Академический Документы
Профессиональный Документы
Культура Документы
Hypertension 08.08.2018
Загружено:
Emily Eresuma0 оценок0% нашли этот документ полезным (0 голосов)
227 просмотров13 страницPediatric Morning Report
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документPediatric Morning Report
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
227 просмотров13 страницHypertension 08.08.2018
Загружено:
Emily EresumaPediatric Morning Report
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 13
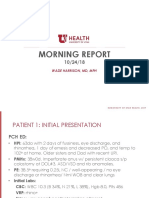
11 year old male, previously healthy, presenting
with chest pain after doing a flip on a trampoline,
over rotating, and landing his chest on his knees and
thighs
Vitals
BP 172/106 (197/143), HR 72, T 36.8, RR 22,
97%RA WT 42 kg, HT 159cm
PE
Tenderness to palpation over chest
WHAT DO YOU WANT TO
DO?
DIFFERENTIAL
Workup
• Normal CXR, no labs
DC
• Follow-up with cardiology
• 178/136
Cardiology (6 days later)
173/119
ECG, ECHO, labs
Ordered renal US w/ doppler, started
on Amlodipine 5mg, sent to
FOLLOW-UP nephrology
Nephrology (2 days later)
158/108
UA normal
Ordered CTA
• Based on age, height percentile, gender
• Measured manually, proper sized cuff, RUE
Hypertension is sustained elevation of
systolic or diastolic BP at or above 95%ile
(Stage I between 95-99%ile, Stage II
>99%ile)
Hypertensive Urgency
Elevated BP without acute target organ
damage
Hypertensive Emergency
Elevated BP with acute target organ
damage (CV, CNS, kidneys)
Hypertensive Encephalitis
HA, emesis, temp change, vision change,
ataxia, AMS)
Should have gotten:
UA, Chem, CBC, +/- CXR, head CT, ECG
When stable: Renal US with doppler,
complement C3, ANA, ECHO, renin,
aldosterone, TSH, tox screen
Cardiac – Coarctation, KD
Renal – SLE, RAS, renal parenchymal disease (reflux, PKD, AKI),
transplant, glomerulonephritis
Endocrine – Metabolic disorder, diabetes, obesity hyperthyroid or
hypothyroid, mineralcorticoid excess (hyperaldosteronism)
Onc – Wilms, pheochromocytoma
Other – White coat hypertension, steroids, stimulants, Williams,
essential, increased ICP, trauma, OSA, ingestions/toxins, NSAID
5-10% of childhood hypertension
Includes:
Fibromuscular dysplasia, vasculitis (Takayasu’s, PAN), extrinsic
compression (tumor, trauma), syndromes (NF1, tuberous sclerosis,
Williams’, Marfans), other (radiation, UAC, trauma, transplant)
Urgent: PICU -> Nicardipine,
labetolol drip, nitroprusside aim for
~ 25% reduction
Medical: Antihypertensives
TREATMENT Amlodipine (Ca channel blocker)
Don’t use ACE or ARB initially if
unknown diagnosis
Cause-specific Treatment
• Labs – CBC, CMP, UA, thyroid studies,
Workup • Renal US with doppler, NO ECHO!
• If primary HTN -> ACE, ARB
Medication • If unknown -> Amlodipine
• Nephrology (secondary workup),
Referrals ophthomology
Chronic, large vessel disease of unknown etiology
Affects aorta and major branches
Inflammation of vessel wall, with infiltration by T-cells, NK, plasma cells,
macrophages -> narrowing, fibrosis, aneurysm
Presents with non-specific findings- malaise, weight loss, fever, htn,
abdominal pain
Labs nonspecific – elevated ESR, CRP when active. Nee CTA!
