with the poliovirus. There are three serotypes of the poliovirus. The virus typically enters the body through the mouth and replicates in the throat and gastrointestinal tract before spreading to the nervous system where it can cause paralysis. Most polio infections are asymptomatic, but it can cause a range of symptoms from minor illness to paralysis. There is no cure for polio, so treatment focuses on rehabilitation and prevention through vaccination.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
100%(1)100% нашли этот документ полезным (1 голос)
97 просмотров14 страницPoliomyelitis
Загружено:
adericky84Poliomyelitis, commonly known as polio, is caused by infection with the poliovirus. There are three serotypes of the poliovirus. The virus typically enters the body through the mouth and replicates in the throat and gastrointestinal tract before spreading to the nervous system where it can cause paralysis. Most polio infections are asymptomatic, but it can cause a range of symptoms from minor illness to paralysis. There is no cure for polio, so treatment focuses on rehabilitation and prevention through vaccination.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 14
infection with a member of the genus
Enterovirus known as poliovirus (RNA viruses).
This group of prefers to inhabit the
gastrointestinal tract
Three serotypes of poliovirus have been
identified—poliovirus type 1 (PV1), type 2
(PV2), and type 3 (PV3). PV1 is the most
commonly encountered form, and the one
most closely associated with paralysis.
Rapidly inactivated by heat, formaldehyde,
chlorine, ultraviolet light
Entry into mouth
Replication in pharynx, GI tract,
local lymphatics
Hematologic spread to lymphatics
and central nervous system
Viral spread along nerve fibers
Destruction of motor neurons
The disease is transmitted primarily via the
fecal-oral route, by ingesting contaminated
food or water
occasionally transmitted via the oral-oral
route
Outcome Proportion of cases[
Asymptomatic 90 – 95%
Minor illness 4 – 8%
Non-paralytic aseptic 1 - 2%
meningitis
Paralytic poliomyelitis 0,1 – 1,5%
— Spinal polio 79% of paralytic cases
— Bulbospinal polio 19% of paralytic cases
— Bulbar polio 2% of paralytic cases
Bulbospinal Polio
• Accounts for 19%
of paralytic cases
• Virus attack motor
neuron anterior
cornu spinal
flaccid
• Affects extremities
and cranial nerves
• Leads to severe
respiratory
involvement
• Accounts for 2% of
paralytic polio
• Virus attacks
motor neurons in
brainstem
• Affects cranial
nerve function
• Primarily inhibits
ability to breathe,
speak, and swallow
effectively
acute onset of flaccid paralysis in one or more limbs
with decreased or absent tendon reflexes in the
affected limbs, that cannot be attributed to another
apparent cause, and without sensory or cognitive loss
Early symptoms of paralytic polio include high fever,
headache, stiffness in the back and neck,
asymmetrical weakness of various muscles, sensitivity
to touch, difficulty swallowing, muscle pain, loss of
superficial and deep reflexes, paresthesia (pins and
needles), irritability, constipation, or difficulty
urinating. Paralysis generally develops one to ten days
after early symptoms begin, progresses for two to
three days, and is usually complete by the time the
fever breaks.
Poliovirus the mouth, infecting the pharynx (throat) and
intestinal mucosa. It gains entry by binding to a immunoglobulin-
like receptor.
The virus begins to replicate. Poliovirus divides within
gastrointestinal cells for about a week, from where it spreads to
the tonsils, the intestinal lymphoid tissue, and the deep cervical
and mesenteric lymph nodes, where it multiplies abundantly.
The virus is subsequently absorbed into the bloodstream –>
Known as viremia, the presence of virus in the bloodstream
enables it to be widely distributed throughout the body. Poliovirus
can survive and multiply within the blood and lymphatics for long
periods of time, sometimes as long as 17 weeks. In a small
percentage of cases, it can spread and replicate in other sites
such as the reticuloendothelial tissues, and Rarely, this may
progress and the virus may invade the central nervous system,
provoking a local inflammatory response.
In most cases this causes a self-limiting inflammation of the
meninges, which is known as non-paralytic aseptic.The
mechanisms by which poliovirus spreads to the CNS are poorly
understood
A laboratory diagnosis : from a stool
sample or a swab of the pharynx.
Antibodies to poliovirus can be diagnostic,
and are generally detected in the blood of
infected patients early in the course of
infection.Analysis of the patient's
cerebrospinal fluid (CSF), which is collected
by a lumbar puncture ("spinal tap"), reveals
an increased number of white blood cells
(primarily lymphocytes)
There is no cure for polio
Supportive measures include
antibiotics to prevent infections in
weakened muscles,
analgesics for pain, moderate
exercise and a nutritious diet.
Treatment of polio often requires
long-term rehabilitation, including
physical therapy, braces, corrective
shoes and, in some cases,
orthopedic surgery
Vaccine
Two vaccines are used
throughout the world to
combat polio
1. was developed in 1952
by Jonas Salk Salk
vaccine, or inactivated
poliovirus vaccine (given
by injection)
2. Albert Sabin in 1960
developed an oral polio
vaccine
Вам также может понравиться
- Poliomyelitis: Abarca, Mark Nerza, Lourelie BSN3-AДокумент45 страницPoliomyelitis: Abarca, Mark Nerza, Lourelie BSN3-Arhimineecat71Оценок пока нет
- Upper Motor Neuron PDFДокумент3 страницыUpper Motor Neuron PDFkevin_jawanОценок пока нет
- Low Back PainДокумент34 страницыLow Back PainFAMED RESIDENTS CESMEDОценок пока нет
- Advances in The Diagnosis & Management of Neck Pain - Article.Документ19 страницAdvances in The Diagnosis & Management of Neck Pain - Article.salmankhan09215Оценок пока нет
- Muscular DystrophyДокумент3 страницыMuscular Dystrophyderrickmason626Оценок пока нет
- Okubadeja N - Epidemiology and Classification of Movement DisordersДокумент50 страницOkubadeja N - Epidemiology and Classification of Movement DisordersVictoria NatashaОценок пока нет
- Crush Injury and Crush Syndrome PDFДокумент2 страницыCrush Injury and Crush Syndrome PDFMichael DrakeОценок пока нет
- Cranial Nerve Exam Part1Документ9 страницCranial Nerve Exam Part1Jennifer Pisco LiracОценок пока нет
- Fibromyalgia 2010Документ68 страницFibromyalgia 2010Dicky Ariyono BumbunganОценок пока нет
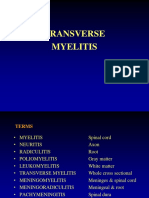
- Transverse MyelitisДокумент19 страницTransverse MyelitisAnonymous YHQmN8a01100% (1)
- Motor Neuron DiseaseДокумент8 страницMotor Neuron DiseaseyigoОценок пока нет
- Prof. Dr. Dr. Eka J. Wahjoepramono, M.D.,PHDДокумент52 страницыProf. Dr. Dr. Eka J. Wahjoepramono, M.D.,PHDAndrew Sabastian Geraldyno Paago100% (1)
- Patent Ductus ArteriosusДокумент31 страницаPatent Ductus ArteriosussuderiОценок пока нет
- Antithrombotic Therapy For VTE Disease CHEST Guideline and Expert Panel ReportДокумент38 страницAntithrombotic Therapy For VTE Disease CHEST Guideline and Expert Panel ReportAdriana VasilicaОценок пока нет
- Module 1 - NeuropsychologyДокумент4 страницыModule 1 - Neuropsychologyaysha farihaОценок пока нет
- Optic Nerve PathologiesДокумент64 страницыOptic Nerve Pathologieshasan aslamОценок пока нет
- LMN VS UmnДокумент10 страницLMN VS UmnyosuaОценок пока нет
- Viral MeningitisДокумент22 страницыViral MeningitisdariailmasariОценок пока нет
- Peripheral Nerve InjuriesДокумент12 страницPeripheral Nerve InjuriesJiggs LimОценок пока нет
- Juvenile Idiopathic ArthritisДокумент52 страницыJuvenile Idiopathic ArthritishasanajОценок пока нет
- Ring Enhancing LesionsДокумент50 страницRing Enhancing LesionsVivek GuptaОценок пока нет
- Cerebellar Disorders: Dr. Mohamed Nasreldin HamdoonДокумент14 страницCerebellar Disorders: Dr. Mohamed Nasreldin HamdoonMohamed Nasreldin HamdoonОценок пока нет
- Pathology of Peripheral Nerve and Skeletal Muscle - DAДокумент46 страницPathology of Peripheral Nerve and Skeletal Muscle - DASinta Dewi AdityaniОценок пока нет
- Presented By:: Ali Jaber Al-Faifi Salman NasserДокумент23 страницыPresented By:: Ali Jaber Al-Faifi Salman NasserCalvin PrasetioОценок пока нет
- Infections of The Central Nervous System08Документ47 страницInfections of The Central Nervous System08Annisa SasaОценок пока нет
- Low Back Pain: Department of Neurology Christian University of Indonesia Medical FacultyДокумент23 страницыLow Back Pain: Department of Neurology Christian University of Indonesia Medical FacultySandra Anastasia GultomОценок пока нет