Later – diminished pulses, claudication, fibrosis, aneurysms, renal failure,
cardiac ischemia or failure, stroke
Treatment includes steroids, MTX, other steroid sparing, angioplasty and
stents
20% have monophasic course; 93% survival at 5 years
Вам также может понравиться
- Kidney Disorders 03.27.2019Документ33 страницыKidney Disorders 03.27.2019Emily EresumaОценок пока нет
- Food Challenge 03.20.2019Документ17 страницFood Challenge 03.20.2019Emily EresumaОценок пока нет
- Ophtho Pearls 03.13.2019Документ17 страницOphtho Pearls 03.13.2019Emily EresumaОценок пока нет
- Board Prep Metabolics Feb 2019Документ23 страницыBoard Prep Metabolics Feb 2019Emily EresumaОценок пока нет
- Dangers of Vaping 03.15.2019Документ23 страницыDangers of Vaping 03.15.2019Emily EresumaОценок пока нет
- Pediatric Hypertension Noon Conference 03.20.2019Документ44 страницыPediatric Hypertension Noon Conference 03.20.2019Emily EresumaОценок пока нет
- Morning Report Case Presentation: APRIL 1, 2019Документ14 страницMorning Report Case Presentation: APRIL 1, 2019Emily EresumaОценок пока нет
- Investing 101 For Residents: RJ Nemeyer MDДокумент12 страницInvesting 101 For Residents: RJ Nemeyer MDEmily EresumaОценок пока нет
- Case Presentation: Tad MiyaДокумент41 страницаCase Presentation: Tad MiyaEmily EresumaОценок пока нет
- Board Prep Genetics Dec 2018Документ62 страницыBoard Prep Genetics Dec 2018Emily EresumaОценок пока нет
- Tachycardia How To Keep Your Patient Alive in The Middle of The NightДокумент30 страницTachycardia How To Keep Your Patient Alive in The Middle of The NightEmily Eresuma100% (1)
- Somatization 01.28.2019Документ28 страницSomatization 01.28.2019Emily EresumaОценок пока нет
- Bells Palsy or Stroke 02.06.2019Документ19 страницBells Palsy or Stroke 02.06.2019Emily EresumaОценок пока нет
- Board Prep GI Jan 2019Документ32 страницыBoard Prep GI Jan 2019Emily EresumaОценок пока нет
- Board Prep Emergency Ingestions Dec.2018Документ46 страницBoard Prep Emergency Ingestions Dec.2018Emily EresumaОценок пока нет
- Chronic Granulomatous Disease 01.23.2019Документ10 страницChronic Granulomatous Disease 01.23.2019Emily EresumaОценок пока нет
- Anemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentДокумент16 страницAnemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentEmily EresumaОценок пока нет
- Morning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Документ24 страницыMorning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Emily EresumaОценок пока нет
- Ventilators 11.07.2018Документ38 страницVentilators 11.07.2018Emily EresumaОценок пока нет
- Pertussis 01.14.2019Документ29 страницPertussis 01.14.2019Emily EresumaОценок пока нет
- Morning Report: Melanie Nelson, PGY-2Документ25 страницMorning Report: Melanie Nelson, PGY-2Emily EresumaОценок пока нет
- Wilderness Medicine 11.20.2018Документ12 страницWilderness Medicine 11.20.2018Emily EresumaОценок пока нет
- Limping 12.10.2018Документ32 страницыLimping 12.10.2018Emily Eresuma100% (1)
- Jaundice 11.28.2018Документ13 страницJaundice 11.28.2018Emily EresumaОценок пока нет
- Morning Report: Lindsey Gakenheimer-Smith MD PGY3Документ20 страницMorning Report: Lindsey Gakenheimer-Smith MD PGY3Emily EresumaОценок пока нет
- Morning Report: Wade Harrison, MD, MPHДокумент13 страницMorning Report: Wade Harrison, MD, MPHEmily EresumaОценок пока нет
- MysteryCase 10.22.18Документ10 страницMysteryCase 10.22.18Emily EresumaОценок пока нет
- Pediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Документ35 страницPediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Emily EresumaОценок пока нет