- Diseases of Spine andДокумент37 страницDiseases of Spine andgunawan djayaОценок пока нет
- RS2480 Amputation 2018Документ49 страницRS2480 Amputation 2018Hung Sarah100% (1)
- Brachial Plexus InjuryДокумент21 страницаBrachial Plexus InjurySemi IqbalОценок пока нет
- Acute and Chronic Chorea in Childhood: Donald L. Gilbert, MD, MSДокумент6 страницAcute and Chronic Chorea in Childhood: Donald L. Gilbert, MD, MSKalindraParahitaОценок пока нет
- Spinal Cord Injury PDFДокумент14 страницSpinal Cord Injury PDFNiaОценок пока нет
- Diagnosis Skdi Neuro NewДокумент49 страницDiagnosis Skdi Neuro NewmerrykartikaОценок пока нет
- Patogenesis TBДокумент46 страницPatogenesis TBJaya Semara PutraОценок пока нет
- 3A Neurology FlashcardsДокумент14 страниц3A Neurology FlashcardsJustin ChangОценок пока нет
- Movement Disorders 4335Документ28 страницMovement Disorders 4335Fitri Amelia RizkiОценок пока нет
- Pediatric Limbs DeformitiesДокумент139 страницPediatric Limbs DeformitiesrachmadyОценок пока нет
- SSPEДокумент8 страницSSPEJanellah batuaan100% (1)
- Juvenile Idiopathic ArthritisДокумент4 страницыJuvenile Idiopathic ArthritisAmmarОценок пока нет
- Cervical SpondylosisДокумент25 страницCervical Spondylosisjeevan ghimireОценок пока нет
- CNS Congenital AnomaliesДокумент74 страницыCNS Congenital AnomaliesMoh DrhusseinyОценок пока нет
- Types of Cerebral Herniation and Their Imaging FeaturesДокумент42 страницыTypes of Cerebral Herniation and Their Imaging FeaturesRazan AlayedОценок пока нет
- Diabetic NeuropathyДокумент9 страницDiabetic Neuropathyapi-511118388Оценок пока нет
- Difference Between Hypersplenism and SplenomegalyДокумент6 страницDifference Between Hypersplenism and SplenomegalyshahikamunaferОценок пока нет
- Motor Neuron DiseaseДокумент24 страницыMotor Neuron DiseasemanikantatssОценок пока нет
- Undergraduate Neurosurgery Lecture NotesДокумент124 страницыUndergraduate Neurosurgery Lecture NotesLuquiitas LasernaОценок пока нет
- Cervical SpondylosisДокумент9 страницCervical SpondylosisNurHidayah Borhanudin100% (1)
- Pseudo BulbarДокумент5 страницPseudo BulbarRegina CaeciliaОценок пока нет
- Pulmonary Rehabilitation: Airway DiseasesДокумент7 страницPulmonary Rehabilitation: Airway DiseasesshivamptОценок пока нет
- Stroke Syndromes (Etiology & Clinical Features)Документ40 страницStroke Syndromes (Etiology & Clinical Features)nisha_m_patel2006Оценок пока нет
- December 2013 What Is Necrotizing Fasciitis? What Are Its Causes? How Will You Manage Such A Case?Документ3 страницыDecember 2013 What Is Necrotizing Fasciitis? What Are Its Causes? How Will You Manage Such A Case?Vaibhav BharatОценок пока нет
- Cerebral InfarctionДокумент2 страницыCerebral InfarctionMarie Aurora Gielbert MarianoОценок пока нет
- Approach To AtaxiaДокумент6 страницApproach To AtaxiaVivek KumarОценок пока нет
- Final Coma StimulationДокумент23 страницыFinal Coma StimulationpreetisagarОценок пока нет
- The "when" and "where" of α-synucleinopathies: Insights from REM sleep behavior disorderДокумент3 страницыThe "when" and "where" of α-synucleinopathies: Insights from REM sleep behavior disorderSandsackОценок пока нет
- Deep Vein ThrombosisДокумент5 страницDeep Vein ThrombosisnikaaraaaОценок пока нет
- R.N. Kapoor Memorial Homoeopathic Hospital & Medical College, INDOREДокумент12 страницR.N. Kapoor Memorial Homoeopathic Hospital & Medical College, INDOREvinay patidar100% (1)
- Meningocele & Spina BifidaДокумент21 страницаMeningocele & Spina BifidakeynechristaОценок пока нет
- Peripheral Neuropathy: By: R'Syah ESI NeurologistДокумент39 страницPeripheral Neuropathy: By: R'Syah ESI Neurologistraynhard b. fandres100% (2)