- Halloween Safety: Dominique ChevalierДокумент21 страницаHalloween Safety: Dominique ChevalierEmily EresumaОценок пока нет
- Foster Care in Utah: Marlayna DespresДокумент11 страницFoster Care in Utah: Marlayna DespresEmily EresumaОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Radiology ReviewerДокумент26 страницRadiology ReviewerSean Jodi CosepeОценок пока нет
- Motion Is LotionДокумент2 страницыMotion Is LotionQing JyulyanОценок пока нет
- Sindromul - De.epuizare (Bourn-Out) La Medici. F Matache. Full PDFДокумент10 страницSindromul - De.epuizare (Bourn-Out) La Medici. F Matache. Full PDFCosmin BurleanuОценок пока нет
- Ocular EmergencyДокумент29 страницOcular EmergencyMohammad Farouq Omar100% (3)
- 30947630Документ12 страниц30947630carolinapolotorresОценок пока нет
- Peripheral Blood SmearДокумент46 страницPeripheral Blood SmearAris ResurreccionОценок пока нет
- Unicef in IndiaДокумент22 страницыUnicef in IndiaNamita Kothari100% (1)
- Equine Field SurgeryДокумент6 страницEquine Field SurgeryRuchiОценок пока нет
- Five Overall Health-Improving Benefits of Royal JellyДокумент2 страницыFive Overall Health-Improving Benefits of Royal JellyHayCurtis38Оценок пока нет
- HIV SeminarДокумент45 страницHIV SeminarDelphy VargheseОценок пока нет
- Test 1 Part 1 TapecsriptДокумент19 страницTest 1 Part 1 TapecsriptMerryОценок пока нет
- 2020-21 Big Game Status BookДокумент200 страниц2020-21 Big Game Status BookAaron Meier0% (1)
- HPV Vaccination: It'S Us Against The Human PapillomavirusДокумент30 страницHPV Vaccination: It'S Us Against The Human Papillomavirussalam majzoubОценок пока нет
- FREE Ace Essays - Miss CivicДокумент13 страницFREE Ace Essays - Miss CivicLOVENNATH A/L RAVI Moe100% (1)
- Fenotipos Sepsis 3Документ5 страницFenotipos Sepsis 3Gerardo LermaОценок пока нет
- Eng PDFДокумент98 страницEng PDFMark Anthony MadridanoОценок пока нет
- Drug-Food Interactions in Anti-Cancer TherapyДокумент16 страницDrug-Food Interactions in Anti-Cancer Therapyさゆう FayaОценок пока нет
- Chapter 1 Serology DZ 2010Документ77 страницChapter 1 Serology DZ 2010Anduamlak TeferaОценок пока нет
- Abduraham Rayyan-Module-Cardiovascular-SystemДокумент17 страницAbduraham Rayyan-Module-Cardiovascular-SystemRAYYAN ENIL ABDURAHAMОценок пока нет
- RESEARCH (Edited)Документ6 страницRESEARCH (Edited)Navarrete, AliceОценок пока нет
- Healthy Foods and The Body Parts They ResembleДокумент4 страницыHealthy Foods and The Body Parts They ResembleRobert AndujarОценок пока нет
- Banana Leaf ScanningДокумент24 страницыBanana Leaf ScanningFatima Dela Cruz LascanoОценок пока нет
- Physiology Biochemistry Gen Surgery AnswersДокумент7 страницPhysiology Biochemistry Gen Surgery AnswersSanОценок пока нет
- Focusing On Children Mental HealthДокумент2 страницыFocusing On Children Mental HealthDzatil HusniОценок пока нет
- 2013 ASA Guidelines Difficult AirwayДокумент20 страниц2013 ASA Guidelines Difficult AirwayStacey WoodsОценок пока нет
- Nle Final Coaching Jul 3-4-2021Документ1 страницаNle Final Coaching Jul 3-4-2021Linsae HiyasОценок пока нет
- Cardioogy and Nephrology, MCQ'sДокумент5 страницCardioogy and Nephrology, MCQ'sLong Live PakistanОценок пока нет
- EAES 2015 Scientific Program BucharestДокумент14 страницEAES 2015 Scientific Program BucharestIulia NiculaeОценок пока нет
- Biol 312 - Internal 2004Документ1 страницаBiol 312 - Internal 2004api-3763291Оценок пока нет
- Case Taking Proforma - Respiratory SystemДокумент7 страницCase Taking Proforma - Respiratory SystemK Haynes Raja100% (11)