- ASIA Impairment ScaleДокумент10 страницASIA Impairment Scaleazimahzainal211Оценок пока нет
- Chapter 11Документ25 страницChapter 11Marjorie PuzoОценок пока нет
- The Spiritist Review - Journal of Psychological Studies - 1864 - January - Healing MediumsДокумент5 страницThe Spiritist Review - Journal of Psychological Studies - 1864 - January - Healing MediumsWayne BritoОценок пока нет
- Karling Aguilera-Fort ResumeДокумент4 страницыKarling Aguilera-Fort Resumeapi-3198760590% (1)
- Youcastr Case StudyДокумент2 страницыYoucastr Case StudyMomina NadeemОценок пока нет
- CatalysisДокумент50 страницCatalysisnagendra_rdОценок пока нет
- May 29Документ2 страницыMay 29gerrymattinglyОценок пока нет
- Usher Hall, Edinburgh: HistoryДокумент1 страницаUsher Hall, Edinburgh: HistoryTarun TangoОценок пока нет
- BBB 4M1 Summative Article ExpectationsДокумент3 страницыBBB 4M1 Summative Article ExpectationsMuhammad SherazОценок пока нет
- Application of A One-Dimensional Large-Strain Consolidation Model To A Fullscale Tailings Storage Facility PDFДокумент11 страницApplication of A One-Dimensional Large-Strain Consolidation Model To A Fullscale Tailings Storage Facility PDFchenОценок пока нет
- Sacred Books of The East Series, Volume 47: Pahlavi Texts, Part FiveДокумент334 страницыSacred Books of The East Series, Volume 47: Pahlavi Texts, Part FiveJimmy T.100% (1)
- J. C. Penney and Ron JohnsonДокумент8 страницJ. C. Penney and Ron JohnsonadamОценок пока нет
- PPSC Lecturer Mathematics 2004Документ1 страницаPPSC Lecturer Mathematics 2004Sadia ahmadОценок пока нет
- Brand Relevance - 1Документ2 страницыBrand Relevance - 1Ayan PandaОценок пока нет
- How To Reset AutoCAD To Defaults - AutoCAD 2019 - Autodesk Knowledge NetworkДокумент11 страницHow To Reset AutoCAD To Defaults - AutoCAD 2019 - Autodesk Knowledge NetworkZina MorОценок пока нет
- Bts Kat ArmyДокумент3 страницыBts Kat ArmyBeakatrine CabreraОценок пока нет
- Azevedo Slum English 1926Документ90 страницAzevedo Slum English 1926Nealon Isaacs100% (1)
- FIDP Business Ethics and Social Responsibility PDFДокумент7 страницFIDP Business Ethics and Social Responsibility PDFRachell Mae Bondoc 1Оценок пока нет
- Z Transform Part 1 PDFДокумент16 страницZ Transform Part 1 PDFAnanth SettyОценок пока нет
- Elasticity of Demand: Managerial EconomicsДокумент41 страницаElasticity of Demand: Managerial EconomicsSomasundaram LakshminarasimhanОценок пока нет
- Restitution of Conjugal RightsДокумент3 страницыRestitution of Conjugal Rightsvalerian fernandesОценок пока нет
- Sampling TechДокумент5 страницSampling TechJAMZ VIBESОценок пока нет
- Translator Resume SampleДокумент2 страницыTranslator Resume SampleIsabel JimenezОценок пока нет
- Dacera Vs Dela SernaДокумент2 страницыDacera Vs Dela SernaDarlo HernandezОценок пока нет
- Life in The Middle Ages Unit Study - Grade 8Документ21 страницаLife in The Middle Ages Unit Study - Grade 8HCSLearningCommonsОценок пока нет
- KISS Notes The World CommunicatesДокумент30 страницKISS Notes The World CommunicatesJenniferBackhus100% (4)
- Continue: Struggle For Pakistan I H Qureshi PDFДокумент3 страницыContinue: Struggle For Pakistan I H Qureshi PDFDESI Mp350% (2)
- Silk Road ActivityДокумент18 страницSilk Road Activityapi-332313139Оценок пока нет
- 5990 3285en PDFДокумент16 страниц5990 3285en PDFLutfi CiludОценок пока нет
- LLCE CoursДокумент18 страницLLCE CoursDaphné ScetbunОценок пока нет
- Kutuzov A Life in War and Peace Alexander Mikaberidze 2 Full ChapterДокумент67 страницKutuzov A Life in War and Peace Alexander Mikaberidze 2 Full Chapterjanice.brooks978100% (6)